Abstract
Purpose
To investigate the anatomic characteristics of eyes with pathological myopia and peripapillary intrachoroidal cavitation (ICC) located temporal to the optic disc.
Methods
A total of 125 with pathologic myopia were scanned with swept-source optical coherence tomography (OCT). Temporal ICC was defined as ICC located temporal to the optic disc seen in horizontal OCT section through the optic disc center. Definition of pathologic myopia was refractive error >8.00 diopters (D) or an axial length >26.5 mm.
Results
In all, 17 eyes of 16 patients had temporal ICC. All of the eyes had temporal or temporally wider annular conus. The ICC was observed temporal to the optic disc in 15 of 17 eyes, and 2 of the remaining eyes also had inferior ICC. Even in the two eyes with both temporal and inferior ICC, the temporal ICC was much wider than the inferior ICC. Inner retinal defect at the border of conus and temporal ICC was detected in two eyes. The temporal ICC was extensive in the posterior fundus with the average width of 1467.8±1328.1 μm (range; 442–6200 μm) in a horizontal section. In two eyes, the temporal ICC extended beyond the central fovea.
Conclusions
Peripapillary ICC can develop temporal to the optic disc without involving the area inferior to optic disc in highly myopic eyes. Temporal ICC appeared much wider than inferior ICC, which is usually restricted to the area around the optic disc. The possible reasons why ICC develops in temporal to the optic disc are presented.
Similar content being viewed by others
Introduction
A peripapillary intrachoroidal cavitation (ICC) is a yellowish–orange lesion located inferior to the optic nerve in highly myopic eyes.1, 2, 3, 4, 5, 6, 7 This condition was originally reported as a peripapillary detachment of pathologic myopia,2 however, later studies using more recent versions of optical coherence tomographic (OCT) instruments showed that this was not a detachment of the retinal pigment epithelium (RPE) but an ICC.5 We have reported that a peripapillary ICC was observed in 5% (32/631) of eyes with pathologic myopia, and 71% of the eyes with peripapillary ICC had glaucomatous visual field defects.3 A PubMed search on 29 July 2012 using keyword ‘intrachoroidal cavitation’ extracted seven articles1, 5, 6, 8, 9, 10, 11 and a search for ‘peripapillary detachment in pathologic myopia’ extracted nine articles.2, 3, 4, 7, 12, 13, 14 In all of these studies, the peripapillary ICC developed inferior to the optic disc. Even when the peripapillary ICC was extensive around the optic disc, the ICC always involved the area inferior to the optic disc.3
We recently found eyes with peripapillary ICCs, which were located temporal to the optic disc without involving the area inferior to the optic disc. These temporal ICCs differed from the typical inferior peripapillary ICC by being more extensive, and in some cases, extending beyond the central fovea. Also in some cases, an inner retinal defect was observed between the temporal edge of a myopic conus and the ICC. As the inner retinal defect might damage the nerve fibers between the optic nerve and the macular area, it became important to study the characteristics of the temporal ICCs in more detail.
Thus, the purpose of this study was to examine the OCT characteristics of temporally located peripapillary ICCs, and to report the demographic features of the patients with this defect. We also describe two cases with both temporal and inferior ICCs with the temporal ICC much wider than the inferior ICC.
Materials and methods
Patients
Approval was obtained from the ethics committee of the Tokyo Medical and Dental University to perform this retrospective study, and the procedures were used during the examinations conformed to the tenets of the Declaration of Helsinki. A written informed consent was obtained from all participants.
The medical records of highly myopic patients whose papillary and peripapillary regions were examined by swept-source OCT in the High Myopia Clinic of the Tokyo Medical and Dental University were retrospectively reviewed, and the patients who had a peripapillary ICC located temporal to the optic disc, a temporal ICC, were identified. The definition of pathologic myopia was a refractive error (myopic spherical equivalent) >8.00 diopters (D) or an axial length >26.5 mm. All of the participants had a comprehensive ocular examination including measurements of the refractive error (spherical equivalent), axial length with the IOL master (Carl Zeiss Meditec, Dublin, CA, USA), and fundus photography (TRC-50DX, Topcon, Tokyo, Japan).
Swept-source optical coherence tomography (swept-source OCT)
All of the eyes were examined by a prototype swept-source OCT instrument manufactured by Topcon Corporation (Tokyo, Japan). This swept-source OCT system has an A-scan repetition rate of 100 000 Hz, and its light source is a wavelength-sweeping laser centered at 1050 nm with an approximate 100 nm tuning range. However, the effective bandwidth was approximately 60 nm because of the absorption of some of the energy by water. The axial resolution was calculated to be 8 μm in tissue with a lateral resolution of 20 μm. The imaging depth was 2.6 mm in tissue, and the lateral scan length was adjustable.
Three scanning protocols were used: three-dimensional (3D) volumetric scans, raster scans and radial scans. The scan was centered on the center of the optic disc or on the central fovea. The 3D volumetric data were acquired in 0.8 s and each 3D scan covered an area of 6 × 6 mm2 with a 256 (horizontal) × 256 (vertical) A-scan density. To improve the image quality, three consecutive B-scan images were averaged by a weighted moving average method. Each of the raster or radial scans had a lateral scan length of either 6 or 12 mm. A single image was made up of 1024 A-line acquired in 10 ms. Typically, 32 B-scan images were recorded and averaged by post-processing to yield a de-speckled B-scan image. The width of the ICC was measured with the built-in caliper function of the OCT software by one masked author (MM).
All of the patients were examined with a swept-source OCT, and a temporal ICC was detected in a horizontal OCT section through the center of the optic disc. An inferiorly located peripapillary ICCs was determined in a vertical OCT section through the center of the optic disc.
Results
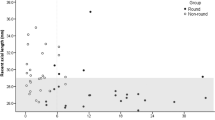
We examined the medical records of 125 patients whose papillary and peripapillary regions were examined by swept-source OCT. Of these, 16 patients (12.8%) were found to have a temporal ICC; 15 were unilateral cases and one was a binocular case. There were 6 men and 10 women whose average age was 60.1±11.8 years with a range of 41 to 85 years. The average refractive error (spherical equivalent) was –15.0±4.1 D with a range of −10.0 to −20.5 D. The average axial length was 29.2±1.4 mm with a range of 26.8–31.0 mm. Sixteen of the eyes had a temporal conus and the remaining eye had an annular conus. All of the 17 eyes had a posterior staphyloma; type I in 1 eye, type II in 2 eyes and type IX in the remaining 14 eyes (Curtin’s classification).12
The funduscopic appearance and fluorescein angiographic findings of eyes with a temporal ICC were very similar to that of the inferior ICC, viz., the ICC appeared as an orange-colored lesion with ill-defined borders in 6 of the 17 eyes (Figures 1 and 3). In the other 11 eyes, the orange color of the temporal ICC was not obvious, and a yellowish chorioretinal atrophy overlying the ICC prevented a clear observation of the color in 6 of these 11 eyes (Figures 4 and 5). The ICC in the other five eyes was detected in the OCT images but was too small to be distinguished ophthalmoscopically. The temporal ICC was hypofluorescent in the early angiographic phase and mildly hyperfluorescent in the late phase in all of the 10 eyes, which were examined angiographically.
(a–d) Appearance of an ICC located temporal to the optic disc in a highly myopic eye with myopic CNV. (a) Fundus photograph of the left eye of a 68-year-old man with a refractive error (spherical equivalent) of −10.0 D and axial length of 27.5 mm. A large temporal conus and scarred CNV (arrow) surrounded by chorioretinal atrophy can be seen. An ill-defined, yellowish–orange lesion can be seen temporal to the optic disc (arrowheads). The OCT scan directions for B, C and D images are shown as white lines with arrows. (b, c) Horizontal OCT scans shown as white lines in Figure a show an ICC temporal to the optic nerve. The sclera is bowed posteriorly in the area of the ICC. The retina is herniated at the border of myopic conus and ICC, and a hyporeflective space suggests the presence of fluid within the cavity of the ICC. (d) Oblique OCT scan shown in Figure a showing an ICC. The ICC extends to the area of the myopic CNV. One large hyporeflective cavity suggests fluid within the ICC. Scale bars=1 mm. (e–j) Findings in an eye with an ICC, which is present temporal to the optic disc in a highly myopic eye with myopic CNV. (e) Fundus photograph of the left eye of a 64-year-old woman with a refractive error of −20.5 D (spherical equivalent) and axial length of 31.0 mm. A large temporal conus and scarred CNV (arrow) with chorioretinal atrophy can be seen. An ill-defined, yellowish–orange lesion is observed temporal to the optic disc (arrowheads). The scanned lines by OCT in Figures c–f are shown as white lines with arrows. (f) Late phase of the fundus fluorescein angiogram shows mild hyperfluorescence (arrowheads) at the corresponding area, which is observed as orange lesion temporal to the optic disc in the color fundus photograph. Scarred CNV shows tissue staining (arrow). (g) Horizontal OCT scan shown in Figure a shows the presence of an ICC temporal to the optic nerve. The sclera is bowed posteriorly in the area of the ICC. The retina is herniated at the border of myopic conus and the inner retina overlying the area between the ICC and conus is very thin. Multiple hyporeflective cavities suggesting the presence of fluid can be seen within the ICC. (h) Adjacent horizontal OCT scan shows an ICC. A CNV is observed as a subretinal elevation in the right part of the figure. Hyporeflective space suggesting the fluid is observed within the cavity of the ICC. (i, j) Vertical OCT scans show that the inner retina is very thin (arrowheads) over the ICC. There is another gap in the layer of retinal pigmented epithelium (RPE) around the inferotemporal retinal vessels (arrows). Scale bars=1 mm.
The OCT findings of the temporal ICC were very similar to those of the inferior ICC.1, 2, 3, 5, 6 The sclera was bowed posteriorly in the area of the ICC (Figures 1 and 2) although the bowing was not obvious in the smaller ICCs. Inner retinal defects were detected at the border of the conus and temporal ICC in two eyes. A slight herniation of the nerve tissue into the ICC was observed in 13 of 17 eyes, and a hyporeflective space in the OCT images suggested the presence of fluid within the ICC in 9 of 17 eyes (Figures 1 and 2). In eyes with no inner retinal defect, there was a triangular thickening of the choroid with the base at the temporal border of the optic disc as we reported for inferior ICCs (Figures 3, 4, 5).1 The choroidal thickening appeared to be accompanied by a stretching of the border between the choroid and optic nerve, that is, the bordering tissue of Jacoby (Figures 2 and 3).13, 14 Also in some cases, a defect was observed in the bordering tissue of Jacoby (Figure 2).
A highly myopic eye with ICC, which is located both temporal and inferior to the optic disc. (a) Fundus photograph of the left eye of a 63-year-old woman with a refractive error of −16.0 D (spherical equivalent) and axial length of 26.8 mm. A small temporal conus can be seen. An ill-defined, yellowish–orange lesion suggestive of a peripapillary ICC is observed inferior to the optic disc. (b) The scanned lines by OCT are shown as white lines with arrows. (c) A long horizontal OCT scan shows a wide ICC temporal to the optic nerve. The ICC is observed to extend beyond the central fovea (arrowhead). A hyporeflective space suggestive of fluid within the ICC is observed. The stretched border tissue (arrow) is seen between the ICC and optic nerve. (d) A long oblique OCT scan shows that temporal ICC spreads temporally beyond the central fovea (arrowhead). A hyporeflective space suggestive of the fluid within the ICC is observed. An intrascleral vessel (arrow), which appears to communicate with the choroid at the ICC area is observed. (e) An oblique OCT scan shows that the border tissue (arrow) is stretched along the margin of the optic nerve and the temporal ICC. (f) A short horizontal OCT scan shows that the border tissue (arrows) is disrupted between the optic disc and temporal ICC. The inner retina is herniated into the ICC in the area where the border tissue is disrupted. (g) A vertical OCT section shows an ICC is present inferior to the optic disc. A disruption of the border tissue between the optic nerve and ICC is also seen (arrow). (h) A vertical OCT scan across the central fovea shows that the subfoveal choroid appears thickened because of the temporal ICC. Scale bars=1 mm.
Findings in an eye with a small ICC temporal to the myopic conus. (a) Fundus photograph of the right eye of a 60-year-old man with a refractive error of −13.5 D (spherical equivalent) and axial length of 30.3 mm. A large temporal conus is seen. An ill-defined, yellowish–orange lesion suggestive of an ICC is observed temporal to the optic disc. The scanned lines by OCT are shown as white lines with arrows. (b) A magnified image of top left panel shows an ill-defined, yellowish–orange lesion suggestive of an ICC (arrowheads) temporal to the optic disc. A small pit is observed within the conus area (arrow). (c) A horizontal OCT scan shows a small ICC temporal to the myopic conus. The choroid appears to be thickened in a triangular manner in the ICC area. The border tissue between myopic conus and temporal ICC is stretched (arrow). A hyporeflective cavity in the area of the conus pit is observed (arrowhead). (d) In an adjacent horizontal OCT scan shows a small ICC temporal to the myopic conus. A conus pit is also observed (arrowhead). (e) A horizontal OCT scan shows a small ICC temporal to the myopic conus. Some tissues (arrowhead) appear to protrude beyond the margin of the retinal pigmented epithelium. (f, g) Vertical OCT scans show that the ICC space is connected to intrascleral blood vessels (arrow). (h) A short horizontal OCT scan shows that an ICC space appears to be connected to an intrascleral blood vessel (arrow). Scale bars=1 mm.
Eyes with a small ICC temporal to the myopic conus. (a) Fundus photograph of the pseudophakic left eye of a 62-year-old woman with an axial length of 30.0 mm. A large temporal conus is seen. Yellowish–orange lesion suggestive of an ICC can be seen but is not obvious because of diffuse chorioretinal atrophy temporal to myopic conus. The scanned lines by OCT are shown as white lines with arrows. (b) An oblique OCT scan shows a small ICC temporal to the myopic conus. The border tissue between the myopic conus and ICC is stretched (arrowhead). (c) Another oblique OCT scan shows a small ICC temporal to myopic conus. A slight herniation of the inner retina into the ICC is seen. (d) An oblique OCT scan shows an ICC temporal to the conus. The sclera is bowed posteriorly in the area of the ICC. Some tissue with mild hyper-reflectivity (arrow) is seen beneath the RPE within the ICC. (e) Fundus photograph of the pseudophakic right eye of a 68-year-old man with an axial length of 30.5 mm. A large temporal conus and macular chorioretinal atrophy around secondary to myopic choroidal neovascularizarion are seen. Yellowish–orange lesion suggestive of ICC is present but is not obvious because of a fusion of the large temporal conus and macular atrophy. The scanned lines by OCT are shown as white lines with arrow. (f) An oblique OCT scan shown in Figure e shows a temporal ICC. A slight herniation of inner retina into the ICC is also seen. Some tissues (arrowhead) appear to protrude beyond the margin of the retinal pigmented epithelium. Scale bars=1 mm.
(a–d) Appearance of a small ICC temporal to the myopic conus. (a) Fundus photograph of the left eye of a 60-year-old man with a refractive error of −12.0 D (spherical equivalent) and with an axial length of 29.0 mm. A large temporal conus and a scarred CNV surrounded by yellowish chorioretinal atrophy can be seen. The yellowish–orange lesion is suggestive of an ICC but is not obvious because of a large temporal conus and macular chorioretinal atrophy around the scarred CNV. The scanned lines by OCT are shown as white lines with arrow. (b) At the border between myopic conus and ICC, the choroid seems to be thickened (arrowhead). The cross-section of branches of Zinn–Haller arterial ring is also seen (arrow). (c) The choroid appears to be thickened in triangular manner in the area of ICC (arrowhead). The CNV is also seen (arrow). (d) A vertical OCT scan shows an ICC temporal to myopic conus. A border tissue between the conus and ICC appears to be stretched (arrow). (e, f) Adjacent vertical OCT scans shown in Figure a shows that the entire thickness of the choroid seems to be attached beneath the RPE in the area of ICC (arrowheads) and the separation appears to occur in the suprachoroidal space. Scale bars=1 mm. (e–h) The patient with a small area of an ICC temporal to myopic conus in one eye. (e) Fundus photograph of the right eye of a 41-year-old man with a refractive error (spherical equivalent) of −10.0 D and an axial length of 27.0 mm. A large temporal conus is seen. Yellowish–orange lesion suggestive of an ICC is present but is not obvious temporal to myopic conus. The scanned line by OCT is shown as white line with arrow. (f) Fundus photograph of the left eye of the same patient with a refractive error (spherical equivalent) of −10.0 D and with an axial length of 26.9 mm. A temporal conus is seen. A yellowish–orange lesion suggestive of an ICC is present but is not obvious temporal to the myopic conus. The scanned line by OCT is shown by the white line with arrow. (g) A horizontal OCT scan across the central fovea shown in Figure a shows that the choroid is thickened in triangular manner just temporal to the myopic conus, and a part of the ICC can be seen. (h) A horizontal OCT scan across the central fovea shown in Figure b shows no thickening of the choroid temporal to the myopic conus. Scale bars=1 mm.
In five eyes, the full thickness of the choroid appeared to be attached to the RPE in the area of the ICC, and the separation of the ICC appeared to occur at the suprachoroidal space (Figures 4 and 5) as we reported for the inferior1 and macular9 ICCs.
In addition to the location, one of the features of temporal ICCs that differentiated them from the inferior ICCs was their extensive width in the posterior fundus. The average width of the temporal ICC in the horizontal OCT scan across the center of the optic disc was 1467.8±1328.1 μm with a range of 442–6200 μm. In two eyes, the temporal ICC extended beyond the central fovea (Figure 2), and in one of these, the subfoveal choroidal thickness in the vertical OCT scan through the fovea appeared thickened because of a separation at the suprachroidal space (Figure 2g).
Two eyes with a temporal ICC also had an inferior ICC, and a direct communication between the two cavities was detected in one of these two eyes (Figure 2). However, even in this patient, the temporal ICC was much wider than the inferior ICC.
In our earlier study on macular ICCs,9 we found intrascleral vessels very close to the area of the cavitation in 19 of 31 eyes with a macular ICC. In this study, we also found intrascleral vessels very close to the area of temporal ICC in 3 of 17 eyes (Figures 2 and 3). One of these three eyes was examined by 3D OCT, and there appeared to be a direct communication between the intrascleral vessels and the vessels in the area of the temporal ICC (Figure 3, Supplementary video 1).
In all, 8 of the 17 eyes (47.1%) in this study had macular chorioretinal atrophy because of the atrophic phase of myopic choroidal neovascularization (myopic CNV). All of these eight eyes did not have an inferior ICC accompanying the temporal ICC. In addition, two of these 17 eyes had a conus pit15 near the temporal ICC (Figure 3).
Conclusion
Our results showed that 15 highly myopic eyes had an ICC temporal to the optic disc that did not extend to the area inferior to the optic disc. We also found two eyes with both inferior and temporal ICC, however, the temporal ICC was much more extensive than the inferior ICC (Figure 2). The appearance of the fundus, angiographic and OCT findings of the temporal ICCs were very similar to those reported for inferior ICCs.1, 2, 3, 5
In addition to its location, a major feature of the temporal ICC was its large size. Although the width of the inferior ICCs was not measured, the inferior ICC appeared to be restricted to the region around the myopic conus in most of the reported cases including ours.1, 2, 3, 5, 6 In this study, the average width of the temporal ICC was 1467.8±1328.1 μm with a maximum value of 6200 μm (Figure 2). In fact, the temporal ICC extended far beyond the central fovea in two eyes.
The characteristics of temporal ICCs did not provide clues on why they tend to be large. One possibility could be that the area temporal to the optic disc between the conus and central fovea might be the area where the mechanical tension is the highest in eyes with pathological myopia. On the other hand in eyes with an inferior ICC, the inferior edge of the staphyloma was generally close to the inferior border of the optic disc, and the inferior ICC did not appear to spread beyond the inferior edge of the staphyloma.
In the two cases where the temporal ICC spread beyond the fovea, the image of a vertical OCT scan across the central fovea looked as if the subfoveal choroid was thickened (Figure 2g). This case in combination with the results of our previous study on macular ICCs9 indicate that it would be better to exclude cases of temporal and macular ICCs in the measurement of the subfoveal choroidal thickness in highly myopic eyes.
It was not determined at which level the ICC separated from the underlying tissue. Although an ICC was originally reported as a cavitation within the choroid, we recently found that the entire thickness of the choroid remained attached onto the RPE in the area of a peripapillary inferior ICC1 or in a macular ICC.9 In eyes with a temporal ICC, we also found that the entire thickness of the choroid was attached to the RPE in the area of the temporal ICC. These observations suggest that the separation of a temporal ICC develops at the level of suprachoroidal space at least in some cases.
The reason why the ICC develops temporal to the optic disc is not clear. All of the eyes with temporal ICC had a temporal or temporally wider annular conus. We suggested that the deformation of the posterior wall of the eye is more pronounced in the area of the conus because overlying layers are thinner than in the more normal regions temporal to the conus.1 Also, we found macular atrophy with scarred CNV in 8 of the 17 eyes with an ICC. Among the 15 eyes with a temporal ICC and without an inferior ICC, 8 (53.3%) had macular atrophy. We recently reported that ICCs are present on and around a patchy chorioretinal atrophy in the macular area, that is, a macular ICC.9 The histological findings of a myopic conus and patchy atrophy are similar; the RPE and choriocapillaris are absent,16 and there is a destruction of the underlying Bruch’s membrane and photoreceptors. Although the intraocular pressure is uniformly distributed on all walls of the eye, the expansion of the posterior wall should be more pronounced in the areas of patchy atrophy or around a myopic conus. Thus, the area between the myopic conus and macular chorioretinal atrophy tends to be greatly stretched because the areas of both the myopic conus and macular atrophy are more stretched than surrounding normal areas. Also, there appears to be a greater adhesion of RPE and scarred CNV, and thus the RPE is relatively less flexible to the mechanical expansive force. This adhesion might act as a force pulling the RPE to the site of foveal CNV and might facilitate the tissue dissociation at the edge of the temporal conus.
In two of the eyes with a temporal ICC, an inner retinal defect was detected along the temporal border of myopic conus. The temporal ICC and the inner retinal defect between the ICC and myopic conus might damage axonal flow of the nerves connecting the central fovea and optic nerve head, which would then result in a central scotoma. However, caution is needed because the central scotoma, which could be caused by temporal ICC might be missed by the concurrent presence of a myopic CNV and macular atrophy.
As we reported in macular ICC,9 large intrascleral vessels were found in close proximity to the area of the temporal ICC in three eyes. Whether there is a causative relationship between the presence of such a large vessel within the sclera and the development of macular or temporal ICC is not conclusive, however, it might be possible that the elasticity and rigidity of the sclera in the area adjacent to such large intrascleral vessels within the thin sclera of highly myopic eyes might be reduced.
There are several limitations in the study. We determined the presence of an inferior ICC in the vertical OCT sections through the center of the optic disc, but it is possible that the inferior ICC is dislocated to inferonasally by a tortion of the optic disc. However, in the 15 eyes we did not detect the inferior ICC also in the inferonasal OCT section in vertical sections (data not shown). As a result of a lack of follow-up data, it is not clear whether the temporal or inferior ICC develops first in the two eyes with both types of ICC. In the eyes with macular atrophy, there still is a possibility that the temporal ICC developed from macular ICC around the macular atrophy. However, the ICC was the deepest at the edge of myopic conus, which suggests that temporal ICC begins from the conus edge. The visual field data were not analyzed because the judgment of central scotoma is difficult in eyes with macular atrophy.
In conclusion, we found peripapillary ICCs which were present temporal to the optic disc. The temporal ICCs tend to be extensive, and in some cases extend beyond the central fovea. The influence of temporal ICC on the visual field in highly myopic eyes needs to be investigated.

References
Spaide RF, Akiba M, Ohno-Matsui K . Evaluation of peripapillary intrachoroidal cavitation with swept source and enhanced depth imaging optical coherence tomography. Retina 2012; 32: 1037–1044.
Freund KB, Ciardella AP, Yannuzzi LA, Pece A, Goldbaum M, Kokame GT et al. Peripapillary detachment in pathologic myopia. Arch Ophthalmol 2003; 121 (2): 197–204.
Shimada N, Ohno-Matsui K, Yoshida T, Yasuzumi K, Kojima A, Kobayashi K et al. Characteristics of peripapillary detachment in pathologic myopia. Arch Ophthalmol 2006; 124 (1): 46–52.
Shimada N, Ohno-Matsui K, Nishimuta A, Tokoro T, Mochizuki M . Peripapillary changes detected by optical coherence tomography in eyes with high myopia. Ophthalmology 2007; 114 (11): 2070–2076.
Toranzo J, Cohen SY, Erginay A, Gaudric A . Peripapillary intrachoroidal cavitation in myopia. Am J Ophthalmol 2005; 140 (4): 731–732.
Wei YH, Yang CM, Chen MS, Shih YF, Ho TC . Peripapillary intrachoroidal cavitation in high myopia: reappraisal. Eye (Lond) 2009; 23 (1): 141–144.
Forte R, Pascotto F, Cennamo G, de Crecchio G . Evaluation of peripapillary detachment in pathologic myopia with en face optical coherence tomography. Eye 2008; 22 (1): 158–161.
Akimoto M, Akagi T, Okazaki K, Chihara E . Recurrent macular detachment and retinoschisis associated with intrachoroidal cavitation in a normal eye. Case Report Ophthalmol 2012; 3 (2): 169–174.
Ohno-Matsui K, Akiba M, Moriyama M, Ishihashi T, Hirakata A, Tokoro T . Intrachoroidal cavitation in macular area of eyes with pathologic myopia. Am J Ophthalmol 2012; 154: 382–393.
Park SC, De Moraes CG, Teng CC, Tello C, Liebmann JM, Ritch R . Enhanced depth imaging optical coherence tomography of deep optic nerve complex structures in glaucoma. Ophthalmology 2012; 119: 3–9.
Faghihi H, Hajizadeh F, Riazi-Esfahani M . Optical coherence tomographic findings in highly myopic eyes. J Ophthalmic Vis Res 2010; 5 (2): 110–121.
Curtin BJ . The posterior staphyloma of pathologic myopia. Trans Am Ophthalmol Soc 1977; 75: 67–86.
Hogan MJ . Optic nerve. Histology of the Human Eye. WB Saunders: Philadelphia, 1971; 527–606.
Anderson DR . Ultrastructure of meningeal sheaths. Normal human and monkey optic nerves. Arch Ophthalmol 1969; 82 (5): 659–674.
Ohno-Matsui K, Akiba M, Moriyama M, Shimada N, Ishibashi T, Tokoro T et al. Acquired optic nerve and peripapillary pits in pathologic myopia. Ophthalmology 2012; 119 (8): 1685–1692.
Dichtl A, Jonas JB, Naumann GO . Histomorphometry of the optic disc in highly myopic eyes with absolute secondary angle closure glaucoma. Br J Ophthalmol 1998; 82 (3): 286–289.
Acknowledgements
We thank Professor Duco Hamasaki for his critical discussion and final manuscript revision. Dr Masahiro Akiba is an employee of Topcon Corporation. This study was supported in part by research grant 22390322 and 23659808 from the Japan Society for the Promotion of Science, Tokyo, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Eye website
Supplementary information
Rights and permissions
About this article
Cite this article
Ohno-Matsui, K., Shimada, N., Akiba, M. et al. Characteristics of intrachoroidal cavitation located temporal to optic disc in highly myopic eyes. Eye 27, 630–638 (2013). https://doi.org/10.1038/eye.2013.16
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2013.16
Keywords
This article is cited by
-
Relationship between the structure and microcirculation of the optic disc region and myopic traction maculopathy in highly myopic eyes
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Advances in myopia research anatomical findings in highly myopic eyes
Eye and Vision (2020)
-
Epidemiologie und Anatomie der Myopie
Der Ophthalmologe (2019)
-
Preserved retinal sensitivity in spatial correspondence to an intrachoroidal cavitation area with full thickness retinal defect: a case report
BMC Ophthalmology (2016)
-
Macular retinal detachment associated with intrachoroidal cavitation in myopic patients
Graefe's Archive for Clinical and Experimental Ophthalmology (2015)