Abstract
Purpose
To prospectively compare the effects of half-dose verteporfin (3 mg/m2) photodynamic therapy (1/2 PDT) with those of one-third-dose verteporfin (2 mg/m2) PDT (1/3 PDT) for chronic central serous chorioretinopathy (CSC).
Methods
Sixteen eyes of 16 consecutive patients with chronic CSC were enrolled and followed up for a 3-month study period. The first 10 patients received 1/2 PDT and the next 6 patients received 1/3 PDT. The resolution rate of subretinal fluid (SRF) was compared between the two groups. The changes in the choroidal thickness inside and outside the PDT-applied area in both groups were also evaluated.
Results
SRF disappeared in all eyes (100%) in the 1/2 PDT group and in two eyes (33%) in the 1/3 PDT group. In the 1/2 PDT group, choroidal thickness inside and outside the PDT-applied area reduced significantly from the baseline (inside, from 387±24 to 325±25 μm; outside, from 292±25 to 249±19 μm; both P=0.005). In the 1/3 PDT group, choroidal thickness decreased in two eyes where SRF disappeared (inside, 87.2 and 90.9% of the baseline; outside, 91.4 and 92.6% of the baseline), but did not change in the other four eyes where SRF remained (inside, 104.1, 100.0, 105.1, and 100.5% of the baseline; outside, 98.9, 103.0, 100.0, and 99.0% of the baseline).
Conclusions
1/2 PDT is more effective than 1/3 PDT in the resolution of SRF for chronic CSC. Decrease in the choroidal thickness after PDT may be related to the resolution of SRF in chronic CSC.
Similar content being viewed by others
Introduction
Central serous chorioretinopathy (CSC) is characterized by an accumulation of subretinal fluid (SRF) in the posterior pole and is a common condition in middle-aged men with a so-called A-type personality.1, 2 Although acute CSC could be resolved spontaneously, approximately half of the patients have recurrence or persistence of SRF and require treatment.3 Laser photocoagulation (LP) is generally used to treat CSC. However, CSC with subfoveal or parafoveal leakage points, and chronic CSC with broad and indistinct leakage are difficult to treat with LP because of the complication of scotoma.4 Choroidal neovascularization (CNV) is also known as a serious complication of LP.5, 6, 7, 8
Recently, photodynamic therapy (PDT) with verteporfin has been shown to be effective in reducing SRF and improving visual acuity for chronic CSC.9, 10, 11, 12 However, post-PDT complications such as secondary CNV, pigmentary changes of the retinal pigment epithelium (RPE), and persistent choriocapillaris hypoperfusion have been reported.10, 13, 14, 15 To minimize these side effects and to obtain the maximum effects, half-dose verteporfin PDT has been conducted successfully in chronic CSC without serious complications.16, 17, 18, 19 However, the optimal dosage of verteporfin required to treat chronic CSC has not been established. The lowest dose of verteporfin required to treat acute CSC successfully was reported to be 30% of the conventional dosage.20 Thus, the purpose of this study was to prospectively compare the results of half-dose verteporfin (3 mg/m2) PDT (1/2 PDT) with those of one-third-dose verteporfin (2 mg/m2) PDT (1/3 PDT) for chronic CSC. The primary outcome measure was the disappearance rate of SRF. Secondary outcome measures were the changes in best-corrected visual acuity (BCVA) and central retinal sensitivity. In addition, we studied the changes in the anatomical structure of the choroid after PDT to find the factors associated with the resolution of SRF.
Materials and methods
Study design and patient recruitment
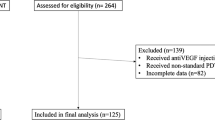
This study was a prospective, non-randomized, consecutive, open-label case series conducted in the Department of Ophthalmology, Nagoya University Graduate School of Medicine. Sixteen eyes of 16 patients with chronic CSC were recruited from July 2009 to January 2010. The first ten patients received 1/2 PDT and the next six patients received 1/3 PDT. Because there was no previous report that showed the effects of 1/3 PDT on chronic CSC, we set the number of patients in the 1/3 PDT group (n=6) lesser than that of the 1/2 PDT group (n=10). CSC was diagnosed if SRF caused by idiopathic leakage from the RPE was present at the macula. Leakage from the RPE was detected by fluorescein angiography. Indocyanine green angiography (ICGA) was used to confirm the presence of choroidal vascular hyperpermeability. The inclusion criteria were the following: (1) presence of SRF involving the foveal region persisting for 3 months or more, (2) difficulty to treat with LP because of leakage from the subfovea, parafovea, or broad area, (3) BCVA between 35 and 85 Early Treatment of Diabetic Retinopathy Study (ETDRS) letters, and (4) age between 20 and 70 years. The exclusion criteria were as follows: (1) previous PDT or focal thermal LP to treat CSC, (2) CNV or other maculopathy, (3) choroidopathy that may affect the choroidal thickness, (4) previous intravitreal injections of anti-vascular endothelial growth factor drugs, and (5) intake of medication such as corticosteroids, adrenergic agonists, or adrenergic antagonists.
Photodynamic therapy
When performing 1/2 PDT and 1/3 PDT, only the dosage of verteporfin (Visudyne; Novartis AG, Bülach, Switzerland) was changed from the conventional PDT recommended by the Age-Related Macular Degeneration with Photodynamic Therapy investigation.21 In 1/2 PDT 3 mg/m2 of verteporfin was infused, and in 1/3 PDT 2 mg/m2 of verteporfin was infused. After treatment, patients were instructed to avoid strong light for 5 days.
Baseline and follow-up examinations
Patients were assessed at baseline and followed up at 4 days, 1 month, and 3 months after PDT. BCVA and macular sensitivity were measured, and optical coherence tomography (OCT) was performed at each visit. The examiners were masked to the type of the treatment that patients received. BCVA was measured using the ETDRS charts at 4 m. Macular sensitivity was evaluated after pupil dilatation using microperimeter-1 (Nidek, Vigonza, Italy). A white Goldmann III spot size was used in a 4-2-1 staircase strategy. Thirty-three stimulus points covering the area of the central 15° diameter around the macula were examined. The average sensitivity of the 33 points was defined as the central retinal sensitivity. At post-PDT visits, the same locations as baseline were examined using the eye-tracking function of microperimeter-1. OCT images were obtained using spectral-domain OCT (Spectralis HRA+OCT, Heidelberg Engineering, Heidelberg, Germany). A series of horizontal scans were taken through the fovea and the area to be treated. The enhanced depth-imaging technique22, 23, 24 was used to obtain the clear images of the choroid. OCT images were used to measure the choroidal thickness, the cross-sectional area of the large choroidal veins, and the vertical and the horizontal diameters of the large choroidal veins. These were measured both inside and outside the PDT-applied area. Fovea was included in the PDT-applied area in all cases. The location examined as inside the PDT-applied area was the subfovea. The location examined as outside the PDT-applied area was one at 1.0 mm temporal distance from the temporal edge of the PDT spot line. Choroidal veins were identified during the venous phase of ICGA. Large veins running perpendicularly to horizontal OCT scans and having a horizontal diameter of >200 μm were defined as the large choroidal vein. The choroidal thickness and the cross-sectional area of the large choroidal veins were evaluated in both treatment groups. The diameters of the large choroidal veins were evaluated in the 1/2 PDT group. The choroidal thickness and the diameters of the large choroidal veins were measured using the built-in caliper function of the Heidelberg Eye Explore software. The cross-sectional area of the large choroidal veins was measured using the NIH Image 1.61 software (developed at the US National Institutes of Health and available on the Internet at http://rsb.info.nih.gov/nih-image/). At post-PDT visits, OCT was performed at the same locations as at baseline by using the eye-tracking function of Spectralis OCT.
The protocol for this prospective study was approved by the Institutional Review Board of Nagoya University Graduate School of Medicine before the study initiation, and written informed consent was obtained from all patients. The procedures of this study followed the tenets of the Declaration of Helsinki.
Statistics
Statistical analyses were performed using PASW statistics version 18.0 (SPSS Inc., IBM Corporation, Chicago, IL, USA). Comparisons were made between the two treatment groups using Fisher's exact test for gender and the disappearance rate of SRF, and using Mann–Whitney U test for the other clinical data. P values of less than 0.05 were considered to be statistically significant.
Wilcoxon signed-rank test with Bonferonni correction was used to compare the baseline clinical data with those of 4 days, 1 month, and 3 months. P values of <0.017 were taken to be statistically significant.
Results
Patients' baseline demographics and clinical data
The baseline demographic and clinical data of the two treatment groups are summarized in Table 1. No significant differences were found in age, gender, baseline BCVA, baseline retinal sensitivity, duration of symptoms, foveal thickness at baseline, choroidal thickness at baseline, size of the choroidal vein at baseline, and PDT spot size between the two treatment groups. The representative cases of the 1/2 and 1/3 PDT groups are shown in Figures 1 and 2, respectively.
Images of a 49-year-old man with chronic central serous chorioretinopathy treated with half-dose verteporfin photodynamic therapy (PDT). Blurred vision of 30 months duration was noted in his left eye. The best-corrected visual acuity measured by Early Treatment of Diabetic Retinopathy Study charts was 52 letters before PDT, which increased to 62 letters at 3 months after PDT. Spectral-domain optical coherence tomography images before (a) and 3 months after PDT (b). Red double arrows indicate the vertical and horizontal diameters of the subfoveal choroidal vein. White arrowheads indicate the inner sclera border. Subretinal fluid was completely resolved, and the subfoveal choroidal thickness reduced from 398 to 352 μm after PDT. Reduction in the vertical diameter and no change in the horizontal diameter were seen after PDT. Early-phase fluorescein angiogram before PDT (c) showed focal leakages from the retinal pigment epithelium at the macula. Middle-phase indocyanine green angiogram before PDT (d) showed hyperfluorescence secondary to vascular hyperpermeability at the macula. The white dashed circle indicates the PDT spot area of 4000 μm diameter. Results of microperimeter-1 before (e) and 3 months after PDT (f). The mean retinal sensitivity of the central 15° around the macula increased from 9.2 to 16.0 dB after PDT.
Images of a 49-year-old man with chronic central serous chorioretinopathy treated with one-third-dose verteporfin photodynamic therapy (PDT). He complained of image distortion of 12 months duration in his right eye. The best-corrected visual acuity measured by Early Treatment of Diabetic Retinopathy Study charts was 80 letters before PDT and 79 letters at 3 months after PDT. Spectral-domain optical coherence tomography images before (a) and 3 months after PDT (b). Red double arrows indicate the vertical and horizontal diameters of the subfoveal choroidal vein. White arrowheads indicate the inner sclera border. Subretinal fluid persisted, and there was no change in the subfoveal choroidal thickness (303 μm) after PDT. Neither the vertical nor the horizontal diameter changed significantly after PDT. Early-phase fluorescein angiogram before PDT (c) showed focal leakages from the retinal pigment epithelium at the macula. Middle-phase indocyanine green angiogram before PDT (d) showed hyperfluorescence secondary to vascular hyperpermeability at the macula. The white dashed circle indicates the PDT spot area of 2600 μm diameter. Results of microperimeter-1 before (e) and 3 months after PDT (f). The mean retinal sensitivities of the central 15° around the macula were 17.0 dB before PDT and 17.7 dB after PDT.
Disappearance rate of SRF
At 1 month, 7 eyes (70%) in the 1/2 PDT group had complete resolution of SRF compared with 2 eyes (33%) in the 1/3 PDT group. At 3 months, all 10 eyes (100%) in the 1/2 PDT group had complete resolution of SRF, and the same 2 eyes (33%) in the 1/3 PDT group maintained the complete resolution. The SRF disappearance rate of the 1/2 PDT group was significantly greater than that of the 1/3 PDT group at 3 months (P=0.008).
Changes in visual acuity
In the 1/2 PDT group, significant improvement was seen at 3 months compared with the baseline (P=0.007). In the 1/3 PDT group, no significant improvement from the baseline was seen at any visit after PDT. No significant difference in gained ETDRS was found between the two groups at any visit after PDT (Table 2).
Changes in central retinal sensitivity
In the 1/2 PDT group, significant improvements were seen at 1 month and 3 months compared with the baseline (both, P=0.005). In the 1/3 PDT group, no significant improvement from the baseline was seen at any visit after PDT. At 1 month and 3 months, gained retinal sensitivities of the 1/2 PDT group were significantly greater than those of the 1/3 PDT group (Table 2).
Changes in choroidal thickness inside the PDT-applied area
In the 1/2 PDT group, significant reductions were seen at 1 month and 3 months compared with the baseline (both, P=0.005). In the 1/3 PDT group, there was no significant change from the baseline at any visit after PDT. At 1 month and 3 months, the reduction rates of the 1/2 PDT group were significantly greater than those of the 1/3 PDT group (Table 2). Within the 1/3 PDT group, choroidal thickness inside the PDT-applied area decreased in two eyes where SRF disappeared (87.2 and 90.9% of the baseline at 3 months), but did not decrease in the other four eyes where SRF remained (104.1, 100.0, 105.1, and 100.5% of the baseline at 3 months).
Changes in choroidal thickness outside the PDT-applied area
In the 1/2 PDT group, significant reductions were seen at 1 month and 3 months compared with the baseline (both, P=0.005). In the 1/3 PDT group, there was no significant change from the baseline at any visit after PDT. At 1 month and 3 months, the reduction rates in the 1/2 PDT group were significantly greater than those of the 1/3 PDT group (Table 2). Within the 1/3 PDT group, choroidal thickness outside the PDT-applied area decreased in two eyes where SRF disappeared (91.4 and 92.6% of the baseline at 3 months), but did not decrease in the other four eyes where SRF remained (98.9, 103.0, 100.0, and 99.0% of the baseline at 3 months).
Changes in cross-sectional area of the large choroidal vein
Both inside and outside the PDT-applied area, the reduction rates of the 1/2 PDT group were significantly greater than those of the 1/3 PDT group at all visits after PDT (Table 2).
Changes in the diameters of the large choroidal vein in the 1/2 PDT group
Both inside and outside the PDT-applied area, the reduction rates of the vertical diameter were significantly greater than those of the horizontal diameter at all visits after PDT (Table 3).
Safety
None of the patients developed any systemic adverse event associated with verteporfin infusion. No ocular side effects, including development of CNV, were seen in any cases throughout the follow-up period.
Discussion
As CSC is a benign disorder and patients usually have a good baseline visual function, it is important to seek the best PDT protocol in order to obtain the maximum effect and the minimum complications. Half-dose PDT has been conducted to chronic CSC with relative safety,16, 17, 18, 19 but treatment with verteporfin at less than 50% of the conventional dosage has not been attempted for chronic CSC. Previous studies have shown that cytotoxicity and vascular damage associated with PDT are dose dependent.25, 26 In this prospective clinical trial, we compared the efficacy and safety of 1/2 PDT with those of 1/3 PDT for chronic CSC.
Zhao et al20 conducted PDT with verteporfin at 30% of the conventional dosage in 8 eyes with acute CSC, and all eyes (100%) had resolution of SRF. In this study, one-third dose was effective in only 2 out of 6 eyes (33%) with chronic CSC. In eyes with CSC, SRF accumulates when the exudation of serous fluid from choroidal vessels exceeds the barrier and the pump functions of RPE.27 Because retinal atrophy occurs in chronic stage of CSC,28 the barrier and the pump functions of RPE may be weaker and SRF may accumulate with less exudation in chronic CSC compared with acute CSC. Stronger suppression of the exudation from the choroid may be necessary for the resolution of SRF in chronic CSC than in acute CSC.
The mechanism of the action of PDT in CSC has not been fully understood, but the changes in choroidal structures after PDT in this study provide a useful clue. Choroidal thickness and the cross-sectional area of the large choroidal vein significantly decreased after PDT in the 1/2 PDT group, but did not change in the 1/3 PDT group. The SRF disappearance rate was greater in the 1/2 PDT group than in the 1/3 PDT group. Within the 1/3 PDT group, choroidal thickness decreased in two eyes where SRF disappeared, but did not change in the other four eyes where SRF remained. Considering these facts, the thinning of the choroid and the reduction of the size of the choroidal vein may be related to the resolution of SRF. To the best of our knowledge, this is the first study reporting the unchanged choroidal thickness after ineffective PDT.
In chronic CSC, the speed of the SRF resolution after PDT is relatively fast. SRF disappeared in 1 month in all successful cases in this study. There are two reports19, 24 that compared the efficacy of half-dose PDT with LP in treating chronic CSC. Both studies reported that SRF disappeared in all eyes in both the PDT group and the LP group. But faster SRF resolution was observed in the PDT group compared with the LP group. In the study of Lim et al,19 1 out of 14 eyes (7%) in the PDT group and 5 out of 12 eyes (42%) in the LP group had residual SRF at 1 month after PDT. In the study of Maruko et al,24 2 out of 8 eyes (25%) in the PDT group and 9 out of 12 eyes (75%) in the LP group had residual SRF at 1 month after PDT. Maruko et al24 also reported that choroidal thickness decreased after half-dose PDT, but did not change after LP. Faster resolution of SRF after half-dose PDT may be related to the thinning of the choroid.
Pryds and Larsen29 reported that the reduction of choroidal thickness occurred not only inside the PDT-applied area but also outside the PDT-applied area after a half-light dose PDT for chronic CSC. In this study, choroidal thickness and the cross-sectional area of the large choroidal vein significantly decreased both inside and outside the PDT-applied area after 1/2 PDT. These findings suggest that the PDT affects the choroid not only inside but also outside the PDT-applied area. We speculated that PDT first decreases the size of the large choroidal veins and choroidal blood flow in the PDT-applied area. As the choroidal vascular system is an anastomosing network, the influence of the reduction of choroidal blood flow spreads through the posterior pole and the decrease in the size of the large choroidal veins occurs outside the PDT-applied area secondarily.
In this study, the reduction rate of the vertical diameter of the large choroidal veins was greater than that of the horizontal diameter in the 1/2 PDT group. Our previous study has demonstrated that a significant correlation exists between choroidal thickness and the ratio of vertical/horizontal diameter of the large choroidal veins in normal eyes.30 The higher mobility of the vertical diameter compared with that of the horizontal diameter may be the characteristic of the large choroidal veins. Observing the change in the shapes of the choroidal veins may provide a clue on the integrity of the choroidal circulation.
This study has several limitations, including small sample size and short-term follow-up period. Patients were consecutive and were not matched for the degree of hyperpermeability on ICGA. A randomized clinical trial with larger sample size and longer follow-up period is necessary to draw definitive conclusions.
To determine the optimal dose of verteporfin for chronic CSC, another dosage, such as between 2 and 3 mg/m2, needs to be evaluated. In addition, there are many parameters of PDT besides dosage, such as light energy, time interval between injection and irradiation, duration of photosensitization, and PDT spot size. We need to conduct a head-to-head comparison of each parameter of PDT to decide the optimal protocol of PDT for chronic CSC.

References
Gass JD . Pathogenesis of disciform detachment of the neuroepithelium. Am J Ophthalmol 1967; 63: 587–615.
Yannuzzi LA . Type-A behavior and central serous chorioretinopathy. Retina 1987; 7: 111–131.
Gilbert CM, Owens SL, Smith PD, Fine SL . Long-term follow-up of central serous chorioretinopathy. Br J Ophthalmol 1984; 68: 815–820.
Brancato R, Scialdone A, Pece A, Coscas G, Binaghi M . Eight-year follow-up of central serous chorioretinopathy with and without laser treatment. Graefes Arch Clin Exp Ophthalmol 1987; 225: 166–168.
Ficker L, Vafidis G, While A, Leaver P . Long-term follow-up of a prospective trial of argon laser photocoagulation in the treatment of central serous retinopathy. Br J Ophthalmol 1988; 72: 829–834.
Leaver P, Williams C . Argon laser photocoagulation in the treatment of central serous retinopathy. Br J Ophthalmol 1979; 63: 674–677.
Robertson DM, Ilstrup D . Direct, indirect, and sham laser photocoagulation in the management of central serous chorioretinopathy. Am J Ophthalmol 1983; 95: 457–466.
Chen SN, Hwang JF, Tseng LF, Lin CJ . Subthreshold diode micropulse photocoagulation for the treatment of chronic central serous chorioretinopathy with juxtafoveal leakage. Ophthalmology 2008; 115: 2229–2234.
Yannuzzi LA, Slakter JS, Gross NE, Spaide RF, Costa DL, Huang SJ et al. Indocyanine green angiography-guided photodynamic therapy for treatment of chronic central serous chorioretinopathy: a pilot study. Retina 2003; 23: 288–298.
Cardillo Piccolino F, Eandi CM, Ventre L, Rigault de la Longrais RC, Grignolo FM . Photodynamic therapy for chronic central serous chorioretinopathy. Retina 2003; 23: 752–763.
Shanmugam PM, Agarwal M . Indocyanine green angiography-guided photodynamic therapy for treatment of chronic central serous chorioretinopathy: a pilot study. Retina 2004; 24: 988–989.
Taban M, Boyer DS, Thomas EL, Taban M . Chronic central serous chorioretinopathy: photodynamic therapy. Am J Ophthalmol 2004; 137: 1073–1080.
Colucciello M . Choroidal neovascularization complicating photodynamic therapy for central serous retinopathy. Retina 2006; 26: 239–242.
Chan WM, Lam DS, Lai TY, Tam BS, Liu DT, Chan CK . Choroidal vascular remodeling in central serous chorioretinopathy after indocyanine green guided photodynamic therapy with verteporfin: a novel treatment at the primary disease level. Br J Ophthalmol 2003; 87: 1453–1458.
Colucciello M . Choroidal neovascularization complicating photodynamic therapy for central serous retinopathy. Retina 2006; 26: 239–242.
Chan WM, Lai TY, Lai RY, Tang EW, Liu DT, Lam DS . Safety enhanced photodynamic therapy for chronic central serous chorioretinopathy: one-year results of a prospective study. Retina 2008; 28: 85–93.
Senturk F, Karacorlu M, Ozdemir H, Karacorlu SA, Uysal O . Microperimetric changes after photodynamic therapy for central serous chorioretinopathy. Am J Ophthalmol 2011; 151: 303–309.
Fujita K, Yuzawa M, Mori R . Retinal sensitivity after photodynamic therapy with half-dose verteporfin for chronic central serous chorioretinopathy: short-term results. Retina 2010; 30: 772–778.
Lim JW, Kang SW, Kim YT, Chung SE, Lee SW . Comparative study of patients with central serous chorioretinopathy undergoing focal laser photocoagulation or photodynamic therapy. Br J Ophthalmol 2011; 95: 514–517.
Zhao MW, Zhou P, Xiao HX, Lv YS, Li CA, Liu GD et al. Photodynamic therapy for acute central serous chorioretinopathy: the safe effective lowest dose of verteporfin. Retina 2009; 29: 1155–1161.
Treatment of age-related macular degeneration with photodynamic therapy (TAP) study group Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin. One-year results of 2 randomized clinical trials--TAP repotr. Arch Ophthalmol 1999; 117: 1329–1345.
Spaide RF, Koizumi H, Pozzoni MC . Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol 2008; 146: 496–500.
Imamura Y, Fujiwara T, Margolis R, Spaide RF . Enhanced depth imaging optical coherence tomography of the choroid in central serous chorioretinopathy. Retina 2009; 29: 1469–1473.
Maruko I, Iida T, Sugano Y, Ojima A, Ogasawara M, Spaide RF . Subfoveal choroidal thickness after treatment of central serous chorioretinopathy. Ophthalmology 2010; 117: 1792–1799.
Schmidt-Erfurth U, Michels S, Barbazetto I, Laqua H . Photodynamic effects on choroidal neovascularization and physiological choroid. Invest Ophthalmol Vis Sci 2002; 43: 830–841.
Schlötzer-Schrehardt U, Viestenz A, Naumann GO, Laqua H, Michels S, Schmidt-Erfurth U . Dose-related structural effects of photodynamic therapy on choroidal and retinal structures of human eyes. Graefes Arch Clin Exp Ophthalmol 2002; 240: 748–757.
Eandi CM, Ober M, Iranmanesh R, Peiretti E, Yannuzzi LA . Acute central serous chorioretinopathy and fundus autofluorescence. Retina 2005; 25: 989–993.
Wang MS, Sander B, Larsen M . Retinal atrophy in idiopathic central serous chorioretinopathy. Am J Ophthalmol 2002; 133: 787–793.
Pryds A, Larsen M . Choroidal thickness following extrafoveal photodynamic treatment with verteporfin in patients with central serous chorioretinopathy. Acta Ophthalmol 2011 e-pub ahead of print 17 May 2011; doi: 10.1111/j.1755-3768.2011.02157.x.
Tanabe H, Ito Y, Iguchi Y, Ozawa S, Ishikawa K, Terasaki H . Correlation between cross-sectional shape of choroidal veins and choroidal thickness. Jpn J Ophthalmol 2011; 55: 614–619.
Acknowledgements
This work was supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (Dr Ito, C2159225).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Uetani, R., Ito, Y., Oiwa, K. et al. Half-dose vs one-third-dose photodynamic therapy for chronic central serous chorioretinopathy. Eye 26, 640–649 (2012). https://doi.org/10.1038/eye.2012.66
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.66
Keywords
This article is cited by
-
Central serous chorioretinopathy: updates in the pathogenesis, diagnosis and therapeutic strategies
Eye and Vision (2023)
-
Choroidal hemodynamics in central serous chorioretinopathy after half-dose photodynamic therapy and the effects of smoking
Scientific Reports (2022)
-
Decrease in choroidal blood flow after half and one-third dose verteporfin photodynamic therapy for chronic central serous chorioretinopathy
BMC Ophthalmology (2021)
-
One-year results of half-dose versus one-third-dose photodynamic therapy in chronic or recurrent central serous chorioretinopathy
BMC Ophthalmology (2021)
-
Optical Coherence Tomography Angiography for Diagnosis of Choroidal Neovascularization in Chronic Central Serous Chorioretinopathy after Photodynamic Therapy
Scientific Reports (2019)