Abstract
Purpose
To report clinical observations and surgical management in a large series of patients with orbitofacial neurofibromatosis type 1 (OFNF).
Patients and methods
Patients were identified and medical records reviewed for demographic data, ophthalmologic examinations, surgical interventions, and procedure outcome to create a retrospective, non-comparative case series of patients with OFNF seen at one medical centre over a 23-year period.
Results
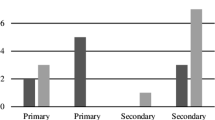
Sixty patients with OFNF (31 females and 29 males; mean age, 14 years) were followed for an average of 5.7 years. Presenting signs and symptoms included eyelid swelling in all patients, ptosis in 56 (93.3%), proptosis in 34 (56.6%), dystopia or strabismus in 30 (50%), and decreased visual acuity in 50 (83.3%). Surgical intervention included ptosis repair in 54 (90%; mean 1.6 surgical procedures), facial and orbital tumour debulking in 54 (90%; mean 2.3 surgeries), and canthoplasty in 28 (46.6%) patients. Eleven patients required enucleation or exenteration of a blind eye.
Conclusion
Patients with OFNF often require multiple procedures to preserve vision, prevent additional disfigurement, and achieve cosmetic rehabilitation. Patients need regular ophthalmological monitoring given the potential for progressive visual and cosmetic consequences.
Similar content being viewed by others
Introduction
Neurofibromatosis type 1 (NF1; von Recklinghausen disease; OMIM 162200) is a fairly frequent (1 in 3000 live births), autosomal dominant, neurocutaneous disorder that has considerable clinical variability and the potential for multisystem involvement.1 Although most commonly benign, neurofibromas (NFs) have the potential of malignant transformation2 and can have devastating functional and cosmetic effects. In orbitofacial NF1 (OFNF), which occurs in 1–22% of patients, NFs may cause progressive, disfiguring tumours of the orbital, facial, and temporal areas.3, 4 In this study, we review the experience with surgical management of OFNF in patients seen at the King Khaled Eye Specialist Hospital (KKESH), a tertiary eye care referral centre in Riyadh, Saudi Arabia, and the largest eye facility in the Middle East.
Patients and methods
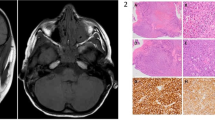
Patients with OFNF treated at KKESH over a 23-year period were identified and their medical records reviewed to catalogue demographic information, presenting signs and symptoms, ophthalmologic examination data, diagnostic studies performed, and surgical interventions rendered. All patients had NF1 on the basis of clinical criteria established by the National Institute of Health,5, 6 and the diagnosis of OFNF was confirmed histologically in all surgical cases.1, 3 Pathological specimens ranged from small tissue biopsy sample obtained at the time of ptosis correction to bulky tumours up to 25 cm in aggregate.
Visual acuity (VA) was recorded for each eye at least at the time of diagnosis and at the last eye examination. Involvement of eyelid, brow, face, and orbit was categorized. The preoperative and postoperative photographs were compared when possible, functional and aesthetic outcome of surgery and complications of the procedures were assessed, and subsequent progression of deformity (if any) was documented. High-resolution head computed tomography (CT) with 1–3 mm image thickness and 3-Tesla magnetic resonance imaging (MRI) were performed to assist in assessing extent of NF-related disease and deformity.
We certify that all applicable institutional and governmental regulations regarding the ethical use of human volunteers were followed during this research.
Results
A total of 60 patients with OFNF (31 females and 29 males; mean age 14 years; range 2 months to 45 years) were treated over a 23-year period. Average follow-up duration was 5.7 years (range 1 month to 23 years). All patients had unilateral orbitofacial involvement (Figure 1) except for one patient that had bilateral OFNF (Figure 2). Computed tomography of the head was performed in 54 patients and MRI was performed in 26 patients.
(a) A 10-year-old boy with left-sided OFNF causing left upper eyelid fullness, ptosis, and facial asymmetry. (b) Axial head CT image of the same patient showing secondary sphenoid wing and orbital dysplasia on the left with larger globe on the left (without glaucoma) and NF infiltration of the orbit, temporal region, and lacrimal gland.
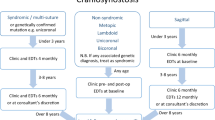
Signs and symptoms at initial exam are summarized in Table 1. Upper eyelid swelling or fullness was present in all patients, and ptosis of the upper eyelid secondary to diffuse infiltration or nodular NF (Figure 3) occurred in 56 patients (93.3%). The lateral canthus was detached in 36 patients (60%; Figure 4). Bony dysplasia of the skull or orbit was documented in 54 patients (90%; Figure 1), with proptosis present in 34 (56.6%) and globe dystopia in 30 (50%). Optic pathway gliomas (OPGs) were found in nine patients (15%) and were bilateral in three patients (Figure 5).
(a) External photograph of a 3-year-old child with OFNF who presented with swelling and fullness of his right upper eyelid due to infiltration by a plexiform NF. Clinical examination revealed multiple café au lait spots over other parts of his body. (b) Father of child in (a) with multiple facial NFs.
(a) A 4-year-old boy presented with left upper eyelid ptosis with an s-shaped contour caused by plexiform NF infiltration associated with NF1. (b) The patient in (a) at age 12 years. (c) The patient in (a) at age 15 years. He had rapid progression of OFNF over his teenage years despite several surgical corrections of ptosis and tumour debulking.
(a) A 2-year-old girl presented with decreased bilateral vision, proptosis, and orbital dystopia. (b) Axial MRI image of patient in (a) showed bilateral ON gliomas with remodelling of the left orbit. (c) Post-operative external photograph of the patient in (a) after placement of a cosmetic prosthetic shell in the left anophthalmic socket. (d) Globe and a very thick segment of optic nerve glioma after left-sided enucleation and tumour resection on patient in (a).
The primary surgical procedures performed included correction of ptosis, debulking of tumour, and reattachment of the canthal tendon. Additional procedures included correction of entropion or ectropion caused either by the disease process or by the complications of earlier surgical procedures. Entropion was corrected by tumour debulking if caused by the tumour or by reattachment of the lower eyelid retractors if it was due to postoperative complications. Lower eyelid-shortening procedures in the form of pentagonal wedge resection, tarsal strip, or periosteal flap canthoplasty were performed to address lower eyelid ectropion, lateral canthal displacement, a wide palpebral aperture, and malposition of the eyelid.
Lateral canthoplasty was usually performed by attaching the lower eyelid tarsus to the inner periosteum of the supra-lateral orbital rim area. Transnasal medial canthopexy was undertaken in cases of medial canthal complex displacement. As floppy eyelids may also result in secondary ectropion because of marked laxity of both limbs of the medial and lateral canthal tendons, in these cases, the lids were shortened with full-thickness pentagonal resections and sutured to the periosteum. Additional laxity was treated by medial canthal repositioning, lateral periosteal flap, and upper lid bipedicle flap. In most cases, surgery was tailored to the patient's symptoms and progression of the disease. In cases of lateral canthal distension, canthal reattachment was achieved with nonabsorbable sutures. Brow slings (fascia lata, gortex, or silicon rods) were used to elevate eyelids when levator aponeurosis function was poor or heavily infiltrated by tumour. Fascia lata sling was used in some patients to reattach the lower lid tendon to the drilled orbital rim.
Table 2 details the type and number of surgical procedures performed. Ptosis surgery was the most common procedure (Figure 6) with patients commonly requiring multiple surgeries. Tumour debulking was carried out in 54 patients at some point during their course (Figure 7), but complete excision was never possible due to the extent of lesion and infiltration into the surrounding soft tissue and vital structures (Figure 8). In approximately half of the cases, canthoplasty was necessary to reattach the lateral canthal tendon. Correction of upper and lower eyelid entropion or ectropion was performed less commonly. Patients with primary lower lid mechanical ectropion due to tumour were successfully treated by horizontal pentagonal lid resection.
(a) This 6-year-old boy had left upper eyelid fullness and ptosis due to plexiform NF. Previous frontalis suspension surgery had failed. (b) Coronal orbital CT images of patient in (a) revealed soft tissue infiltration of left superior orbit and enlargement of orbital cavity. (c) Patient in (a) with satisfactory cosmesis after debulking of orbital tumour along with correction of left upper eyelid ptosis.
(a) This 18-year-old girl had right-sided OFNF with tumour involvement of right forehead, brow, and lid. She underwent multiple resections of her tumours in an effort to obtain acceptable cosmesis. She was, nevertheless, severely amblyopic in the occluded right eye. (b) Same patient as (a) after most recent surgical resection of her forehead, eye brow and eyelid tumour.
Table 3 details the clinical and surgical course of 11 patients who underwent removal of the globe on the affected side, most commonly because of congenital glaucoma and/or proptosis of a blind eye. NF involvement was typically marked in the orbit and face ipsilateral to the removed globe, but tumour mass itself was not the reason for enucleation or evisceration. None of the patients in this series underwent globe removal because of corneal exposure or surgical complications.
Surgical complications included incompletely corrected ptosis (Figures 7 and 8), ptosis overcorrection, irregular lid contour (Figure 7), dry eye, and corneal exposure (Figure 8). Some patients also developed upper or lower lid entropion or ectropion after tumour resection; for example, three patients had lower eyelid ectropion after tumour debulking surgery (Figure 4). Five patients required removal or revision of frontalis slings due to exposure keratopathy, cosmetically unacceptable lagophthalmos, or infection. None of the patients in this series developed hypertrophic scars or keloid formation, but tumour recurrence commonly appeared at the margins of the previous resection site.
Discussion
This series of 60 patients with OFNF manifesting as NF infiltration of the orbit, eyelid and periocular region causing ptosis, proptosis, detached lateral canthus, and disfiguring facial masses is one of the largest series that have been reported in the literature. There is no indication of an increased frequency of OFNF in the Arabs; however, KKESH is the only major tertiary eye facility in the Middle East, and this is likely responsible for the large patient number, the persistent follow-up of OFNF patients, and a selection bias, with this facility caring for more difficult and more advanced cases of OFNF than is typical. These patients were not treated according to a single protocol; rather, they were cared for by a series of physicians over a period of time, often in different subspecialty clinics.
The referral pattern of patients in this series was different from that of OFNF studies emerging from the NF clinics,1 or the National Neurofibromatosis Foundation International Database.7 OFNF patients are often managed by either plastic surgery services or oculoplastic surgeons,8, 9 but recently Lee et al10, 11 described their experience with 42 OFNF patients over a 20-year period at the Moorfields Eye Hospital, London. Their study is the most similar to the current observations; nevertheless, it is possible that some of the results reported here can be generalized only with caution to other centres.
As detailed in Table 1, OFNF has a predilection for the brow and/or upper lid, lateral eyelid being affected more than medial, leading to the classic s-shaped lid deformity; Figures 4a and 6a), although at times the orbit (Figures 1b and 6b), the anterior globe, and other facial areas (Figures 1 and 4) are involved instead of, or in addition to, the lid.4, 10 Only one side of the face was generally affected for reasons that are currently unclear. The most common exception to this rule was OPG (Figure 5), which are often bilateral in NF1 and which in general are not associated with other manifestations of OFNF.12, 13, 14 Unfortunately, tumour progression is the hallmark of this disease in childhood, often leading to increasing tumour mass, progressive disfigurement, and decreased vision (Figure 4).3 In general, the diagnosis of OFNF was not a major problem; the potential benefits and risks of surgical treatment were the primary concern of families and physicians.
CT and MRI were invaluable for assessment and follow-up of OFNF changes. NFs of the face, temple, and orbit were generally not encapsulated but rather infiltrated into nearby normal tissue. NFs in this region also interacted with the contiguous bone and globe, changing the shape of the developing skull (secondary sphenoid dysplasia)15 and orbit16 and enlarging the ipsilateral globe (Figure 1).17 These progressive changes are not clearly correlated with tumour volume and are currently not treatable even though they can have substantial visual and cosmetic implications. CT scans helped delineate tumour extent and bony involvement, although soft-tissue characterization was limited, whereas MRI provided superior soft-tissue characterization and relative demarcation of tumours from normal tissue.16 NFs generally appeared hypointense on CT and T1-weighted MRI images and enhanced with contrast.15, 16 Neuroimaging was essential to identify intracranial extension of NFs from the orbit into the cavernous sinus, as intracranial involvement was routinely not marked by either motility abnormalities or signs of orbital venous congestion (Figure 1).16 Finally, high-resolution neuroimaging of the optic nerves and chiasm is the most reliable way to make the diagnosis of OPG.18, 19
Similarly to previous studies,10 the most common surgical procedures performed in our series were related to ptosis and lid involvement. The primary indications for lid surgery in OFNF were functional, with the goal of uncovering an obscured visual axis to prevent amblyopia in visually immature children (Figures 1 and 3). Debulking of an eyelid tumour was also at times necessary for cosmetic reasons or to prevent anisometropia due to the mechanical effect of an overlying thick eyelid. Although some patients benefited from external levator resection, the majority needed selective debulking surgery because of extensive tissue NF infiltration in lid, brow, and/or orbit. In general, pentagonal excision was used to remove nodular NFs causing mechanical ptosis in the upper lid or ectropion in the lower lid, although some patients developed conjunctival prolapse after large levator resections. Large tumours of the upper and lower eyelid sometimes caused lengthening of the lids by traction on the lateral canthal tendon (Figure 4). In other instances, tumour infiltration weakened those tendons. Canthoplasty in these patients helped to reduce the length of the eyelids and provided strength to hold the lids at a proper height against the globe. Non-absorbable sutures or fascia lata sling were used to attach the lateral canthal tendon to the lateral orbital rim area.
Repeat eyelid surgery was sometimes necessary due to regrowth of the eyelid tumour, again causing mechanical ptosis. Sometimes, disinsertion of the levator aponeurosis caused ptosis after debulking of the tumour, and levator advancement was necessary. In other cases of aggressive tumour debulking, lid retraction needed to be treated by recession to prevent exposure keratopathy. The number of surgeries required for ptosis correction ranged from one to six (mean 1.6) and one to nine for tumour debulking from the periocular areas (mean 2.3). Some patients had complete ptosis that required multiple eyelid operations. Most surgeons recommend that surgery to repair occlusive ptosis be contemplated at an early age to preserve visual function and to avoid facial deformity. In contrast to the report by Lee et al,10 in which all patients achieved satisfactory elevation of the upper eyelid above the visual axis, surgical results in the current patient series were not particularly rewarding in younger patients who required multiple surgeries.
These patients also required surgery for debulking tumour involving the brow, cheek, or temporal region (Figures 4 and 8). Treatment of these facial tumours was challenging due to the risks of bleeding, facial nerve damage, and exposure keratopathy.20, 21 Complete excision of NFs was not practical in any patient due to extensive, diffuse soft-tissue infiltration and lack of encapsulation. Large forehead tumours (Figure 7) often resulted in excessive brow ptosis and secondary eyelid ptosis and therefore required debulking for functional as well as cosmetic reasons. Large upper cheek tumours sometimes caused lower eyelid retraction, ectropion, and lagophthalmos resulting in exposure keratopathy (Figure 4). Three patients in our study had lower eyelid entropion with medial trichiasis due to enlarging NF of the cheek that required local excision. Similar observations were made by Lee et al,11 where four of the nine children had significant cheek involvement in addition to the involvement of the eyelid, brow, and orbits. In general, large tumours of the forehead, cheek, or temple area required debulking because they were cosmetically disfiguring. Large unilateral facial tumours sometimes caused a head tilt towards the side of the tumour, and surgery was necessary because of neck posture as well as cosmesis.
Repeat debulking procedures were necessary in the setting of tumour progression, which often occurred at the margin of a previous resection. Our results support previous observations that disease recurrence and functional and aesthetic relapse should be expected, but the interim satisfaction of the visually and socially rehabilitated patient is a worthwhile objective.10, 11, 20, 21, 22 Rapid recurrence of the disease seemed more evident in younger children with conservative eyelid resection. We suggest that surgery for paediatric OFNF be considered at an early age only to preserve visual function and to deal with socially stigmatizing facial deformity. Otherwise, we agree with others10 that surgery should be delayed until adulthood, when the disease is generally more stable.
Most of our patients had unilateral disease; however one patient had severe, bilateral OFNF (Figure 2).10, 16 This patient required multiple intraocular, eyelid, brow, forehead, and cheek debulking and reconstructive surgeries, but the results obtained were not satisfactory, both because of rapidly progressive facial NF and because of eventual blindness OU due to total retinal detachments precipitated at least in part by severe buphthalmos subsequent to congenital glaucoma. This patient vividly illustrated the potential tragic implications of this disease.
Proptosis was often severe, caused by ipsilateral globe enlargement,23 orbital and sphenoid dysplasia (Figure 1),15, 16 and/or OPG (Figure 5). Orbital involvement by NF was frequent but generally was not treated as an independent entity because orbital NFs by themselves did not typically cause optic nerve compression, significant proptosis, or major ocular motility abnormalities. OPGs are the most common CNS tumours in patients with NF1, generally heralded by decreased VA and/or optic atrophy. Fifteen percent occurrence in our series is in agreement with the range of 1.5–24% in other series of OPGs,24, 25 implying that OPG is no more common in OFNF than in NF1, with predominant manifestation outside the head and face. Similar to previous reports,12, 18, 19 most of our patients with OPG presented with decreased VA and/or proptosis, and neuroimaging generally revealed thickening and/or tortuosity of the optic nerve or chiasm. Biopsy was not undertaken, as the diagnosis of OPG was made by neuroimaging. In our study, only those children who had documented progression of symptoms were treated, and enucleation or surgical excision of the orbital component of an OPG were contemplated only for cosmetic purposes or to remove an exposed, blind eye (Figure 5).
Table 3 details the clinical and surgical course of the 11 patients in this series who required removal of the globe. These patients generally had extensive ipsilateral orbital and facial tumour, but in none of the patients, the tumour bulk was directly related to the removal of the globe. Almost all had a blind, cosmetically disfigured eye because of glaucoma, OPG, or both, and enucleation, evisceration, or exenteration was performed because of severe proptosis or phthisis bulbi. These patients also generally underwent multiple facial tumour debulking surgeries, but the relative success of these surgeries did not directly impact the decision to eventually remove the globe.
We do not recommend routine enucleation or evisceration of all blind eyes because a cosmetic shell can be worn with improved cosmesis. Elective enucleation, evisceration, or exenteration of a blind, cosmetically disfigured eye was undertaken only to provide enough room to allow a prosthetic shell for a buphthalmic eye or as part of the debulking process in the setting of a severely proptotic globe due to skull and orbital dysplasia and orbital tumour mass. Subtotal anterior exenteration was necessary in some patients with a blind, buphthalmic globe and massive orbital and/or eyelid plexiform NFs. Other centres agree with this approach. Madil et al26 reported a 12-year-old girl whose cosmesis and social interaction were improved markedly after a subtotal exenteration of a buphthalmic globe along with the removal of large, disfiguring eyelid and orbital plexiform NF. Abouchadi et al24 recently reported their experience with six OFNF patients associated with severe spheno-orbital dysplasia, fronto-temporal meningoencephalocele causing pulsatile exophthalmos, and a non-functional eye. Exenteration was performed in all six along with reconstruction of the greater wing of the sphenoid using iliac bone graft and a titanium plate.
The main objectives of oculoplastic management in these patients were to preserve vision and improve appearance. Similar to others,10, 11, 20, 21, 22, 27 we recommend a step-wise approach based on the need for visual rehabilitation in children and functional and cosmetic concerns in adults. Because of the more static nature of the tumour in adults, an aggressive surgical approach can be undertaken in hope of achieving a permanent and definitive result.10 Preservation of a non-functional globe is appropriate except in severe OFNF that causes significant deformity and requires radical resection that may include enucleation or exenteration.

References
Riccardi VM . Neurofibromatosis: phenotype, natural history and pathogenesis. Johns Hopkins University Press: Baltimore, 1992.
Wong WW, Hirose T, Scheithauer BW, Schild SE, Gunderson LL . Malignant peripheral nerve sheath tumor: analysis of treatment outcome. Int J Radiat Oncol Biol Phys 1998; 42 (2): 351–360.
North K . Neurofibromatosis Type 1 in Childhood. MacKeith Press: London, 1997.
Erb MH, Uzcategui N, See RF, Burnstine MA . Orbitotemporal neurofibromatosis: classification and treatment. Orbit 2007; 26 (4): 223–228.
National Institutes of Health Consensus Development Conference Statement: neurofibromatosis. Neurofibromatosis, July 13–15 1987, Bethesda, USA 1988; 1 (3): 172–178.
Mulvihill JJ, Parry DM, Sherman JL, Pikus A, Kaiser-Kupfer MI, Eldridge R . NIH conference. Neurofibromatosis 1 (Recklinghausen disease) and neurofibromatosis 2 (bilateral acoustic neurofibromatosis). Ann Intern Med 1990; 113 (1): 39–52.
Friedman JM, Birch P, Greene C . National Neurofibromatosis Foundation International Database. Am J Med Genet 1993; 45 (1): 88–91.
Dutton JJ, Tawfik HA, DeBacker CM, Lipham WJ, Gayre GS, Klintworth GK . Multiple recurrences in malignant peripheral nerve sheath tumor of the orbit: a case report and a review of the literature. Ophthal Plast Reconstr Surg 2001; 17 (4): 293–299.
Fan XQ, Lin M, Li J, Zhou HF, Fu Y . [Removal and plastic reconstructive surgery of orbital neurofibroma]. Zhonghua Yi Xue Za Zhi 2007; 87 (46): 3264–3267.
Lee V, Ragge NK, Collin JR . Orbitotemporal neurofibromatosis. Clinical features and surgical management. Ophthalmology 2004; 111 (2): 382–388.
Lee V, Ragge NK, Collin JR . The surgical management of childhood orbito-temporal neurofibromatosis. Br J Plast Surg 2003; 56 (4): 380–387.
Listernick R, Louis DN, Packer RJ, Gutmann DH . Optic pathway gliomas in children with neurofibromatosis 1: consensus statement from the NF1 Optic Pathway Glioma Task Force. Ann Neurol 1997; 41 (2): 143–149.
Liu GT, Brodsky MC, Phillips PC, Belasco J, Janss A, Golden JC et al. Optic radiation involvement in optic pathway gliomas in neurofibromatosis. Am J Ophthalmol 2004; 137 (3): 407–414.
Seiff SR, Brodsky MC, MacDonald G, Berg BO, Howes Jr EL, Hoyt WF . Orbital optic glioma in neurofibromatosis. Magnetic resonance diagnosis of perineural arachnoidal gliomatosis. Arch Ophthalmol 1987; 105 (12): 1689–1692.
Jacquemin C, Bosley TM, Liu D, Svedberg H, Buhaliqa A . Reassessment of sphenoid dysplasia associated with neurofibromatosis type 1. AJNR Am J Neuroradiol 2002; 23 (4): 644–648.
Jacquemin C, Bosley TM, Svedberg H . Orbit deformities in craniofacial neurofibromatosis type 1. AJNR Am J Neuroradiol 2003; 24 (8): 1678–1682.
Morales J, Chaudhry IA, Bosley TM . Glaucoma and globe enlargement associated with neurofibromatosis type 1. Ophthalmology 2009; 116 (9): 1725–1730.
Pilling RF, Taylor RH . Screening children with NF1 for optic pathway glioma – no. Eye (Lond) 2010; 24 (9): 1432–1434.
Simmons I, Gogi D . Screening children with NF1 for optic pathway glioma – yes. Eye (Lond) 2010; 24 (9): 1429–1431.
Jackson IT . Management of craniofacial neurofibromatosis. Facial Plast Surg Clin North Am 2001; 9 (1): 59–75, viii.
Jackson IT, Carbonnel A, Potparic Z, Shaw K . Orbitotemporal neurofibromatosis: classification and treatment. Plast Reconstr Surg 1993; 92 (1): 1–11.
Marchac D, Britto JA . Remodelling the upper eyelid in the management of orbitopalpebral neurofibromatosis. Br J Plast Surg 2005; 58 (7): 944–956.
Hoyt CS, Billson FA . Buphthalmos in neurofibromatosis: is it an expression of regional giantism? J Pediatr Ophthalmol 1977; 14 (4): 228–234.
Abouchadi A, Nassih M, Rzin A, Elgbouri H, Jidal B . [Orbito-temporal plexiform neurofibroma: 6 cases]. Rev Stomatol Chir Maxillofac 2005; 106 (5): 272–275.
Lewis RA, Gerson LP, Axelson KA, Riccardi VM, Whitford RP . von Recklinghausen neurofibromatosis. II. Incidence of optic gliomata. Ophthalmology 1984; 91 (8): 929–935.
Madill KE, Brammar R, Leatherbarrow B . A novel approach to the management of severe facial disfigurement in neurofibromatosis type 1. Ophthal Plast Reconstr Surg 2007; 23 (3): 227–228.
Boulanger JM, Larbrisseau A . Neurofibromatosis type 1 in a pediatric population: Ste-Justine's experience. Can J Neurol Sci 2005; 32 (2): 225–231.
Acknowledgements
No financial support from any source was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chaudhry, I., Morales, J., Shamsi, F. et al. Orbitofacial neurofibromatosis: clinical characteristics and treatment outcome. Eye 26, 583–592 (2012). https://doi.org/10.1038/eye.2011.336
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.336
Keywords
This article is cited by
-
Trametinib for orbital plexiform neurofibromas in young children with neurofibromatosis type 1
Child's Nervous System (2021)
-
Differential gene methylation and expression of HOX transcription factor family in orbitofacial neurofibroma
Acta Neuropathologica Communications (2020)
-
Surgical correction in orbitotemporal neurofibromatosis with dystopia
BMC Ophthalmology (2016)