Abstract
Purpose
The aim of this study was to investigate the incidence of intraocular pressure (IOP) elevation after resident-performed cataract surgery and to determine variables, which influence postoperative day 1 (POD1) IOP.
Methods
In all, 1111 consecutive cataract surgeries performed only by training residents between 1 July 2001 and 30 June 2006 were included. Elevated IOP was defined as ≥23 mm Hg. Surgeries were classified according to the presence of POD1-IOP elevation. Fisher's exact test and Student t-test were used to compare both groups. Multivariate analyses using generalized estimating equations were performed to investigate predictor variables associated with POD1-IOP elevation.
Results
The average preoperative IOP was 16.0±3.2 mm Hg and the average POD1-IOP was 19.3±7.1 mm Hg, reflecting a significant increase in IOP (P<0.001, paired t-test). The incidence of POD1-IOP elevation ≥23 mm Hg was 22.0% (244/1111). Presence of glaucoma and ocular hypertension, higher preoperative IOP, and longer axial length were frequently encountered variables in the POD1-IOP elevation group (all P<0.05). Using a multivariate analysis, presence of glaucoma (P=0.004, OR=2.38; 95% confidence interval (95% CI)=1.31–4.30), presence of ocular hypertension (P=0.003, OR=6.09; 95% CI=1.81–20.47), higher preoperative IOP (P<0.001, OR=3.73; 95% CI=1.92–7.25), and longer axial length (P=0.01, OR=1.15; 95% CI=1.03–1.29) were significant predictive factors for POD1-IOP elevation.
Conclusions
IOP elevation on the first postoperative day following resident-performed cataract surgery occurred frequently (22.0%). Increased early postoperative IOP was associated with presence of glaucoma and ocular hypertension, higher preoperative IOP, and longer axial length.
Similar content being viewed by others
Introduction
Early postoperative elevation in intraocular pressure (IOP) following cataract surgery is a frequently reported adverse event that surgeons must address. The incidence of early postoperative IOP increase is reported to be 2.3–8.9% in all cataract extractions.1, 2 This increase typically peaks at 3–7 h after surgery and persists during the first 24 h.3, 4, 5, 6 The extent of such an early IOP increase has been reported to be related to anterior chamber inflammation and prostaglandin release,5, 7 capsulorhexis size,8 type of surgical procedure performed,9 and residual viscoelastic material.4, 5 Although most eyes can tolerate the transient IOP elevation that occurs after cataract surgery, IOP spikes are potentially more dangerous in eyes with previous optic nerve compromise, such as those with preexisting damage from glaucoma or atherosclerosis-related ischemia.10, 11 Furthermore, extremely high or prolonged ocular hypertension can also result in severe corneal edema, pain, anterior ischemic optic neuropathy, and central retinal vein occlusion.12 Interventions to minimize early IOP spikes include techniques for removing viscoelastic materials,4, 13 prophylactic use of intracameral acetylcholine,13 and use of systemic or topical ocular hypotensive medications.11, 13 To our knowledge, the incidence of and preoperative factors associated with early IOP elevation on postoperative day 1 (POD1) after cataract surgeries performed only by training residents have not yet been reported.
Materials and methods
A database containing all cataract extraction surgeries performed in the teaching service of Harvard Medical School, Department of Ophthalmology at the Comprehensive Ophthalmology Service of the Massachusetts Eye and Ear Infirmary was constructed. The details of this IRB approved database have been previously described.14
In all, 1684 consecutive cataract surgeries performed mainly by residents from 1 July 2001 to 30 June 30 2006 were reviewed. In all, 102 surgeries with intraoperative vitreous loss (VL) and anterior vitrectomy were excluded because of the patient use of prescribed oral acetazolamide 250 mg (Diamox; Taro Pharmaceuticals Inc., Hawthorne, NY, USA) immediately postoperatively. Of the remaining 1582 surgeries, 305 surgeries performed by attending surgeons were excluded and additional 166 surgeries were excluded because of the lack of data such as preoperative IOP and POD1-IOP. Finally, 1111 surgeries were included in the analysis. Preoperative, perioperative, and postoperative information were gathered for all surgeries. Patient age, eye, diabetes mellitus (DM), glaucoma, ocular hypertension, glaucoma suspect, history of uveitis, presence of pseudoexfoliation syndrome (PXF), age-related macular degeneration (AMD), previous intraocular surgery, preoperative best spectacle-corrected visual acuity (BSCVA) and IOP, axial length, academic period in which the surgery was performed, type of surgical incision, ophthalmic viscosurgical device (OVD), and intraoperative complications including anterior capsular tear (ACT), posterior capsule tear (PCT), zonulysis, and conversion from clear corneal or scleral tunnel incision to extracapsular cataract extraction (ECCE) were all evaluated in the analysis. Intraoperatively, sodium hyaluronate (Healon; Abbott Medical Optics Inc., Santa Ana, CA, USA) was used for all procedures from July 2001 until November 2005, and combined chondroitin sulfate and sodium hyaluronate (Duovisc; Alcon Laboratories Inc., Fort Worth, TX, USA) were used for all procedures after this time. Postoperative data was analyzed with respect to BSCVA and IOP on the first postoperative day with elevated IOP defined as ≥23 mm Hg. IOP was checked by a Goldmann applanation tonometer and BSCVA was measured using standardized Snellen chart testing on the last preoperative visit and the first postoperative day. Improvement in BSCVA was defined as the difference between the BSCVA at the last preoperative visit and the first postoperative day. The main outcome measured was presence of POD1-IOP elevation.
First, surgeries were classified into two groups according to the presence or absence of POD1-IOP elevation. Fisher's exact test was used to compare eye, DM, glaucoma, ocular hypertension, glaucoma suspect, history of uveitis, PXF, AMD, previous intraocular surgery, academic period in which the surgery was performed, type of surgery, type of OVD, ACT, PCT, zonulysis, and conversion to ECCE. The Student t-test was used to compare age, preoperative BSCVA and IOP, axial length, the first postoperative day BSCVA, improvement in BSCVA at the fist postoperative day, and difference between preoperative IOP and POD-IOP.
Second, the relationships between predictor variables and POD1-IOP elevation were assessed by univariate and multivariate analyses using generalized estimating equations (GEEs). Age, laterality of eye operated on, DM, glaucoma, ocular hypertension, glaucoma suspect, history of uveitis, PXF, AMD, previous intraocular surgery, preoperative BSCVA and IOP, axial length, surgical academic quarter during which the surgery was performed, type of surgery, type of OVD, ACT, PCT, zonulysis, and conversion to ECCE were included as predictor variables. Age and variables with a P-value ≤0.20 in univariate analyses were candidates for the multivariate model. Then, a backward elimination process was used to develop the final model using P-value. The level of significance was set at 0.05. All P-values are two-tailed. Analyses were conducted using the SPSS program (version 19.0; IBM SPSS Inc., Chicago, IL, USA) and the SAS program (version 9.1; SAS Institute Inc., Cary, NC, USA).
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Results
Description of investigated variables
The average age in all surgeries was 70.9±10.8. In all, 49.2% (547/1111) of surgeries were of right eye and 50.8% (564/1111) were of left eye. In all, 259 patients had bilateral cataract surgery and 593 patients underwent unilateral surgery. A total of 18.8% (209/1111) of surgeries were diabetic, 5.7% (63/1111) had glaucoma, 0.6% (7/1111) had ocular hypertension, and 2.9% (32/1111) were glaucoma suspects. In all, 0.3% (3/1111) of surgeries had history of uveitis, 5.9% (65/1111) was found to have PXF preoperatively, 8.9% (99/1111) had AMD, and 7.5% (83/1111) had a history of intraocular surgery. Preoperative BSCVA (log MAR) was 0.52±0.48 and axial length was 23.8±1.7 mm. A total of 25.7% (286/1111) of surgeries were performed from January to March, 28.0% (311/1111) were from April to June, 22.1% (246/1111) were from July to September, and 24.2% (268/1111) were from October to December. 85.3% (948/1111) of surgeries were performed by clear cornea incision, 6.0% (67/1111) were by sclera tunnel incision, 2.0% (22/1111) were by ECCE, and 6.7% (74/1111) did not have a record. Healon was used in 82.5% (917/1111) and Duovisc was in 17.5% (194/1111). In all, 2.1% (23/1111) of surgeries had intraoperative ACT, 2.3% (26/1111) had PCT, 0.9% (10/1111) had zonulysis, and 0.7% (8/1111) had a conversion from clear corneal incision or sclera tunnel to ECCE. Postoperative BSCVA at day 1 (log MAR) was 0.48±0.49 and improvement in BSCVA at day 1 was −0.03±0.47. The average preoperative IOP was 16.0±3.2 mm Hg and the average POD1-IOP was 19.3±7.1 mm Hg, reflecting a significant increase in IOP (P<0.001, paired t-test). The difference between preoperative IOP and POD1-IOP was 3.4±6.7 mm Hg.
Distribution of IOP
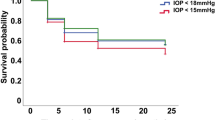
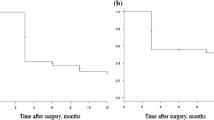
The incidence of preoperative IOP ≥23 mm Hg preoperatively was 3.1% (34/1111). In all, 2.6% of eyes (28/1111) were between 23 and 25 mm Hg, and 0.5% (6/1116) were between 26 and 29 mm Hg (Table 1). The incidence of increased IOP ≥23 mm Hg on the first postoperative day was 22.0% (244/1111). A total of 7.1% of eyes (79/1111) were between 23 and 25 mm Hg, 6.9% (76/1111) between 26 and 29 mm Hg, 5.5% (61/1111) between 30 and 39 mm Hg, and 2.5% (28/1111) were ≥40 mm Hg.
Comparison between POD1-IOP elevation group and control
To determine which variables were associated with IOP elevation on the first postoperative day after cataract extraction, all of the surgeries were classified into two groups, eyes with elevated IOP ≥23 mm Hg and eyes with IOP <23 mm Hg on the first postoperative day. The frequency of glaucoma and ocular hypertension was higher in the POD1-IOP elevation group (P=0.001 and P=0.007, respectively; Table 2). Preoperative IOP and axial length were higher in the POD1-IOP elevation group (P<0.001 and P=0.007, respectively). Furthermore, the difference between preoperative IOP and POD1-IOP was also higher in the POD1-IOP elevation group (P<0.001, Table 2).
Predictor factors for POD1-IOP elevation
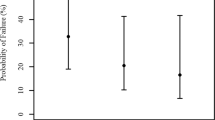
Univariate analysis using GEE revealed presence of glaucoma and ocular hypertension, axial length, and preoperative IOP were predictive for the POD1-IOP elevation: presence of glaucoma (P=0.001, OR=2.57; 95% confidence interval (95% CI)=1.45–4.54, Table 3) and ocular hypertension (P<0.001, OR=10.35; 95% CI=3.18–33.70), higher preoperative IOP (P<0.001, OR=3.88; 95% CI=2.06–7.31), and longer axial length (P=0.02, OR=1.12; 95% CI=1.02–1.23).
Multivariate analysis using GEE with backward elimination showed glaucoma, ocular hypertension, preoperative IOP, and axial length were predictive for the POD1-IOP elevation: presence of glaucoma (P=004, OR=2.38; 95% CI=1.31–4.30, Table 4) and ocular hypertension (P=003, OR=6.09; 95% CI=1.81–20.47), higher preoperative IOP (P<0.001, OR=3.73; 95% CI=1.92–7.25), and longer axial length (P=0.01, OR=1.15; 95% CI=1.03–1.29).
Discussion
The literature abounds with reports of intraoperative complications resulting from cataract surgeries performed by residents in training.15, 16, 17, 18, 19 Studies have documented the incidence of PCTs to range from 2.1 to 9.9% in resident-performed surgeries,15, 16, 17, 18, 19, 20, 21 although these incidences were higher than those reported by experienced surgeons (0.45–2.5%),20, 22, 23 and the incidence of VL was from 1.8 to 14.7%. The rates differed depending on the studies. Various patient characteristics such as mature 4+ nuclear sclerotic cataracts, zonular weakness following ocular trauma, and PXF were known to be related to increased risk of complications in resident-performed cataract surgeries.24 Nevertheless, there were few reports regarding the incidence of and preoperative factors associated with early IOP elevation after cataract surgeries performed by training residents.
The incidence of increased early postoperative IOP was reported in 1999 to be 7.9% in a study of 15 787 cases (77% phacoemulsification and 23% ECCE).25 In a study including phacoemulsification cases only, the incidence of early postoperative increased IOP was reduced to only 1.0% (http://one.aao.org/CE/PracticeGuidelines/PPP.aspx?sid=a3043761-ec14-40a0-bb84-d353240d211e). Comparison among studies is limited because the definitions of ‘IOP increase’ and surgeon's experience such as resident vs non-trainee were different. However, the incidence of IOP ≥26 mm Hg at 24 h after surgery was estimated to be 11.8% by three training surgeons.26 We similarly found our incidence to be 14.9% (165/1111; P=0.56, Fisher's exact test).
There is controversy regarding the pathophysiology of early IOP elevation after cataract surgery. IOP elevation was named Healon-block glaucoma, because aqueous outflow was obstructed by this high-molecular-weight viscoelastic material.27, 28 It was well known that the turnover of injected sodium hyaluronate depended on the viscosity of the injected solution and the less viscous sodium hyaluronate resulted in shorter prolonged IOP rise in owl monkey eyes than did higher viscosity preparations of sodium hyaluronate.29 Mechanical deformation of angle structures before or during surgery, inflammation, hemorrhage, pigment dispersion, and retained lenticular materials are also theorized to cause early IOP rises.30
In our analysis, we found that presence of glaucoma and ocular hypertension, higher preoperative IOP, and longer axial length were predictive risk factors for increased POD1-IOP following cataract surgery.
Glaucoma is a well-known risk factor for early postoperative IOP increase.5, 31, 32, 33, 34 Glaucomatous eye had a higher IOP than normal eyes and glaucoma suspect eyes at POD1, even with the use of topical β-blockers and α-agonists at the time of surgery in glaucoma and glaucoma suspect eyes.32 The IOP in eyes with primary open angle glaucoma (POAG) increased from postoperative day 1 to 3 and afterward gradually decreased, whereas the IOP in normal eyes was reduced from the first day after surgery.33
Myopia is known to be one of risk factors for POAG.35, 36, 37 It was reported that compared with patient groups whose axial length was under 25 mm, the other group whose axial length was over 25 mm had a statistically significant IOP increase 1 day after uneventful phacoemuslification.38 Our study also confirms that longer axial length is associated with an increased first postoperative day IOP.
PXF is known to be related to ocular hypertension and OAG,39, 40, 41 but the relationship to early increased postoperative IOP is controversial. Non-glaucomatous eyes with PXF were reported not to show IOP increase at the postoperative day 1 after sclera tunnel incision and phacoemulsification.42 Conversely, it was also reported that when compared with non-PXF patients, the non-glaucomatous PXF patients had a significant IOP increase on POD1 after phacoemulsification.43 Furthermore, the type of intraoperative OVD was also one of the predictive factors for early postoperative IOP increase. A significantly higher mean IOP was showed on the first postoperative day after phacoemulsification in patients who received Viscoat (4% chondroitin sulfate/3% sodium hyaluronate, Alcon Laboratories Inc.) than in patients who received Provisc (1.4% sodium hyaluronate, Alcon Laboratories Inc.).44 However, after 24 h and at 1 week postoperatively, there was no difference in IOP. The mean IOP increased at 6 h after small incision phacoemulsification using either Viscoat or Healon 5 (2.3% higher molecular weight sodium hyaluronate, Abbott Medical Optics Inc.) and found that mean IOP was significantly higher in the Viscoat group at this time point.10 Even though the mechanism of postoperative IOP increase has not been fully investigated, the amount of remaining OVD at the end of surgery may influence the level of early postoperative IOP. Sodium hyaluronate can be removed more quickly and easily, as it is highly cohesive. The difficulty in removing dispersive OVDs, such as chondroitin sulfate, has been reported with an in vitro model.45 However, in our study, PXF and the type of intraoperative OVD were not predictive factors for the first postoperative day IOP increase.
In addition, 305 surgeries performed by attending surgeons were excluded because we novelly aimed to investigate the risk factors for POD1-IOP elevation in the resident-performed cataract surgeries. However, compared with attending surgeon-performed cataract surgeries the incidence of POD1-IOP elevation was not higher in the training resident-performed cataract surgeries (P=0.94, χ2-test, data not shown).
The limitations of our study include its retrospective nature, and the variable hour intervals between surgery and POD1 follow-up visits. In addition, all IOP measurements were not individually corrected for corneal thickness. One could argue that corneal edema with pachymetry readings would need to be considered a confounder in any studies on postoperative IOP measurements. The central corneal thickness was reported to increase in the immediate postoperative period 6% thicker at day 1 after cataract surgery returning to the preoperative thickness at 1 week.46 It is well known that thicker cornea in non-surgical patients causes an overestimation of IOP measured by applanation tonometry.47, 48, 49 However, as the measurements compared preoperative with postoperative IOP for each individual patient rather than the mean between groups, the corneal pachymetry will have a lesser role in the variability of the values.
In summary, increased IOP on the first postoperative day following cataract surgery occurs frequently (22.0%). Understanding the variables that may be associated with an increased likelihood of an elevated postoperative IOP will help in preventing and treating this transient but potentially harmful complication.

References
Allan BD, Baer RM, Heyworth P, Duguid IG, Dart JK . Conventional routine clinical review may not be necessary after uncomplicated phacoemulsification. Br J Ophthalmol 1997; 81: 548–550.
McKellar MJ, Elder MJ . The early complications of cataract surgery: is routine review of patients 1 week after cataract extraction necessary? Ophthalmology 2001; 108: 930–935.
Ahmed II, Kranemann C, Chipman M, Malam F . Revisiting early postoperative follow-up after phacoemulsification. J Cataract Refract Surg 2002; 28: 100–108.
Kohnen T, von Ehr M, Schutte E, Koch DD . Evaluation of intraocular pressure with Healon and Healon GV in sutureless cataract surgery with foldable lens implantation. J Cataract Refract Surg 1996; 22: 227–237.
O’Brien PD, Ho SL, Fitzpatrick P, Power W . Risk factors for a postoperative intraocular pressure spike after phacoemulsification. Can J Ophthalmol 2007; 42: 51–55.
Falck A, Hautala N, Turunen N, Airaksinen PJ . A four-year prospective study on intraocular pressure in relation to phacoemulsification cataract surgery. Acta Ophthalmol 2009; e-pub ahead of print 9 December 2009; doi:10.1111/j.1755-3768.2009.01790.x.
Laurell CG, Wickstrom K, Zetterstrom C, Lundgren B . Inflammatory response after endocapsular phacoemulsification or conventional extracapsular lens extraction in the rabbit eye. Acta Ophthalmol Scand 1997; 75: 401–404.
Cekic O, Batman C . Effect of capsulorhexis size on postoperative intraocular pressure. J Cataract Refract Surg 1999; 25: 416–419.
Lagreze WD, Bomer TG, Funk J . Effect of surgical technique on the increase in intraocular pressure after cataract extraction. Ophthalmic Surg Lasers 1996; 27: 169–173.
Rainer G, Menapace R, Findl O, Georgopoulos M, Kiss B, Petternel V . Intraocular pressure after small incision cataract surgery with Healon5 and Viscoat. J Cataract Refract Surg 2000; 26: 271–276.
Cetinkaya A, Akman A, Akova YA . Effect of topical brinzolamide 1% and brimonidine 0.2% on intraocular pressure after phacoemulsification. J Cataract Refract Surg 2004; 30: 1736–1741.
Rhee DJ, Deramo VA, Connolly BP, Blecher MH . Intraocular pressure trends after supranormal pressurization to aid closure of sutureless cataract wounds. J Cataract Refract Surg 1999; 25: 546–549.
Wedrich A, Menapace R . Intraocular pressure following small-incision cataract surgery and polyHEMA posterior chamber lens implantation. A comparison between acetylcholine and carbachol. J Cataract Refract Surg 1992; 18: 500–505.
Cremers SL, Ciolino JB, Ferrufino-Ponce ZK, Henderson BA . Objective assessment of skills in intraocular surgery (OASIS). Ophthalmology 2005; 112: 1236–1241.
Albanis CV, Dwyer MA, Ernest JT . Outcomes of extracapsular cataract extraction and phacoemulsification performed in a university training program. Ophthalmic Surg Lasers 1998; 29: 643–648.
Cruz OA, Wallace GW, Gay CA, Matoba AY, Koch DD . Visual results and complications of phacoemulsification with intraocular lens implantation performed by ophthalmology residents. Ophthalmology 1992; 99: 448–452.
Allinson RW, Metrikin DC, Fante RG . Incidence of vitreous loss among third-year residents performing phacoemulsification. Ophthalmology 1992; 99: 726–730.
Corey RP, Olson RJ . Surgical outcomes of cataract extractions performed by residents using phacoemulsification. J Cataract Refract Surg 1998; 24: 66–72.
Smith JH, Seiff SR . Outcomes of cataract surgery by residents at a public county hospital. Am J Ophthalmol 1997; 123: 448–454.
Ang GS, Whyte IF . Effect and outcomes of posterior capsule rupture in a district general hospital setting. J Cataract Refract Surg 2006; 32: 623–627.
Lee JS, Hou CH, Yang ML, Kuo JZ, Lin KK . A different approach to assess resident phacoemulsification learning curve: analysis of both completion and complication rates. Eye (Lond) 2009; 23: 683–687.
Pingree MF, Crandall AS, Olson RJ . Cataract surgery complications in 1 year at an academic institution. J Cataract Refract Surg 1999; 25: 705–708.
Gimbel HV, Sun R, Ferensowicz M, Anderson Penno E, Kamal A . Intraoperative management of posterior capsule tears in phacoemulsification and intraocular lens implantation. Ophthalmology 2001; 108: 2186–2189; discussion 2190–2182.
Rutar T, Porco TC, Naseri A . Risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Ophthalmology 2009; 116: 431–436.
Desai P, Minassian DC, Reidy A . National cataract surgery survey 1997-8: a report of the results of the clinical outcomes. Br J Ophthalmol 1999; 83: 1336–1340.
Browning AC, Alwitry A, Hamilton R, Rotchford A, Bhan A, Amoaku WM . Role of intraocular pressure measurement on the day of phacoemulsification cataract surgery. J Cataract Refract Surg 2002; 28: 1601–1606.
Barron BA, Busin M, Page C, Bergsma DR, Kaufman HE . Comparison of the effects of Viscoat and Healon on postoperative intraocular pressure. Am J Ophthalmology 1985; 100: 377–384.
Hoffer KJ . Effects of extracapsular implant techniques on endothelial density. Arch Ophthalmol 1982; 100: 791–792.
Schubert HD, Denlinger JL, Balazs EA . Exogenous Na-hyaluronate in the anterior chamber of the owl monkey and its effect on the intraocular pressure. Exp Eye Res 1984; 39: 137–152.
Krug JJ . Glaucoma after cataract surgery. In: Albert D, Jakobiec FA (eds). Principles and Practice of Ophthalmology, 2nd edn. WB Saunders: Philadelphia, 2000, pp 2824–2834.
Barak A, Desatnik H, Ma-Naim T, Ashkenasi I, Neufeld A, Melamed S . Early postoperative intraocular pressure pattern in glaucomatous and nonglaucomatous patients. J Cataract Refract Surg 1996; 22: 607–611.
Shingleton BJ, Rosenberg RB, Teixeira R, O’Donoghue MW . Evaluation of intraocular pressure in the immediate postoperative period after phacoemulsification. J Cataract Refract Surg 2007; 33: 1953–1957.
Yasutani H, Hayashi K, Hayashi H, Hayashi F . Intraocular pressure rise after phacoemulsification surgery in glaucoma patients. J Cataract Refract Surg 2004; 30: 1219–1224.
Alwitry A, Rotchford A, Gardner I . First day review after uncomplicated phacoemulsification: is it necessary? Eur J Ophthalmol 2006; 16: 554–559.
Charliat G, Jolly D, Blanchard F . Genetic risk factor in primary open-angle glaucoma: a case-control study. Ophthalmic Epidemiol 1994; 1: 131–138.
Landers J, Goldberg I, Graham SL . Analysis of risk factors that may be associated with progression from ocular hypertension to primary open angle glaucoma. Clin Exp Ophthalmol 2002; 30: 242–247.
Suzuki Y, Iwase A, Araie M, Yamamoto T, Abe H, Shirato S et al. Risk factors for open-angle glaucoma in a Japanese population: the Tajimi Study. Ophthalmology 2006; 113: 1613–1617.
Cho YK . Early intraocular pressure and anterior chamber depth changes after phacoemulsification and intraocular lens implantation in nonglaucomatous eyes. Comparison of groups stratified by axial length. J Cataract Refract Surg 2008; 34: 1104–1109.
Hiller R, Sperduto RD, Krueger DE . Pseudoexfoliation, intraocular pressure, and senile lens changes in a population-based survey. Arch Ophthalmol 1982; 100: 1080–1082.
Ekstrom C . Elevated intraocular pressure and pseudoexfoliation of the lens capsule as risk factors for chronic open-angle glaucoma. A population-based five-year follow-up study. Acta Ophthalmol 1993; 71: 189–195.
Klemetti A . Intraocular pressure in exfoliation syndrome. Acta Ophthalmol Suppl 1988; 184: 54–58.
Wirbelauer C, Anders N, Pham DT, Wollensak J, Laqua H . Intraocular pressure in nonglaucomatous eyes with pseudoexfoliation syndrome after cataract surgery. Ophthalmic Surg Lasers 1998; 29: 466–471.
Pohjalainen T, Vesti E, Uusitalo RJ, Laatikainen L . Intraocular pressure after phacoemulsification and intraocular lens implantation in nonglaucomatous eyes with and without exfoliation. J Cataract Refract Surg 2001; 27: 426–431.
Kovacevic S, Pastar Z, Sessa Z, Krpina V, Paic E . Comparison of the effect of two viscoelastic agents on an early postoperative intraocular pressure. Coll Antropol 2005; 29 (Suppl 1): 115–117.
Assia EI, Apple DJ, Lim ES, Morgan RC, Tsai JC . Removal of viscoelastic materials after experimental cataract surgery in vitro. J Cataract Refract Surg 1992; 18: 3–6.
Salvi SM, Soong TK, Kumar BV, Hawksworth NR . Central corneal thickness changes after phacoemulsification cataract surgery. J Cataract Refract Surg 2007; 33: 1426–1428.
Bhan A, Browning AC, Shah S, Hamilton R, Dave D, Dua HS . Effect of corneal thickness on intraocular pressure measurements with the pneumotonometer, Goldmann applanation tonometer, and Tono-Pen. Invest Ophthalmol Vis Sci 2002; 43: 1389–1392.
Doughty MJ, Zaman ML . Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Surv Ophthalmol 2000; 44: 367–408.
Ehlers N, Bramsen T, Sperling S . Applanation tonometry and central corneal thickness. Acta Ophthalmol 1975; 53: 34–43.
Acknowledgements
This study was supported in part by grants from the Research to Prevent Blindness, the Norman Knight Ophthalmology Legacy Fund, and the Massachusetts Lions Foundation, the Harvard 50th Anniversary Scholars Grant, a grant (2009-464) from the Asan Institute for Life Sciences, Seoul, Republic of Korea, and National Research Foundation of Korea (NRF) Grant funded by the Korean Government (NRF-2008-331-E00209).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Material has been previously presented at the American Society of Cataract and Refractive Surgery (ASCRS) Meeting on May, 2006.
Rights and permissions
About this article
Cite this article
Kim, J., Jo, MW., Brauner, S. et al. Increased intraocular pressure on the first postoperative day following resident-performed cataract surgery. Eye 25, 929–936 (2011). https://doi.org/10.1038/eye.2011.93
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.93
Keywords
This article is cited by
-
Cataract surgery and IOP: a systematic review of randomised controlled trials
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Ocular complications of perioperative anesthesia: a review
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)
-
Phacoemulsification in patients with uveitis: long-term outcomes
BMC Ophthalmology (2020)
-
Brimonidine–timolol versus brinzolamide–timolol for treatment of elevated intraocular pressure after phacoemulsification surgery
International Ophthalmology (2018)
-
Is the 1-day postoperative IOP check needed post uncomplicated phacoemulsification in patients with glaucoma and ocular hypertension?
Eye (2015)