Abstract
Aim
To investigate cases with conjunctival pigmentation originating from sclerotomy sites after 23-gauge microincisional vitrectomy surgery (MIVS).
Methods
This is a retrospective study comprised of 185 eyes from 185 consecutive patients who underwent 23-gauge MIVS. The authors investigated the incidence and the clinical factors associated with conjunctival pigmentation, including indication of vitrectomy and surgical procedures.
Results
Eight eyes (4.3%) from 185 eyes showed conjunctival pigmentation after surgery within 7 days postoperatively. Light microscopic examination of excised tissue showed infiltration of abundant dark brownish colored melanophages with surrounding scattered, finely granular, melanin pigments. C3F8 gas tamponade (OR, 9.4; 95% CI, 1.9–44.5; P=0.005) was significantly associated with conjunctival pigmentation. The mean surface area (21.26±2.21 mm2) of three eyes with C3F8 tamponade was significantly larger than that of five eyes (2.51±0.73 mm2) without tamponade (P=0.025). Neither leakage nor hypotony was found.
Conclusions
Intraocular melanin pigments could prolapse through the sclerotomy site and cause conjunctival pigmentation after 23-gauge MIVS. Thus, preoperative warning is necessary in patients with 23-gauge MIVS.
Similar content being viewed by others
Introduction
Microincision vitrectomy surgery (MIVS) by a 25-gauge vitrectomy system was proposed by Fujii et al.1 Since then, 25-gauge vitrectomy has been reported to reduce the operating time and postoperative inflammation compared with the conventional 20-gauge vitrectomy.2, 3, 4, 5
In 2005, Eckardt introduced a 23-gauge MIVS with less instrument flexibility allowing greater ocular rotation and the ability to perform a more complete peripheral vitrectomy.6 Thus, the 23-gauge system has become an option for MIVS. Several studies reported the safety and effectiveness of the 23-gauge MIVS.7, 8, 9, 10, 11 However, there have been questions regarding the self-sealing characteristics and postoperative hypotony in some of the cases.8, 12, 13
Previously localized conjunctival and episcleral pigmentation after 20-gauge conventional vitrectomy has been considered owing to a reaction to the sutures used to close the sclerotomy site.14
Recently, a case of conjunctival pigmentation after 23-gauge MIVS for retinal detachment surgery was reported.15 Furthermore, the authors reported that it occurred even after using the 25-gauge chandelier illumination system.16
To our knowledge, the clinical factors for conjunctival pigmentation after 23-gauge MIVS have not been reported before. In the present study, the authors evaluated the cases that showed conjunctival pigmentation originating from sclerotomy sites after 23-gauge MIVS. In addition, the authors investigated the clinical factors associated with conjunctival pigmentation, including indication of vitrectomy and surgical procedures.
Patients and methods
Patients and study design
The authors did a retrospective chart review of all the patients who had 23-gauge MIVS. The study was done in accordance with the Declaration of Helsinki, and the study protocol was approved by the Institutional Review Board of Kyungpook National University Hospital. All patients were informed of the procedure and informed consent was obtained.
The inclusion criteria of the study included patients who had 23-gauge MIVS and were followed up for more than 2 months. The exclusion criteria were as follows: patients with primary or acquired conjunctival melanosis or melanocytic tumors, patients with chronic exposure to various topical or systemic medications including epinephrine, tetracycline, and chlorpromazine, patients with previous ocular surgery including pterygium or vitrectomy surgery (except cataract surgery), and patients with intravitreal injections within 12 months. When the lesion was revealed within 2 months of the follow-up period after surgery, the eyes were classified as eyes with conjunctival pigmentation. In patients with bilateral surgery, only the first eye that was operated on was included.
The patients’ records were reviewed for age, sex, lens status, indication of vitrectomy, surgical procedures, operating time, and postoperative complications. The intraoperative argon laser photocoagulation was classified into three groups as follows: none, focal (partial panretinal photocoagulation or demarcation laser for retinal breaks), and complete panretinal photocoagulation. Each patient underwent complete preoperative ophthalmic examinations including slit-lamp biomicroscopy, intraocular pressure (IOP) measurement using applanation tonometry, and fundus examination by indirect ophthalmoscopy. B-scan ultrasonography was done in eyes with vitreous hemorrhage severe enough to obscure the fundus examination. Follow-up examinations were done from day 1 to 7 and at weeks 2, 4, and 8, postoperatively.
The surface area of conjunctival pigmentation included the conjunctiva of all visible punctated pigmentation around the sclerotomy site. Patients with conjunctival pigmentation had slit-lamp photography at every follow-up period. The maximal surface area from the affected eye was measured by Eye image capture program (E-medio, Seoul, Korea) for image capture, and Image J program (http://rsbweb.nih.gov/ij/; open source, public domain software) for measurement at 2 months postoperatively.
Surgical technique
The surgical procedures were done by a single surgeon (SK). The procedure was started by conjunctival displacement in the inferotemporal, superotemporal, and superonasal quadrants using a special pressure plate (DORC, Auidland, Holland) to hold it firmly to the sclera. A 0.72-mm wide 23-gauge stiletto blade (45° angle; BD Medical-Ophthalmic Systems, Franklin Lakes, NJ, USA) was then inserted at a 15°–30° angle through the conjunctiva, sclera, and pars plana 4.0 mm from the limbus. The microcannula was then inserted through the conjunctival incision and into the sclera tunnel using a specially designed blunt inserter (DORC). For maintenance of IOP, the infusion pressure was adjusted to as high as 20 mm Hg using the Accurus Vitrectomy System (Alcon Laboratories, Fort Worth, TX, USA). Then, the microcannulae were plugged and the infusion line was closed before the corneal incision procedure. All of the phakic eyes with cataract underwent combined phacoemulsification with 2.75 mm clear corneal incision using the Legacy or Infinity System (Alcon Laboratories).
Then, 23-gauge MIVS procedures were done using the Accurus vitrectomy system adjusting the infusion pressure by as high as 35 mm Hg. A core vitrectomy and detachment of the posterior hyaloid face was performed. Vitreous base shaving under sclera depression was done to remove peripheral cortical vitreous in eyes with proliferative diabetic retinopathy (PDR) and rhegmatogenous retinal detachment (RRD). Endolaser photocoagulation was done to complete panretinal photocoagulation up to the anterior retina in eyes with PDR. Retinal breaks were treated with demarcation laser with or without C3F8 gas tamponade. After the vitrectomy and other intraocular manipulations were completed, infusion pressure was adjusted by as high as 20 mm Hg. Implantation of an acrylic foldable 6.0 mm intraocular lens was done without corneal wound suture. Then, the superotemporal and superonasal trocars were removed with the infusion clamped. The inferotemporal cannula and infusion line were removed en bloc with the infusion unclamped followed by conjunctival repositioning. After gentle pressure using a Q-tip over the sclerotomy sites, both conjunctiva and scleral incision of the entry sites were closed together with a single releasable 8-0 polyamide (Monosof, Syneture, Covidien, Mansfield, MA, USA), creating hemi-bow ties in all sclerotomy sites.17 Then, dexamethasone and gentamycin were injected subconjunctivally. The postoperative regimen included 0.3% topical ofloxacin eye drops four times per day for 1 week and 1% topical prednisolone acetate eye drops four times per day that was usually tapered off over 4 weeks. All of the sutures were released at the slit-lamp 1 day after surgery. Each wound was evaluated for leakage by Seidel test at postoperative follow-up. Patients who had fluid–gas exchange were instructed to remain face down for 7 to 10 days.
Statistical analysis
Means were used for description of quantitative data, and percentages were used for qualitative data. Two-sample t-test or Mann–Whitney U-test was done for quantitative data, and χ2-test or Fisher’s exact test was used to compare qualitative data. Multivariate model was done using variables that were significantly associated with the conjunctival pigmentation in univariate analysis. Statistical analyses were done using SPSS software (version 14.0; SSPS Inc., Chicago, IL, USA). For all statistical tests, P<0.05 was considered significant.
Results
A total of 210 eyes from 210 patients were enrolled in this study. Nineteen eyes were excluded, including two eyes with pre-existing conjunctival nevus, seven eyes with previous ocular surgery, and ten eyes owing to loss of follow-up. A total of 185 eyes from 185 patients met the inclusion criteria. Eight eyes (4.3%) from 8 patients showed conjunctival pigmentation after 23-gauge MIVS, and 177 eyes (95.7%) from 177 patients showed no lesion. Demographics and clinical data of the patients are summarized in Table 1.
Age, sex, lens status, indication of vitrectomy, operating time, simultaneous cataract extraction, scleral buckle, cryotherapy, and silicone oil tamponade were not associated with the conjunctival pigmentation after 23-gauge MIVS (P>0.05, respectively).
Eight eyes (100%) with conjunctival pigmentation and 90 eyes (50.8%) without conjunctival pigmentation had complete vitrectomy, including vitreous base dissection (P=0.007). One eye (12.5%) with conjunctival pigmentation and 16 eyes (9.1%) without conjunctival pigmentation had complete PRP (P=0.545). Three eyes (37.5%) with conjunctival pigmentation and 11 eyes (6.2%) without conjunctival pigmentation had C3F8 tamponade at the end of vitrectomy (P=0.016). Three eyes in the group with conjunctival pigmentation included two eyes of PDR with multiple retinal breaks and one eye of RRD. Eleven eyes in the group without conjunctival pigmentation had macular hole.
Multivariate logistic regression analysis confirmed that C3F8 tamponade (OR, 9.4; 95% CI, 1.9–44.5; P=0.005) was associated to the conjunctival pigmentation after 23-gauge MIVS.
Table 2 showed the clinical characteristics of the eight eyes from eight patients with conjunctival pigmentation. Seven eyes (87.5%) had 23-gauge MIVS for PDR. All of the 8 eyes had complete vitrectomy including vitreous base dissection, and showed the conjunctival pigmentation within 7 days after vitrectomy. Owing to multiple retinal tears, one eye with RRD and two eyes with PDR had C3F8 tamponade at the end of vitrectomy.
The surface area of inferotemporal lesion was 23.79 mm2 in case 2 and the surface area of superotemporal lesion was 20.28 mm2 in case 3. The mean of the maximal surface area (21.26±2.21 mm2) of three eyes with C3F8 tamponade was significantly larger than that of five eyes (2.51±0.73 mm2) without C3F8 tamponade (Mann–Whitney U-test, P=0.025).
Neither leakage nor hypotony (IOP <6 mm Hg) was found in all of the 185 eyes during the follow-up period. Also, there was no case of endophthalmitis.
Case report (case 2)
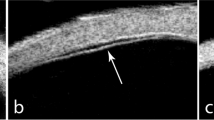
A 74-year-old female patient presented sudden decreased visual acuity due to vitreous hemorrhage secondary to PDR. At 5 days after combined phacoemulsification and 23-gauge MIVS, conjunctival pigmentation was found in superonasal and inferotemporal sclerotomy sites (Figure 1a). Two months after the surgery, excisional biopsy was done under topical anesthesia owing to a cosmetic problem and a necessity to rule out melanoma. Light microscopic examination of excised tissue showed non-keratinizing squamous epithelium and substantia propria of the conjunctiva (Figure 1b). Infiltration of abundant dark brownish colored melanophages, which are macrophages that have ingested melanin pigments in the substantia propria, was observed at higher magnification. Scattered, finely granular, melanin pigments surrounding the melanophages were also noted. Neither nevus cell nor melanoma cell was observed in the sample. Six weeks after the conjunctival excision, there were remnants of a pigmented lesion in the right inferotemporal site.
(a) Slit-lamp photograph at 2 months after 23-gauge microincisional vitrectomy surgery showed pigmentation in the right inferotemporal sclerotomy site (case 2). (b) Light microscopic examination of excised tissue showed non-keratinizing squamous epithelium (asterisk) and substantia propria (arrowhead) of the conjunctiva. Infiltration of abundant dark brownish colored melanophages (arrows), which contained abundant melanin pigments in the substantia propria, was seen. In addition, it showed scattered, finely granular, melanin pigments surrounding the melanophages. Neither nevus cell nor melanoma cell was observed. (H&E staining, original magnification × 400).
Discussion
To our knowledge, clinical factors related to conjunctival pigmentation after 23-gauge MIVS have not been reported before this, and the authors investigated 8 eyes (4.3%) with conjunctival pigmentation from 191 eyes, which had 23-gauge MIVS.
Smiddy et al18 reported dark brown pigmentation at episclera and conjunctiva, measured 10 × 6 mm size surrounding a sclerotomy site after 20-gauge conventional vitrectomy and retinal reattachment surgery. Histological techniques identified the pigmented materials as melanin. The location of the melanin in macrophages and in the extracellular space showed that it does not originate from the conjunctiva but from the eye. Liu et al19 investigated the material prolapsed from the sclerotomy sites of 36 cases during 20-gauge standard vitrectomy. Light microscopic analyses of 35 cases (97.2%) showed a large amount of well-proportioned eosinophilic vitreous tissue with scattered pigment granules and small, pigmented globules. A portion of the ciliary tissue prolapsed in six cases (together with some retinal tissues in three cases), including ciliary non-pigmented epithelium, pigmented epithelium, and ciliary muscles.
In the present study, H&E staining of excised tissue of case 2 showed infiltration of abundant dark brownish colored melanophages in the substantia propria, which is similar to the study by Smiddy et al.18 The authors also speculated that the melanin was discharged from the sclerotomy sites. First, there was no pre-existing conjunctival pigmentation and it occurred exactly on the sclerotomy sites in the affected eye, in particular, within 7 days postoperatively. Second, based on the light microscopic examination, there was neither nevus cell nor melanoma cell.
Previous studies have shown that cryotherapy causes release of both extracellular melanin and viable retinal pigment epithelial (RPE) cells, and the released pigments prolapse through the sclerotomy sites.18, 20, 21
In the present study, C3F8 tamponade was associated to the conjunctival pigmentation. The mean of the maximal surface area of three eyes with C3F8 tamponade was significantly larger than that of five eyes without C3F8 tamponade. These three eyes included two eyes that had PDR with multiple retinal tears and one eye that had RRD. It is possible that the RPE cells release from the retinal tears and prolapse through the sclerotomy sites. Thus, 11 eyes with macular hole could not show any conjunctival pigmentation, though these eyes had C3F8 tamponade.
Although the factor of complete vitrectomy in the univariate analysis (P=0.007) was not significant in the multivariate analysis (P>0.05), it could not be excluded from one of the risk factors. First, it could be due to the small number of cases with conjunctival pigmentation in this study. Second, previous reports showed that complete vitrectomy could be more related to the sclerotomy leakage in MIVS. Bourla et al22 reported that scleral wound leakage occurred despite oblique 25-gauge trocar insertions in more than one-third of the cases (36.4%) that received gas tamponade with vitreous base dissection for RRD. Nagpal et al23 reported that an endoscopic view of a 23-gauge sclerotomy site with core vitrectomy showed the incarceration of vitreous to be plugging the inner opening of the sclerotomy. In addition, this vitreous was believed to serve as sealing the ports from inside and preventing further leakage. Woo et al13 reported that, specifically, vitreous base dissection is one of the risk factors of sclerotomy leakage requiring suture placement after 23-gauge MIVS due to the reduced plugging effect of remnants of vitreous under sclerotomy.
In the present study, no vitreous clogging due to complete vitrectomy could affect undetectable leakage of melanin pigments through the sclerotomy sites in eight eyes with conjunctival pigmentation. Eighty-seven eyes that had core vitrectomy due to non-diabetic vitreous hemorrhage or epiretinal membrane or macular hole did not show any conjunctival pigmentation. It was probably due to the plugging effect by the remnants of vitreous.
It is possible that the conjunctival pigmentation may be due to racial variation. However, the authors of this study were unable to compare their results to Caucasian patients or dark skinned patients owing to the absence of any previous reports. In addition, conjunctival pigmentation may occur owing to the two-step DORC cannula system. In our previous report after using the 25-gauge Torpedo Mini-Light chandelier illumination system with the same 2-step technique, there were three cases of conjunctival pigmentation. Furthermore, conjunctival pigmentation could have occurred owing to the following reasons: genetic predisposition of the Asian patient population, undetected pre-existing primary or acquired conjunctival melanosis due to the nature of a retrospective study, the type of suture used, the intraocular tamponade material used, the duration of the surgery, and the use of inadvertent cautery at the end of the surgery.
The current study has several limitations, including its retrospective nature, a small number of cases, and no comparison with the other types of vitrectomy such as 20-gauge and 25-gauge. However, this study shows conjunctival pigmentation occurred within 1 week postoperatively without any sign of sclerotomy site leakages. Preoperative warning for such a complication is necessary in patients with 23-gauge MIVS. In addition, a further prospective study with a wide range of racial variation is necessary.

References
Fujii GY, De Juan Jr E, Humayun MS, Pieramici DJ, Chang TS, Awh C et al. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology 2002; 109 (10): 1807–1813.
Ibarra MS, Hermel M, Prenner JL, Hassan TS . Longer-term outcomes of transconjunctival sutureless 25-gauge vitrectomy. Am J Ophthalmol 2005; 139 (5): 831–836.
Kadonosono K, Yamakawa T, Uchio E, Yanagi Y, Tamaki Y, Araie M . Comparison of visual function after epiretinal membrane removal by 20-gauge and 25-gauge vitrectomy. Am J Ophthalmol 2006; 142 (3): 513–515.
Lakhanpal RR, Humayun MS, de Juan Jr E, Lim JI, Chong LP, Chang TS et al. Outcomes of 140 consecutive cases of 25-gauge transconjunctival surgery for posterior segment disease. Ophthalmology 2005; 112 (5): 817–824.
Rizzo S, Genovesi-Ebert F, Murri S, Belting C, Vento A, Cresti F et al. 25-gauge, sutureless vitrectomy and standard 20-gauge pars plana vitrectomy in idiopathic epiretinal membrane surgery: a comparative pilot study. Graefes Arch Clin Exp Ophthalmol 2006; 244 (4): 472–479.
Eckardt C . Transconjunctival sutureless 23-gauge vitrectomy. Retina 2005; 25 (2): 208–211.
Fine HF, Iranmanesh R, Iturralde D, Spaide RF . Outcomes of 77 consecutive cases of 23-gauge transconjunctival vitrectomy surgery for posterior segment disease. Ophthalmology 2007; 114 (6): 1197–1200.
Gupta OP, Ho AC, Kaiser PK, Regillo CD, Chen S, Dyer DS et al. Short-term outcomes of 23-gauge pars plana vitrectomy. Am J Ophthalmol 2008; 146 (2): 193–197.
Lott MN, Manning MH, Singh J, Zhang H, Singh H, Marcus DM . 23-gauge vitrectomy in 100 eyes: short-term visual outcomes and complications. Retina 2008; 28 (9): 1193–1200.
Tewari A, Shah GK, Fang A . Visual outcomes with 23-gauge transconjunctival sutureless vitrectomy. Retina 2008; 28 (2): 258–262.
Park DH, Shin JP, Kim SY . Surgically induced astigmatism in combined phacoemulsification and vitrectomy; 23-gauge transconjunctival sutureless vitrectomy versus 20-gauge standard vitrectomy. Graefes Arch Clin Exp Ophthalmol 2009; 247 (10): 1331–1337.
Warrier SK, Jain R, Gilhotra JS, Newland HS . Sutureless vitrectomy. Indian J Ophthalmol 2008; 56 (6): 453–458.
Woo SJ, Park KH, Hwang JM, Kim JH, Yu YS, Chung H . Risk factors associated with sclerotomy leakage and postoperative hypotony after 23-gauge transconjunctival sutureless vitrectomy. Retina 2009; 29 (4): 456–463.
Michels RG . Vitreous Surgery. St Louis, CV: Mosby, 1981, pp 412.
Cha DM, Woo SJ, Ahn J, Park KH . A case of sympathetic ophthalmia presenting with extraocular symptoms and conjunctival pigmentation after repeated 23-gauge vitrectomy. Ocul Immunol Inflamm 2010; 18 (4): 265–267.
Park DH, Shin JP, Kim SY . Conjunctival pigmentation after 25-gauge chandelier illumination system. Br J Ophthalmol 2010; 94 (11): 1547.
Lee BR, Song Y . Releasable suture technique for the prevention of incompetent wound closure in transconjunctival vitrectomy. Retina 2008; 28 (8): 1163–1165.
Smiddy WE, Yeo JH, Michels RG, Green WR . Conjunctival pigmentation following pars plana vitrectomy. Retina 1987; 7 (1): 38–40.
Liu W, Huang SY, Zhang P, Tang SB, Li JQ, Zheng HL . Bioptic significance of incarcerated contents at sclerotomy sites during vitrectomy. Retina 2004; 24 (3): 407–411.
Campochiaro PA, Kaden IH, Vidaurri-Leal J, Glaser BM . Cryotherapy enhances intravitreal dispersion of viable retinal pigment epithelial cells. Arch Ophthalmol 1985; 103 (3): 434–436.
Glaser BM, Vidaurri-Leal J, Michels RG, Campochiaro PA . Cryotherapy during surgery for giant retinal tears and intravitreal dispersion of viable retinal pigment epithelial cells. Ophthalmology 1993; 100 (4): 466–470.
Bourla DH, Bor E, Axer-Siegel R, Mimouni K, Weinberger D . Outcomes and complications of rhegmatogenous retinal detachment repair with selective sutureless 25-gauge pars plana vitrectomy. Am J Ophthalmol 2010; 149 (4): 630–634.
Nagpal M, Wartikar S, Nagpal K . Comparison of clinical outcomes and wound dynamics of sclerotomy ports of 20, 25, and 23 gauge vitrectomy. Retina 2009; 29 (2): 225–231.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Park, D., Shin, J. & Kim, S. Conjunctival pigmentation after 23-gauge microincisional vitrectomy surgery. Eye 25, 1465–1470 (2011). https://doi.org/10.1038/eye.2011.199
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.199
Keywords
This article is cited by
-
Sympathetic ophthalmia after 27-G pars plana vitrectomy
BMC Ophthalmology (2021)