Abstract
Aim
To determine whether there is an association between complement factor H (CFH) or LOC387715 genotypes and response to treatment with photodynamic therapy (PDT) for exudative age-related macular degeneration (AMD).
Methods
Sixty-nine patients being treated for neovascular AMD with PDT were genotyped for the CFH Y402H and LOC387715 A69S polymorphisms by allele-specific digestion of PCR products. AMD phenotypes were characterized by clinical examination, fundus photography, and fluorescein angiography.
Results
Adjusting for age, pre-PDT visual acuity (VA), and lesion type, mean VA after PDT was significantly worse for the CFH TT genotype than for the TC or CC genotypes (P=0.05). Post-PDT VA was significantly worse for the CFH TT genotype in the subgroup of patients with predominantly classic choroidal neovascular lesions (P=0.04), but not for the patients with occult lesions (P=0.22). For the LOC387715 A69S variant, there was no significant difference among the genotypes in response to PDT therapy.
Conclusions
The CFH Y402H variant was associated with a response to PDT treatment in this study. Patients with the CFH TT genotype fared significantly worse with PDT than did those with the CFH TC and CC genotypes, suggesting a potential relationship between CFH genotype and response to PDT.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is the leading cause of blindness in developed countries, with choroidal neovascularization (CNV; exudative AMD) responsible for 90% of this severe vision loss.1 Recently, a single nucleotide polymorphism (SNP; rs1061170) predicted to result in a coding variation (Y402H) in the complement factor H (CFH) gene on chromosome 1q32 was found to be strongly associated with AMD.2, 3, 4, 5 The presence of the CFH Y402H polymorphism correlates with both exudative6, 7 and advanced atrophic8 AMD, as well as AMD progression,9 but limited data are available evaluating AMD phenotypes or response to treatment with regard to CFH genotype.10, 11, 12, 13
The association of AMD with two distinct polymorphisms within chromosome 10q26 has identified this region as a second major locus contributing to AMD pathogenesis. The non-synonymous SNP rs10490924, predicted to result in a coding variation (A69S) within the hypothetical gene LOC387715, was found to confer an increased risk for development of AMD,14, 15 and this locus has been renamed ARMS2 (age-related maculopathy susceptibility gene 2). A second SNP in this region (rs11200638), located approximately 5.5 kb downstream of rs10490924 in the putative GC-rich promoter of the HTRA1 gene, is also associated with an increased risk of AMD.16, 17 LOC387715 and HTRA1 mRNA have been found in human retina, but it remains unclear if either of the polymorphisms in the 10q26 region (rs10490924 and rs11200638) is causally associated with AMD.
Photodynamic therapy (PDT) with verteporphin has played a key role in the treatment of AMD-related CNV over the past decade. Intravenous administration of the photosensitizer verteporphin, followed by activation with a non-thermal laser, initiates a photochemical reaction involving singlet oxygen and reactive oxygen intermediates that damage endothelial cells lining the CNV and leads to selective occlusion of these vessels.18 PDT is now increasingly being used in combination with other treatment modalities such as antibodies against vascular endothelial growth factor for exudative AMD.
Genotype–phenotype correlation studies of small cohorts have suggested that the AMD-associated CFH Y402H genetic variant may play a role in the type or size of neovascular complex that forms in exudative AMD.10, 11, 12 The purpose of this study was to evaluate the potential association between response to treatment for neovascular AMD with PDT and the CFH Y402H variant. We also examined one of the chromosome 10q polymorphic loci, LOC387715 A69S, for any relationship to treatment response.
Materials and methods
Patients and clinical examination
This study was approved by the Washington University Human Research Protection Office and the Barnes Retina Institute Study Center and was conducted in accordance with Health Insurance Portability and Accountability Act regulations. All participants were enrolled from the clinical offices of the Barnes Retina Institute and signed written informed consent prior to participation.
As part of a larger case–control study, mouthwash samples were collected from 69 patients with exudative AMD who had undergone treatment for a neovascular membrane with PDT with verteporphin alone, according to recommended standard procedures.19 AMD phenotypes were characterized by clinical examination, including dilated fundus exam, fundus photography, and fluorescein angiography. Fluorescein angiograms obtained upon initial presentation of active choroidal neovascular lesions were classified as either predominantly classic or occult. None of the lesions treated with PDT was classified as minimally classic. Angiograms were read independently by two retina specialists (MAB and RSA) masked to CFH genotype. Any discrepancies in lesion classification were openly adjudicated. Angiograms were obtained either digitally with a Zeiss fundus camera (Carl Zeiss Inc., Thornwood, NY, USA) and imaging software (OIS, Sacramento, CA, USA), or using film with a Zeiss FF4 fundus camera. Snellen visual acuity (VA) was recorded for all AMD subjects at initial presentation and at follow-up visits. For all calculations and comparisons, Snellen acuities were converted to logMAR values. These values were converted back to Snellen acuities for reporting the results.
DNA preparation and genotyping
Participants provided buccal tissue samples by expectorating into 50 ml conical tubes (Falcon; BD Biosciences, San Jose, CA, USA) after vigorously rinsing for 30 s with ∼20 ml Scope mouthwash (Procter & Gamble, Cincinnati, OH, USA). Genomic DNA was prepared from buccal cells using the Puregene mouthwash kit (Gentra Systems, Minneapolis, MN, USA) and quantified by absorbance at 260 nm (GeneQuant pro; GE Healthcare, Buckinghamshire, UK). Exon-9 of CFH was PCR-amplified using AmpliTaq Gold Universal PCR Master Mix (ABI, Foster City, CA, USA) and gene-specific primers located in intron-8 (5′-ctttgttagtaactttagttcgtcttcag) and intron-9 (5′-acaaggtgacataaacattttgcc). Similarly, exon-1 of LOC387715 was amplified using primers located in the 5′-untranslated region (5′-tgagtgagatggcagctgg) and intron-1 (5′-tccagctattcaaccagagg). For restriction fragment length analysis, CFH amplicons (443 bp) and LOC387715 amplicons (547 bp) were digested with Hsp92II (Promega, Madison, WI, USA) and PvuII (New England Biolabs, Ipswich, MA, USA), respectively, according to the manufacturers' instructions then visualized on 2.5% agarose gels stained with SYBR Gold (Molecular Probes, Invitrogen, Carlsbad, CA, USA).
Data analysis
Descriptive statistics for all demographic and clinical variables were calculated and comparisons were made using the t-test for means with continuous data (ie, age, VA, etc.) and the χ2 test for categorical data (ie, gender). Comparisons between genotypes were adjusted for multiple comparisons using the Bonferroni multiple comparison correction, and the reported P-values reflect this correction. The association between genotype and VA was assessed using generalized linear modelling techniques, with VA expressed in logMAR units, using the homozygous mutation (CC for CFH, and TT for LOC387715) as the basis of comparison. The post-treatment VA was modelled after adjustment for pretreatment acuity, age, genotype, and lesion type as these are known to be associated with either response to treatment or VA. Genotype was included in the model with a dummy variable for the homozygous candidate allele (ie, CC for CFH, TT for LOC387715) with the P-value associated with the coefficient indicating if post-treatment VA was influenced by the candidate allele (P⩽0.05 indicating a significant association).
Results
Sixty-nine patients with exudative macular degeneration who received treatment with PDT in one eye were enrolled in the study. Demographic information and characterization of AMD phenotypes are presented in Table 1.
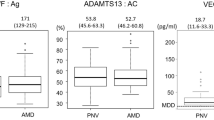
Table 2 displays the distribution of demographic and clinical phenotype data for the AMD patients according to CFH genotype. The at-risk CFH CC genotype was seen in 29.0% of PDT patients, and the overall frequency of the C allele in this population was 53.6%. Mean age and gender distribution were similar among the three CFH genotypes. The percentage of patients with predominantly classic lesions was significantly greater in the CFH CC group compared to the CFH TC and TT groups (P=0.003). The greatest linear dimension of the choroidal neovascular lesions did not differ by CFH genotype (P=0.74). There was no difference in the median number of treatments per month of follow-up among the CFH genotypes (P=0.79).
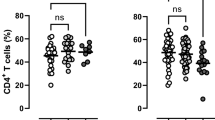
We examined the pre- and post-PDT VA for all eyes in the study by CFH genotype (Table 3). Mean pre-PDT VA was not significantly different among the CFH genotypes (P=0.12). To evaluate response to treatment with PDT by genotype, we examined post-PDT VA after adjusting for age, pre-PDT VA, and lesion type. We found that the mean post-PDT VA for the CFH TT genotype was significantly worse than post-PDT VA of the TC and CC genotypes (P=0.05).
The above regression approach assumes that the effect of lesion type is additive and does not interact with the other independent variables in the model. It is possible that the genotype, age, or pre-PDT VA may have different effects on post-PDT VA depending on the lesion type.20 Therefore, we examined response to PDT by CFH genotype in eyes with predominantly classic lesions (N=32) and eyes with occult lesions (N=37) independently (Table 3). In each case, our evaluation of post-PDT VA was adjusted for age and pre-PDT VA. For patients with predominantly classic lesions, mean pre-PDT VA was not different among the CFH genotypes (P=0.12), but mean post-PDT VA for the CFH TT genotype was significantly worse than for the CFH TC and CC genotypes (P=0.04). For patients with occult lesions, there was no significant difference in mean pre-PDT VA (P=0.51), or mean post-PDT VA (P=0.22) among the CFH genotypes.
Table 4 displays the distribution of demographic and clinical phenotype data for the AMD patients according to LOC387715 genotype. The at-risk LOC387715 TT genotype was seen in 21.8% of PDT patients, and the overall frequency of the T allele in this population was 42.8%. Mean age and gender distribution were similar among the three LOC387715 genotypes. There was no difference in the percentage of patients with predominantly classic lesions (P=0.47), the greatest linear dimension of the neovascular lesions (P=0.53), or the median number of treatments per month of follow-up (P=0.82) among the three LOC387715 genotypes.
We examined the pre- and post-PDT VA for all eyes in the study by LOC387715 genotype (Table 5). Mean pre-PDT VA was not significantly different among the LOC387715 genotypes (P=0.87). To evaluate response to treatment with PDT, we evaluated post-PDT VA, adjusting for age, pre-PDT VA, and lesion type, and found that mean post-PDT VA also is not significantly different among the LOC387715 genotypes (P=0.09).
We examined response to PDT by LOC387715 genotype in eyes with predominantly classic lesions (N=32) and eyes with occult lesions (N=37) independently (Table 5). For patients with predominantly classic lesions, mean pre-PDT VA (P=0.75) and mean post-PDT VA (P=0.54) were not different among the LOC387715 genotypes. For patients with occult lesions, there was no significant difference in mean pre-PDT VA (P=0.59) or mean post-PDT VA (P=0.08) among the LOC387715 genotypes.
Discussion
In our study population, we have identified a significant association between the CFH Y402H variant and response to treatment for neovascular AMD with PDT. While a small number of reports have correlated AMD clinical phenotypes with CFH Y402H genotype,10, 11, 12 with one study demonstrating a possible association between PDT response and CFH genotype,11 there are still few data available regarding such genotype–phenotype correlations.
The overall frequency of the higher risk CFH Y402H C allele in our population (53.6%) is similar to previous reports. We found a significant difference in the percentage of eyes in each CFH genotype group with predominantly classic lesions, consistent with our and other earlier reports,10, 11, 12 which found a higher percentage of predominantly classic lesions in the CFH CC group. In this study, we found no difference in lesion size according to CFH genotype, suggesting that any differences seen in response to PDT are independent of the size of the CNV.
Visual acuity at presentation was the worst in the lower risk CFH TT group (P=0.12), consistent with our previous studies.12, 13 Mean post-PDT VA declined 2.2 lines for both the CFH CC and TC genotypes, but fell 4.0 lines for the TT genotype. After correcting for age, pre-PDT VA, and lesion type, we found this difference in post-PDT VA to be significant (P=0.05). This is interesting because it suggests that patients without the higher risk CFH C allele fared worse with PDT than patients with the C allele. These results support the findings of Goverdhan et al11 who found VA loss after PDT to be greatest in their patients with the CFH TT genotype. The fact that post-PDT VA was significantly worse in the CFH TT group suggests that genetic factors may play a critical role in the efficacy of therapeutic interventions for exudative AMD. One possibility is that patients with the CFH TT genotype might develop CNV lesions that lack the presumed inflammatory changes associated with the C allele, and this actually makes them less susceptible to treatment with PDT. Interestingly, in our previous study examining response to intravitreal injection of the anti-vascular endothelial growth factor antibody bevacizumab, we found poorer post-treatment VA in AMD patients with the CFH CC genotype compared to the TC and TT genotypes.13 These results emphasize the different pharmacologic mechanisms used in the two therapies and may be related to alterations in local inflammatory mediators according to CFH genotype. When we evaluated post-PDT VA according to lesion type (predominantly classic vs occult), we found that the majority of the difference in post-PDT VA for the CFH TT group was due to eyes with predominantly classic lesions.
The overall frequency of the LOC387715 high-risk T allele in our population was 42.8%, consistent with previous reports. Phenotypic characteristics were very similar across the LOC387715 genotypes, with no significant difference seen in the percentage of patients with predominantly classic lesions, the greatest linear dimension of the lesion, or the number of treatments per month of follow-up. Initial VA was also very similar among the LOC387715 genotypes. Mean post-PDT VA declined 1.0 line for the LOC387715 TT genotype, 2.1 lines for the GT genotype, and 4.1 lines for the GG genotype. Similar to our findings with CFH, it was patients with no high-risk LOC387715 T allele that fared the worst with PDT treatment. In this case, however, when we controlled for age, pre-PDT VA, and lesion type, the difference between the post-PDT VAs for the LOC387715 genotypes did not reach statistical significance (P=0.08). Because the protein product of the LCO387715 gene has not been characterized, it is difficult to speculate on the meaning of this finding, but it is interesting that for LOC387715, like CFH, the lack of the at-risk allele tended to be associated with a poorer response to PDT. When we evaluated post-PDT VA according to lesion type, we found that the majority of this difference was due to patients with occult lesions. This is in contrast to the CFH data, in which the majority of the difference in post-PDT VA for the CFH TT group was driven by eyes with predominantly classic lesions.
This retrospective study was limited by the size of the patient cohort. In spite of this, we did identify significant differences in response to PDT among the CFH genotypes. We were not able to adequately assess the interaction of the CFH Y402H and LOC387715 A69S variants because the number of patients with each of the resulting nine genotypes was too small for meaningful statistical analysis. Further investigation with a larger patient cohort may allow for the evaluation of such gene interactions and their relationship to treatment response.
In summary, we have evaluated AMD clinical phenotypic characteristics and response to treatment with PDT with respect to the CFH Y402H and LOC387715 A69S variants. We found that patients with the CFH TT genotype fared worse with PDT than did patients with the CFH CC and TC genotypes. This difference was predominantly due to differences seen in patients with predominantly classic lesions. As further data are available regarding correlation of AMD-associated genotype and response to treatment, these data may be useful in helping tailor treatment for exudative macular degeneration.
References
Bressler NM, Bressler SB, Fine SL . Age-related macular degeneration. Surv Ophthalmol 1988; 32: 375–413.
Klein RJ, Zeiss C, Chew EY, Tsai J-Y, Sackler RS, Haynes C et al. Complement factor H polymorphism in age-related macular degeneration. Science 2005; 308: 385–389.
Edwards AO, Ritter III R, Abel KJ, Manning A, Panhuysen C, Farrer LA . Complement factor H polymorphism and age-related macular degeneration. Science 2005; 308: 421–424.
Haines JL, Hauser MA, Schmidt S, Scott WK, Olson LM, Gallins P et al. Complement factor H variant increases the risk of age-related macular degeneration. Science 2005; 308: 419–421.
Hageman GS, Anderson DH, Johnson LV, Hancox LS, Taiber AJ, Hardisty LI et al. A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc Natl Acad Sci USA 2005; 102: 7227–7232.
Souied EH, Levziel N, Richard F, Dragon-Durey M-A, Coscas G, Soubrane G et al. Y402H complement factor H polymorphism associated with exudative age-related macular degeneration in the French population. Mol Vis 2005; 11: 1135–1140.
Lau L-I, Chen S-J, Cheng C-Y, Yen M-Y, Lee F-L, Lin M-W et al. Association of the Y402H polymorphism in complement factor H gene and neovascular age-related macular degeneration in Chinese patients. Invest Ophthalmol Vis Sci 2006; 47: 3242–3246.
Postel EA, Agarwal A, Caldwell J, Gallins P, Toth C, Schmidt S et al. Complement factor H increases risk for atrophic age-related macular degeneration. Ophthalmology 2006; 113: 1504–1507.
Seddon JM, Francis PJ, George S, Schultz DW, Rosner B, Klein ML . Association of CFH Y402H and LOC387715 A69S with progression of age-related macular degeneration. JAMA 2007; 297: 1793–1800.
Wegscheider BJ, Weger M, Renner W, Steinbrugger I, März W, Mossböck G et al. Association of complement factor H Y402H gene polymorphism with different subtypes of exudative age-related macular degeneration. Ophthalmology 2007; 114: 738–742.
Goverdhan SV, Hannan S, Newsom RB, Luff AJ, Griffiths H, Lotery AJ . An analysis of the CFH Y402H genotype in AMD patients and controls from the UK, and response to PDT treatment. Eye 2007, e-pub ahead of print April 2007.
Brantley Jr MA, Edelstein SL, King JM, Apte RS, Kymes SM, Shiels A . Clinical phenotypes associated with the complement factor H Y402H variant in age-related macular degeneration. Am J Ophthalmol 2007; 144: 404–408.
Brantley Jr MA, Fang AM, King JM, Tewari A, Kymes SM, Shiels A . Association of complement factor H and LOC387715 genotypes with response of exudative age-related macular degeneration to intravitreal bevacizumab. Ophthalmology 2007; 114: 2168–2173.
Jakobsdittr J, Conley YP, Weeks DE, Mah TS, Ferrell RE, Gorin MB . Susceptibility genes for age-related macular degeneration on chromosome 10q26. Am J Hum Genet 2005; 77: 389–407.
Rivera A, Fisher SA, Fritsche LG, Keilhauer CN, Lichtner P, Meitinger T et al. Hypothetical LOC387715 is a second major susceptibility gene for age-related macular degeneration, contributing independently of complement factor H to disease risk. Hum Mol Genet 2005; 14: 3227–3236.
DeWan A, Liu M, Hartman S, Zhang SS-M, Liu DTL, Zhao C et al. HTRA1 promoter polymorphism in wet age-related macular degeneration. Science 2006; 314: 989–992.
Yang Z, Camp NJ, Sun H, Tong Z, Gibbs D, Cameron DJ et al. A variant of the HTRA1 gene increases susceptibility to age-related macular degeneration. Science 2006; 314: 892–893.
Virgili G, Do DV, Bressler NM, Menchini U . New therapies for neovascular age-related macular degeneration: critical appraisal of the current evidence. Acta Ophthalmol Scand 2007; 85: 6–20.
Verteporfin Roundtable Participants. Guidelines for using verteporfind (Visudyne) in photodynamic therapy for choroidal neovascularization due to age-related macular degeneration and other causes: update. Retina 2005; 25: 119–134.
Bressler NM, Arnold J, Benchaboune M, Blumenkranz MS, Fish GE, Gragoudas ES et al. Verteporfin therapy of subfoveal choroidal neovascularization in patients with age-related macular degeneration: additional information regarding baseline lesion composition's impact on vision outcomes—TAP report no. 3. Arch Ophthalmol 2002; 120: 1443–1454.
Acknowledgements
This study was supported by NEI Grant EY012284, NEI Core Grant 5 P30 EY02687, and a grant from Research to Prevent Blindness to the Department of Ophthalmology and Visual Sciences at Washington University School of Medicine. No conflicting relationship exists for any author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brantley, M., Edelstein, S., King, J. et al. Association of complement factor H and LOC387715 genotypes with response of exudative age-related macular degeneration to photodynamic therapy. Eye 23, 626–631 (2009). https://doi.org/10.1038/eye.2008.28
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.28
Keywords
This article is cited by
-
Association of an age-related maculopathy susceptibility 2 gene variant with the 12-month outcomes of intravitreal aflibercept combined with photodynamic therapy for polypoidal choroidal vasculopathy
Japanese Journal of Ophthalmology (2019)
-
A prospective multicenter study on genome wide associations to ranibizumab treatment outcome for age-related macular degeneration
Scientific Reports (2017)
-
The role of glial cells and the complement system in retinal diseases and Alzheimer’s disease: common neural degeneration mechanisms
Experimental Brain Research (2014)
-
The significance of the complement system for the pathogenesis of age-related macular degeneration — current evidence and translation into clinical application
Graefe's Archive for Clinical and Experimental Ophthalmology (2011)
-
Genetic Predictors of Response to Photodynamic Therapy
Molecular Diagnosis & Therapy (2011)