Abstract
Purpose
To evaluate the adequacy of common disinfection regimens for disposable tonometer tips and assess if disinfection of reusable prisms or the use of disposable tips is preferable.
Methods
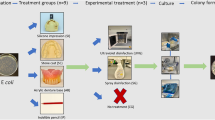
We used disposable tonometer tips, using the same material and tip diameter of standard Goldmann tonometer prism. Strains of Pseudomonas aeruginosa, Staphylococcus aureus, Bacillus subtilisand Candida albicanswere tested according to the European standard guidelines for disinfectants test. Antimicrobial effectiveness of the following disinfection practices has been assessed: dry wipe, Minuten wipes (Alpro®), soaking in 3% hydrogen peroxide, 0.5% benzalkonium chloride, and 0.5% Pantasept® for 1, 5, and 15 min. All tests have been performed three times and all conditions tested in duplicate.
Results
Dry wiping and 1 min soak in 3% hydrogen peroxide were ineffective on all microrganisms. Minuten wipes, 1 min soak in 0.5% benzalkonium chloride or 3% hydrogen peroxide were ineffective on B. subtilis. 0.5% Pantasept® soak was effective in 1 min for all microrganisms tested, whereas 3% hydrogen peroxide and 0.5% benzalkonium chloride soaks were effective when performed for at least 5 min. B. subtiliswas the most resistant organism to disinfectant regimes at 1 min time.
Conclusions
Results of our study demonstrate a relative disinfection efficacy for the different evaluated regimens, provided that correct exposure times are adopted for the chosen disinfectants, a condition difficult to ensure in a busy clinic setting. We conclude that disposable prism tonometry provides a safe alternative to Goldmann tonometry.
Similar content being viewed by others
Introduction
The ophthalmologist’s office is an environment with significant potential for the transmission of infections. Pathogens are regularly introduced into the office by patients with systemic or ocular infections and the eye is particularly susceptible to infection with Gram-negative bacilli, adenoviruses, Herpes simplex and fungi, transferred by contaminated ophthalmic instruments.1
Moreover, the acquired immunodeficiency syndrome (AIDS) epidemic and the isolation of human immunodeficiency virus (HIV) from human tears,2 corneas3 and contact lenses4 have focused attention on the infected patient as a source of transmission of disease.
The most frequently reported infections transmitted by contaminated ophthalmic equipment have been those with adenoviruses5, 6, 7 but in theory, a number of diseases could be spread in the same manner. Whereas some ocular infections, such as adenoviral conjunctivitis, are self-limiting and their long-term sequelae are very infrequent, some agents are responsible for sight threatening courses. Among these, bacteria and Acanthamoeba have become much more prevalent since the advent of widespread soft contact lens wear and can be responsible for infection cases enough severe to require penetrating keratoplasty or even enucleation as treatment.8, 9
Hepatitis B (HBV) and C (HCV) viruses are far more prevalent in the population than HIV10, 11 and can cause chronic hepatitis. It has been demonstrated that hepatitis B infection can be transmitted after infectious exposure of the ocular surface alone.12
The isolation of hepatitis C virus from tear fluid and aqueous humour13, 14, 15, 16 raises the possibility of transfer of hepatitis C virus during the course of an ophthalmologic examination, that is, Goldmann tonometry and trial contact lens fitting.17
Possible risk of horizontal transmission of vCJD via contact tonometry has given further cause for concern.18, 19, 20, 21
Tonometer heads used for measuring intraocular pressure come into direct contact with the cornea and so pose a high risk of cross-infection.1
Tonometer tips have been frequently identified as major vehicles of infection.22, 23 Prevention of all infections is desirable, but it is especially critical in the case of HIV and hepatitis C virus because it is currently not possible to immunize against these viruses.
Good hygienic practice, including hand washing, is the logical first step in reducing the spread of infections and is good medical practice to disinfect any office equipment that comes in direct contact with patients.
Failure to efficiently disinfect Goldmann tonometer tips could represent a possible mode of infection transmission.17
A review of the literature reveals that many disinfection methods are suggested for tonometric prisms, even if it is not always clear which organisms are eliminated and which may be left behind with every single regimen.24
Chemical disinfectants have variable ability to eradicate pathogenic bacteria such as Pseudomonas aeruginosa, Serratia marcescens, and Staphylococcus aureus.25, 26, 27, 28 HIV has been proved to be susceptible to most chemical cleaning regimens while these agents are differently effective in their ability to kill fungal spores, prions and Acanthamoeba. Actually, data from literature report some problems concerning disinfectant efficacy (appropriate concentration and exposure times, in vitro and in vivo different interactions between tested strains and germicides) even considering the consequent tonometer prism damages and iatrogenic corneal deepithelialization and stromal opacification caused by incomplete removal of disinfectant from tonometer tip.7, 29, 30, 31, 32 Consequently, it is very difficult to find an ideal chemical disinfecting system for tonometer prism easily and safely applicable in the ophthalmologist’s office.
The Centers for Disease Control and Prevention (CDC) and the American Academy of Ophthalmology (AAO) have established guidelines for office disinfection of trial contact lenses and tonometers.33
The aim of this study was to evaluate the adequacy of some cleansing and disinfection regimens recommended by tonometer manufacturers and by the guidelines of the CDC and the AAO, using sterile disposable tonometer tips contaminated on their contact surfaces with different microrganisms belonging to the most frequent species responsible for corneal infections. This will enable us to assess risk for horizontal transmission by contact tonometry and to address the question whether a stringent decontamination of reusable prisms or use of sterile disposable tips or shields should be preferred.
Materials and methods
Disposable sterile tonometer tips (TONOJET L900, Luneau, France) made from clear acrylic plastic but with the same tip diameter as the standard Goldmann tonometer prism were used.
Four different strains were used for the test: P. aeruginosa ATCC 15 442, S. aureus ATCC 6538, Bacillus subtilis ATCC 6633 and Candida albicans ATCC 10231. The strains were grown on Mueller–Hinton and Sabouraud agar plates, respectively, at 35°C for 48 h. Isolated colonies were suspended in sterile phosphate-buffered saline (PBS) to an optical density corresponding to 108 colony forming units per ml for each organism to be tested according to the European Committee for Standardization (ECS)34 for disinfectants testing on surfaces. Serial dilutions of the inoculum were made in 0.85% saline and plated in duplicate onto Mueller–Hinton and Sabouraud agar to check for inoculum size and purity of suspensions.
Antibacterial and antifungal effectiveness of the following disinfection practices was evaluated: (a) wiping by towels moistened with <1% tert. alkylamines and quat. alkyl-ammoniumpropionate in 55% ethanol, n−/isopropanol mixture (Minuten wipes, Alpro®), according to the instructions for use provided by the manufacturer; (b) soaking in 3% hydrogen peroxide for 1, 5, and 15 min; (c) soaking in 0.5% benzalkonium chloride for 1, 5, and 15 min; (d) soaking in 0.5% glutaraldheyde (Pantasept®, Haag-Streit International) for 1, 5, and 15 min. No treatment and dry wiping (simple cleaning) were used as growth control procedures.
The tests were performed by the following procedure: (i) the tonometer tip was soaked for 10 s, corresponding to the average tonometry time, into the suspension of the organism under study; (ii) the entire tonometer was soaked into the disinfectant solution under test for 1, 5, and 15 min or, alternatively, the tonometer tip was wiped for 10 s with dry or Minuten wipes (according to the instructions of the manufacturer); (iii) the tonometer was rinsed under a moderate flow of sterile saline solution for 5 s, then dried twice with a sterile paper towel; (iv) the tonometer tip was pressed firmly onto the surface of a Mueller Hinton or Sabouraud agar plate for 10 s; (v) the plates were incubated at 37°C and examined for growth after 24 and 48 h.
Growth of the four microbial species was assessed through visual inspection of the plates evaluating the presence of the expected colonies at the inoculation points on the agar surface. The microbial species could be easily differentiated by the characteristic pigmentation of the colonies of P. aeruginosa and S. aureus, by the large, feathery and spreading appearance of those of B. subtilis and by the white, creamy, yeast-like appearance of those of C. albicans. Morphological colony identification was confirmed by Gram staining. Only colonies showing the expected macroscopical and microscopical characters were considered.
All the tests were performed three times and all conditions were tested in duplicate.
Results
The results of the disinfection tests are summarized in Table 1.
From our results, the 10 s wiping by Minuten wipes was effective on all the strains tested with the only exception of B. subtilis. Soaking in Pantasept® completely eliminated in 1 min all the contaminating microorganisms, whereas 0.5% benzalkonium chloride after 1 min soaking was effective on all the strains but B. subtilis, which required 5 min for disinfection. Hydrogen peroxide 3% solution soaking was effective only when the disinfection procedure was performed for at least 5 min, regardless the strain tested. Dry wiping cleaning was ineffective to eliminate the contamination.
Discussion
In ophthalmology, the gold standard for intraocular pressure measurement remains the Goldmann tonometry. Goldmann applanation tonometry is performed on most patients who are examined in the ophthalmologist’s office. A recent study estimated that tonometry is performed on 122 million patients annually35 and it is well known that some diseases, for example adenovirus keratoconjunctivitis, can be unintentionally transmitted during this investigation.7 Tonometer prisms, then, may represent a prime vehicle for cross-infections. Furthermore, approximately 70 million people throughout the world wear contact lens, often for extended wear, so it is not surprising that contact lens related microbial keratitis is increasingly turning to be a worldwide Public Health problem.8 Actually, Pseudomonas spp. and Staphylococcus spp. are the most commonly isolated microbes in corneal infections related to contact lens wear, followed by protozoa (for example, Acanthamoeba spp.) and rarely fungi.8
Although most bacteria are sensitive to brief exposures to many common disinfectants,36 viruses, especially those without a lipid envelope, can be more resistant:37 for example, herpes simplex virus can live up to 8 h when kept moist38 and adenovirus can survive for 7–14 days at room temperature on a dry surface.39
The CDC’s recommendations suggest to wipe the tonometer tip and then disinfect it with a 5 min soak in either a 1 : 10 dilution of sodium hypochlorite (household bleach), 3% hydrogen peroxide, or 70% isopropyl alcohol. The AAO, in conjunction with the National Society for the Prevention of Blindness and the Contact Lens Association of Ophthalmologists, has adopted these recommendations and added the option of simply wiping the tip with a 70% isopropyl alcohol swab.33
Five-minute soaks in the disinfectants hydrogen peroxide, iodophor, and sodium hypochlorite were found to be effective against adenovirus.40 However, one study41 has demonstrated that hepatitis B virus DNA is still detectable by polymerase chain reaction on tonometer tips after disinfection with several methods, including 70% isopropyl wipe, 70% ethanol wipe, 10 min 500–ppm chlorine soak, and 10 min 1% glutaraldehyde soak, while a simple soap and water wash removed all detectable hepatitis B virus DNA.
Of potential concern is the finding that the very common method of using a 70% isopropyl alcohol wipe for disinfection decontaminated only half of the tonometer tips tested.24
The wipe disinfection methods are certainly more convenient than the soaking methods, both in terms of disinfection time and reduced risks of damaging the instrument. Treating only the tip of the tonometer instead of the entire prism, the damages to the prism that have been observed in extended soaking regimens42, 43, 44 could be prevented, but the reduced contact time may not be adequate for complete disinfection.
When soaking methods are used, it is important to rinse the tonometer tip to eliminate residues of bleach or hydrogen peroxide or allow the alcohol to evaporate before applanation to avoid iatrogenic corneal deepithelialization and stromal opacification.29, 30
Adherence to these guidelines should greatly reduce the spread of infections.
However, none of the foregoing disinfection techniques are routinely effective against Acanthamoeba, that is, killed by 3% hydrogen peroxide but only after several hour soaking for cleaning contact lenses45and 2 h soaking for tonometer tips.24 Although this ocular infection agent is less common than bacteria or virus (the incidence has been estimated between one in 10 000 to two in 1 million contact lens wearers5), it should not be disregarded because of close association with contact lens wear and potentially devastating sequelae. However, even if there are various disinfectant regimens effective against Acanthamoeba (like stronger solutions of available chlorine) chemical alterations to tonometer prism and iatrogenic corneal deepithelialization and stromal opacification are to be considered.29, 30, 31, 32 Hence, in cases of suspected Acanthamoeba keratitis (which would include any red, painful eye), it may be wise to have a tonometer prism that can be set aside for the necessary disinfection time or to use disposable prism or silicone tonometer shields instead. Such shields have been used to prevent the spread of infection and as an alternative to repeated chemical disinfection of the tonometer prism.46, 47 In any case, the soaking time able to kill Acanthamoeba is impractical for a device that is in constant use in the office.
The results of our study demonstrate a variety of disinfection activity by the different regimens evaluated. The 0.5% glutaraldehyde solution, recommended by tonometer manufacturers, was quickly effective on all the strains under study. Minuten wipes failed to eliminate B. subtilis contamination in 10 s, corresponding to the contact time suggested by the manufacturer’s instructions. Antimicrobial disinfection was not achieved before 5 min with 3% hydrogen peroxide soaks, regardless the tested strain. Also the benzalkonium chloride 0.5% solution requested 5 min soaking to decontaminate from B. subtilis the tonometer tips, confirming that, under our experimental conditions, B. subtilis was the most resistant organism.
Exposition time to the disinfecting agent is hence of capital importance for achieving an effective result and differences in the ability to resist to disinfection for the different microbial species must be taken into account.
Inadequate disinfection of reusable prisms carries the risk of cross-transmission of bacterial and viral conjunctivitis.5 Furthermore, the ever-increasingly busy nature of the clinics makes it difficult to ensure adequate disinfection of the Goldmann prism after every use. In a busy clinic setting, IOP of patients need to be checked at short intervals and it is difficult to ensure Goldmann prism disinfection for the recommended minimum time after every use; in any case, the very common method of using 70% isopropyl alcohol, that is, wiping, decontaminated only half of the tonometer tips tested.24 Moreover, obtaining reliable pressure readings with prisms damaged by disinfectant regimens is questionable.32
All these considerations should induce ophthalmologists to prefer the use of disposable tonometer tips in their every day clinical practice to eliminate any risk of cross-infections.
Recent studies48, 49, 50 demonstrate the accuracy and reliability of disposable prism tonometry when compared to the gold standard of Goldmann tonometry. Inferences from these studies indicate within the advantages of disposable prisms, a short learning curve, ease of use, and reproducibility of results. The main disadvantage of disposable prisms is the cost factor, but a widespread use would greatly reduce their price.
We conclude that disposable prism tonometry provides a reliable, effective, and safe alternative to Goldmann tonometry in routine clinical practice with the advantages of eliminating the need for chemical disinfection and eliminating the risk of cross-infection.
All these considerations are applicable not only to tonometer prisms, but also to any ophthalmic devices which have a direct contact with the ocular surface of patients and whose disinfection is required during routinary clinical practice.
References
Dart CR . Audit of decontamination procedures for specialist ophthalmic equipment. J Hospital Infection 1995; 29: 297–300.
Fujikawa L, Salahuddin S, Ablashi D, Palestine AG, Masur H, Nussenblatt RB et al. HTLV-III in the tears of AIDS patients. Ophthalmology 1986; 93: 1479–1481.
Cantrill H, Henry K, Jackson B, Erice A, Ussery F, Balfour Jr H . Recovery of human immunodeficiency virus from ocular tissues in patients with acquired immune deficiency sydrome. Ophthalmology 1988; 95: 1458–1462.
Tervo T, Lahdevirta J, Vaheri A, Valle S, Suni J . Recovery of HTLV-III from contact lenses. Lancet 1986; 1: 379–380.
Koo D, Bouvier B, Wesley M, Courtright P, Reingold A . Epidemic keratoconjunctivitis in a university medical center ophthalmology clinic: need for re-evaluation of the design and disinfection of instruments. Infect Control Hosp Epidemiol 1989; 10: 547–552.
Warren D, Nelson K, Farrar J, Hurwitz E, Hierholzer J, Ford E et al. A large outbreak of epidemic keratoconjunctivitis: problems in controlling nosocomial spread. J Infect Dis 1989; 160: 938–943.
Centers for Disease Control and Prevention. Epidemic keratoconjunctivitis in an ophthalmology clinic of California. MMWR 1990; 39: 598–601.
Giese MJ, Weissman BA . Contact lens associated corneal infections. Where do we go from here? Clin Exp Optom 2002; 85: 141–148.
Schaumberg D, Snow K, Dana M . The epidemic of acanthamoeba keratitis: where do we stand? Cornea 1998; 17: 3–10.
Robert L, Chamberland M, Cleveland J . Investigations of patients of health care workers infected with HIV: The centers for disease control and prevention database. Ann Intern Med 1995; 122: 653–657.
Recommendations for follow up of health care workers after occupational exposure to hepatitis C virus. MMWR 1997; 45: 603–606.
Bond W, Petersen N, Favero M, Ebert J, Maynard J . Transmission of type B viral hepatitis via eye inoculation of a chimpanzee. J Clin Microbiol 1982; 15: 533–534.
Shimazaki J, Tsubota K, Fukushima Y, Honda M . Detection of hepatitis C virus RNA in tears and aqueous humor. Am J Ophthalmol 1994; 118: 524–525.
Feucht HH, Polywka S, Zollner B, Laufs R . Greater amount of HCV-RNA in tears compared to blood. Microbiol Immunol 1994; 38: 157–158.
Feucht HH, Zollner B, Schroter M, Altrogge H, Laufs R . Tear fluid of hepatitis C virus carriers could be infectious. J Clin Microbiol 1995; 33: 2202–2203.
Mendel I, Muraine M, Riachi G, el Forzli F, Bertin C, Colin R et al. Detection and genotyping of the hepatitis C RNA in tear fluid from patients with chronic hepatitis C. J Med Virol 1997; 51: 231–233.
Segal WA . Disinfection of Goldmann tonometers after contamination with hepatitis C virus. Am J Ophthalmol 2001; 131: 184–187.
Davanipour Z, Alter M, Sobel E, Asher D, Gajdusek DC . Creutzfeldt-Jakob disease: possible medical risk factors. Neurology 1985; 35: 1483–1486.
Walia JS . Possible iatrogenic transmission of Creutzfeldt-Jakob disease via tonometer tips: a review of the literature. Optometry 2001; 72: 649–652.
Amin SZ, Smith L, Luthert PJ, Cheetham ME, Buckley RJ . Minimising the risk of prion transmission by contact tonometry. Br J Ophthalmol 2003; 87: 1360–1362.
Lim R . Retention of corneal epithelial cells following goldmann tonometry:implications for CJD risk. Br J Ophthalmol 2003; 87: 583–586.
Murrah W . Epidemic keratoconjunctivitis. Ann Ophthalmol 1988; 20: 36–38.
Colon LE . Keratoconjunctivitis due to adenovirus type 8: report on a large outbreak. Ann Ophthalmol 1991; 23: 63–65.
Smith CA . Disinfection of tonometers and contact lenses in the office setting: Are current techniques adequate? Am J Ophthalmol 1999; 127: 77–84.
McLaughlin W, Hallberg K, Tuovinen O . Chemical inactivation of microorganisms on rigid gas permeable contact lenses. Optom Vis Sci 1991; 68: 721–727.
Keeven J, Wrobel S, Portoles M, DeCicco B . Evaluating the preservative effectiveness of RGP lens care solutions. CLAO J 1995; 21: 238–241.
Rosenthal RA, Stein JM, McAnally CL, Schlech BA . A comparative study of the microbiologic effectiveness of chemical disinfectants and peroxide-neutralizer systems. CLAO J 1995; 21: 99–110.
Parment P, Colucci B, Nystrom B . The efficacy of soft contact lens disinfection solutions against Serratia marcescens and Pseudomonas aeruginosa. Acta Ophthalmol Scand 1996; 74: 235–237.
Soukiasian SH, Ardouriun GK, Weiss JS, Kachadoorian HA . A complication from alcohol swabbed tonometer tips. Am J Ophthalmol 1988; 105: 424–425.
Levenson J . Corneal damage from improperly cleaned tonometer tips. Arch Ophthalmol 1989; 107: 1117.
Maldonado MJ . Corneal epithelial alterations resulting from use of chlorine-disinfected contact tonometer after myopic photorefractive keratectomy. Ophthalmology 1998; 105 (8): 1546–1549.
Kniestedt C, Sturmer J, Stamper RL . Clinical alert: damage to Goldmann applanation tonometer tips. Acta Ophthalmol Scand 2005; 83 (1): 129–130.
Lichter P . Controlling risks of the possible transmission of human immunodeficiency virus. Ophthalmology 1989; 96: 1.
European Standard WI 216028, European Committee for Standardization. Chemical disinfectants and antiseptic—Quantitative surface test for the evaluation of bactericidal and/or fungicidal activity disinfectants used in food, industrial, domestic and institutional areas- Test method without mechanical action and requirements. C.E.N September 1998; 21.
MicroScientific Industries Inc. Survey (November), Palatine, IL. 1996.
Dychdala G . Antiseptics and disinfectants. In: S. Block (ed). Disinfection, sterilization, and preservation. Lea and Febiger: Philadelphia, 1991.
Prince H, Prince D, Prince R . Principles of viral control and transmission. In: S. Block (ed). Disinfection, sterilization, and preservation. Lea and Febiger: Philadelphia, 1991.
Ventura L, Dix R . Viability of herpes simplex type 1 on the applanation tonometer. Am J Ophthalmol 1986; 103: 48–52.
Hara J, Okamoto S, Minekawa Y, Yamazaki K, Kase T . Survival and disinfection of adenovirus type 19 and enterovirus 70 in ophthalmic practice. Jpn J Ophthalmol 1990; 34: 421–427.
Threlkeld AB, Froggott JW, Schein OD, Forman MS . Efficacy of a disinfectant wipe method for the removal of adenovirus 8 from the tonometer tips. Ophthalmology 1993; 100: 1841–1845.
Su C, Bowden S, Fong L, Taylor H . Current tonometer disinfection may be inadequate for hepatitis B virus. Arch Ophthalmol 1994; 112: 1406–1407.
Chronister CL . Effects of disinfecting solutions on tonometer tips. Optom Vis Sci 1990; 67: 818–821.
Lingel NJ . Effects of disinfecting solutions recommended by the Centers for Disease Control on Goldmann tonometer biprisms. J Am Optom Assoc. 1992; 63: 43–48.
Chronister CL . Structural alteration of tonometer tips after repeated swabbing with disinfectants. Optom Vis Sci 1994; 71: 290–292.
Silvany R, Dougherty J, McCulley J, Wood T, Bowman R, Moore M . The effect of currently available contact lens disinfection systems on Acanthamoeba castellanii and Acanthamoeba polyphaga. Ophthalmology 1989; 97: 286–290.
Hodkin M, Pavilack M, Musch D . Pneumotonometry using sterile single-use tonometer covers. Ophthalmology 1992; 99: 688–695.
Maldonado M, Rodriguez-Galieter A, Cano-Parra J, Menezo J, Diaz-Llopis M . Goldmann applanation tonometry using sterile disposable silicone tonometer shields. Ophthalmology 1996; 103: 815–821.
Desai SP, Sivakumar S, Fryers PT . Evaluation of a disposable prism for applanation tonometry. Eye 2001; 15: 279–282.
Kim P, Lertsumitkul S, Clark M, Gardner L, Macken . Accuracy of the tonosafe disposable tonometer head compared to the goldmann tonometer alone. Clin Exp Ophthalmol 2004; 32: 364.
Salvi SM . Use of disposable prism tonometry in routine clinical practice. Eye 2004; 1–4.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing Interest: The authors have no financial interest in any of the products mentioned
Rights and permissions
About this article
Cite this article
Cillino, S., Casuccio, A., Giammanco, G. et al. Tonometers and infectious risk: myth or reality? Efficacy of different disinfection regimens on tonometer tips. Eye 21, 541–546 (2007). https://doi.org/10.1038/sj.eye.6702269
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702269
Keywords
This article is cited by
-
Hygiene in der Augenarztpraxis
Der Ophthalmologe (2016)
-
Reliability of tonosafe disposable tonometer prisms: clinical implications from the Veterans Affairs Boston Healthcare System Quality Assurance Study
Eye (2011)
-
Minimal cross-infection risk through Icare rebound tonometer probes: a useful tool for IOP-screenings in developing countries
Eye (2010)
-
Bacterial contamination of the disposable prism holder during routine tonometry for intraocular pressure
Eye (2009)