Abstract
Purpose
To determine the incidence of cataract following intravitreal triamcinolone (IVTA) for diabetic macular oedema.
Methods
Prospective, non-randomised, interventional cohort case series. A total of 27 eyes of 27 patients with diabetic macular oedema received an intravitreal injection of 4 mg (0.1 ml) of triamcinolone acetonide inferotemporally through the pars plana under direct vision. In 20 patients the fellow eye served as control, whereas seven patients had both eyes injected (not simultaneously). Seven patients had a repeat (second) injection in the same eye. The main outcome measures were cataract and intraocular pressure (IOP) rise of at least 5 mmHg (IOP responder).
Results
The mean follow-up time was 18.9 months (range 13–29 months). A total of 22 (81%) of 27 eyes developed cataract during the follow-up period, of which 20 (74%) were posterior subcapsular in nature. None of the 20 uninjected fellow eyes developed posterior subcapsular cataract. Mean time to cataract formation was 16.2 months. In the seven patients who had both eyes injected, mean time to cataract formation was 16.5 and 17.1 months in the first and second eye, respectively. Mean time to cataract formation in seven eyes receiving a repeat second injection was 17.9 months. There was no significant difference in cataract formation between IOP responders (85%) and non-responders (79%) (P=1.00, Fisher's exact test). Uneventful cataract surgery was performed in six eyes of five patients.
Conclusion
This study demonstrates that given appropriate long-term follow-up, the majority of patients, even after a single IVTA injection, will go on to develop cataract, of which posterior subcapsular will be by far the most common.
Similar content being viewed by others
Introduction
Intravitreal triamcinolone (IVTA) is now a well-established treatment for diabetic macular oedema both with1, 2, 3 and without 4, 5 prior macular laser treatment.
Since June 2002, we have been using IVTA in the treatment of diabetic macular oedema.6, 7 A well-known complication of steroid usage is cataract formation and in particular posterior subcapsular cataract (PSC).8 This study reports the results of clinical observation on a cohort of patients who had IVTA injected to manage diabetic macular oedema in phakic eyes.
Materials and methods
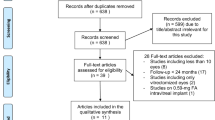
The records of all patients treated with IVTA for diabetic macular oedema between June 2002 and April 2005 were examined. A total of 30 eyes of 30 patients were identified. Of which three patients had type I and 27 had type II diabetes mellitus. The following parameters were recorded before and following treatment; LogMAR best-corrected visual acuity, corrected reading ability, lens status (clinical examination by slit-lamp following dilation), intraocular pressure, and central macular thickness using Ocular Coherence Tomography (Stratus/Zeiss OCT III), when this instrument was introduced into our department. Following treatment, patients were reviewed at 1 week, 1 month, 3 months, and at 3-monthly intervals following this.
Only 27 patients were included in the analysis as one patient had died, one was lost to follow-up at 3 months and one had cataract formation that was inconclusive from the medical records.
In 20 patients the fellow eye served as control, while seven patients had both eyes injected (not simultaneously). Seven patients had a repeat (second injection) in the same eye. Where a patient had both eyes injected, only the first injected eye was included in the analysis.
Informed consent was obtained from each patient. The eye was injected with 0.1 ml (4 mg) of triamcinolone acetonide (Kenalog 40; Bristol-Myers Squibb). The method of injection is as in our previous papers.6, 7
Results
The mean age of the patients was 67. 6 years at injection, with a range of 32–80 years. A total of 22 (81%) of 27 eyes developed significant cataract, with 20 (74%) of the 27 eyes developing PSC. Five (19%) of 27 eyes did not develop cataract during the follow-up period (Figure 1). One patient was lost to regular follow-up 3 months postinjection, but had developed a dense white cataract when they were next seen (17 months postinjection). One patient developed cataract (between 12 and 15 months postinjection) and went on to have cataract surgery but the case notes did not state the type of cataract.
None of the 20 uninjected fellow eyes developed PSC or other significant cataract. The time to first documentation of significant cataract was 16.2 months, with a range of 3–29 months. A total of 13 eyes showed a significant IOP rise (defined as an IOP rise ⩾5 mmHg) on at least one postinjection visit, whereas 14 eyes did not. There was no significant difference in cataract formation between IOP responders (85%) and non-responders (79%) (P=1.00, Fisher's exact test).
In the seven patients who had a repeat (second) injection in the same eye, mean time to second injection was 10.4 months, with a range of 4–16 months. Time to first documentation of significant cataract (‘Significant cataract’ - cataracts observed in this study considered to have a significant effect on vision in the absence of macular pathology) was 17.9 months from first injection. This is actually a longer average time than those eyes that received a single injection (16.2 months), perhaps indicating that it is the first injection that is the most cataractogenic.
In the seven patients who had both eyes injected (not simultaneously), six of seven second eyes developed PSC. Mean time to cataract formation in the second injected eye was not significantly different at 16.5 months, whereas in the first injected eye it was 17.1 months.
Six (22%) of 13 IOP responders developed raised IOP considered to require treatment. In all cases, the IOP was adequately controlled with topical glaucoma medication, with some patients requiring oral acetazolamide for a short period of time. Four (67%) of these six eyes developed PSC. The remaining two eyes did not develop cataract. The mean time to cataract formation in the four raised IOP responder eyes requiring treatment was 14.25 months (SD=7.0 months). Twenty-one (78%) of the 27 eyes did not develop raised IOP requiring treatment. Sixteen (76%) of these 21 eyes developed PSC. Time to cataract formation in these eyes was 17.7 months (SD=7.6 months). There was no significant difference in cataract formation between IOP responders requiring treatment (67%) and those not requiring treatment (76%) (P=0.63, Fisher's exact test).
The only other complication of IVTA injection was in a warfarinised patient who developed a subconjunctival haematoma, which eventually required surgical excision.9
Discussion
Formation of PSC is a well-known side effect of corticosteroids, whether administered by topical, systemic,8 or intravitreal route.13
To the best of our knowledge, previous studies from other authors investigating the role of IVTA in the treatment of diabetic macula oedema have followed patients for a relatively short time only, with mean follow-up times varying from 33 to 11.7 months.11 Consequently, this has not given investigators the opportunity to identify the long-term sequalae following IVTA, in particular, significant cataract formation.
Some studies report no cataract formation 6 2 and 104 months post-IVTA. One study with a 3-month follow-up reports cataract formation in 3% of patients.3 Studies with a 6-months follow-up report varying rates of cataract formation. 3.8,10 6.25,1 6.711 and 17%,12 all much lower than in our prospective case series. One paper13 found that 24% of eyes treated with IVTA developed cataract by 2 years, but this was when IVTA was used as a treatment for ARMD and not diabetic macular oedema. PSC, even at an early stage, can be very detrimental to visual function and can render OCT scanning ineffective. This is important as OCT is used to monitor central macular thickness and architecture, as well as to determine the need for further treatment. We have noticed that early PSC results in poor-quality OCT scans.
One weakness of this study is that cataracts were graded without the use of any classification system, such as the LOCS system. The cataracts were graded by any one of the three authors. However, all PSCs observed in this study were considered to have the potential to have a significant effect on vision (Figure 2).
We found no significant difference in cataract formation between IOP responders (85%) and non-responders (79%). This contradicts the findings of Gillies et al,14 who found a significant difference in cataract formation in non-diabetic eyes between IOP responders (51%) and non-responders (3%) after 2 years. We therefore do not support the view that PSC is unlikely to develop in eyes that do not experience elevated IOP after IVTA. As we have not found an association between IOP and PSC, the mechanisms for development of steroid-related cataract and raised IOP are likely to be different in diabetic eyes.
One could postulate that the high rate of cataract in our series is owing to our injection technique but this is unlikely, as we have followed a standardised protocol for IVTA injection.1
It is interesting to note that IVTA is being used as a primary treatment for diabetic macular oedema4, 5 and that The National Eye Institute, US, is performing a randomised controlled trial comparing macular laser treatment vs IVTA.15 This will inevitably lead to almost every treated eye developing sight-threatening cataract.
References
Martidis A, Duker JS, Greenberg PB, Rogers AH, Puliafito CA, Reichel E et al. Intravitreal triamcinolone for refractory diabetic macular oedema. Ophthalmology 2002; 109: 920–927.
Massin P, Audren F, Haouchine B, Erginay A, Bergmann JF, Benosman R et al. Intravitreal triamcinolone acetonide for diabetic diffuse macular oedema. Ophthalmology 2004; 111: 218–225.
Sutter FKP, Simpson JM, Gillies MC . Intravitreal triamcinolone for diabetic macular oedema that persists after laser treatment. Ophthalmology 2004; 111: 2044–2049.
Karacorlu M, Ozdemir H, Karacorlu S, Alacali N, Mudun B, Burumcek E . Intravitreal triamcinolone as a primary therapy in diabetic macular oedema. Eye, advance online publication 13. 8. 04 sj.eye.6701512.
Ozkkiris A, Evereklioglu C, Erkilic K, Tamcelik N, Mirza E . Intravitreal triamcinolone acetonide injection as a primary treatment for diabetic macular oedema. Eur J Ophthalmol 2004; 14 (6): 543–549.
Negi AK, Vernon SA, Lim CS, Owen-Armstrong K . Intravitreal triamcinolone improves vision in eyes with chronic diabetic macular oedema refractory to laser photocoagulation. Eye 2004 (E-pub ahead of print).
Islam MS, Negi A, Vernon SA . Improved visual acuity and macular thickness 1 week after intravitreal triamcinolone for diabetic macular oedema. Eye 2004 (E-pub ahead of print).
Kanski JJ . Clinical Ophthalmology A Systematic Approach, 5th Ed. p 167.
Gupta R, Negi AK, Vernon SA . Severe sub-conjunctival haemorrhage following Intravitreal triamcinolone for refractory diabetic oedema. Eye 2005; 19: 590–591.
Jonas JB, Kreissig I, Sofker A, Degenring RF . Intravitreal injection of triamcinolone for diffuse diabetic macular oedema. Arch Ophthalmol 2003; 121: 57–61.
Ciardella AP, Klancnik J, Schiff W, Barile G, Langton K, Chang S . Intravitreal triamcinolone for the treatment of refractory diabetic macular oedema with hard exudates: an ocular coherence tomography study. Br J Ophthalmol 2004; 88: 1131–1136.
Lam DSC, Chan CKM, Tang EWH, Li KKW, Fan DSP, Chan WM . Intravitreal triamcinolone for diabetic macular oedema in Chinese patients: six month prospective longitudinal pilot study. Clin Exp Ophthalmol 2004; 32: 569–572.
Gillies MC, Simpson JM, Billson FA, Luo W, Penfold P, Chua W et al. Safety of an intravitreal injection of triamcinolone. Arch Ophthalmol 2004; 122: 336–340.
Gillies MC, Kuzniarz M, Craig J, Ball M, Luo W, Simpson JM . Intravitreal triamcinolone-induced elevated intraocular pressure is associated with the development of posterior subcapsular cataract. Ophthalmology 2005; 112: 139–143.
Flynn HW, Scott IU . Intravitreal triamcinolone acetonide for macular oedema associated with diabetic retinopathy and venous occlusive disease: it's time for clinical trials. Arch Ophthalmol 2005; 123: 258–259.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Islam, M., Vernon, S. & Negi, A. Intravitreal triamcinolone will cause posterior subcapsular cataract in most eyes with diabetic maculopathy within 2 years. Eye 21, 321–323 (2007). https://doi.org/10.1038/sj.eye.6702304
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702304
Keywords
This article is cited by
-
Cataract progression after primary pars plana vitrectomy for uncomplicated rhegmatogenous retinal detachments in young adults
International Journal of Retina and Vitreous (2024)
-
Comparison of methods to experimentally induce opacification and elasticity change in ex vivo porcine lenses
Scientific Reports (2021)
-
Results of intravitreal triamcinolone acetonide in patients with macular edema secondary to branch retinal vein occlusion
International Journal of Clinical Pharmacy (2014)