Abstract
Purpose
To assess visual acuity (VA) and health-related quality of life (HRQoL) outcomes in patients with and without age-related maculopathy (ARM) after cataract surgery.
Methods
Patients aged 60+ years who had undergone cataract surgery at the Westmead Hospital during 2001–2003 were re-examined 1–3 years after surgery. Tests included VA and assessment of visual- and HRQoL using standardised questionnaires (VF-14, SF-12). Preoperative comorbidity data were collected from medical records. Poor surgical outcomes (VA<6/12; no VA improvement; lowest quintile of VF-14, SF-12 scores) were compared in patients with and without ARM, adjusting for age, sex, preoperative systemic comorbidities, ocular comorbidities and surgical or postoperative complications.
Results
Of 622 surviving patients, 454 (73%) were followed up for a mean period of 2.8 years. Similar proportions with VA≥6/12 were observed in patients with (80.2%) and without (88.8%) pre-existing ARM. Preoperative early ARM was only associated with slightly lower mean VF-14 scores (87.64 with vs92.58 without ARM, P=0.01). Increasing age and preoperative ocular comorbidities were associated with all poor outcomes measured. Low SF-12 scores were associated with preoperative systemic comorbidities.
Conclusion
Our study documents favourable cataract surgical outcomes 1–3 years after cataract surgery in patients with preoperative ARM.
Similar content being viewed by others
Introduction
Cataract surgery is among the most frequently performed surgical procedures.1, 2, 3, 4, 5 Several studies have reported improved visual function and quality of life (QoL) in up to 90% of patients who underwent cataract surgery .6, 7, 8, 9 In general, persons less likely to experience improvement are older and have ocular comorbidities.2, 10, 11, 12
Both age-related maculopathy (ARM) and cataract are strongly age related13, 14, 15, 16 and often present concurrently in older persons.16 Previously, patients with ARM or other ocular comorbidities were considered unlikely to benefit from cataract surgery.2, 10, 11 Recent studies, however, indicate that ARM patients can achieve significant gains in visual function and QoL within months to a year after surgery.17, 18, 19, 20 Few studies, however, have assessed long-term (at least 1 year) surgery outcomes in patients with pre-existing ARM.20 Some population-based reports have suggested an increased long-term risk of developing late ARM in eyes after cataract surgery.21, 22, 23
This study aimed to assess mid- to long-term visual and health-related quality of life (HRQoL) outcomes in a hospital-based sample of patients who had cataract surgery at least 1 year earlier, and to compare outcomes between patients with and without preoperative ARM, plus factors associated with poor outcomes.
Methods
Westmead Hospital is the major public hospital in western Sydney (Australia) and provides public eye services to local residents. In this study, we invited consecutive patients aged 60+ years who had undergone cataract surgery at Westmead Hospital in the last 2 years to return for follow-up examinations. Study procedures were approved by the hospital Human Ethics Committee and informed consent was obtained.
Over a period of 2 years till June 2003, 941 routine cataract procedures were performed, including 718 procedures on 671 patients aged 60+ years with available medical records; as 49 died before the follow-up examinations, 454/622 survivors (73%) were examined.
Preoperative information was obtained retrospectively, by reviewing medical records, including demography, systemic and ocular comorbidities, smoking, preoperative visual acuity (VA) and postoperative surgical complications. To define persons with and without ARM before surgery, the 4-week postoperative clinical notes were used to confirm the preoperative assessment in most patients.24 We considered that the improved postoperative fundal view would provide a more reliable diagnosis of ARM lesions. The early ARM lesions recorded were soft drusen or macular retinal pigment epithelial (RPE) abnormalities (hyper- or hypo-pigmentation); the late lesions recorded were geographic atrophy and neovascular ARM. Using the 4-week postoperative clinical notes did not change any late ARM assessments but did result in a small number (only six cases, 6.1%) of changes to early ARM assessments.24
Participants were re-examined during March–December 2004. VA was measured under standard illumination using Snellen charts with distance correction, if worn, then with pinhole. We defined the following visual impairment levels: no impairment if VA≥6/12; mild if VA<6/12–≥6/24; moderate if VA<6/24–≥6/60; severe if VA<6/60. Structured interviews using VF-14 and SF-12 questionnaires were conducted.
Vision-related QoL was measured using the Visual Function Index (VF-14),9, 25, 26 with scores ranging from 0 (complete loss of visual ability) to 100 (no loss of visual ability).9, 26 The SF-12 (SF-36 short version) was used to assess HRQoL. SF-12 scores were highly correlated with SF-36 summary measures,27 and summarised into mental and physical component scores (MCS, PCS). In general, each component's population mean score is around 50; scores below 50 indicate disability (mild 40–49; moderate 30–39; severe<30). Each question's response is tagged with weights, differently for MCS, PCS. These weights are added to a constant to give the final score of 100.27
Characteristics assessed in relation to surgical outcomes included age, sex, systemic (eg ischaemic heart disease, stroke, diabetes) and ocular comorbidities, other than ARM (eg diabetic retinopathy, glaucoma, cataract type), potential sight-threatening surgical and postoperative complications (eg posterior capsular tear, cystoid macular oedema). The following poor surgical outcomes were defined: lowest quintile VF-14 and SF-12 scores; VA<6/12 in the operated eye; no VA improvement (equal to or worse than preoperative VA).
Statistical Analysis System (V8.2 SAS Institute, Cary, NC) was used for statistical analyses, including χ2 statistics, general linear, and logistic regression models. We converted Snellen VA to logMAR VA for the purpose of statistical analysis as follows: Snellen VA 6/6=logMAR VA 0; 6/7.5=0.1; 6/9=0.2; 6/12=0.3; 6/15=0.4; 6/18=0.5; 6/24=0.6; 6/30=0.7; 6/36=0.8; 6/48=0.9; and 6/60=1.0. General linear models were used to compare mean VA, VF-14, SF-12 scores in patients with/ without preoperative ARM, after adjusting for age, sex, systemic, and ocular comorbidities. Logistic regression models assessed factors associated with poor surgical outcomes, while adjusting for age, sex, preoperative systemic, and ocular comorbidities. Proportions, adjusted means, P-values, odds ratios (OR), and 95% confidence intervals (CI) are presented.
Results
Mean postoperative follow-up period of the 454 patients was 2.8 years (range 0.9–3.4 years). Preoperative characteristics of surviving patients examined at follow-up (n=454) were compared with those of persons not examined (n=168) or deceased (n=49) before follow-up (Table 1). Patients who had moved away or declined further participation were not significantly different from study participants by age or major illness history. Those who had died (n=49) were older or more likely to have had ischaemic heart disease. Mean age of participants (74% Caucasian) was 76 (SD±7.0) years. Mean follow-up VA was 0.21 or 6/9 and the mean VA gain after surgery was 0.28 (approximately three lines on the Snellen chart).
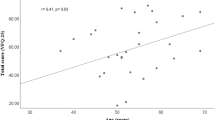
Figure 1 shows proportions with visual impairment before and after surgery. Visual impairment improved by at least one category in 201/454 patients (44.3%), as highlighted in the diagonal boxes, was unchanged in 234 (51.5%), and deteriorated in 19 eyes (4.2%). Overall, postoperative VA was 6/12 or better in 87.0% of eyes. Relatively similar proportions were observed in patients with (80.2%) or without preoperative ARM lesions (88.8%).
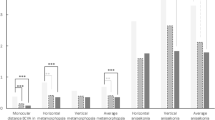
Adjusted means for VA, VF-14, SF-12 scores and VA gain after surgery in patients with/ without early/ late ARM lesions, are shown in Table 2. After adjusting for age, sex, systemic, and other ocular comorbidities, patients with late ARM before surgery had significantly lower postoperative mean VF-14 scores and mean VA, and experienced negative VA gain, than patients without late ARM. Patients with early ARM before surgery had nonsignificantly lower mean VF-14 and SF-12 scores, lower mean VA and less VA gain postoperatively than patients without ARM.
Table 3 show the proportions with different adverse surgical outcomes by potential predictors. Patients older or with ocular comorbidities were more likely to have low follow-up VF-14 scores, while systemic comorbidities led to significantly lower SF-12 mental, physical component scores. Old age and ocular comorbidities or late ARM were significantly associated with postoperative visual impairment.
Table 4 shows factors associated poor surgical outcomes after adjusting for age, sex, preoperative VA, ocular and systemic comorbidities, and ARM. Patients with non-ARM ocular comorbidities were around three times more likely to have low VF-14 (OR 2.77, CI 1.65–4.64), visual impairment (OR 3.59, CI 1.98–6.52) or no visual improvement (OR 2.72, CI 1.53–4.84) postoperatively. Systemic comorbidities were predicted by both low SF-12 MCS (OR 2.25, CI 1.37–3.68) and PCS (OR 2.59, CI 1.56–4.28). Preoperative early ARM was not associated with any measured adverse surgical outcomes.
Discussion
In this hospital-based sample of 454 cataract surgery patients aged 60+ years, follow-up examinations were conducted for an average 2.8 years (range 1.0–3.5 years) after surgery. We found that 44.3% of patients achieved improvement in visual impairment, with 87% achieving VA≥6/12. Relatively similar proportions of patients with (80.2%) and without (88.8%) preoperative ARM improved postoperatively. Preoperative late ARM led to significantly poorer VA and vision-related QoL, whereas preoperative early ARM gave similar postoperative mean VA and QoL as those without ARM. Patients of older age, or with ocular comorbidities before surgery were more likely to have poorer postoperative vision-related QoL (VF-14) and VA outcomes, while those with systemic comorbidities were more likely to have poorer HRQoL (SF-12).
The proportions of our patients with and without ARM achieving VA≥6/12, 1–3 years after surgery, were similar to previously reported short-term cataract surgery visual outcomes.2, 12, 28, 29, 30 Using this same cohort, we previously reported that 82% of persons with ARM achieved VA≥6/12, 4 weeks after surgery.24 Several studies have reported short-term (up to 1 year) postoperative best-corrected VA.2, 12, 28, 29 In general, VA≥6/12 was achieved overall in 90% of eyes, and in 95% of eyes without pre-existing ocular disease. In the Auckland Cataract Study cohort of 97 patients aged 76.3 (±9.9) years, randomly selected from 480 participants, 95% of eyes maintained a best-corrected VA≥6/12, 2 years after surgery.31 Our sample had relatively high prevalence of ocular comorbidities and diabetes,30 a longer follow-up period, and used pinhole VA. All these factors could have influenced postoperative VA levels and contributed to the slightly lower proportion with long-term VA≥6/12 in our sample.
Several preoperative characteristics associated with poor surgical outcomes identified in this study are similar to findings from earlier studies.2, 10, 11, 12 Previous studies have also reported poor mid- to long-term outcomes in patients with surgical/ postoperative complications.10 Our failure to find such associations suggests that surgical complications may predominantly influence only short-term surgical outcomes in this sample.
We found that patients with late ARM before surgery had poor vision-related QoL and a higher proportion had postoperative visual impairment. Presence of preoperative early ARM, however, had a marginal effect on postoperative VA, vision-related and HRQoL over this period, but none of these outcomes were statistically significantly different from patients without early ARM. Our findings are in agreement with previous reports of short-term surgical outcomes.17, 18, 19, 20 Shuttleworth et al.18 reported that two-thirds of ARM patients felt that cataract surgery was worthwhile. Armbrecht et al.17 reported that patients with mild or moderate ARM had significant improvements in HRQoL and visual function 3–5 months after surgery, particularly with moderately severe cataract.
Overall, our study achieved reasonable participation and follow-up rates. Weaknesses include its hospital-based sample, use of medical records to document preoperative ARM signs and the use of pinhole VA as a surrogate measure of best-corrected VA.
In summary, we report that 87% of public hospital-derived patients achieved VA at least 6/12, 1–3 years after cataract surgery. Increasing age and preoperative ocular comorbidities including late ARM, were factors associated with low VF-14 scores and failure of VA improvement. Systemic comorbidities were also related to poorer VA and low SF-12 scores. Preoperative early ARM was not significantly associated with low postoperative VA or low VF-14 scores.
The benefit from cataract surgery to patients with early ARM after more than 3 years, however, was not examined in our study. This is particularly relevant as a number of reports have suggested that increased progression to late ARM may be a long-term phenomenon.21
References
Keeffe JE, Taylor HR . Cataract surgery in Australia 1985–94. Aust NZ J Ophthalmol 1996; 24: 313–317.
Desai P, Minassian DC, Reidy A . National cataract surgery survey 1997–8: a report of the results of the clinical outcomes. Br J Ophthalmol 1999; 83: 1336–1340.
McCarty CA, Keeffe JE, Taylor HR . The need for cataract surgery: projections based on lens opacity, visual acuity, and personal concern. Br J Ophthalmol 1999; 83: 62–65.
Batterbury M, Khaw PT, Hands R, Elkington AR . The cataract explosion: the changing pattern of diagnoses of patients attending an ophthalmic outpatient department. Eye 1991; 5: 369–372.
Tan AG, Wang JJ, Rochtchina E, Jakobsen K, Mitchell P . Increase in cataract surgery prevalence from 1992–1994 to 1997–2000: analysis of two population cross-sections. Clin Experiment Ophthalmol 2004; 32: 284–288.
Desai P, Reidy A, Minassian DC, Vafidis G, Bolger J . Gains from cataract surgery: visual function and quality of life. Br J Ophthalmol 1996; 80: 868–873.
Tielsch JM, Steinberg EP, Cassard SD, Schein OD, Javitt JC, Legro MW et al. Preoperative functional expectations and postoperative outcomes among patients undergoing first eye cataract surgery. Arch Ophthalmol 1995; 113: 1312–1318.
Schein OD, Steinberg EP, Javitt JC, Cassard SD, Tielsch JM, Steinwachs DM et al. Variation in cataract surgery practice and clinical outcomes. Ophthalmology 1994; 101: 1142–1152.
Steinberg EP, Tielsch JM, Schein OD, Javitt JC, Sharkey P, Cassard SD et al. National study of cataract surgery outcomes. Variation in 4-month postoperative outcomes as reflected in multiple outcome measures. Ophthalmology 1994; 101: 1131–1140.
Schein OD, Steinberg EP, Cassard SD, Tielsch JM, Javitt JC, Sommer A . Predictors of outcome in patients who underwent cataract surgery. Ophthalmology 1995; 102: 817–823.
Lundstrom M, Stenevi U, Thorburn W . Outcome of cataract surgery considering the preoperative situation: a study of possible predictors of the functional outcome. Br J Ophthalmol 1999; 83: 1272–1276.
Westcott MC, Tuft SJ, Minassian DC . Effect of age on visual outcome following cataract extraction. Br J Ophthalmol 2000; 84: 1380–1382.
Klein BE, Klein R, Linton KL . Prevalence of age-related lens opacities in a population. The Beaver Dam Eye Study. Ophthalmology 1992; 99: 546–552.
Klein R, Klein BE, Linton KL . Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology 1992; 99: 933–943.
Foran S, Wang JJ, Mitchell P . Causes of visual impairment in two older population cross-sections: the Blue Mountains Eye Study. Ophthalmic Epidemiol 2003; 10: 215–225.
Wang JJ, Foran S, Mitchell P . Age-specific prevalence and causes of bilateral and unilateral visual impairment in older Australians: the Blue Mountains Eye Study. Clin Experiment Ophthalmol 2000; 28: 268–273.
Armbrecht AM, Findlay C, Kaushal S, Aspinall P, Hill AR, Dhillon B . Is cataract surgery justified in patients with age related macular degeneration? A visual function and quality of life assessment. Br J Ophthalmol 2000; 84: 1343–1348.
Shuttleworth GN, Luhishi EA, Harrad RA . Do patients with age related maculopathy and cataract benefit from cataract surgery? Br J Ophthalmol 1998; 82: 611–616.
Lundstrom M, Brege KG, Floren I, Lundh B, Stenevi U, Thorburn W . Cataract surgery and quality of life in patients with age related macular degeneration. Br J Ophthalmol 2002; 86: 1330–1335.
Armbrecht AM, Findlay C, Aspinall PA, Hill AR, Dhillon B . Cataract surgery in patients with age-related macular degeneration: one-year outcomes. J Cataract Refract Surg 2003; 29: 686–693.
Wang JJ, Klein R, Smith W, Klein BE, Tomany S, Mitchell P . Cataract surgery and the 5-year incidence of late-stage age-related maculopathy: pooled findings from the Beaver Dam and Blue Mountains eye studies. Ophthalmology 2003; 110: 1960–1967.
Klein R, Klein BE, Jensen SC, Cruickshanks KJ . The relationship of ocular factors to the incidence and progression of age-related maculopathy. Arch Ophthalmol 1998; 116: 506–513.
Klein R, Klein BE, Wong TY, Tomany SC, Cruickshanks KJ . The association of cataract and cataract surgery with the long-term incidence of age-related maculopathy: the Beaver Dam Eye Study. Arch Ophthalmol 2002; 120: 1551–1558.
Pham TQ, Wang JJ, Maloof A, Mitchell P . Cataract surgery in patients with age-related maculopathy: pre-operative diagnosis and post-operative visual acuity. Clin Experiment Ophthalmol 2005; 33(4): 360–363.
Alonso J, Espallargues M, Andersen TF, Cassard SD, Dunn E, Bernth Petersen P et al. International applicability of the VF-14. An index of visual function in patients with cataracts. Ophthalmology 1997; 104: 799–807.
Steinberg EP, Tielsch JM, Schein OD, Javitt JC, Sharkey P, Cassard SD et al. The VF-14. An index of functional impairment in patients with cataract. Arch Ophthalmol 1994; 112: 630–638.
Ware Jr J, Kosinski M, Keller SD . A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34: 220–233.
Riley AF, Malik TY, Grupcheva CN, Fisk MJ, Craig JP, McGhee CN . The Auckland Cataract Study: co-morbidity, surgical techniques, and clinical outcomes in a public hospital service. Br J Ophthalmol 2002; 86: 185–190.
Murphy C, Tuft SJ, Minassian DC . Refractive error and visual outcome after cataract extraction. J Cataract Refract Surg 2002; 28: 62–66.
Pham TQ, Wang JJ, Rochtchina E, Maloof A, Mitchell P . Systemic and ocular comorbidity of cataract surgical patients in a western Sydney public hospital. Clin Experiment Ophthalmol 2004; 32: 383–387.
Thompson AM, Sachdev N, Wong T, Riley AF, Grupcheva CN, McGhee CN . The Auckland Cataract Study: 2 year postoperative assessment of aspects of clinical, visual, corneal topographic and satisfaction outcomes. Br J Ophthalmol 2004; 88: 1042–1048.
Author information
Authors and Affiliations
Corresponding author
Additional information
Commercial relationship: None
Rights and permissions
About this article
Cite this article
Pham, T., Cugati, S., Rochtchina, E. et al. Age-related maculopathy and cataract surgery outcomes: visual acuity and health-related quality of life. Eye 21, 324–330 (2007). https://doi.org/10.1038/sj.eye.6702171
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702171
Keywords
This article is cited by
-
Quality of life in age-related macular degeneration: a review of available vision-specific psychometric tools
Quality of Life Research (2008)
-
Besteht ein Zusammenhang zwischen Katarakt-Chirurgie und AMD?
Spektrum der Augenheilkunde (2008)