Abstract
Objective
To investigate whether there is an association between the magnitude of retinal haemodynamic abnormalities in patients with age-related macular degeneration (AMD) and the degree of severity of the AMD.
Methods
A retinal laser Doppler system (Canon CLBF 100) was used to measure retinal arterial haemodynamic parameters in 25 eyes of 25 patients with AMD and nine eyes of nine age-matched control subjects. Severity of AMD was classified into Mild (n=11), Moderate (n=7), or Severe (n=7). The pulsatility ratio (PR), the pulsatility index (PI), and the resistivity index (RI) were determined.
Results
PR, PI, and RI in the patients with AMD were each significantly higher than in the control group, and increased monotonically with increasing severity of AMD. However, there were no differences in mean blood velocity, arterial diameter, or blood flow rate among the groups. This suggests that the increased blood flow pulsatility in the retinal arteries of the eyes with AMD is not due to increased distal vascular resistance, but instead is likely due to a loss of compliance in the arterial vasculature leading to the eye.
Conclusion
Our results suggest that an increasing vascular rigidity in the systemic arterial circulation is directly associated with an increasing severity of AMD.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is currently the most common cause of incurable blindness and visual impairment in industrialized countries.1 Prevention of AMD is hampered by a lack of knowledge about the aetiology of the disease and about the identity of modifiable risk factors.
Several studies using colour Doppler imaging have reported that circulatory abnormalities are present in the posterior ciliary arteries and in the central retinal artery in patients with AMD.2, 3, 4, 5 A common finding has been an increase in the pulsatility of the blood speed in these arteries. The interpretation of such a finding, however, remains ambiguous, since an increase in pulsatility can be associated with pathology either proximal or distal to the measurement site. In order to resolve this ambiguity, it is necessary to determine the actual blood flow rate, which requires knowledge of the arterial diameter at the measurement site as well as the time-average blood speed during the cardiac cycle. Colour Doppler imaging does not provide these measurements. Although impaired foveal choroidal capillary blood flow has been found in AMD using laser Doppler flowmetry,6 there has been no previous report on haemodynamic abnormalities in the major retinal vessels in patients with AMD.
In this study, we measured the actual blood flow rate as well as the pulsatile characteristics of the blood flow in an effort to determine whether there is intraretinal vascular pathology associated with AMD, or whether the haemodynamic abnormalities measured in retinal arteries simply reflect a more generalized systemic vascular pathology in patients with AMD.
Methods
Patients from Schepens Retina Associates Foundation were enrolled in the study. In all, 25 patients with AMD and nine age-matched healthy control subjects were examined. Patients with AMD who also had other diseases of the eye that might possibly affect the retinal circulation, such as diabetic retinopathy, glaucoma, or those with a history of laser treatment or intraocular surgery, were excluded. All subjects were informed about the nature of the study and gave their consent to be included. The research followed the tenets of the Declaration of Helsinki. All subjects underwent a complete ophthalmic examination including slit-lamp biomicroscopy, Snellen visual acuity, and intraocular pressure measurement. Stereoscopic colour fundus photographs were taken using a Topcon TRC-50EX fundus camera (Topcon Corporation, Tokyo, Japan). The photographs were used for classifying the degree of severity of the AMD according to the Age-Related Eye Disease Study (AREDS) system.7 Eyes were classified into four AREDS categories by an examiner (ES) without knowledge of the retinal haemodynamic results: Category 1, few if any small drusen; Category 2, extensive small drusen or nonextensive intermediate-sized drusen; Category 3, extensive intermediate-sized drusen, at least one large drusen, or noncentral geographic atrophy; or Category 4, evidence of neovascular AMD or central geographic atrophy. In our study, we combined those in Categories 1 and 2 into a Mild group. Those in Category 3 were designated as a Moderate group, and those in Category 4 as a Severe group. Only one eye of each subject was included. In patients with AMD, the study eye was selected randomly when both eyes were classified with the same AMD severity. The eye with the more severe AMD was selected when the AMD severity was asymmetric. The characteristics of the control subjects and the patients in each AMD group are summarized in Table 1.
The Canon laser Doppler Flowmeter model CLBF 100 (Canon, Tokyo, Japan) was used to measure the blood column diameter (D), the centreline blood velocity (V), and the blood flow (F) in major temporal retinal arteries.8 The instrument is equipped with an automatic eye tracking system that maintains centration of the laser beam measuring on the target blood vessel even during eye movements. The beam from a red 675-nm diode laser is used for blood velocity measurements. The Doppler-shifted light scattered from the flowing blood cells in the target vessel is detected simultaneously in two directions separated by a fixed angle. The signals from two photomultiplier tube detectors undergo computer-controlled spectrum analysis, and sequential measurements of V are performed automatically. Results are acquired at 50 measurements per second for 2 s, yielding quasicontinuous traces of the systolic–diastolic variation of the arterial blood velocity.
Three indices of pulsatility, the pulsatility ratio (PR), the pulsatility index (PI), and the resistivity index (RI) (also known as Pourcelot's ratio9), were calculated from the blood velocity traces. PR is expressed as PSV/EDV, where PSV is the peak velocity during systole and EDV is the end diastolic velocity; PI is expressed as (PSV−EDV)/MV, where MV is the time-average mean velocity during the cardiac cycle; RI is expressed as (PSV−EDV)/PSV.
Student's unpaired t-test was used for the comparison of differences between control subjects and patients with AMD. One-way analysis of variance (ANOVA) was used for multiple comparisons. Significances of individual differences were evaluated by using the Scheffe F-test if ANOVA was significant. Spearman's correlation analysis was used to determine whether PR, PI, or RI was correlated with the severity of AMD.
Results
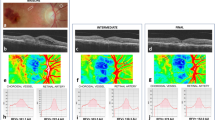
Figure 1 shows representative fundus photographs of a control subject (A), and patients with a Mild (B), Moderate (C), and Severe AMD (D).
Figure 2 shows the variation during cardiac cycles of the centreline blood velocity measured in a major temporal retinal artery in a control subject and in a patient with AMD. The blood flow is markedly more pulsatile in the patient with AMD compared to that in the control subject.
The values of PR, PI, and RI in the patients with AMD and in the control group are shown in Table 2. Each index was significantly higher in the patients than in the controls.
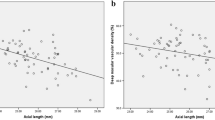
As shown in Figure 3, PR increased monotonically from 4.2±1.2 (mean±SD) in the control group to 6.4±2.7 in the mild group to 7.8±3.8 in the moderate group to 9.5±5.1 in the severe group (Spearman's ρ=0.59, P=0.0010). Similarly, PI increased monotonically from 1.4±0.3 in the control group to 1.7±0.2 in the mild group to 1.8±0.4 in the moderate group to 2.0±0.5 in the severe group and correlated with the severity of AMD (Spearman's ρ=0.52, P=0.0042). Also, RI increased monotonically from 0.75±0.07 in the control group to 0.82±0.06 in the mild group to 0.84±0.09 in the moderate group to 0.87±0.06 in the severe group and correlated with the severity of AMD (Spearman's ρ=0.59, P=0.0010). ANOVA was statistically significant for PR (P=0.022), PI (P=0.017), and RI (P=0.0076). PR (P=0.031), PI (P=0.023), and RI (P=0.012) were each significantly higher in the severe group compared to the control group (Scheffe F-test).
As shown in Figure 4, mean velocity was 31.9±8.3 mm/s in the control group, 34.5±9.6 mm/s in the mild group, 25.8±9.2 mm/s in the moderate group, and 29.5±8.8 mm/s in the severe group. Diameter was 106±9 μm in the control group, 110±11 μm in the mild group, 108±16 μm in the moderate group, and 120±12 μm in the severe group. Flow was 8.4±3.1 μl/min in the control group, 10.7±4.7 μl/min in the mild group, 7.4±4.0 μl/min in the moderate group, and 10.2±3.9 μl/min in the severe group. There were no significant correlations between mean velocity, diameter or flow, and severity of AMD. There were no significant differences in mean velocity, diameter, or flow across the four groups.
Discussion
This study demonstrates that blood flow in retinal arteries is more pulsatile in patients with AMD than in healthy controls. Furthermore, all three indices of pulsatility (PR, PI, and RI) increased monotonically with increasing severity of AMD. However, the average retinal blood flow and average retinal blood velocity were not significantly different across the four groups. Our finding of no decrease in the average blood flow rate in patients with AMD is consistent with the results of Medeiros et al,10 who reported that there was no detectable loss of ganglion cell layer (GCL) neurons in nonexudative AMD and that relatively many GCL neurons survive even in exudative AMD despite massive photoreceptor loss. When GCL neurons degenerate and die, it is likely that both retinal metabolism and retinal blood flow would be decreased. Clearly, this is not the case in AMD. The retinal haemodynamic results in the patients with severe AMD appear to be part of a continuum of changes seen across the four study subgroups. The damage associated with mild, moderate, or severe AMD affects the outer retina and seemingly spares the inner retina, which is nourished by the retinal circulation.
Typically, an increased PR, PI, or RI is an indicator of increased vascular resistance to flow and/or decreased vascular compliance,11, 12 distal to the measurement site. If this were the case, however, then the average blood flow would also be reduced. The average retinal blood flow was not significantly different across the four groups in the present study. Such retinal haemodynamic results in patients with AMD indicate that there may be a more generalized circulatory abnormality proximal to the eye. Specifically, it is likely that patients with AMD have a stiffer, less compliant arterial vasculature leading to the eye, and that the loss of compliance of the large blood vessels is due to age-related degenerative changes in collagen and elastin.13
A recent histopathological study14 has shown that in patients with AMD, the macular Bruch's membrane, comprised of inner and outer collagen-rich layers flanking a central layer of elastin and elastin-associated proteins, is thinner and more porous than in age-matched controls. The increased porosity is due to larger gaps in the elastin layer in eyes with AMD. As the authors of this study point out, it is not clear whether the elastin layer degrades more rapidly in eyes with AMD, or whether the deficit of elastin is present from the time of birth. In either case, it is the deficit of elastin, both in Bruch's membrane and in the walls of large conduit arteries, that likely links AMD with the stiffening of the systemic vasculature and the resulting haemodynamic changes observed in the retina. In the conduit arteries, the fracture of elastin fibres leads to the transfer of stress to collagen fibres, which are 100–1000 times stiffer than elastin,15 while in Bruch's membrane, gaps in the elastin layer provide the substrate for the development of AMD.
Epidemiological studies have also shown that patients with AMD often have concomitant systemic vascular disease such as arterial hypertension, atherosclerosis, or hypercholesteraemia.1, 16, 17, 18, 19, 20 In fact, as shown in Table 1, a number of our study patients with AMD were being treated for these disorders. Smoking, hypertension, and elevated serum cholesterol have been shown to be risk factors for both AMD and cardiovascular disease. Specifically, it has been reported that a high total serum cholesterol level is a risk factor for both neovascular AMD and geographic atrophy.21 In addition, there have been reports linking statin use with a lower risk of AMD.22, 23 Statins, hydroxymethyl glutaryl coenzyme A reductase inhibitors, are prescribed to help reduce low-density lipoprotein (LDL) cholesterol levels by inhibiting cholesterol production and increasing LDL cholesterol removal from plasma. The overlap in risk factors for AMD and cardiovascular disease has led to the suggestion that a common disease mechanism may be operative in both AMD and cardiovascular disease.
Friedman24, 25, 26 has suggested that AMD shares both risk factors and pathogenetic mechanisms with atherosclerosis, resulting in the deposition of lipid in the sclera and in Bruch's membrane. He proposes an alternate explanation for the ocular haemodynamic abnormalities observed in AMD, suggesting that an increasingly rigid sclera would act to encapsulate the ocular vasculature in a more incompressible compartment, leading to a greater degree of systolic–diastolic variation in the blood velocity during the cardiac cycle. The answer to the question of whether AMD-related haemodynamic abnormalities are due to increased scleral rigidity, increased systemic vascular rigidity, or both awaits further investigation.
In summary, our results add support to the conjecture that AMD and cardiovascular disease share the same modifiable risk factors. Treatments aimed at preventing systemic arterial rigidity may also be effective in preventing the onset or slowing the progression of AMD.
References
Tomany SC, Wang JJ, van Leenwen R, Klein R, Mitchell P, Vingerling JR et al. Risk factors for incident age-related macular degeneration. Pooled findings from 3 continents. Ophthalmology 2004; 111: 1280–1287.
Ciulla TA, Harris A, Chung HS, Danis RP, Kagemann L, McNulty L et al. Color Doppler imaging discloses reduced ocular blood flow velocities in nonexudative age-related macular degeneration. Am J Ophthalmol 1999; 128: 75–80.
Hosal BM, Karakoç G, Gürsel E, Çamur M . Color Doppler imaging of the retrobulbar circulation in age-related macular degeneration. Eur J Ophthalmol 1998; 8: 234–238.
Friedman E, Krupsky S, Lane AM, Oak SS, Friedman ES, Egan K et al. Ocular blood flow velocity in age-related macular degeneration. Ophthalmology 1995; 102: 640–646.
Dimitrova G, Tamaki Y, Kato S . Retrobulbar circulation in patients with age-related maculopathy. Eye 2002; 16: 580–586.
Grunwald JE, Hariprasad SM, DuPont J, Maguire MG, Fine SL, Brucker AJ et al. Foveolar choroidal blood flow in age-related macular degeneration. Invest Ophthalmol Vis Sci 1998; 39: 385–390.
The Age-Related Eye Disease Study Research Group. The age-related eye disease study system for classifying age-related macular degeneration from stereoscopic color fundus photographs: the age-related eye disease study report. Number 6. Am J Ophthalmol 2001; 132: 668–681.
Yoshida A, Feke GT, Mori F, Nagaoka T, Fujio N, Ogasawara H et al. Reproducibility and clinical application of a new developed stabilized retinal laser Doppler instrument. Am J Ophthalmol 2003; 135: 356–361.
Pourcelot L . Indications de l'ultrasonographie Doppler dans l'etude des vaisseaux peripheriques. Rev Prat 1975; 25: 4671–4680.
Medeiros NE, Curcio CA . Preservation of ganglions cell layer neurons in age-related macular degeneration. Invest Ophthalmol Vis Sci 2001; 42: 795–803.
Polska E, Kircher K, Ehrlich P, Vecsel PV, Schmetterer L . RI in central retinal artery as assessed by CDI does not correspond to retinal vascular resistance. Am J Physiol 2001; 280: H1442–H1447.
Bude R, Rubin J . Relationship between the resistive index and vascular compliance and resistance. Radiology 1999; 211: 411–417.
Klein R, Klein BEK, Tomany SC, Cruickshanks KJ . The association of cardiovascular disease with the long-term incidence of age-related maculopathy. Ophthalmology 2003; 110: 636–643.
Chong NHV, Keonin J, Luthert PJ, Frennesson CI, Weingeist DM, Wolf RL et al. Decreased thickness and integrity of the macular elastic layer of Bruch's membrane correspond to the distribution of lesions associated with age-related macular degeneration. Am J Pathol 2005; 166: 241–251.
Martyn CN, Greenwald SE . Impaired synthesis of elastin in walls of aorta and large conduit arteries during early development as an initiating event in pathogenesis of systemic hypertension. Lancet 1997; 350: 953–955.
Vingerling JR, Dielemans I, Bots ML, Hofman A, Grobbee DE, de Jong PT . Age-related macular degeneration is associated with atherosclerosis. The Rotterdam Study. Am J Epidemiol 1995; 142: 404–409.
van Leeuwen R, Ikram MK, Vingerling JR, Witteman JC, Hofman A, de Jong PT . Blood pressure, atherosclerosis, and the incidence of age-related maculopathy: The Rotterdam study. Invest Ophthalmol Vis Sci 2003; 44: 3771–3777.
Snow KK, Seddon JM . Do age-related macular degeneration and cardiovascular disease share common antecedents? Ophthal Epidemiol 1999; 6: 125–143.
AREDS Research Group. Associations of mortality with ocular disorders and an intervention of high-dose antioxidants and zinc in the age-related eye disease study. AREDS Report No. 13. Arch Ophthalmol 2004; 122: 716–726.
Chaine G, Hullo A, Sahel J, Soubrane G, Espinasse-Berrod MA, Schutz D et al. Case–control study of the risk factors for age related macular degeneration. Br J Ophthalmol 1998; 82: 996–1002.
McGwin Jr G, Owsley C, Curcio CA, Crain RJ . The association between statin use and age related maculopathy. Br J Ophthalmol 2003; 87: 1121–1125.
Wilson HL, Schwartz DM, Bhatt HRF, Mcculoch CE, Duncan JL . Statin and aspirin therapy are associated with decreased rate of choroidal neovascularization among patients with age-related macular degeneration. Am J Ophthalmol 2004; 137: 615–624.
Hall NF, Gale CR, Syddall H, Phillips DI, Martyn CN . Risk of macular degeneration in users of statins: cross sectional study. BMJ 2001; 323: 375–376.
Friedman E . A hemodynamic model of the pathogenesis of age-related macular degeneration. Am J Ophthalmol 1997; 124: 677–682.
Friedman E . The role of the atherosclerotic process in the pathogenesis of age-related macular degeneration. Am J Ophthalmol 2000; 130: 658–663.
Friedman E . Update of the vascular model of AMD. Br J Ophthalmol 2004; 88: 161–163.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was presented in part at the 2004 Annual Meeting of the Association for Research in Vision and Ophthalmology, 25–29 April 2004. Financial Interest Disclosure: None of the authors has any commercial or proprietary interest in the instrumentation described in this article.
Rights and permissions
About this article
Cite this article
Sato, E., Feke, G., Menke, M. et al. Retinal haemodynamics in patients with age-related macular degeneration. Eye 20, 697–702 (2006). https://doi.org/10.1038/sj.eye.6701951
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701951
Keywords
This article is cited by
-
Elevated retinal artery vascular resistance determined by novel visualized technique of laser speckle flowgraphy in branch retinal vein occlusion
Scientific Reports (2021)
-
The flicker response of venous oxygen saturation is significantly reduced in the early and late stages of age-related macular degeneration
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)
-
Effects of topical carteolol on retinal arterial blood flow in primary open-angle glaucoma patients
Japanese Journal of Ophthalmology (2012)
-
The pulsating brain: A review of experimental and clinical studies of intracranial pulsatility
Fluids and Barriers of the CNS (2011)
-
The clinical utility of colour Doppler imaging
Eye (2007)