Abstract
Purpose To compare the quality of anaesthesia and complication rates between three sub-Tenon cannula of increasing length (anterior Greenbaum, mid Kumar–Dodds, and posterior Steven's sub-Tenon's cannulae).
Methods A total of 150 patients undergoing cataract extraction were randomised to receive a sub-Tenon injection of 5 ml of 2% lidocaine with hyaluronidase with one of the three cannulae. The development of akinesia was assessed every 2 min over a 6-min period. Complications were also recorded.
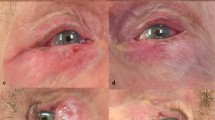
Results There was no difference in the onset of akinesia, with 46, 50, and 46 patients achieving adequate akinesia within 6 min for the anterior, mid, and posterior groups respectively (P>0.05). There was an increase in retained lid opening with anterior compared to mid and posterior cannulae (P=0.0001). There was significantly less retained lid closure with the posterior compared to the mid or anterior cannulae (P<00001). The mean (range, SD) scores for pain during injection were 0.4 (0–5, 0.83), 1.2 (0–9, 1.96), and 1.1 (0–6, 1.19) for the anterior, mid, and posterior groups, respectively. These were not significantly different between the anterior and mid groups, or the mid and posterior groups (P>0.05), but there was significantly more pain on injection with the posterior compared to the anterior groups (P<0.01). All patients scored intraoperative pain as zero. There was significantly more chemosis in the anterior group (76%) compared to the mid (20%) and posterior (32%) groups (P<0.0001). There were significantly (P=0.0004) more conjunctival haemorrhages in the anterior group (56%) than the mid (20%) or posterior (20%) groups.
Conclusions We have shown that all three cannulae provide high-quality anaesthesia with minor differences in retained muscle activity, chemosis, and haemorrhage rates.
Similar content being viewed by others
Introduction
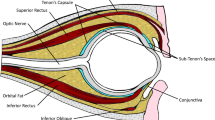
Sub-Tenon's anaesthesia is becoming increasingly popular for ophthalmic surgery. 1 It is believed to have advantages over sharp needle techniques in terms of reduced risks of globe perforation, retrobulbar haemorrhage, and brainstem anaesthesia. Delivery of local anaesthetic solution into the sub-Tenon space has been described using a variety of cannulae.2, 3, 4 The three most commonly used cannulae at the North Riding Infirmary, Middlesbrough, UK include a 12 mm plastic anterior sub-Tenon cannula (Greenbaum cannula, Figure 1), an 18 mm plastic mid sub-Tenon cannula (Kumar–Dodds cannula, Figure 2), and a 25 mm metal curved posterior sub-Tenon (Stevens cannula, Figure 3). Serious complications of sub-Tenon anaesthesia are rare but have been documented.5, 6, 7 Minor complications are more common, and include pain on injection (44%), chemosis (25–100%), and conjunctival haemorrhage (20–100%).2, 8, 9 The influence of dedicated sub-Tenon cannulae on the development of akinesia and the incidence of complications has received less attention. LaMarnierre et al10 compared the Greenbaum cannula method with the Ripart injection technique, and found no difference in analgesia, but a higher incidence of chemosis with the Greenbaum cannula. Similarly, Tokuda et al11 compared the delivery of 3 ml of local anaesthetic into varying depths of the sub-Tenon's and found no difference in analgesic efficacy. In this prospective study, we compared the onset of akinesia, analgesia, and complications using three different sub-Tenon cannulae.
Methods and materials
After obtaining Local Hospital Ethics Committee approval, 150 patients scheduled for routine cataract extraction surgery were enrolled. Patients were excluded if they were unwilling to participate, if there were communication difficulties, if their medication included anticoagulant or nonsteroidal antiinflammatory medication, or if there was any history of allergy to the study drugs. Informed consent was obtained. At the beginning of each operating list, a sealed envelope was opened, which contained a random choice of cannula to be used during that session.
Patients were not starved and received no sedative premedication. In the anaesthetic room, baseline globe and eyelid movements were assessed, routine monitoring applied, and an intravenous cannula sited. Topical anaesthesia of the conjunctiva was achieved by administering 2–3 drops of 0.5% proxymetacaine. A standard sub-Tenon technique was performed, incising conjunctiva and Tenon's capsule in the inferonasal quadrant followed by a slow injection of 5 ml of lidocaine 2% with hyaluronidase 30 iu/ml using one of the three cannulae. Assessment of block by observing ocular movement in the secondary directions of gaze (abduction, adduction, medial, and lateral) was performed at 2 min intervals using the scoring system shown in Table 1 by an experienced anaesthetic nurse who was unaware of the type of cannula used. Full movement (ie no block) scored 12 points, whereas full block scored zero. A score of four or less was deemed adequate for surgery. If after 6 min the block was inadequate for surgery, supplementary anaesthesia was provided by a further injection of 3 ml of the same local anaesthetic solution. Oblique muscle and eyelid movements were scored as present or absent. Immediately after surgery, patients were asked to score injection and peroperative pain using a verbal rating scale (0 no pain–10 worst pain imaginable). Complications such as chemosis and haemorrhage were noted. For analysis, patients were divided into three groups; those who received the Greenbaum cannula (anterior group), the Kumar–Dodds cannula (mid group), and the Steven's cannula (posterior group). Data were analysed with Graphpad Instat version 2.04 using Fisher's exact test or Dunnet's multiple comparison test where appropriate. Results were considered significant when P<0.05.
Results
Analysis of the demographic data revealed a significant difference in age between the mid and posterior groups (Table 2). Although statistically significant, this difference is unlikely to have any clinical relevance. Similar numbers of patients in each group achieved a block score <4 within 6 min (Table 3). Supplementary injections were required by two, zero, and three patients in the anterior, mid, and posterior groups, respectively (P>0.05). There were differences in block of oblique and lid muscles activity between the groups. The mean (range, SD) scores for pain during injection were 0.4 (0–5, 0.83), 1.2 (0–9, 1.96), and 1.1 (0–6, 1.19) for the anterior, mid, and posterior groups, respectively. These were not significantly different between the anterior and mid groups, or the mid and posterior groups (P>0.05), but there was significantly more pain on injection with the posterior compared to the anterior groups (P<0.01). All patients scored intraoperative pain as zero. As Figure 4 shows, there was significantly more chemosis in the anterior group compared to the mid and posterior groups (P<0.0001). There were significantly more conjunctival haemorrhages in the anterior groups than the mid or posterior groups (P=0.0004).
Discussion
Factors influencing the choice of sub-Tenon cannula include local availability, operator training, operator experience, and cannula characteristics such as effectiveness, ease of use, and adverse event profile. The cannulae used in this study are straightforward to use with minimal differences in insertion technique. They provided comparable high-quality akinesia of the recti muscles, but there were statistically significant differences in terms of blockade of the oblique muscles, lid opening, and closing. However, none of the surgeons encountered any difficulties attributable to a lack of akinesia, and as modern phacoemulsification techniques can be performed with a mobile eye, these differences are unlikely to be clinically relevant. In situations where a greater degree of akinesia is desirable (trainee surgeon, corneal graft surgery, etc) it would be worth avoiding the shorter anterior cannula that produced marginally less ocular akinesia. This may be due to the local anaesthetic solution tracking anteriorly under the conjunctiva, producing chemosis, with relatively less volume of the local anaesthetic agent reaching posteriorly to the innervation of the ocular muscles. Chemosis develops where there is incomplete dissection of the sub-Tenon space, lax tissues, a high distending pressure during injection, a higher volume of local anaesthetic, and, as we have demonstrated, anterior placement of the local anaesthetic solution. It is not known whether the chemosis seen with the anterior cannula could be reduced by minimising the distending pressure during injection. Although unsightly, chemosis rarely presents a problem during routine cataract surgery. However, in glaucoma surgery some surgeons feel that chemosis may interfere with the construction of scleral flap.
The anterior cannula was associated with a significantly higher incidence of conjunctival haemorrhage. This may be due to tearing of fine conjunctival blood vessels as the local anaesthetic tracks subconjunctivally. Again this should not affect the surgical field, but the cosmetic consequences may assume greater importance for the patient in the week following surgery. The mean pain scores during injection were low with all the cannulae. The anterior cannulae appeared to cause the least pain, but differences were small and very unlikely to have clinical relevance.
In summary, high-quality local anaesthesia can be achieved with any of these three cannula. There is a higher incidence of chemosis and haemorrhage with the anterior cannula, although this is rarely problematic.
References
Park A . Local anaesthesia for routine ocular surgery. Br J Anaesth 1999; 82: 153–154.
Stevens J . A new local anaesthesia technique for cataract extraction by one quadrant sub-Tenon's infiltration. Br J Ophthalmol 1992; 76: 670–674.
Kumar C, Dodds C . A disposable plastic sub-Tenon cannula. Anaesthesia 2001; 56: 399–400.
Greenbaum S . Parabulbar anesthesia. Am J Ophthalmol 1992; 114: 776.
Olitsky S, Juneja R . Orbital haemorrhage after the administration of sub-Tenon's infusion anaesthsia. Ophthalmic Surg Lasers 1997; 28: 145–146.
Frieman B, GFriedberg M . Globe perforation associated with sub-Tenon's anaesthesia. Am J Ophthalmol 2001; 131: 520–521.
Jaycock P, Mather C, Ferris J, Kirkpatrick J . Rectus muscle trauma complicating sub-Tenon's local anaesthesia. Eye 2001; 15: 583–586.
Verghese I, Sivraj P, Lai Y . The effectiveness of sub-Tenon's infiltration of local anaesthesia for cataract surgery. Aust N Z J Ophthalmol 1996; 24: 117–120.
Kumar C, Dodds C . Evaluation of Greenbaum's sub-Tenon's block. Br J Anaesthe 2001; 87: 631–633.
La Marnierre E, Mage F, Alberti M, Batisse J, Baltenneck A . Comparison between Greenbaum's parabulbar anesthesia and Ripart's subtenon anesthesia in the anterior segment surgery. J Fr Ophthalmol 2002; 25: 161–165.
Tokuda Y, Onda K, Yoshitomi F, Inouye J, Amano S, Oshika T . Comparison of sub-Tenon's anaesthesia by different delivery techniques in cataract surgery. Eye 1999; 13: 640–642.
Author information
Authors and Affiliations
Corresponding author
Additional information
The abstract of this study was presented at the Third Annual National Meeting of British Ophthalmic Anaesthesia Society, August 2001.
Rights and permissions
About this article
Cite this article
Kumar, C., Dodds, C., McLure, H. et al. A comparison of three sub-Tenon's cannulae. Eye 18, 873–876 (2004). https://doi.org/10.1038/sj.eye.6701332
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701332