Abstract
Background/Objectives:
Little is known about factors associated with weight change post discharge from hospital; yet poor nutritional status in the transition from hospital to community can result in readmission. This exploratory study aimed to determine the factors associated with weight change 30 days post discharge defined as weight gain (WG; 5+ pounds), weight loss (WL; 5+pounds) or weight stable (WS).
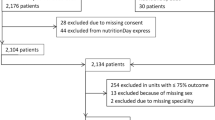
Subjects/Methods:
A total of 922 medical or surgical patients were recruited from 16 acute care hospitals in 8 Canadian provinces. Telephone interviews were completed with 747 (81%) participants 30 days post discharge using a standardized questionnaire that included: self-reported weight change, assessment of appetite, usage of healthcare services and supports for food-related activities of daily living. Covariates collected during hospitalization, including nutritional status at discharge evaluated by subjective global assessment (SGA), were used in logistic regressions.
Results:
Among the 747 patients, 26% reported WL, 16.7% had WG and 57.2% were WS. Those with WG were: younger (odds ratio (OR) 0.77 (0.69, 0.85)), male (OR 1.71 (1.12, 2.61)), malnourished at discharge (SGA B OR 2.13 (1.36, 3.33), SGA C OR 2.76 (1.19, 6.62)), and had a good appetite based on the low OR for fair/poor appetite (OR 0.28 (0.11, 0.66)). WL was associated with being on a special diet (OR 1.45 (1.07,1.96)) and reporting fair/poor appetite (OR 2.67 (1.76, 4.07)).
Conclusions:
Weight change was relatively common with WL predominating. Several variables were identified to be predictors of WL or weight gain, with appetite being common to both. Future work to further define and confirm these associations is warranted.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Allard JP, Keller H, Jeejeebhoy KN, Laporte M, Duerksen D, Gramlich L et al. Malnutrition at hospital admission: contributors and impact on length of stay. A prospective cohort study from the Canadian Malnutrition Task Force. JPEN J Parenter Enteral Nutr 2015; 40: 487–497.
Badgwell B, Stanley J, Chang GJ, Katz MHG, Lin HY, Ning J et al. Comprehensive geriatric assessment of risk factors associated with adverse outcomes and resource utilization in cancer patients undergoing abdominal surgery. J Surg Oncol 2013; 108: 182–186.
Allaudeen N, Vidyarthi A, Maselli J, Auerbach A . Redefining readmission risk factors for general medicine patients. J Hosp Med 2011; 6: 54–60.
Allard JP, Keller H, Jeejeebhoy KN, Laprote M, Duerksen DR, Gramlich L et al. Decline in nutritional status is associated with prolonged length of stay in hospitalized patients admitted for 7 days or more: a prospective cohort study. Clin Nutr 2015; 35: 144–152.
Allard JP, Keller H, Teterina A, Jeejeebhoy KN, Laporte M, Duerksen DR et al. Lower handgrip strength at discharge from acute care hospitals is associated with 30- day readmission: a prospective cohort study. Clin Nutr 2016; 35: 1535–1542.
Buys DR, Rother DL, Ritchie CS, Sawyer P, Allman RM, Funkhouser EM et al. Nutritional risk and body mass index predict hospitalization, nursing home admissions, and mortality in community-dwelling older adults: results form the UAB Study of Aging with 8.5 years of follow-up. J Gerontol A Biol Sci Med Sci 2014; 69: 1146–1153.
Charlton KE, Nichols C, Bowden S, Lambert K, Barone L, Mason M et al. Older rehabilitation patients are at high risk of malnutrition: evidence from a large Australian database. J Nutr Health Aging 2010; 14: 622–628.
Boumendjel N, Herrmann F, Girod V, Sieber C, Rapin C-H . Refrigerator content and admission in old people. Lancet 2000; 356: 563.
Lum HD, Studenski SA, Degenholtz HB, Hardy SE . Early hospital readmission is a predictor of one-year mortality in community-dwelling older Medicare beneficiaries. J Gen Intern Med 2012; 27: 1467–1474.
Neelemaat F, Bosmans JE, Thijs A, Seidell JC . Post-discharge nutritional support in malnourished elderly individuals improves functional limitations. J Am Med Dir Assoc 2011; 12: 295–301.
Deutz NE, Matheson EM, Matarese LE, Lu M, Baggs GE, Nelson JL et alon behalf of the NOURISH Study group. Readmission and mortality in malnourished, older, hospitalized adults treated with a specialized oral nutritional supplement: a randomized clinical trial. Clin Nutr 2016; 35: 18–26.
Beck A, Holst M, Rasmussen HH . Oral nutritional support of old patients after discharge from hospital: systematic review and meta-analysis of randomized controlled trials. Clin Rehabil 2013; 27: 19–27.
Beck AM, Andersen UT, Leedo E, Jensen LL, Martins K, Quvang M et al. Does adding a dietician to the liaison team after discharge of geriatric patients improve nutritional outcome: a randomized controlled trial. Clin Rehabil 2015; 29: 1117–1128.
Calvillo-King L, Arnold D, Eubank KJ, Lo M, Yunyngying P, Stietglitz H et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Inter Med 2012; 28: 269–282.
Perruccio AV, Losina E, Wright EA, Katz JN . Aggregate health burden and the risk of hospitalization in older persons post hip replacement surgery. J Gerontol A Biol Sci Med Sci 2013; 68: 293–300.
Detsky AS, Baker JP, Johnston N, Whittaker S, Mendelson RA, Jeejeebhoy KN . What is subjective global assessment of nutritional status? J Parenter Enteral Nutr 1987; 11: 8–13.
Charlson ME, Pompei P, Ales KL, MacKenzie CR . A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383.
Schindler K, Pernicka E, Laviano A, Howard P, Schutz T, Bauer P et al. How nutritional risk is assessed and managed in European hospitals: a survey of 21,007 patients findings from the 2007-2008 cross-sectional nutritionDay survey. Clin Nutr 2010; 29: 552–559.
Keller HH, Goy R, Kane S-L . Validity and reliability of SCREEN II (SeniorsIn the Community: Risk Evaluation for Eating and Nutrition- version II). Eur J Clin Nutr 2005; 59: 1149–1157.
Keller H, Payette H, Laporte M, Bernier P, Allard JP, Duerksen DR et al Predictors of dietitian care in the community post hospitalization: a Canadian Malnutrition Task Force (CMTF) study (submitted).
Deschodt M, Devriendt E, Sabbe M, Knockaert D, Deboutte P, Boonen S et al. Characteristics of older adults admitted to the emergency department (ED) and their risk factors for ED readmission based on comprehensive geriatric assessment: a prospective cohort study. BMC Geriatr 2015; 15: 54.
Keller H, Allard JP, Laporte M, Davidson B, Payette H, Bernier P et al. Predictors of dietitian consult on medical and surgical wards. Clin Nutr 2015; 34: 1141–1145.
Lainscak M, Farkas J, Frantal S, Singer P, Bauer P, Hiesmayr M et al. Self-rated health, nutritional intake and mortality in adult hospitalized patients. Eur J Clin Invest 2014; 44: 813–824.
Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR . Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult hospital malnutrition. J Acad Nutr Diet 2013; 113: 1219–1237.
Keller H, Vesnaver E, Davidson B, Allard J, Laporte M, Bernier P et al. Providing quality nutrition care in acute care hospitals: perspectives of nutrition care personnel. J Hum Nutr Diet 2014; 27: 192–202.
Laporte M, Keller H, Payette H, Allard JP, Duerksen DR, Bernier P et al. Validity and reliability of the new Canadian Nutrition Screening tool in the ‘real-world’ hospital setting. Eur J Clin Nutr 2015; 69: 558–564.
Akhtar U, Keller HH, Tate RB, Lengyel CO . Construct validation of three nutrition questions using health and diet ratings in older Canadian males living in the community. Can J Diet Prac Res 2015; 76: 1–6.
Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI et al. Diagnoses and timing of 30- day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA 2013; 309: 355–363.
Vashi AA, Fox JP, Carr BG, D'Onofrio G, Pines JM, Ross JS et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA 2013; 309: 364–371.
Legrain S, Tubach F, Bonnet-Zamponi D, Lemaire A, Aquino JP, Paillaud E et al. A new multimodal geriatric discharge-planning intervention to prevent emergency visits and rehospitalizations of older adults: The Optimization of Medication in AGEd Multicenter Randomized Control Trial. J Am Geriatr Soc 2011; 59: 2017–2028.
Acknowledgements
We are grateful to the 18 sites and their coordinators who collected the data for this cohort study and Bridget Davidson, the project manager. We also appreciate the statistical expertise of Anastasia Teterina. Funding was provided by the Canadian Nutrition Society after receiving unrestricted grants from Abbott Laboratories, Baxter, Fresenius-Kabi Canada, Nestlé Health Science and Pfizer. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
HK, GL, AJ, DD, LM and JK have been on Speakers Bureau lists for Abbott Laboratories and/or Nestlé Health Sciences for the past 2 years. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Keller, H., Laporte, M., Payette, H. et al. Prevalence and predictors of weight change post discharge from hospital: a study of the Canadian Malnutrition Task Force. Eur J Clin Nutr 71, 766–772 (2017). https://doi.org/10.1038/ejcn.2016.277
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2016.277