Abstract
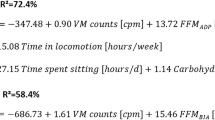
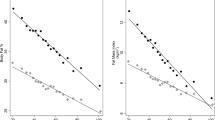
It is well documented that meeting moderate-to-vigorous physical activity guidelines of 150 min per week is protective against chronic disease, and this is likely explained by higher energy expenditure (EE). In opposition, sedentary behavior (low EE) seems to impair health outcomes. There are gold standard methods to measure EE such as the doubly labeled water (DLW) or calorimetry. These methods are highly expensive and rely on complex techniques. Motion sensors present a good alternative to estimate EE and have been validated against these reference methods. This review summarizes findings from previous reviews and the most recently published studies on the validity of different motion sensors to estimate physical activity energy expenditure (PAEE) and total energy expenditure (TEE) against DLW, and whether adding other indicators may improve these estimations in children and adults. Regardless of the recognized validity of motion sensors to estimate PAEE and TEE at the group level, individual bias is very high even when combining biometric or physiological indicators. In children, accelerometers explained 13% of DLW’s PAEE variance and 31% of TEE variance. In adults, DLW’s explained variance was higher, 29 and 44% for PAEE and TEE, respectively. There is no ideal device, but identifying postures seems to be relevant for both children and adults’ PAEE estimates. The variance associated with the number of methodological choices that these devices require invite investigators to work with the raw data in order to standardize all these procedures and potentiate the accelerometer signal-derived information. Models that consider biometric covariates seem only to improve TEE estimations, but adding heart rate enhances PAEE estimations in both children and adults.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Pinheiro Volp AC, Esteves de Oliveira FC, Duarte Moreira Alves R, Esteves EA, Bressan J . Energy expenditure: components and evaluation methods. Nutr Hosp 2011; 26: 430–440.
Hills AP, Mokhtar N, Byrne NM . Assessment of physical activity and energy expenditure: an overview of objective measures. Front Nutr 2014; 1: 5.
Sanders JP, Loveday A . Devices for self-monitoring sedentary time or physical activity: a scoping review. J Med Internet Res 2016; 18: e90.
Coward WA . Stable isotopic methods for measuring energy expenditure. The doubly-labelled-water (2H2(18)O) method: principles and practice. Proc Nutr Soc 1988; 47: 209–218.
Westerterp KR . Physical activity and physical activity induced energy expenditure in humans: measurement, determinants, and effects. Front Physiol 2013; 4: 90.
de Graauw SM, de Groot JF, van Brussel M, Streur MF, Takken T . Review of prediction models to estimate activity-related energy expenditure in children and adolescents. Int J Pediatr 2010; 2010: 489304.
Bailey RC, Olson J, Pepper SL, Porszasz J, Barstow TJ, Cooper DM . The level and tempo of children's physical activities: an observational study. Med Sci Sports Exerc 1995; 27: 1033–1041.
Crouter SE, Churilla JR, Bassett DR Jr . Estimating energy expenditure using accelerometers. Eur J Appl Physiol 2006; 98: 601–612.
Barnett A, Cerin E, Vandelanotte C, Matsumoto A, Jenkins D . Validity of treadmill- and track-based individual calibration methods for estimating free-living walking speed and VO2 using the Actigraph accelerometer. BMC Sports Sci Med Rehabil 2015; 7: 29.
Crouter SE, Clowers KG, Bassett DR Jr . A novel method for using accelerometer data to predict energy expenditure. J Appl Physiol 2006; 100: 1324–1331.
van Hees VT, Gorzelniak L, Dean León EC, Eder M, Pias M, Taherian S et al. Separating movement and gravity components in an acceleration signal and implications for the assessment of human daily physical activity. PLoS One 2013; 8: e61691.
Rothney MP, Neumann M, Beziat A, Chen KY . An artificial neural network model of energy expenditure using nonintegrated acceleration signals. J Appl Physiol 2007; 103: 1419–1427.
Montoye AH, Mudd LM, Biswas S, Pfeiffer KA . Energy expenditure prediction using raw accelerometer data in simulated free living. Med Sci Sports Exerc 2015; 47: 1735–1746.
Ellis K, Kerr J, Godbole S, Lanckriet G, Wing D, Marshall S . A random forest classifier for the prediction of energy expenditure and type of physical activity from wrist and hip accelerometers. Physiol Meas 2014; 35: 2191–2203.
Staudenmayer J, He S, Hickey A, Sasaki J, Freedson P . Methods to estimate aspects of physical activity and sedentary behavior from high-frequency wrist accelerometer measurements. J Appl Physiol 2015; 119: 396–403.
Bonomi AG, Goris AH, Yin B, Westerterp KR . Detection of type, duration, and intensity of physical activity using an accelerometer. Med Sci Sports Exerc 2009; 41: 1770–1777.
Fairclough SJ, Noonan R, Rowlands AV, Van Hees V, Knowles Z, Boddy LM . Wear compliance and activity in children wearing wrist- and hip-mounted accelerometers. Med Sci Sports Exerc 2016; 48: 245–253.
Skender S, Ose J, Chang-Claude J, Paskow M, Brühmann B, Siegel EM et al. Accelerometry and physical activity questionnaires - a systematic review. BMC Public Health 2016; 16: 515.
Matthews CE, Hagstromer M, Pober DM, Bowles HR . Best practices for using physical activity monitors in population-based research. Med Sci Sports Exerc 2012; 44: S68–S76.
Jeran S, Steinbrecher A, Pischon T . Prediction of activity-related energy expenditure using accelerometer-derived physical activity under free-living conditions: a systematic review. Int J Obes 2016; 40: 1187–1197.
Plasqui G, Bonomi AG, Westerterp KR . Daily physical activity assessment with accelerometers: new insights and validation studies. Obes Rev 2013; 14: 451–462.
Murakami H, Kawakami R, Nakae S, Nakata Y, Ishikawa-Takata K, Tanaka S et al. Accuracy of wearable devices for estimating total energy expenditure: comparison with metabolic chamber and doubly labeled water method. JAMA Intern Med 2016; 176: 702–703.
Leenders NY, Sherman WM, Nagaraja HN . Energy expenditure estimated by accelerometry and doubly labeled water: do they agree? Med Sci Sports Exerc 2006; 38: 2165–2172.
Sasaki JE, Hickey AM, Staudenmayer JW, John D, Kent JA, Freedson PS . Performance of activity classification algorithms in free-living older adults. Med Sci Sports Exerc 2016; 48: 941–950.
Rowlands AV, Yates T, Olds TS, Davies M, Khunti K, Edwardson CL . Sedentary sphere: wrist-worn accelerometer-brand independent posture classification. Med Sci Sports Exerc 2016; 48: 748–754.
Nguyen A, Moore D, McCowan I . Unsupervised clustering of free-living human activities using ambulatory accelerometry. Conference proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference 2007; 23-26 August 2007; Lyon, France, pp 4895-4898.
Zhang K, Werner P, Sun M, Pi-Sunyer FX, Boozer CN . Measurement of human daily physical activity. Obes Res 2003; 11: 33–40.
Lof M . Physical activity pattern and activity energy expenditure in healthy pregnant and non-pregnant Swedish women. Eur J Clin Nutr 2011; 65: 1295–1301.
Brazeau AS, Beaudoin N, Belisle V, Messier V, Karelis AD, Rabasa-Lhoret R . Validation and reliability of two activity monitors for energy expenditure assessment. J Sci Med Sport 2016; 19: 46–50.
Correa JB, Apolzan JW, Shepard DN, Heil DP, Rood JC, Martin CK . Evaluation of the ability of three physical activity monitors to predict weight change and estimate energy expenditure. Appl Physiol Nutr Metab 2016; 41: 758–766.
Ekelund U, Yngve A, Brage S, Westerterp K, Sjostrom M . Body movement and physical activity energy expenditure in children and adolescents: how to adjust for differences in body size and age. Am J Clin Nutr 2004; 79: 851–856.
Corder K, Ekelund U, Steele RM, Wareham NJ, Brage S . Assessment of physical activity in youth. J Appl Physiol 2008; 105: 977–987.
Schoeller DA, Jefford G . Determinants of the energy costs of light activities: inferences for interpreting doubly labeled water data. Int J Obes Relat Metab Disord 2002; 26: 97–101.
Crouter SE, Churilla JR, Bassett DR Jr . Accuracy of the Actiheart for the assessment of energy expenditure in adults. Eur J Clin Nutr 2008; 62: 704–711.
Brage S, Brage N, Franks PW, Ekelund U, Wareham NJ . Reliability and validity of the combined heart rate and movement sensor Actiheart. Eur J Clin Nutr 2005; 59: 561–570.
Silva AM, Santos DA, Matias CN, Judice PB, Magalhaes JP, Ekelund U et al. Accuracy of a combined heart rate and motion sensor for assessing energy expenditure in free-living adults during a double-blind crossover caffeine trial using doubly labeled water as the reference method. Eur J Clin Nutr 2015; 69: 20–27.
Santos DA, Silva AM, Matias CN, Magalhaes JP, Fields DA, Minderico CS et al. Validity of a combined heart rate and motion sensor for the measurement of free-living energy expenditure in very active individuals. J Sci Med Sport 2014; 17: 387–393.
Assah FK, Ekelund U, Brage S, Wright A, Mbanya JC, Wareham NJ . Accuracy and validity of a combined heart rate and motion sensor for the measurement of free-living physical activity energy expenditure in adults in Cameroon. Int J Epidemiol 2011; 40: 112–120.
Brage S, Westgate K, Franks PW, Stegle O, Wright A, Ekelund U et al. Estimation of free-living energy expenditure by heart rate and movement sensing: a Doubly-Labelled Water Study. PLoS One 2015; 10: e0137206.
Villars C, Bergouignan A, Dugas J, Antoun E, Schoeller DA, Roth H . Validity of combining heart rate and uniaxial acceleration to measure free-living physical activity energy expenditure in young men. J Appl Physiol 2012; 113: 1763–1771.
Judice PB, Santos DA, Hamilton MT, Sardinha LB, Silva AM . Validity of GT3X and actiheart to estimate sedentary time and breaks using ActivPAL as the reference in free-living conditions. Gait Posture 2015; 41: 917–922.
Shephard RJ, Tudor-Locke C (eds). The Objective Monitoring of Physical Activity: Contributions of Accelerometry to Epidemiology, Exercise Science and Rehabilitation, 1st edn, Springer International Publishing: Switzerland, 2016..
Lee IM, Shiroma EJ . Using accelerometers to measure physical activity in large-scale epidemiological studies: issues and challenges. Br J Sports Med 2014; 48: 197–201.
Corder K, Sharp SJ, Atkin AJ, Andersen LB, Cardon G, Page A et al. Age-related patterns of vigorous-intensity physical activity in youth: the International Children's Accelerometry Database. Prev Med Rep 2016; 4: 17–22.
Loyen A, Van Hecke L, Verloigne M, Hendriksen I, Lakerveld J, Steene-Johannessen J et al. Variation in population levels of physical activity in European adults according to cross-European studies: a systematic literature review within DEDIPAC. Int J Behav Nutr Phys Act 2016; 13: 72.
Acknowledgements
This research was supported by the Interdisciplinary Center for the Study of Human Performance—Portuguese Science and Technology Foundation.
Author contributions
All authors meet the criteria for authorship stated in the Uniform Requirements Submitted to Biomedical Journals. PBJ and LBS were involved in interpreting the results of the analysis and critically reviewed the manuscript. All authors approved the final version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Clinical Nutrition website
Supplementary information
Rights and permissions
About this article
Cite this article
Sardinha, L., Júdice, P. Usefulness of motion sensors to estimate energy expenditure in children and adults: a narrative review of studies using DLW. Eur J Clin Nutr 71, 331–339 (2017). https://doi.org/10.1038/ejcn.2017.2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2017.2
This article is cited by
-
Compensatory mechanisms from different exercise intensities in type 2 diabetes: a secondary analysis of a 1-year randomized controlled trial
Acta Diabetologica (2023)
-
Total energy expenditure among children with motor, intellectual, visual, and hearing disabilities: a doubly labeled water method
European Journal of Clinical Nutrition (2021)
-
The validity of two widely used commercial and research-grade activity monitors, during resting, household and activity behaviours
Health and Technology (2020)
-
Response to ‘The importance of nuance in statements about methods for human energy expenditure estimation that use motion sensors’
European Journal of Clinical Nutrition (2017)
-
The importance of nuance in statements about methods for human energy expenditure estimation that use motion sensors
European Journal of Clinical Nutrition (2017)