Abstract
Background/Objective:
The present study evaluated the mental health and psychological functioning of bariatric patients before surgery, and after 1 year and 10 year follow-ups, and compared them with participants in a dietary program. Such long follow-up is rare, but strongly recommended by the American Association of Bariatric Surgeons.
Subjects/Methods:
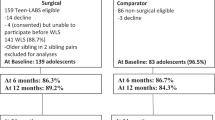
Thirty-six bariatric surgery patients and 34 participants of a weight loss program were weighed and assessed at all 3 points in time. Participants were administered the mental health inventory, neuroticism, sense of control and fear of intimacy scales. Along with these mental and psychological measurements, the medical outcome short form (SF-36) was used.
Results:
The surgery group achieved successful weight loss outcomes (27% reduction of pre-operative weight) after 10 years and better than baseline health-related quality-of-life scores. However, their general mental health, neuroticism, sense of control and fear of intimacy scores showed significant deterioration in comparison to pre-operative levels after 10 years. The dietary group participants remained psychologically stable among all three points in time.
Conclusions:
This study highlights the importance of identifying a risk group among bariatric patients for which the dietary and psychological follow-up may be of special significance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Canetti L, Elizur Y, Karni Y, Berry EM . Health-related quality of life changes and weight reduction after bariatric surgery vs. a weight-loss program. Isr J Psychiatry Relat Sci 2013; 50: 194–201.
Mamplekou E, Komesidou V, Bissias C, Papakonstantinou A, Melissas J . Psychological condition and quality of life in patients with morbid obesity before and after surgical weight loss. Obes Surg 2005; 15: 1177–1184.
American Society for Bariatric Surgery, Society of American Gastrointestinal Endoscopic Surgeons. Guidelines for laparoscopic and open surgical treatment of morbid obesity. Obes Surg 2000; 10: 378–379.
Sarwer DB, Wadden TA, Fabricatore AN . Psychosocial and behavioral aspects of bariatric surgery. Obes Res 2005; 13: 639–648.
Julia C, Ciangura C, Capuron L, Bouillot J-L, Basdevant A, Poitou C et al. Quality of life after Roux-en-Y gastric bypass and changes in body mass index and obesity-related comorbidities. Diabetes Metab 2013; 39: 148–154.
O’Brien PE, Dixon JB, Laurie C, Skinner S, Proietto J, McNeil J et al. Treatment of mild to moderate obesity with laparoscopic adjustable gastric banding or an intensive medical program: a randomized trial. Ann Intern Med 2006; 144: 625–633.
O’Brien PE, Sawyer SM, Laurie C, Brown WA, Skinner S, Veit F et al. Laparoscopic adjustable gastric banding in severely obese adolescents: a randomized trial. J Am Med Assoc 2010; 303: 519–526.
Pories WJ . The surgical approach to morbid obesity. In: Sabiston DC (ed) Textbook of Surgery. Saunders: Philadelphia, 1991, pp 851–865.
Waters GS, Pories WJ, Swanson MS, Meelheim HD, Flickinger EG, May HJ et al. Long-Term studies of mental health after the Greenville gastric bypass operation for morbid obesity. Am J Surg 1991; 161: 154–158.
Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 1995; 222: 339–352.
Mitchell J . Alcohol Use/Abuse and Other Problematic Behaviors that may complicate the post-operative period. International Conference on Eating Disorders at New York; March 2014, Academy of Eating Disorders: New York, NY, USA, 2014.
Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD et al. Long-term mortality after gastric bypass surgery. N Engl J Med 2007; 357: 753–761.
Tindle HA, Omalu B, Courcoulas A, Marcus M, Hammers J, Kuller LH . Risk of suicide after long-term follow-up from bariatric surgery. Am J Med 2010; 123: 1036–1042.
Hsu LK, Benotti PN, Dwyer J, Roberts SB, Saltzman E, Shikora S et al. Nonsurgical factors that influence the outcome of bariatric surgery: A review. Psychosom Med 1998; 60: 338–346.
Peterhänsel C, Petroff D, Klinitzke G, Kersting A, Wagner B . Risk of completer suicide after bariatric surgery: a systematic review. Obes Rev 2013; 14: 369–382.
King WC, Chen JY, Mitchell JE, Kalarchian MA, Steffen KJ, Engel SG et al. Prevalence of alcohol use disorders before and after bariatric surgery. J Am Med Assoc 2012; 307: 2516–2525.
Conason A, Teixeira J, Hsu C-H, Puma L, Knafo D, Geliebter A . Substance use following bariatric weight loss surgery. JAMA Surg 2013; 148: 145–150.
Herpertz S, Tanja L, Burgmer R, Crosby R, De Zwaan M, Müller A . Weight loss and psychological functioning 9 years after bariatric surgery results from the multicentre, prospective essen-bochum university treatment study (EBOTS). Psychosom Med 2014; 76: A-64.
Mitchell JE, King WC, Chen J-Y, Devlin MJ, Flum D, Garcia L et al. Course of depressive symptoms and treatment in the longitudinal assessment of bariatric surgery (LABS-2) study. Obesity 2014; 22: 1799–1806.
Veit CT, Ware JE . The structure of psychological stress and well-being in general populations. J Consul Clin Psychol 1983; 51: 730–742.
Costa PT Jr, McCrae RR . Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factors Inventory (NEO-FFI), Professional Manual. Psychological Assessment Resources: Odessa, FL, USA, 1992.
Lahey BB . Public health significance of neuroticism. Am Psychol 2009; 64: 241–256.
Shapiro DH, Blinder BJ, Hagman J, Pituck S . A psychological “sense-of-control” profile of patients with anorexia nervosa and bulimia nervosa. Psychol Rep 1993; 73: 531–541.
Stutzer A Limited self-control, obesity and the loss of happiness. University of Basel and IZA: Bonn, Germany, 2007. IZA Discussion Papers, No. 2925..
Slochower J, Kaplan SP . Anxiety, perceived control and eating in obese and normal weight persons. Appetite 1980; 1: 75–83.
Ogden J, Clementi C, Aylwin S . The impact of obesity surgery and the paradox of control: A qualitative study. Psychol Health 2006; 21: 273–293.
William AL, Merten MJ . Romantic relationships among women experiencing obesity: Self-perception and weight as barriers to intimacy. Fam Consum Sci Res J 2013; 41: 284–298.
Sklar EM The relationship of fear of intimacy, body image avoidance and body mass index. FIU Electronic Theses and Dissertations, Florida international university, Miami, FL, USA. 2008..
Shapiro DH Manual for the Shapiro Control Inventory (SCI). Behaviordyne, Palo Alto, CA, USA, 1994.
Descutner CJ, Thelen MH . Development and validation of a Fear-of-Intimacy Scale. Psychol Assess 1991; 3: 218–225.
Ware JE, Sherbourne CD . The MOS 36-item short-form health survey (SF-36). I, Conceptual framework and item selection. Med Care 1992; 30: 473–481.
Florian V, Drory I, Mental Health Inventory (MHI). Psychometric properties and normative data in the Israeli population. Psychol 1990; 2: 26–35. (Hebrew).
Montag I, Levin J . The five-factor model and psychopathology in nonclinical samples. Pers Individ Dif 1994; 17: 1–7.
Taubman-Ben-Ari O . Intimacy and risky sexual behavior. Death Stud 2004; 28: 865–887.
Lewin-Epstein N, Sagiv-Shifter T, Shabtai EL, Shmueli A . Validation of the SF-36-Item Short-Form health survey (Hebrew version) in the adult population of Israel. Med Care 1998; 36: 1361–1370.
Cohen J . Statistical Power Analysis for the Behavioral Sciences. Academic Press: New York, NY, USA, 1978.
Karlsson J, Taft C, Rydén A, Sjöström L, Sullivan M . Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: the SOS intervention study. Int J Obes 2007; 31: 1248–1261.
Fobi MA . Surgical treatment of obesity: a review. J Natl Med Assoc 2004; 96: 61–75.
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K et al. Bariatric surgery: a systematic review and meta-analysis. J Am Med Assoc 2004; 292: 1724–1737.
Kruseman M, Leimgruber A, Zumbach F, Golay A . Dietary, weight, and psychological changes among patients with obesity, 8 years after gastric bypass. J Am Diet Assoc 2010; 110: 527–534.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Clinical Nutrition website
Rights and permissions
About this article
Cite this article
Canetti, L., Bachar, E. & Bonne, O. Deterioration of mental health in bariatric surgery after 10 years despite successful weight loss. Eur J Clin Nutr 70, 17–22 (2016). https://doi.org/10.1038/ejcn.2015.112
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2015.112
This article is cited by
-
Personality trait associations with quality-of-life outcomes following bariatric surgery: a systematic review
Health and Quality of Life Outcomes (2023)
-
Taste receptor type 1 member 3 enables western diet-induced anxiety in mice
BMC Biology (2023)
-
Patient-Reported Outcomes and Quality of Life After Single-Anastomosis Duodeno-ileal Bypass with Sleeve Gastrectomy (SADI-S): a Cross-Sectional Study with 283 Patients from a Single Institution
Obesity Surgery (2023)
-
From Weight Bias Internalization to Health-Related Quality of Life: Self-esteem and Psychopathology in Pre-bariatric Surgery Patients
Obesity Surgery (2022)
-
Psychopathology predicts mental but not physical bariatric surgery outcome at 3-year follow-up: a network analysis study
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2022)