Abstract
Background/Objectives:
The association of dietary sodium and cardiovascular disease (CVD), as well as the reduction of sodium intake in the prevention of CVD, has been under debate. To study whether sodium consumption has a role as a risk factor for fatal and non-fatal CVD.
Subjects/Methods:
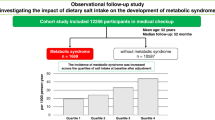
A well-defined population-based cohort of 1045 subjects collected between 1991 and 1993 (mean age 51.4 years) was used with approximately 19 years’ follow-up. At the baseline, 716 subjects filled in a 1-week food follow-up diary, which was used to calculate the daily sodium intake (mg/1000 kcal).
Results:
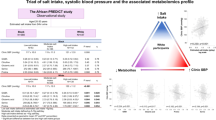
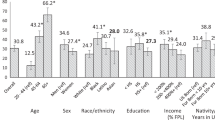
The baseline sodium intake correlated significantly with age (rs=0.117, P=0.002), BMI (rs=0.216, P=0.000), waist circumference (rs=0.268, P=0.000), smoking (rs=0.144, P=0.000), alcohol consumption (rs=0.111, P=0.003), systolic blood pressure (rs=0.106, P=0.005) and low-density lipoprotein (LDL) cholesterol (rs=0.081, P=0.033). Those who had cardiovascular events in the follow-up consumed more sodium at the baseline (mean 2010.4 mg/1000 kcal/day, s.d. 435.2, n=101) compared with the subjects without events (mean 1849.9 mg/1000 kcal/day, s.d. 361.2, n=589; t-test; P=0.001). The incidence of cardiovascular events was greater in the highest quartile (22.1%) than in the lower quartiles (first 11.0%, second 9.9% and third 15.6%; X2; P=0.005). Cox regression analysis showed that sodium intake as a continuous variable predicts CVD events (P=0.031) independently when age, sex, smoking, alcohol consumption, systolic blood pressure, LDL cholesterol and waist circumference were added as covariates. This predictive role is seen especially in the group of subjects on hypertensive medication (P=0.001).
Conclusions:
Dietary sodium intake is a significant independent predictor of cardiovascular events in the study population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Susic D, Frohlich ED . Salt consumption and cardiovascular, renal, and hypertensive diseases: clinical and mechanistic aspects. Curr Opin Lipidol 2012; 23: 11–16.
Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP . Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ 2009; 339: b4567.
Umesawa M, Iso H, Date C, Yamamoto A, Toyoshima H, Watanabe Y et al. Relations between dietary sodium and potassium intakes and mortality from cardiovascular disease: the Japan Collaborative Cohort Study for Evaluation of Cancer Risks. Am J Clin Nutr 2008; 88: 195–202.
Leenen FH, Yuan B . Dietary-sodium-induced cardiac remodeling in spontaneously hypertensive rat versus Wistar-Kyoto rat. J Hypertens 1998; 16: 885–892.
Alam S, Johnson AG . A meta-analysis of randomised controlled trials (RCT) among healthy normotensive and essential hypertensive elderly patients to determine the effect of high salt (NaCl) diet of blood pressure. J Hum Hypertens 1999; 13: 367–374.
Cutler JA, Follmann D, Allender PS . Randomized trials of sodium reduction: an overview. Am J Clin Nutr 1997; 65: 643S–651S.
Cutler JA, Follmann D, Elliott P, Suh I . An overview of randomized trials of sodium reduction and blood pressure. Hypertension 1991; 17: I27–I33.
He FJ, MacGregor GA . Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens 2002; 16: 761–770.
He FJ, MacGregor GA . Importance of salt in determining blood pressure in children: meta-analysis of controlled trials. Hypertension 2006; 48: 861–869.
Law MR, Frost CD, Wald NJ . By how much does dietary salt reduction lower blood pressure? III—Analysis of data from trials of salt reduction. BMJ 1991; 302: 819–824.
Midgley JP, Matthew AG, Greenwood CM, Logan AG . Effect of reduced dietary sodium on blood pressure: a meta-analysis of randomized controlled trials. JAMA 1996; 275: 1590–1597.
Jula A, Ronnemaa T, Rastas M, Karvetti RL, Maki J . Long-term nopharmacological treatment for mild to moderate hypertension. J Intern Med 1990; 227: 413–421.
Rantala AO, Kauma H, Lilja M, Savolainen MJ, Reunanen A, Kesaniemi YA . Prevalence of the metabolic syndrome in drug-treated hypertensive patients and control subjects. J Intern Med 1999; 245: 163–174.
Silaste ML, Junes R, Rantala AO, Kauma H, Lilja M, Savolainen MJ et al. Dietary and other non-pharmacological treatments in patients with drug-treated hypertension and control subjects. J Intern Med 2000; 247: 318–324.
Rastas M, Seppänen R, Knuts L, Karvetti R, Varo P . Nutrient Composition of Foods. Publications of the Social Insurance Institution: Helsinki, 1993.
Khavari KA, Farber PD . A profile instrument for the quantification and assessment of alcohol consumption. The Khavari Alcohol Test. J Stud Alcohol 1978; 39: 1525–1539.
American Society of Hypertension: Recommendations for routine blood pressure measurement by indirect cuff sphygmomanometry. Am J Hypertens 1992; 5: 207–209.
Pajunen P, Jousilahti P, Borodulin K, Harald K, Tuomilehto J, Salomaa V . Body fat measured by a near-infrared interactance device as a predictor of cardiovascular events: the FINRISK'92 cohort. Obesity (Silver Spring) 2011; 19: 848–852.
Forster JL, Jeffery RW, VanNatta M, Pirie P . Hypertension prevention trial: do 24-h food records capture usual eating behavior in a dietary change study? Am J Clin Nutr 1990; 51: 253–257.
Mertz W, Tsui JC, Judd JT, Reiser S, Hallfrisch J, Morris ER et al. What are people really eating? The relation between energy intake derived from estimated diet records and intake determined to maintain body weight. Am J Clin Nutr 1991; 54: 291–295.
Pietinen P . Estimating sodium intake from food consumption data. Ann Nutr Metab 1982; 26: 90–99.
Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ . Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ 2013; 346: f1326.
Oparil S . Low sodium intake—cardiovascular health benefit or risk? N Engl J Med 2014; 371: 677–679.
Graudal NA, Hubeck-Graudal T, Jürgens G . Effects of low-sodium diet vs. high-sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride (Cochrane Review). Am J Hypertens 2012; 25: 1–15.
Tuomilehto J, Jousilahti P, Rastenyte D, Moltchanov V, Tanskanen A, Pietinen P et al. Urinary sodium excretion and cardiovascular mortality in Finland: a prospective study. Lancet 2001; 357: 848–851.
Tunstall-Pedoe H, Woodward M, Tavendale R, A'Brook R, McCluskey MK . Comparison of the prediction by 27 different factors of coronary heart disease and death in men and women of the Scottish Heart Health Study: cohort study. BMJ 1997; 315: 722–729.
Ikehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Inaba Y et alJACC Study Group. Salt preference and mortality from stroke and coronary heart disease for Japanese men and women: the JACC study. Prev Med 2012; 54: 32–37.
Li XY, Cai XL, Bian PD, Hu LR . High salt intake and stroke: meta-analysis of the epidemiologic evidence. CNS Neurosci Ther 2012; 18: 691–701.
Nagata C, Takatsuka N, Shimizu N, Shimizu H . Sodium intake and risk of death from stroke in Japanese men and women. Stroke 2004; 35: 1543–1547.
Sasaki S, Zhang XH, Kesteloot H . Dietary sodium, potassium, saturated fat, alcohol, and stroke mortality. Stroke 1995; 26: 783–789.
He J, Gu D, Chen J, Jaquish CE, Rao DC, Hixson JE et al. Gender difference in blood pressure responses to dietary sodium intervention in the GenSalt study. J Hypertens 2009; 27: 48–54.
Acknowledgements
This work was supported by the Finnish Foundation for Cardiovascular Research.
Author Contributions
The authors’ responsibilities were as follows: OU and YAK designed research; MS, OU and YAK conducted research; M-LS analyzed the dietary data; MS and MÄ analyzed the data; RB supervised the performing of statistical analyses; MÄ, EM, YAK and OU wrote the paper and all authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Äijälä, M., Malo, E., Santaniemi, M. et al. Dietary sodium intake and prediction of cardiovascular events. Eur J Clin Nutr 69, 1042–1047 (2015). https://doi.org/10.1038/ejcn.2015.40
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2015.40
This article is cited by
-
The association of carotid artery atherosclerosis with the estimated excretion levels of urinary sodium and potassium and their ratio in Chinese adults
Nutrition Journal (2021)
-
Urinary sodium excretion and risk of cardiovascular disease in the Chinese population: a prospective study
Hypertension Research (2018)