Abstract
Background/Objectives:
Limited data exist regarding breakfast consumption and its association with cardiovascular disease (CVD) risk factors. This study investigates the relationship between breakfast routine and CVD risk factors in a multinational sample.
Subjects/Methods:
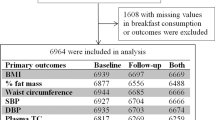
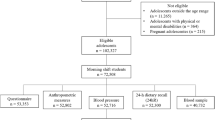
Cross-sectional data from eight European countries participating in the IDEFICS (Identification and prevention of dietary- and lifestyle-induced health effects in children and infants) survey (2007–2008) were used. The sample included ;children 2 to <10 years of age (n=8863, 51.2% boys). The Mann–Whitney ;U-test and logistic regression were used to assess CVD risk factors ;among ;no breakfast (NBrH), occasional breakfast and daily breakfast at home (DBrH) consumption.
Results:
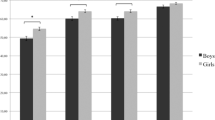
Male school-aged NBrH consumers, ;compared with ;DBrH consumers, ;were more likely to be overweight/obese (odds ratio (OR): 1.37, 95% confidence interval (CI)=1.05–1.79), to have higher risk for high-density lipoprotein (HDL) cholesterol levels lower than 40 mg/dl (OR: 1.69, 95% CI=1.24–2.30), triglycerides (TG) above 75 mg/dl (OR: 1.65, 95% CI=1.24–2.19) and sum of skinfolds greater than the 90th percentile (OR: 1.32, 95% CI=1.0–1.76). Female school-aged NBrH consumers ;compared with ;DBrH consumers ;had a higher risk for waist circumference greater than the 90th percentile (OR: 1.70, 95% CI=1.14–2.51), HDL cholesterol levels lower than 40 mg/dl (OR: 1.65, 95% CI=1.23–2.21), TG above 75 mg/dl (OR: 1.65, 95% CI=1.26–2.17) and total cholesterol/HDL cholesterol ratio >3.5 (OR: 1.39, 95% CI=1.09–1.77). Results remained significant after adjusting for daily physical activity in moderate-to-vigorous physical activity (MVPA) periods (in min/day). Male DBrH consumers, 6 to <10 years of age, had longer daily periods of MVPA compared with ;NBrH consumers ;(32.0±21.4 vs 27.5±18.8, P<0.05). For preschoolers, breakfast consumption was negatively associated with ;CVD risk factors but results of regression models were mostly insignificant.
Conclusions:
Daily breakfast consumption contributes to controlling school-aged children’s weight ;and lipid profile and promotes higher PA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Hayman LL, Williams CL, Daniels SR, Steinberger J, Paridon S, Dennison BA et al. Cardiovascular health promotion in the schools: a statement for health and education professionals and child health advocates from the Committee on Atherosclerosis, Hypertension, and Obesity in Youth (AHOY) of the Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 2004; 110: 2266–2275.
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 2011; 128: S213–S256.
Rampersaud GC, Pereira MA, Girard BL, Adams J, Metzl JD . Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc 2005; 105: 743–760.
Deshmukh-Taskar PR, Nicklas TA, O'Neil CE, Keast DR, Radcliffe JD, Cho S . The relationship of breakfast skipping and type of breakfast consumption with nutrient intake and weight status in children and adolescents: the National Health and Nutrition Examination Survey 1999-2006. J Am Diet Assoc 2010; 110: 869–878.
Utter J, Scragg R, Mhurchu CN, Schaaf D . At-home breakfast consumption among New Zealand children: associations with body mass index and related nutrition behaviors. J Am Diet Assoc 2007; 107: 570–576.
Albertson AM, Affenito SG, Bauserman R, Holschuh NM, Eldridge AL, Barton BA . The relationship of ready-to-eat cereal consumption to nutrient intake, blood lipids, and body mass index of children as they age through adolescence. J Am Diet Assoc 2009; 109: 1557–1565.
Kafatos A, Linardakis M, Bertsias G, Mammas I, Fletcher R, Bervanaki F . Consumption of ready-to-eat cereals in relation to health and diet indicators among school adolescents in Crete, Greece. Ann Nutr Metab 2005; 49: 165–172.
Resnicow K . The relationship between breakfast habits and plasma cholesterol levels in schoolchildren. J Sch Health 1991; 61: 81–85.
Sandercock GR, Voss C, Dye L . Associations between habitual school-day breakfast consumption, body mass index, physical activity and cardiorespiratory fitness in English schoolchildren. Eur J Clin Nutr 2010; 64: 1086–1092.
Di Giuseppe R, Di Castelnuovo A, Melegari C, De Lucia F, Santimone I, Sciarretta A et al. Typical breakfast food consumption and risk factors for cardiovascular disease in a large sample of Italian adults. Nutr Metab Cardiovasc Dis 2012; 22: 347–354.
Hallström L, Labayen I, Ruiz JR, Patterson E, Vereecken CA, Breidenassel C et al. Breakfast consumption and CVD risk factors in European adolescents: the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) Study. Public Health Nutr 2012; 12: 1–10.
Freitas Júnior IF, Christofaro DG, Codogno JS, Monteiro PA, Silveira LS, Fernandes RA . The association between skipping breakfast and biochemical variables in sedentary obese childrenand adolescents. J Pediatr 2012; 161: 871–874.
Corder K, van Sluijs EM, Ridgway CL, Steele RM, Prynne CJ, Stephen AM et al. Breakfast consumption and physical activity in adolescents: daily associations and hourly patterns. Am J Clin Nutr 2013; 99: 361–368.
Schembre SM, Wen CK, Davis JN, Shen E, Nguyen-Rodriguez ST, Belcher BR et al. Eating breakfast more frequently is cross-sectionally associated with greater physical activity and lower levels of adiposity in overweight Latina and African American girls. Am J Clin Nutr 2013; 98: 275–281.
Cuenca-García M, Ruiz JR, Ortega FB, Labayen I, González-Gross M, Moreno LA et al. Association of breakfast consumption with objectively measured and self-reported physical activity, sedentary time and physical fitness in European adolescents: the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) Study. Public Health Nutr 2013; 11: 1–11.
Lyerly JE, Huber LR, Warren-Findlow J, Racine EF, Dmochowski J . Is breakfast skipping associated with physical activity among US adolescents? A cross-sectional study of adolescents aged 12-19 years, National Health and Nutrition Examination Survey (NHANES). Public Health Nutr 2013; 27: 1–10.
Ahrens W, Bammann K, Siani A, Buchecker K, De Henauw S, Iacoviello L et al. The IDEFICS cohort: design, characteristics and participation in the baseline survey. Int J Obes (Lond) 2011; 35: S3–15.
Lanfer A, Hebestreit A, Ahrens W, Krogh V, Sieri S, Lissner L et al. Reproducibility of food consumption frequencies derived from the Children's Eating Habits Questionnaire used in the IDEFICS study. Int J Obes (Lond) 2011; 1: S61–S68.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1240–1243.
Mc Dowell MA, Fryar D, Hirsch R, Ogden CL . Anthropometric reference data for Children and adults: U.S. Population, 1999-2002. Adv Data 2005; 361: 1–5.
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z et al. 2000. CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 2002; 246: 1–190.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004; 114: 555–576.
Peplies J, Günther K, Bammann K, Fraterman A, Russo P, Veidebaum T et al. Influence of sample collection and preanalytical sample processing on the analyses of biological markers in the European multicentre study IDEFICS. Int J Obes (Lond) 2011; 35: S104–S112.
Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG . Calibration of two objective measures of physical activity for children. J Sports Sci 2008; 26: 1557–1565.
United Nations Educational Scientific and Cultural Organization International Standard Classification of Education (ISCED). 2006. http://www.uis.unesco.org/Education/Pages/international-standard-classification-of-education.aspx (accessed 2 February 2012).
Takasaki Y . Serum lipid levels and factors affecting atherogenic index in Japanese children. J Physiol Anthropol Appl Human Sci 2005; 24: 511–515.
Moschonis G, Mavrogianni C, Karatzi K, Iatridi V, Chrousos GP, Lionis C et al. Increased physical activity combined with more eating occasions is beneficial against dyslipidemias in children. The Healthy Growth Study. Eur J Nutr 2013; 52: 1135–1144.
Janz KF, Witt J, Mahoney LT . The stability of children’s physical activity as measured by accelerometry and self-report. Med Sci Sports Exerc 1995; 27: 1326–1332.
Vissers PA, Jones AP, Corder K, Jennings A, van Sluijs EM, Welch A et al. Breakfast consumption and daily physical activity in 9-10-year-old British children. Public Health Nutr 2013; 16: 1281–1290.
Pereira MA, Erickson E, McKee P, Schrankler K, Raatz SK, Lytle LA et al. Breakfast frequency and quality may affect glycemia and appetite in adults and children. J Nutr 2011; 141: 163–168.
Smith KJ, Gall SL, McNaughton SA, Blizzard L, Dwyer T, Venn AJ . Skipping breakfast: longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. Am J Clin Nutr 2010; 92: 1316–1325.
Timlin MT, Pereira MA . Breakfast frequency and quality in the etiology of adult obesity and chronic diseases. Nutr Rev 2007; 65: 268–281.
Bey L, Hamilton MT . Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol 2003; 551: 673–682.
Hamilton MT, Hamilton DG, Zderic TW . Exercise physiology versus inactivity physiology: an essential concept for understanding lipoprotein lipase regulation. Exerc Sport Sci Rev 2004; 32: 161–166.
Tin SP, Ho SY, Mak KH, Wan KL, Lam TH . Location of breakfast consumption predicts body mass index change in young Hong Kong children. Int J Obes (Lond) 2012; 36: 925–930.
de Castro JM . The time of day of food intake influences overall intake in humans. J Nutr 2004; 134: 104–111.
Acknowledgements
This study was conducted as a part of the IDEFICS study and was published on behalf of its European Consortium (http://www.idefics.eu). We gratefully acknowledge the financial support of the European Community within the Sixth RTD Framework Programme Contract no. 016181 (FOOD). We are also grateful for the support provided by school boards, headmasters, teachers, school staff and communities. We thank the IDEFICS children and their parents for participating in this extensive examination.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Papoutsou, S., Briassoulis, G., Wolters, M. et al. No breakfast at home: association with cardiovascular disease risk factors in childhood. Eur J Clin Nutr 68, 829–834 (2014). https://doi.org/10.1038/ejcn.2014.88
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.88
This article is cited by
-
Breakfast consumption among Saudi primary-school children relative to sex and socio-demographic factors
BMC Public Health (2020)
-
Healthy breakfast habits and changes in obesity-related cardiometabolic markers in children: a longitudinal analysis
European Journal of Clinical Nutrition (2020)
-
Soziale Determinanten des täglichen Frühstücksverzehrs bei Schülern in Deutschland
Prävention und Gesundheitsförderung (2018)
-
Determinant factors of physical fitness in European children
International Journal of Public Health (2016)