Abstract
Objective: The paper aims to investigate the relationships of dietary fats to subsequent coronary heart disease (CHD) mortality in men and women while taking account of other CHD-related behaviours.
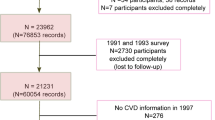
Design: A cohort of randomly selected men and women were interviewed in 1984–85 and monitored subsequently for 16 y for deaths. The interview covered health, health-related behaviours, physical measurements, socio-demographic details and a dietary questionnaire. Appropriate exclusions left 1225 men and 1451 women aged 40–75 with 98 and 57 CHD deaths, respectively. Saturated, polyunsaturated and total fat intakes were estimated.
Setting: The sample was randomly selected from households in Great Britain. The interviews took place in participants' own homes.
Results: Not consuming alcohol, smoking, not exercising and being socially disadvantaged were related to high saturated fat intake and CHD death. Cox survival analyses adjusting for these factors found that a level of saturated fat 100 g per week higher corresponded to a relative risk for CHD death for men of 1.00 (0.86–1.18) and 1.40 (1.09–1.79) for women. This difference between the effects of saturated fat in men and women was statistically significant (P=0.019). Results are also reported for total fat and the relative effects of polyunsaturated and saturated fats.
Conclusions: Strong evidence was found for the within cohort relationship of dietary fat and CHD death in women while no evidence was found for a relationship in men. Possible explanations for this are discussed.
Sponsorship: This study was supported by University of Hertfordshire using funding made available by the UK Higher Education Funding Council.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ascherio A, Rimm EB, Giovannucci EL, Spiegelman D, Stampfer M, Willett WC . 1996 Dietary fat and risk of coronary heart disease in men: cohort follow up study in the United States Br. Med. J. 313: 84–90
Bolton-Smith C, Smith WCS, Woodward M, Tunstall-Pedoe H . 1991 Nutrient intakes of different social-class groups–results from the Scottish-Heart-Health-Study (SHHS) Br. J. Nutr. 65: 321–335
Bolton-Smith C, Woodward M, Tunstall-Pedoe H . 1992 The Scottish Heart Health Study–Dietary-intake by food frequency questionnaire and odds ratios for coronary heart-disease risk. 1. The Macronutrients Eur. J. Clin. Nutr. 46: 75–84
Brousseau ME, Schaefer EJ . 2000 Diet and coronary heart disease: Clinical trials Curr. Atheroscler. Rep. 2: 487–493
Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM et al. 1989 Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART) Lancet ii: 757–761
Cox BD . 1988 Health and Lifestyle Survey, 1984–1985 [computer file] Colchester: ESRC Data Archive
Cox BD . 2001 Health and Lifestyle Survey, Deaths Data [computer file] Colchester: ESRC Data Archive
Cox DR, Oakes D . 1984 Analysis of Survival Data London: Chapman and Hall
Cox BD, Whichelow M . 1996 Ratio of waist circumference to height is better predictor of death than body mass index Br. Med. J. 313: (7070): 1487
Cox BD, Blaxter M, Buckle ALJ, Fenner NP, Golding JF, Gore M et al. 1987 The Health and Lifestyle Survey, Preliminary Report London: Health Promotion Research Trust
Cox BD, Whichelow MJ, Prevost AT . 1998 The development of cardiovascular disease in relation to anthropometric indices and hypertension in British adults Int. J. Obes. Relat. Metab. Disord. 22: 966–973
Doll R, Peto R . 1976 Mortality in relation to smoking: 20 years' observations on male British doctors Br. Med. J. 306: 437–440
Doll R, Gray R, Hafner B, Peto R . 1980 Mortality in relation to smoking: 22 years' observations on female British doctors Br. Med. J. 280: 967–971
Donohue RP, Abbott RD, Bloom E, Reed DM, Yano K . 1987 Central obesity and coronary heart disease in men Lancet i: 822–824
Duncan C, Jones K, Moon G . 1999 Smoking and deprivation: are there neighbourhood effects? Soc. Sci. Med. 48: 497–505
Egger G . 1992 The case for using waist to hip ratio measurements in routine medical checks Med. J. Aust. 156: 280–284
Esrey KL, Joseph L, Grover SA . 1996 Relationship between dietary intake and coronary heart disease mortality: lipid research clinics prevalence follow-up study J. Clin. Epidemiol. 49: 211–216
Fehily AM, Yarnell JWG, Sweetnam PM, Elwood PC . 1993 Diet and incident ischaemic heart disease: the Caerphilly Study Br. J. Nutr. 69: 303–314
Gordon T, Kagan A, Garcia-Palmieri M, Kannel WB, Zukel WJ, Tillotson J et al. 1981 Diet and its relation to coronary heart disease and death in three populations Circulation 63: 500–515
Gregory J, Foster K, Tyler H, Wiseman M . 1990 The Dietary and Nutritional Survey of British Adults London: HMSO
Hegsted DM, McGandy RB, Myers ML, Stare FJ . 1965 Quantitative effects of dietary fat on serum cholesterol in man Am. J. Clin. Nutr. 17: 281–295
Hu FB, Stampfer MJ, Manson JE et al. 1997 Dietary fat intake and the risk of coronary heart disease in women New Engl. J. Med. 337: 1491–1499
Hu FB, Stampfer MJ, Manson JE, Grodstein F, Colditz GA, Speizer FE, Willett WC . 2000 Trends in the incidence of coronary heart disease and changes in diet and lifestyle in women New Engl. J. Med. 343: 530–537
Hu FB, Manson JE, Willett WC . 2001 Types of dietary fat and risk of coronary heart disease: a critical review J. Am. Coll. Nutr. 20: 5–19
Keys A . 1980 Seven Countries: a Multivariate Analysis of Death and Coronary Heart Disease Cambridge, MA: Harvard University Press
Keys A, Anderson JT, Grande F . 1965 Serum-cholesterol response to changes in the diet Metabolism 14: 747–758
de Lezenne Kromhout D, Coulander C . 1984 Diet, prevalence and 10-year mortality from coronary heart disease in 871 middle-aged men: the Zutphen Study Am. J. Epidemiol. 119: 733–741
Kushi LH, Lew RA, Stare FJ, Ellison CR, el Lozy M, Bourke G et al. 1985 Diet and 20-year mortality from coronary heart disease: The Ireland-Boston Diet-Heart Study New Engl. J. Med. 312: 811–818
Marmot MG, Davey Smith G, Stansfeld S, Patel C, North F, Head J et al. 1991 Health inequalities among British civil servants: the Whitehall II study Lancet 337: 1387–1393
Miettinen M, Turpeinen O, Karvonen MJ, Elusuo R, Paavilainen E . 1972 Effect of cholesterol-lowering diet on mortality from coronary heart-disease and other causes Lancet ii: 835–838
Millen BE, Franz MM, Quatromoni PA, Gagnon DR, Sonnenberg LM, Ordovas JM, Wilson PWF, Schaefer EJ, Cupples LA . 1996 Diet and plasma lipids in women. 1. Macronutrients and plasma total and low-density lipoprotein cholesterol in women: The Framingham nutrition studies J. Clin. Epidemiol. 49: 657–663
Morris JN, Marr JW, Clayton DG . 1977 Diet and heart: a postscript Br. Med. J. 2: 1307–1314
Office of Population Censuses and Surveys, Social Survey Division. 1991 Dietary and Nutritional Survey of British Adults, 1986–1987 [computer file] Colchester: ESRC Data Archive
Oshaug A, Bugge KH, Bjønnes CH, Ryg M . 1995 Use of anthropometric measurements in assessing risk for coronary heart disease: a useful tool in work site health screening? Int. Arch. Occup. Environ. Health 67: 359–366
Pietinen P, Ascherio A, Korhonen P, Hartman AM, Willett WC, Albanes D, Virtamo J . 1997 Intake of fatty acids and risk of coronary heart disease in a cohort of Finnish men–the alpha-tocopherol, beta-carotene cancer prevention study Am. J. Epidemiol. 145: 876–887
Ravnskov U . 1998 The questionable role of saturated and polyunsaturated fatty acids in cardiovascular disease J. Clin. Epidemiol. 51: 443–460
Rimm EB, Giovannucci EL, Willett WC, Colditz GA, Ascherio A, Rosner B et al. 1991 Prospective study of alcohol consumption and risk of coronary disease in men Lancet 338: 464–468
Robertson TL, Kato H, Rhoads GG, Kagan A, Marmot M, Syme SL et al. 1977 Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: incidence of myocardial infarction and death from coronary heart disease Am. J. Cardiol. 39: 239–243
Royal College of Physicians, Royal College of Psychiatrists and the Royal College of General Practitioners. 1995 Alcohol and the Heart in Perspective: Sensible Limits Reaffirmed London
Sesso HD, Paffenbarger RS, Lee IM . 2000 Physical activity and coronary heart disease in men–the Harvard Alumni Health Study Circulation 102: 975–980
Shaper AG, Wannamethee G . 1991 Physical activity and ischaemic heart disease in middle-aged British men Br. Heart J. 66: 384–394
Shekelle RB, Shryock AM, Oglesby P, Lepper M, Stamler J, Liu S et al. 1981 Diet, serum cholesterol, and death from coronary heart disease: the Western Electric Study New Engl. J. Med. 304: 65–70
Stamler J, Wentworth D, Neaton JD . 1986 Is the relationship between serum cholesterol and risk of premature death from coronary heart disease continuous or graded? Findings in 356,222 primary screenees of the Multiple Risk Factor Intervention Trial (MRFIT) JAMA 256: 2823–2828
Tefft ME, Boniface DR . 2000 Estimating food and nutrient intake from food frequency questionnaire data by reference to a standard weighed diet survey J. Hum. Nutr. Diet. 13: 219–224
Truswell AS . 1994 Review of dietary intervention studies: effect on coronary events and on total mortality Aust. NZ J. Med. 24: 98–106
UK Heart Attack Study Collaborative Group. 1998 The falling mortality from CHD: a clinicopathological perspective Heart 80: 121–126
WHO. 1978 Arterial Hypertension Geneva: World Health Organization
White A, Nicolaas G, Foster K, Browne F, Carey S . 1993 Health Survey for England 1991 London: HMSO
Willett W . 1990 Nutritional Epidemiology Oxford: Oxford University Press
Willett WC, Stampfer MJ, Manson JE et al. 1993 Intake of trans fatty acids and coronary heart disease among women Lancet 341: 581–585
Yarnell JWG, Fehily AM, Milbank JE, Sweetnam PM, Walker CL . 1983 A short dietary questionnaire for use in an epidemiological survey: comparison with weighed dietary records Hum. Nutr. 37A: 103–112
Acknowledgements
We thank Brian D. Cox and Margaret J. Wichelow of the Department of Community Medicine, Institute of Public Health, University of Cambridge for their general encouragement and provision of improved age data. We also thank Craig Duncan of the University of Portsmouth and Kelvyn Jones of the University of Bristol for their provision of the local deprivation index data for the sample.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boniface, D., Tefft, M. Dietary fats and 16-year coronary heart disease mortality in a cohort of men and women in Great Britain. Eur J Clin Nutr 56, 786–792 (2002). https://doi.org/10.1038/sj.ejcn.1601509
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1601509
Keywords
This article is cited by
-
Association of dietary fatty acids and the incidence risk of cardiovascular disease in adults: the Tehran Lipid and Glucose Prospective Study
BMC Public Health (2020)
-
Dietary total fat, fatty acids intake, and risk of cardiovascular disease: a dose-response meta-analysis of cohort studies
Lipids in Health and Disease (2019)
-
The effect of replacing saturated fat with mostly n-6 polyunsaturated fat on coronary heart disease: a meta-analysis of randomised controlled trials
Nutrition Journal (2017)
-
Sample selection, recruitment and participation rates in health examination surveys in Europe – experience from seven national surveys
BMC Medical Research Methodology (2015)
-
Metabolic syndrome and dietary components are associated with coronary artery disease risk score in free-living adults: a cross-sectional study
Diabetology & Metabolic Syndrome (2011)