Abstract
To document determinants of O-demethylation in critically ill (pre)term neonates and infants, tramadol (M) and O-demethyl tramadol (M1) concentrations were quantified in eighty-six 24 h urine collections and 168 plasma samples. A significant correlation of urine log M/M1 (0.98, SD 0.66) and plasma log M/M1 (0.78, SD 0.45) with postmenstrual age (PMA) (r = −0.69 and −0.65) was observed. One-way analysis of variance documented a significant decrease in urine log and plasma log M/M1 with increasing CYP2D6 activity score (F value 11.6 and 22.55). PMA and CYP2D6 activity score determined the urine and plasma log M/M1 (R2 0.59 and 0.64) in a forward multiple regression model. We therefore conclude that PMA and CYP2D6 polymorphisms determined O-demethylation activity in (pre)term neonates and young infants, illustrating the impact of pharmacogenetics on drug metabolism in neonates although a relevant part of the interindividual varaibility remained unexplained. Besides compound-specific relevance, CYP2D6 iso-enzyme specific data on in vivo ontogeny of O-demethylation can contribute to safer and more effective administration of drugs metabolized by the same route in this population.
Similar content being viewed by others
Main
Interindividual variability in drug metabolism is based on constitution, environment, and genetics, but mainly reflects ontogeny in early life. Although the total cytochrome (CYP) content in fetal liver is 30 to 60% of adult content, iso-enzyme specific ontogeny precludes generalization of a single developmental pattern, necessitating iso-enzyme specific assessment (1). Based on observations on in vivo dextrometorphan in healthy infants and tramadol metabolism in critically ill (pre)term neonates and young infants, phenotypic activity of N-demethylation (CYP3A) displays slower increase to adult activity compared with O-demethylation (CYP2D6) (2,3). In addition to ontogeny, co-morbidity, co-medication, or polymorphisms in drug metabolizing enzymes and transporters likely further contribute to the interindividual variability of drug disposition (1,4,5).
Tramadol (M) hydrochloride is a 4-phenyl-piperidine analogue of codeine and is a racemic mixture of two enantiomers. O-demethylation of (+)-tramadol to O-(+)-demethyl tramadol (M1) is catalyzed by CYP2D6 and to a much lesser extent, by CYP2B6. Tramadol therefore provide us with a probe drug to assess phenotypic variability in O-demethylation activity. The logarithmic value of tramadol over O-demethyl tramadol (log M/M1) has been used to study in vivo CYP2D6 activity in adults, children, and neonates (6–9). Based on urine log M/M1 values, the impact of postmenstrual age (PMA) on phenotypic O-demethylation activity in 29 neonates and young infants was described, but PMA only in part explained (Radj −0.51) the interindividual variability in O-demethylation activity (8). The purpose of this study was to estimate the impact of ontogeny [PMA, postnatal age (PNA), weight] and pharmacogenetics (quantified by the CYP2D6 activity score) on interindividual variability of O-demethylation in early life, based on urine log M/M1 observed in 24 h urine collections and plasma log M/M1 observations during continuous i.v. administration of tramadol in (pre)term neonates and young infants.
METHODS
Clinical characteristics.
The study was conducted in the Gasthuisberg Neonatal Intensive Care Unit (NICU) after approval by the local ethical board. Patients were included after informed written parental consent. The decision to start tramadol was based on standardized evaluation and treatment of pain after various interventions (10). An i.v. loading dose of 2 mg/kg tramadol hydrochloride (Contramal, Grünenthal, Aachen, Germany) was administered as 30 min infusion, was followed by continuous infusion (5–8 mg/kg/24 h of tramadol hydrochloride) (11). Clinical characteristics (PMA, PNA, weight, creatinaemia) were recorded. Observations in a cohort of 29 neonates and young infants earlier reported were also included in the current analysis (8). Patients were allowed to be recruited several times only when the time interval between the end of tramadol administration and subsequent recruitment was at least 1 wk to allow washout.
Sampling strategy and analysis.
Collection of urine was started at the beginning of the i.v. loading dose and was achieved by urinary catheter or plastic collector (Urinocol Pediatrie, Braun Medical, Belgium). All urine was collected in the first 24 h after i.v. administration was started. Urine volume was recorded every 6 h and a sample (0–6, 6–12, 12–18, 18–24 h) was collected and frozen at −20°C. Following preanalytic incubation with β- glucuronidase (5 mg/mL, β-glucuronidase from bovine liver Type B-10, 10,000 units/mg, Sigma Chemical Co. cat no G-0501) in 0.5 M sodium acetate buffer pH 5, Sigma Chemical Co.-Aldrich, Bornem, Belgium), tramadol (M), O-demethyl tramadol (M1) and N-demethyl tramadol (M2) were determined by high performance liquid chromatography (8).
When an arterial line was available, blood samples (0.2 mL) were taken from 4 up to 24 h after initiation of treatment. This time interval was deliberately chosen to enable initial stabilization of the plasma log M/M1 following administration of the loading dose, based on the preliminary report on plasma and urine log M/M1 (8). Blood samples were centrifuged (3 min, 10,000 rpm) shortly after collection and samples were stored at −20°C until analysis. Plasma concentrations of tramadol and O-demethyl tramadol were determined by high performance liquid chromatography (8,11).
Pharmacogenetic analysis.
Genomic DNA was isolated from 200 μL EDTA whole blood using MagNaPure LC (Roche Diagnostics GmbH, Mannheim, Germany). The CYP2D6 2549delA variant (*3 allele, TaqMan allelic discrimination assay 4312554 (Applied Biosystems), the 1846G>A single nucleotide polymorphism (SNP) (*4 allele, DME C_27102431), the 1707delT variant (*6 allele, DME C_32407243), the 100C>T SNP (*10 allele, DME C_11484460) and the 2988G>A SNP (*41 allele, DME C_34816116) were determined using Taqman allelic discrimination assays (DME type) on a ABI Prism 7000 sequence detection system. All assays were performed on 1 ng genomic DNA, in a total reaction volume of 12.5 μL with Taqman Universal Master Mix, CYP2D6 specific primers and two allele-specific minor groove binding (MGB) probes labeled with fluorescent dyes VIC or FAM, complementary to wild type or variant sequence. The thermal profile consisted of denaturation at 95°C for 15 min, followed by 50 cycles of denaturation at 92°C for 15 s and annealing plus extension at 60°C for 1 min. Genotypes were scored by allele-specific fluorescence using SDS 2.2.2 software for allelic discrimination (Applied Biosystems). CYP2D6*9 (2613delAGA) was determined based on the PCR-RFLP method by Gaedigk et al. (12), CYP2D6*5 (gene deletion) was determined based on the method of Hersberger et al. (13), CYP2D6 gene duplication was analyzed according to Lovlie et al. (14). Genotyping analyses were classified using the CYP2D6 activity score (0, 0.5, 1, 1.5, 2, >2) (2,9). Patients in whom no specific single-nucleotide polymorphism (*3, *4, *5, *6, *9, *41, *10, *1×N) was detected were assumed to have an CYP2D6 activity score of 2 (*1/*1).
Data reporting and statistics.
Characteristics and results were reported by mean and SD (Kolmogorov-Smirnov test), otherwise by median and range or incidence.
Urine M, M1, and M2 (mg/L) were converted to tramadol molar equivalent concentrations (M = 263.38 mg/mmol; M1 = 249.38 mg/mmol; M2 = 249.38 mg/mmol). Based on these concentrations and the total urine volume, the retrieval of tramadol in the first 24 h of administration (%, mg tramadol collected/administered) and the log urine M/M1 (0–6, 6–12, 12–18, 18–24 h and 0–24 h) were calculated. One-way analysis of variance (ANOVA) and Newman-Keuls post hoc test were used to assess the impact of consecutive time intervals of urine collection on the urine log M/M1.
Correlations (Spearman) between PMA, PNA, or weight and the 24 h urine log M/M1 were calculated, ANOVA and Newman-Keuls post hoc test were used to study the impact of the CYP2D6 activity score on the 24 h urine log M/M1. Forward multiple regression was subsequently applied to evaluate the effect of PMA, PNA, weight and the CYP2D6 activity score on the 24 h urine log M/M1. Observations collected in cases with or without bladder catheter were compared (Mann-Whitney U). Urine log M/M1 values in cases in whom more than one urine 24 h collection was performed were also analyzed (paired t).
Plasma M and M1 (mg/L) were converted to tramadol molar equivalent concentrations. Based on these values, plasma log M/M1 values were calculated. Correlation (Spearman) between time (since initiation of loading dose) of infusion and plasma M, M1, or log M/M1 was calculated and ANOVA with post hoc Newman-Keuls test was applied in cases in whom at least two plasma samples were available to document stabilization of the log M/M1 values during continuous tramadol infusion after the loading dose. Correlations (Spearman) between PMA, PNA, or weight and plasma log M/M1 were calculated, ANOVA and Newman-Keuls post hoc test were used to study the impact of CYP2D6 activity score on plasma log M/M1. A similar exercise was performed with only the last collected plasma sample in every case. Forward multiple regression was applied to evaluate the effect of PMA, PNA, weight, and CYP2D6 activity score on the plasma log M/M1.
RESULTS
Eighty-six 24 h urine collections were harvested of whom 58 by urinary bladder catheter. Median PNA was 7 (1–159) d, median PMA was 39 (25–62) wk, median weight was 3070 (530–6140) g. Age distribution characteristics were summarized in Table 1. Observations on CYP2D6 polymorphisms were available in 82 of 86 collections. Data on incidence of the different CYP2D6 polymorphisms and the corresponding CYP2D6 activity score are provided in Table 1.
Median urine output for a 6 h collection period was 78 (3–356) mL, equivalent to a median urine output of 4.3 mL/kg/h. Of the total amount of tramadol administered, 47% (14.9)% was retrieved in the 24 h urine collections, mainly based on the parent compound tramadol 85.6% (31–99.1)%. M1 contributed 10.7% (0.2–26.1)% to overall urinary elimination.
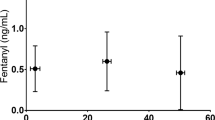
The mean 24 h urine log M/M1 was 0.98 (0.66); the mean urine log M/M1 for the consecutive collections (0–6, 6–12, 12–18, and 18–24 h) was 1.34 (0.85), 1.01 (0.75), 0.9 (0.67), and 0.9 (0.65). A progressive decrease in urine log M/M1 (ANOVA) was documented with consecutive time intervals (F value = 6.82, p < 0.001). Post hoc Newman-Keuls test demonstrated that the urine log M/M1 in the first urine collection was significantly different from the urine log M/M1 of the three other urine collections without additional difference between these three subsequent collections (Fig. 1). There were no significant differences in clinical characteristics or in urine log M/M1 values between cases with (n = 58) or without (n = 28) urinary bladder catheter.
The impact of the time interval of collection on the urine log M/M1. A progressive decrease in the urine log M/M1 was documented with the consecutive time intervals. The urine log M/M1 in the first urine collection was significantly different from the urine log M/M1 in the three subsequent urine collection intervals without additional difference between these collections.
Significant correlations of the 24 h urine log M/M1 with PMA (r = −0.69, 95% CI −0.79 to −0.56, p < 0.0001), PNA (r = −0.47, 95% CI −0.62 to −0.29, p < 0.001) and weight (r = −0.51, 95% CI −0.65 to −0.34, p < 0.001) were observed. ANOVA was applied to study the impact of the CYP2D6 activity score on phenotypic 24 h urine log M/M1 and was significant (F value = 11.61, p < 0.001). Post hoc Newman-Keuls test demonstrated significant differences between consecutive subgroups (Fig. 2). In a forward multiple regression model, PMA and CYP2D6 activity score remained independent variables of the urine log M/M1 and explained 59% (R2 0.59) of the interindividual variability.
Seven patients were included twice and one was included three times. In Table 2, clinical characteristics, CYP2D6 activity score and urine log M/M1 values on 15 observations were presented. When the first and the subsequent collection were compared, median urine log M/M1 decreased from 1.46 (0.02–2.76) to 0.89 (0.08–2.31) (p < 0.01).
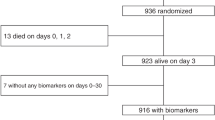
In a subgroup of 41 of 86 patients in whom an arterial access was available, 178 plasma time-concentrations points were collected. The median number of plasma samples collected was 4 (1–10). Mean plasma log M/M1 was 0.78 (0.45). There was no significant correlation between plasma log M/M1 and timing of sampling (Fig. 3) (r = 0.009, 95% CI −0.14 to 0.16, p = 0.9), nor was there a significant correlation between plasma M or plasma M1 concentration and timing of sampling (r = 0.027, 95% CI −0.15 to 0.2, p = 0.76 and r = −0.07, 95% CI −0.24 to 0.11, p = 0.44), reflecting stabilization after the initial loading dose. No significant difference (ANOVA) was observed in plasma log M/M1 values with consecutive sampling. Post hoc Newman-Keuls test did not unveil any difference between subsequent samples.
For 10 plasma-concentrations points, the plasma log M/M1 value could not be calculated because the M1 concentration was below the lower limit of quantification (0.05 μg/mL). In all these samples, patients were later diagnosed as poor metabolizers (CYP2D6 activity score = 0) resulting in five subgroups (0.5, 1, 1.5, 2, and >2) for the ANOVA plasma log M/M1 analysis (Fig. 4).
Significant inverse correlations of the plasma log M/M1 with PMA (r = −0.65, 95% CI −0.73 to −0.55, p < 0.0001), PNA (r = −0.73, 95% CI −0.79 to −0.65, p < 0.0001) and weight (r = −0.36, 95% CI −0.48 to −0.22, p < 0.0001) were documented. Using ANOVA, a progressive significant decrease in plasma log M/M1 with increasing CYP2D6 activity score (F value = 22.55, p < 0.001, Fig. 4) was observed. Newman-Keuls post hoc test demonstrated significant differences between consecutive subgroups (Fig. 4). Correlations between plasma log M/M1 and PMA (p < 0.001), PNA (p < 0.001), or weight (p < 0.05) remained significant and the progressive significant decrease in plasma log M/M1 with increasing CYP2D6 activity score was confirmed when only the last collected plasma log M/M1 in every individual patient was used (F value = 3.22, p < 0.05). In a forward multiple regression model, PMA and CYP2D6 activity score determined the plasma log M/M1 and explained 64% (R2 0.64) of the interindividual variability.
DISCUSSION
CYP2D6 only represents 2% of hepatic CYP content in adults, but mediates metabolism of multiple therapeutics and xenobiotics including β-receptor antagonists, antiarrhythmics, serotonin selective reuptake inhibitors (SSRIs), antipsychotics and opioids like codeine and tramadol, possibly administered to neonate or to mother before (fetal) or after (breastfeeding) birth (1,15,16). Unveiling the different contributors to drug metabolism in early life is therefore of clinical relevance: altered, either reduced or ultra rapid drug metabolism can contribute to therapeutic failure or toxicity as has been anecdotally illustrated by observations on codeine toxicity in a breast fed neonate (16) or an ultra-rapid metabolizing toddler (17). Brousseau et al. (18) recently documented the effect of CYP2D6 polymorphisms on the analgesic response to codeine for pediatric sickle cell crisis. Codeine also undergoes CYP2D6 dependent metabolism to morphine. In this article, we documented the impact of PMA and CYP2D6 polymorphisms on O-demethylation of tramadol in the first months of life.
The impact of CYP2D6 polymorphisms but not age on O-demethylation in healthy full term newborns and infants was recently described based on urine collections following single dose oral dextromethorphan administration (2). Blake et al. (2) documented concordance of phenotypic O-demethylation activity and genotype (CYP2D6 activity score) from 2 wk of PNA onwards in term neonates, therefore equivalent to 42 wk PMA. The current data confirm these findings since ontogeny, i.e., age dependent maturation of O-demethylation activity mainly seems to evolve—at least in preterm neonates—until term age, equivalent to 40 wk PMA.
To illustrate the simultaneous contribution of PMA and CYP2D6 activity score on the 24 urine log, M/M1 values in cases (<37, 37–41, or >41 wk PMA) with a CYP2D6 activity score of 1 or 2 are provided in Figure 5. Besides the significant difference in 24 h urine log M/M1 in patients with a CYP2D6 activity score of 1 or 2, there is a PMA dependent impact on the urine log M/M1 (Fig. 5).
In addition to the work of Blake et al., plasma samples were collected to further validate the approach. Similar to the 24 h urine log M/M1, PMA and CYP2D6 activity score contributed to the interindividual variability plasma log M/M1 in a similar magnitude (R2 0.59 versus 0.64). However, in this specific model of continuous i.v. tramadol administration, single point measurements of plasma log M/M1 plasma resulted in the inability to calculate a log value in 10 of 178 plasma samples collected because the M1 concentration was below the lower limit of quantification. All these samples were collected in individuals who turned out to be poor metabolizers, i.e., CYP2D6 activity score of 0. We therefore suggest that urine collections better display the extent of interindividual phenotypic variability in log M/M1 in early life (Figs. 2 and 4).
The difference between mean values of 24 h urine (0.98) and plasma log M/M1 (0.78) likely reflects the difference in the time frame used for sampling. Urine was collected during a 24 h time interval starting at initiation of the loading dose whereas plasma samples were point measurements collected between 4 and 24 h after initiation of treatment. As mentioned earlier, the choice to collect plasma samples in this specific time interval was based on a preliminary report in which it was documented that approximately 4 h were needed before the plasma log M/M1 became stable in this specific model (8). Theoretically, a urine collection interval that is too short to the half life of the drug or its metabolites might also explain these discordances, but the absence of any correlation between time and plasma M, M1, and log M/M1 was reconfirmed in the current study, suggesting phenotypic stabilization during the time interval investigated. In contrast, a progressive decrease in urine log M/M1 was documented with consecutive time intervals of collection. Using post hoc Newman-Keuls test, urine log M/M1 in the first urine collection was significantly different from the urine log M/M1 in the three subsequent urine collection intervals without additional differences between these collection intervals (Fig. 1).
Özdemir et al. documented differential sensitivity of in vivo CYP2D6 activity based on urine metabolic ratio's to urine pH (21). Although these studies were performed in adults based on oral administration of debrisoquine, dextromethorphan, or metoprolol with oral co-administration of sodium bicarbonate or ammonium chloride, it cannot be excluded that differences in urine pH in this cohort also result in differences in urine log M/M1 values. Unfortunately, we have no data on urine pH in our cohort.
Finally, phenotypic stabilization of a metabolic ratio does not necessary reflects stabilization of metabolic activity, because the phenotypic log M/M1 is the final indicator of disposition, depending on iso-enzyme specific metabolic activity, distribution and (renal) elimination. All these contributors mature. This has been recently stressed by Johnson et al., who documented that the stable urine DM/DX ratio in the first year of life described by Blake et al. not only reflects ontogeny of O-demethylation but also depends on renal drug handling (22). In the current study, both plasma and urine log M/M1 values stabilized during continuous i.v. tramadol administration.
It is important to stress that PMA and CYP2D6 activity score only to a certain extent (R2 0.59 and 0.64) explain the interindividual log M/M1 observed. Only *3, *4, *5, *6, *9, *10, *41 and *1×N CYP2D6 polymorphisms were investigated. Stamer et al. recently documented that *45 and *46 CYP2D6 polymorphisms also contributed to the interindividual variability of enantiomer-specific tramadol metabolism in adults (19). Based on the overall low incidence of *45 and *46 polymorphism in whites (<2%), it is to be anticipated that the impact of these CYP2D6 polymorphisms is limited (22). Besides polymorphisms, disease characteristics like sepsis or cardiac surgery can also contribute to the variability of drug metabolism (4,5).
The current observations contribute to the knowledge of maturational tramadol disposition (15). The high contribution of the mother compound to overall tramadol urinary elimination suggests that metabolic clearance only to a limited extent contributes to tramadol elimination. This is in line with pharmacokinetic studies on i.v. tramadol disposition in neonates and children in which M1 formation clearance represented a minor elimination pathway of tramadol (10,23). It is therefore remarkable that we were unable to document any correlation between age or creatinaemia and urine overall tramadol recovery. During the time interval the study was performed, creatinaemia was determined based on a modified Jaffé method and has only recently been changed to an enzymatic assay and creatinaemia only in part reflects renal function in early life (24). Another logistic problem is the collection of urine as mentioned by Blake et al. (2). However, no differences between cases with or without bladder catheter were observed.
In contrast to limited impact of O-demethylation activity on tramadol clearance, tramadol metabolism is of pharmacodynamic relevance because M1 contributes to the analgesic effect of tramadol (21). In the current study, there is already relevant CYP2D6 activity in term neonates and young infants, but it still needs to be proven that CYP2D6 polymorphisms already contributes to the interindividual pharmacodynamic variability of tramadol (21).
The impact of PMA and CYP2D6 on phenotypic O-demethylation is also of relevance beyond the drug specific observations, because this probe drug unveils determinants of interindividual variability in O-demethylation activity (1,8,15). Besides PMA, CYP2D6 polymorphism contributes to phenotypic O-demethylation activity in neonates, leaving 40% of interindividual variability unexplained.
The current observations illustrate the impact of ontogeny and polymorphisms on phenotypic drug metabolism in (pre)term neonates. Treszl et al. (25), recently reviewed in this journal, observations on the link between polymorphisms and perinatal adaptation. In the current study, CYP2D6 polymorphisms already contribute to perinatal drug metabolism, illustrating the potential contribution of pharmacogenetics in perinatology.
As mentioned earlier, CYP2D6 is of relevance in the disposition of drugs administered to neonate or to mother before (fetal) or after (breastfeeding) birth like opioids (tramadol, codeine) or SSRIs. There is still controversy whether symptoms observed in neonates born to mothers to whom SSRI during pregnancy were administered, reflect neonatal withdrawal (enhanced clearance) or are the manifestation of persistent high SSRI concentrations with toxicity due to limited clearance (26). SSRIs undergo CYP2D6 dependent metabolic clearance. Based on the current data and the data of Blake et al. (2), phenotypic O-demethylation can be predicted by PMA and CYP2D6 polymorphisms. At term age and beyond, it is to be anticipated that CYP2D6 polymorphisms will be the most relevant determinant of metabolic clearance of this drug, resulting in either poor or ultra-extensive metabolic clearance dependent on the CYP2D6 genotype, whereas preterm neonates will display limited metabolic clearance, independent of the CYP2D6 genotype, with potential accumulation or persistent high serum levels.
In conclusion, PMA and CYP2D6 polymorphisms determined O-demethylation activity in early life. Besides compound-specific relevance, the current iso-enzyme specific data on in vivo ontogeny of O-demethylation can contribute to safer and more effective administration of tramadol and other drugs metabolized by the same route in this population.
Abbreviations
- M:
-
tramadol
- M1:
-
O-demethyl tramadol
- M2:
-
N-demethyl tramadol
- PMA:
-
postmenstrual age, weeks
- PNA:
-
postnatal age, days
References
Kearns GL, Abdel-Rahman SM, Alander SW, Blowey DL, Leeder JS, Kauffman RE 2003 Developmental pharmacology: drug disposition, action, and therapy in infants and children. N Engl J Med 349: 1157–1167
Blake MJ, Gaedigk A, Pearce RE, Bomgaars LR, Christensen ML, Stowe C, James LP, Wilson JT, Kearns GL, Leeder JS 2007 Ontogeny of dextromethorphan O- and N-demethylation in the first year of life. Clin Pharmacol Ther 81: 510–516
Allegaert K, van den Anker JN, Debeer A, Cossey V, Verbesselt R, Tibboel D, Devlieger H, de Hoon J 2006 Maturational changes in the in vivo activity of CYP3A4 in the first months of life. Int J Clin Pharmacol Ther 44: 303–308
Lynn A, Nespeca MK, Bratton SL, Strauss SG, Shen DD 1998 Clearance of morphine in postoperative infants during intravenous infusion: the influence of age and surgery. Anesth Analg 86: 958–963
Carcillo JA, Doughty L, Kofos D, Frye RF, Kaplan SS, Sasser H, Burckart GJ 2003 Cytochrome P450 mediated-drug metabolism is reduced in children with sepsis-induced multiple organ failure. Intensive Care Med 29: 980–984
Pedersen RS, Damkier P, Brosen K 2005 Tramadol as a new probe for cytochrome P450 2D6 phenotyping: a population study. Clin Pharmacol Ther 77: 458–467
Stamer UM, Musshoff F, Kobilay M, Madea B, Hoeft A, Stuber F 2007 Concentrations of tramadol and O-desmethyltramadol enantiomers in different CYP2D6 genotypes. Clin Pharmacol Ther 82: 41–47
Allegaert K, van den Anker JN, Verbesselt R, de Hoon J, Vanhole C, Tibboel D, Devlieger H 2005 O-demethylation of tramadol in the first months of life. Eur J Clin Pharmacol 61: 837–842
Abdel-Rahman SM, Leeder JS, Wilson JT, Gaedigk A, Gotschall RR, Medve R, Liao S, Spielberg SP, Kearns GL 2002 Concordance between tramadol and dextromethorphan parent/metabolite ratios: the influence of CYP2D6 and non-CYP2D6 pathways on biotransformation. J Clin Pharmacol 42: 24–29
Allegaert K, Tibboel D, Naulaers G, Tison D, de Jonge A, Van Dijk M, Vanhole C, Devlieger H 2003 Systematic evaluation of pain in neonates: effect on the number of intravenous analgesics prescribed. Eur J Clin Pharmacol 59: 87–90
Allegaert K, Anderson BJ, Verbesselt R, Debeer A, de Hoon J, Devlieger H, van den Anker JN, Tibboel D 2005 Tramadol disposition in the very young: an attempt to assess in vivo cytochrome P-450 2D6 activity. Br J Anaesth 95: 231–239
Gaedigk A, Gotschall RR, Forbes NS, Simon SD, Kearns GL, Leeder JS 1999 Optimization of cytochrome P450 2D6 (CYP 2D6) phenotype assignment using a genotyping algorithm based on allele frequency data. Pharmacogenetics 9: 669–682
Hersberger M, Marti-Jaun J, Rentsch K, Hanseler E 2000 Rapid detection of the CYP2D6*3, CYP2D6*4, and CYP2D6*6 alleles by tetra-primer PCR and of the CYP2D6*5 allele by multiplex long PCR. Clin Chem 46: 1072–1077
Lovlie R, Daly AK, Molven A, Idle JR, Steen VM 1996 Ultrarapid metabolizers of debrisoquine: characterization and PCR-based detection of alleles with duplication of the CYP2D6 gene. FEBS Lett 392: 30–34
Johnson TN 2005 Different pharmacokinetics of tramadol in mothers treated for labour pain and in their neonates. Towards an increased knowledge of paediatric clinical pharmacology. Eur J Clin Pharmacol 61: 929–930
Koren G, Cairns J, Chitayat D, Gaedigk A, Leeder SJ 2006 Pharmacogenetics of morphine poisoning in a breastfed neonate of a codeine-prescribed mother. Lancet 368: 704
Voronov P, Przybylo HJ, Jagannathan N 2007 Apnea in a child after oral codeine: a genetic variant – an ultra-rapid metabolizer. Paediatr Anaesth 17: 684–687
Brousseau DC, McGarver DG, Drendel AL, Divakaran K, Panepinto JA 2007 The effect of CYP2D6 polymorphisms on the response to pain treatment for pediatric sickle cell pain crisis. J Pediatr 150: 623–626
Özdemir M, Crewe KH, Tucker GT, Rostami-Hodjegan A 2004 Assessment of in vivo CYP2D6 activity: differential sensitivity of commonly used probes to urine pH. J Clin Pharmacol 44: 1398–1404
Johnson TN Tucker GT, Rostami-Hodjegan A Development of CYP2D6 and CYP3A4 in the first year of life. Clin Pharmacol Ther [Epub ahead of print]
Stamer UM, Lehnen K, Hothker F, Bayerer B, Wolf S, Hoeft A, Stuber F 2003 Impact of CYP2D6 genotype on postoperative tramadol analgesia. Pain 105: 231–238
Sachse C, Brockmoller J, Bauer S, Roots I 1997 Cytochrome P450 2D6 variants in a Caucasian population: allele frequencies and phenotypic consequences. Am J Hum Genet 60: 284–295
Garrido MJ, Habre W, Rombout F, Trocóniz IF 2006 Population pharmacokinetic/pharmacodynamic modelling of the analgesic effects of tramadol in pediatrics. Pharm Res 23: 2014–2023
van den Anker JN 1997 Renal function in preterm infants. Eur J Pediatr 156: 583–584
Treszl A, Kaposi A, Hajdu J, Szabo M, Tulassay T, Vasarhelyi B 2007 The extent to which genotype information may add to the prediction of disturbed perinatal adaptation: none, minor or major?. Pediatr Res 62: 610–614
Lattimore KA, Donn SM, Kaciroti N, Kemper AR, Neal CR Jr, Vazquez DM 2005 Selective serotonin reuptake inhibitor (SSRI) use during pregnancy and effects on the fetus and newborn: a meta-analysis. J Perinatol 25: 595–604
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the Clinical Research Fund of the University Hospitals Leuven, Belgium (to K.A.), and by grant HD45993 (NICHD) and RR19729 (NCRR) (to J.N.v.d.A.).
Rights and permissions
About this article
Cite this article
Allegaert, K., van Schaik, R., Vermeersch, S. et al. Postmenstrual Age and CYP2D6 Polymorphisms Determine Tramadol O-demethylation in Critically Ill Neonates and Infants. Pediatr Res 63, 674–679 (2008). https://doi.org/10.1203/PDR.0b013e31816ff712
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31816ff712
This article is cited by
-
Precision therapeutics in the NICU: why are we missing the mark?
Journal of Perinatology (2018)
-
Safety, dosing, and pharmaceutical quality for studies that evaluate medicinal products (including biological products) in neonates
Pediatric Research (2017)
-
The Pharmacogenetics of Tramadol
Clinical Pharmacokinetics (2015)
-
Mechanism based medicine in infancy: complex interplay between developmental pharmacology and pharmacogenetics
International Journal of Clinical Pharmacy (2011)
-
Maternal–fetal and neonatal pharmacogenomics: a review of current literature
Journal of Perinatology (2010)