Abstract
To test the hypothesis that an acute increase in O2 tension increases cytosolic calcium ([Ca2+]i) in fetal pulmonary artery endothelial cells (PAECs) via entry of extracellular calcium and subsequent calcium-induced calcium release (CICR) and nitric oxide release, low-passage PAECs (<10 passages) were isolated from the intralobar pulmonary artery (PA) of fetal sheep and maintained under hypoxic conditions (Po2, 25 Torr). Using the calcium-sensitive dye fura-2, we demonstrated that acute normoxia (Po2 = 120 Torr) increased PAECs [Ca2+]i by increasing the rate of entry of extracellular calcium. In the presence of either ryanodine or 2-aminoethoxy-diphenylborate (2APB), normoxia did not lead to a sustained increase in PAECs [Ca2+]i Whole-cell patch clamp studies demonstrated that acute normoxia causes PAEC membrane depolarization. When loaded with the nitric oxide (NO)–sensitive dye, DAF - FM, acute normoxia increased PAEC fluorescence. In PAECs derived from fetal lambs with pulmonary hypertension, an acute increase in O2 tension had no effect on either [Ca2+]i or NO production. Hypoxia increases loading of acetylcholine-sensitive calcium stores, as hypoxia potentiated the response to acetylcholine We conclude that acute normoxia increases [Ca2+]i and NO production in normotensive but not hypertensive fetal PAECs via extracellular calcium entry and calcium release from calcium-sensitive intracellular stores.
Similar content being viewed by others
Main
In the fetus, pulmonary blood flow is limited. At birth, pulmonary blood flow increases eight- to 10-fold (1) and pulmonary arterial pressure decreases to 50% of systemic levels within 24 h after birth (2). The critical physiologic stimuli that account for perinatal pulmonary vasodilation include rhythmic distention of the lung (3), an increase in both shear stress (4), and oxygen tension (5). In response to physiologic stimuli, the pulmonary endothelium elaborates vasoactive mediators such as NO (6), endothelin (7), bradykinin, and prostaglandins. PAEC NO production is necessary (8), although not always sufficient, for the transition of the pulmonary circulation from a high to low resistance circuit.
Vasoactive products produced by the PAECs simultaneously preserve and constrain fetal pulmonary blood flow. During fetal life, inhibition of endothelin, a vasoconstrictive protein produced by the endothelium (7), causes marked pulmonary vasodilation (9). Conversely, inhibition of NO increases pulmonary vascular resistance (8). Among the most important functions of the PAECs is the ability to sense and respond to an increase in oxygen tension at birth. Interestingly, the capacity of the pulmonary circulation to sense and respond to an acute increase in oxygen tension is developmentally regulated. Not until gestation is approximately 85% complete is the fetal pulmonary circulation able to respond to an increase in oxygen tension (10). Vasodilator agents that act through endothelial cell–mediated mechanisms produce only transient pulmonary vasodilation (5,11). Perhaps the relatively narrow developmental window wherein the fetal pulmonary circulation is able to respond to an increase in oxygen tension serves a protective purpose as either too much (12) or too little (13) pulmonary blood flow compromises pulmonary vascular development.
The capacity of PAECs to produce NO (14) may underlie the exquisite sensitivity of the late-gestation pulmonary circulation to an increase in oxygen tension (15). Although the response of PAECs to an acute increase in oxygen tension is biologically imperative, whether and how fetal PA endothelial cells sense and respond to acute increase in oxygen tension remains incompletely understood.
Because intracellular cytosolic calcium ([Ca2+]i) is central to the signal transduction cascade and production of NO by endothelial cells (16), we hypothesized that an acute increase in oxygen tension increases fetal PAEC [Ca2+]i and NO production. Moreover, because oxygen-induced fetal pulmonary vasodilation is attenuated in fetal lambs with chronic intrauterine pulmonary hypertension (17), we hypothesized that an acute increase in oxygen tension would have a relatively attenuated effect on [Ca2+]i and NO production in PAECs derived from lambs with chronic intrauterine pulmonary hypertension. To test these hypotheses, the effect of an acute increase in oxygen tension was determined in PAECs derived from late-gestation fetal lambs with and without chronic intrauterine pulmonary hypertension. The present experimental series provides data that acute normoxia increases [Ca2+]i and NO production from normal but not hypertensive PAECs.
METHODS
Animals.
The procedures used in these studies were reviewed and approved by the Animal Care and Use Committee at the University of Minnesota Medical School.
Cell culture.
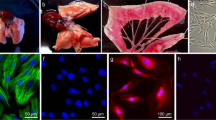
Techniques used for cell isolation and culture have been previously described (18,19). Late-gestation fetal sheep (term = 147 d) from ewes with time-dated pregnancies were used in this study.
Distal (fourth generation or more) PAs were quickly excised and placed in minimal essential media (0.2 mmol/L Ca2+). Low-passage PAECs (<10 passages) were isolated from the macrovasculature (fourth generation) of late-gestation fetal sheep (135 d), cultured on acid-washed glass coverslips (25-mm circle; Fisher Scientific, Pittsburgh, PA). Seeded coverslips were placed in 35-mm culture plates with 1.5 mL of RPMI 1640 with 10% fetal bovine serum, 10% fetal lamb serum, 1% penicillin, 0.15% nystatin, 0.15% gentamicin, 0.8% tysolin, and 1% ampicillin. Cells were maintained at 37°C in a humidified mixture of 5% O2 and 5% CO2.
Chronic intrauterine pulmonary hypertension model.
Surgical ligation of the ductus arteriosus (DA) was performed as previously described (20). Seven to 10 d after surgical ligation of the DA, animals were euthanized rapidly after high-dose maternal and fetal infusions of pentobarbital sodium, and the PAECs were harvested.
Experimental conditions.
Fetal PAECs were maintained in a low oxygen tension environment (25 torr). To evaluate the effect of acute normoxia, oxygen tension was increased to 120 Torr.
Ca2+ imaging.
To assess dynamic changes in [Ca2+]i in individual PAECs, the Ca2+-sensitive fluorophore fura-2–AM (Molecular Probes) was used as previously described (21). Confluent monolayers of fetal ECs on 25-mm2 glass coverslips were placed on the stage of an inverted microscope (Nikon Diaphot). Cells were loaded with 10 nmol/L fura-2–AM and 2.5 μg/mL pluronic acid (Molecular Probes) for 20 min, followed by 20 min in Ca2+-containing solution to allow for de-esterification before the experiment. For each experiment, eight to 10 cells were visualized and ratiometric data were acquired from individual cells.
Electrophysiology studies.
PAECs maintained in culture were prepared and stored in a hypoxic Ca2+-free Hanks solution (see “Solutions and drugs” section). Single cells were enzymatically dispersed using a papain digestion protocol. Briefly, cells were incubated for 30 min at 4°C in Hanks solution containing 0.5 mg/mL papain, 1 mg/mL albumin, and 1 mg/mL dithiothreitol, without ethyleneglycol-bis-(β-aminoethylether)-N,N,N′,N′-tetraacetic acid (EGTA), and then incubated at 37°C for 15–20 min. The cells were washed thoroughly in enzyme-free Hanks solution for at least 10 min and then maintained at 4°C. Several digestions were done each day to ensure cell viability. All cells were studied in identical conditions within 2 h of preparation.
Whole-cell recordings were performed using the amphotericin-perforated patch-clamp technique as previously reported (20). Membrane potential stability was always determined for at least 1 min before any recording. The data were stored and analyzed with commercially available software (pCLAMP version 8.1; Axon Instruments). All experiments were performed at 30°C and in low light intensity because of the light sensitivity of amphotericin B.
NO determination.
Two separate techniques were used to evaluate the effect of an acute increase in oxygen tension on NO production: fluorescent microscopy and an assay for nitrite and nitrate production. In fluorescent microscopy experiments, PAECs were loaded with the NO-sensitive dye DAF-FM (Molecular Probes) for 30 min under conditions of hypoxia. After 30 min, cells were washed with hypoxic buffer to allow for deacetylation. Green fluorescence intensity was measured with excitation at 495 nm and emission at 515 nm. The single wavelength dye DAF-FM increases fluorescence emission intensity concomitant with an increase in NO production. After loading of the endothelial cells under hypoxic conditions, oxygen tension was acutely increased. Fluorescence emission intensity was continuously monitored. In a separate set of experiments, PAECs were treated with the competitive antagonist of NO, nitro-l-arginine, immediately before and during the acute increase in oxygen tension To ensure that experimental findings were not the result of using only a single experimental technique, PAECs were grown in MCDB 131/10% fetal calf serum and distributed into collagen-coated 12-well plates and grown in hypoxia. After cells reached confluence, fresh, prewarmed, hypoxic solution (0.25 mL) was placed on the cells. As controls, blank wells without cells were treated in the same manner. After 24 h, the medium was collected, frozen, and replaced with prewarmed normoxic medium. This supernatant was collected and frozen at 24 h for NO determination. Total nitrate + nitrite were assayed with a fluorometric Nitrate/Nitrite Assay kit (Cayman Chemical, Ann Arbor, MI). Standards were analyzed in medium and fluorescence values of media blanks were subtracted. The cells were counted in a Coulter counter (Beckman Coulter, Fullerton, CA). Data were calculated as micromole per liter divided by cell number.
Solutions and drugs.
The Hanks solution contained (in mmol/L) 145 NaCl, 4.2 KCl, 1 MgCl2, 1.2 KH2PO4, 10 N-2-hydroxyethylpiperazine-N1-2-ethanesulfonic acid (HEPES), 10 glucose, and 0.1 EGTA (pH was adjusted to 7.4 by KOH). The extracellular or experimental solution contained (in mmol/L) 115 NaCl, 5.4 KCl, 1 MgCl2, 1.8 CaCl2, 25 NaHCO3, 10 HEPES, and 10 glucose (pH 7.4 with NaOH). For electrophysiology studies, the standard intracellular pipette solution contained (in mmol/L) 145 KCl, 1 MgCl2, 1 EGTA, 10 HEPES, and 120 μg/mL amphotericin B (pH was adjusted to 7.3 by KOH). For manganese quenching experiments, cells were superfused with a calcium-free solution containing MnCl2 (0.5 mmol/L).
2-Aminomethoxy-diphenylborate (2APB) was purchased from Calbiochem (Laeufelfingen, Switzerland). Cyclopiazonic acid (CPA), a Ca2+-ATPase inhibitor, which passively empties inositol triphosphate (IP3)–sensitive Ca2+ stores was obtained from Alexis Biochemical (San Diego, CA). All fluorescent probes and pluronic f-127 were obtained from Molecular Probes (Eugene, OR). All other compounds were purchased from Sigma Chemical Co. (St. Louis, MO). The drug solutions were adjusted to pH 7.4 before use.
The effect of hypoxia was studied by switching between normoxic and hypoxic perfusate reservoirs. Normoxic solutions were equilibrated with 21% O2, 5% CO2, and 74% N2. Hypoxic solutions were achieved by bubbling with 0% O2 (plus 5% CO2-balance N2) for at least 20 min before cell perfusion. These procedures produced Po2 values in the cell chamber of 125 Torr (21% O2) and 24–30 mm Hg (hypoxia O2). Pco 2 was 36–42 mm Hg, and pH was 7.37–7.42 under these conditions. O2 levels were measured with a Rapidlab Chiron blood gas analyzer.
Statistical analysis.
Throughout, results are presented as means ± standard error (SE). Statistical significance was tested with a t test (paired or unpaired as appropriate); p < 0.05 was taken as the threshold level for statistical significance. Experiments were designed to have a statistical power of at least 90% at a probability level of p < 0.05. A two-way analysis of variance with repeated measures and a Student-Newman-Keuls post hoc test were used to assess the differences between and among groups in electrophysiology and manganese quenching experimental protocols. Values are expressed as means ± SE.
RESULTS
Effects of an acute increase in Po2 on [Ca2+]i in PAECs.
To determine the effect of an acute increase in Po2 on [Ca2+]i, baseline [Ca2+]i measurements were obtained under hypoxic conditions for 5 min. Acute normoxia increased PAECs [Ca2+]i (Fig. 1) within 4 min (p = 0.016). Thirty minutes after the switch to normoxia, the ratio of 340:380-nm wavelength emission intensity had increased by 14.2 ± 0.5% (n = 77; 10 coverslips; five animals; p < 0.01, versus baseline). In PAECs derived from animals with chronic intrauterine pulmonary hypertension, acute normoxia had no effect on the ratio of 340:380-nm wavelength emission intensity over the 30-min study period (percentage of change, 1.2 ± 0.9%; n = 56; seven coverslips, three animals; p > 0.05, versus baseline).
Effect of an acute increase in oxygen tension on fetal PAECs [Ca2+]i. With an acute increase in oxygen tension, the ratio of 340:380-nm fluorescence emission intensity increases progressively over the duration of the study period (black squares). In the absence of extracellular calcium (shaded diamonds), an acute increase in oxygen tension has no effect on PAECs [Ca2+]i. (*p < 0.01 vs 0 calcium). Data are expressed as the percentage of change in signal intensity (y axis) from baseline vs time (x axis).
Contribution of extracellular Ca2+ entry to oxygen-induced increase in PAECs [Ca2+]I.
PAECs were superfused with zero-Ca2+ buffer concomitant with an acute increase in Po 2. In the presence of zero-Ca2+ buffer, acute normoxia had no effect on PAECs [Ca2+]i (Fig. 1). With the reintroduction of extracellular calcium, normoxia increased the ratio of 340:380-nm emission intensity (n = 49; eight coverslips, four animals; p < 0.01, versus baseline normoxia and zero-extracellular calcium). The dihydropyridine-sensitive voltage-operated calcium channel blocker nifedipine (10−6 mol/L) had no effect on either baseline fluorescence intensity (n = 54; eight coverslips, four animals; p > 0.05, versus baseline) or on the normoxia-induced increase in PAECs [Ca2+]i (p > 0.05, versus control cells).
Effects of an acute increase in Po 2 on the rate of extracellular Ca2+ entry in PAECs.
Mn2+ containing, zero-Ca2+ solution was superfused over PAECs, and the rate of fura-2 signal quenching was measured before and after an acute increase in Po2. Over sustained exposure to hypoxia (30 min), the rate of fura-2 quenching was −0.118 (fluorescence units over time; R 2 = 0.9872). Concomitant with an acute increase in oxygen tension, the rate of fura-2 quenching increased by almost 10-fold to −1.114 (Fig. 2; R2 = 0.9725; n = 115 cells; 12 coverslips, five animals; p < 0.001 hypoxia versus normoxia).
Effect of an acute increase in oxygen tension on the rate of manganese quenching of the fura-2 fluorescence signal intensity in fetal PAECs. The rate of fura-2 florescence signal intensity quenching is greater after an increase in oxygen tension from hypoxia (slope = −0.114; shaded dashed line) to normoxia (slope = −1.118; black dashed line; p < 0.001, hypoxia vs normoxia). The increase in the rate of fura-2 signal quenching indicates that extracellular calcium enters the cell more rapidly under conditions of normoxia than hypoxia.
Role of intracellular Ca2+ release on O2-induced increase in [Ca2+]i.
Under hypoxic conditions, neither cyclopiazonic acid (CPA; 10 μmol/L; n = 42 cells; five coverslips, three animals) nor ryanodine (5 μmol/L; n = 38 cells; five coverslips, three animals) at a dose that blocks release of Ca2+ from ryanodine-sensitive stores had an effect on basal PAECs [Ca2+]i. In the presence of ryanodine, acute normoxia initially increased PAECs [Ca2+]i, although the increase was attenuated through the remainder of the 30 min of normoxic exposure (Fig. 3). In the presence of CPA, acute normoxia had no effect on PAECs [Ca2+]i.
Effect of ryanodine on the oxygen-induced increase in fetal PAEC cytosolic calcium. In the presence or absence of ryanodine (shaded line), an acute increase in oxygen tension increased the ratio of 340:380-nm fluorescence emission intensity in fetal PAECs for the initial 10 min of normoxic exposure. Over the subsequent 15 min of exposure to normoxia, PAECs [Ca2+]i decreased, although remaining above baseline values (*p < 0.01, vs ryanodine; **p < 0.01, vs baseline). Data are expressed as percentage change in signal intensity (y axis) from baseline vs time (x axis).
Effect of 2-APB, a pharmacologic antagonist of the inositol triphosphate-sensitive store, on hypoxic PAECs [Ca2+]i and on O2-induced increase in [Ca2+]i.
To determine the role of Ca2+ release on basal PAECs, [Ca2+]i under conditions of hypoxia and upon the O2-induced increase in PAECs [Ca2+]i, 2-APB, a blocker of Ca2+ release from IP3-sensitive stores, was administered to fura-2 loaded PAECs under hypoxic conditions. 2-APB (5 × 10−5 mol/L; n = 27 cells; four coverslips, three animals) increased PAECs [Ca2+]i under hypoxic conditions (p < 0.01, versus baseline). In the presence of 2-APB (10−6 mol/L; n = 51 cells; six coverslips, three animals), acute normoxia had no effect on PAECs [Ca2+]i.
Effects of an acute increase in Po2 on PAEC membrane potential.
In hypoxic conditions, PAEC resting membrane potential was −43 ± 0.5 mV. With an acute increase in oxygen tension, PAEC resting membrane potential decreased to −39 ± 0.4 mV (p < 0.008; n = 5; three animals).
Effects of K+ channel blockers on [Ca2+]i.
Under hypoxic conditions, PAECs were treated with either glibenclamide (10−5 nmol/L), 4-aminopyridine (4-AP) (10−3 mol/L), or tetraethylammonium (TEA) (10−3 mol/L). Glibenclamide, a blocker of ATP-sensitive K+ channels, had no effect on PAEC [Ca2+]i. Either TEA (n = 46; five coverslips, three animals), a KCa channel blocker in millimolar concentrations (22), or 4-AP (n = 52; five coverslips, three animals), a KV channel blocker, increased PAEC [Ca2+]i (p < 0.01, versus baseline for either TEA or 4-AP). Treatment with 4-AP and TEA together resulted in an 11.4 ± 0.4% increase in [Ca2+]i (p < 0.01; n = 47 cells; five coverslips, three animals; Fig. 4).
Effect of K+ channel blockers on the ratio of 340:380-nm fluorescence emission intensity in fetal PAECs. Either TEA (10−3 mol/L) or 4-AP increased PAEC membrane fluorescence (*p < 0.01, vs TEA; **p < 0.01, vs baseline). The combination of TEA and 4-AP produced a greater increase in PAEC [Ca2+]i than either agent alone (p < 0.001, TEA + 4-AP, vs either TEA or 4-AP). Data are expressed as the percentage of change in signal intensity (y axis) from baseline vs K+ channel blocker (x axis).
Effect of oxygen tension on acetylcholine-induced increase in PAEC [Ca2+]i.
Fura-2–loaded hypoxic or normoxic PAEC were treated with acetylcholine in log-order increasing doses (10−7 through 10−2 mol/L). PAECs were treated with acetylcholine under either hypoxic conditions or after <4 min of acute normoxia. Acetylcholine caused a greater increase in hypoxic (n = 67 cells; seven coverslips, four animals), compared with normoxic (n = 72 cells; seven coverslips, four animals), PAEC [Ca2+]i at every concentration studied (Fig. 5, p < 0.01, hypoxia versus normoxia for each concentration). The increase reported in Figure 5 represents the plateau level of emission intensity reached within 3 min of treatment with acetylcholine.
Effect of hypoxia on acetylcholine-induced increase in the ratio of 340:380-nm fluorescence emission intensity in fetal PAECs. Acetylcholine caused a dose-related increase in the ratio of 340:380-nm fluorescence emission intensity in fetal PAECs under either hypoxic or normoxic conditions (*p < 0.001, hypoxia vs baseline). However, for each concentration of acetylcholine studied, the increase in PAEC [Ca2+]i was greater under conditions of hypoxia than normoxia (**p < 0.001, hypoxia vs normoxia). Data are expressed as the percentage of change in signal intensity (y axis) from baseline vs concentration of acetylcholine (x axis).
Effect of an increase in oxygen tension on NO production in normal and hypertensive PAECs
Under hypoxic conditions, NO production was 0.110 ± 0.074 nmol of NO (nanomoles per 105 PAECs) in control cells and 0.052 ± 0.04 μmol/L NO in hypertensive cells (p < 0.02, control versus hypertensive). Normoxia increased NO production to 0.869 ± 0.22 μmol/L NO in control cells (p < 0.01 versus hypoxia), but not in hypertensive PAECs (0.182 ± 0.03 μmol/L NO; p = not significant [NS], versus hypoxia).
As depicted in Figure 6, membrane fluorescence in PAECs loaded with DAF-FM diacetate (Molecular Probes) increased from 105 ± 0.8 to 133 ± 1.0 at 30 min (p < 0.001) concomitant with an acute increase in O2 tension. An acute increase in O2 tension did not increase fluorescence in nitro-l-arginine–treated PAECs (n = 23 cells; three coverslips, two animals). In DAF-FM–loaded PAECs derived from fetal lambs with chronic intrauterine pulmonary hypertension, an acute increase in O2 tension increased membrane fluorescence by only 1.7 ± 0.8% (n = 31 cells; four coverslips, two animals; p > 0.05 versus hypoxia; p < 0.001 versus control cells).
Effect of an acute increase in oxygen tension on NO production in fetal PAECs. An acute increase in oxygen tension caused an increase in DAF-FM membrane fluorescence (*p < 0.01 vs baseline, **p < 0.001, vs control; solid black line). With ongoing hypoxia (hypoxic time control; shaded line), there was no change in fetal PAEC DAF-FM membrane fluorescence. When fetal PAECs derived from fetal lambs with chronic intrauterine pulmonary hypertension (Hypertensive) were exposed to acute normoxia, there was no increase in DAF-FM membrane fluorescence.
DISCUSSION
We report that an acute increase in Po 2 directly increases [Ca2+]i in fetal PAECs (Fig. 1). With an acute increase in oxygen tension, the rate of calcium entry into PAECs increases (Fig. 2) and PAECs depolarize (Fig. 3). The sustained and progressive increase in PAEC [Ca2+]i entails calcium release from intracellular stores as previously reported (14,23) and increases PAEC NO production. As acetylcholine causes a greater increase in hypoxic, compared with normoxic PAEC [Ca2+]I, the low oxygen tension environment of the normal fetus may load the intracellular stores, thereby preparing PAECs to respond to acute normoxia. PAECs derived from fetal lambs with chronic intrauterine pulmonary hypertension do not respond to an acute increase in oxygen tension with either an increase in [Ca2+]i or NO production, supporting the proposition that the intrauterine environment informs the response of endothelial cells to physiologic stimuli (24).
Data supporting the notion that the initial normoxia associated increase in PAEC [Ca2+]i is dependent on the entry of extracellular calcium includes the observation that acute normoxia had no effect on [Ca2+]i in the presence of zero extracellular calcium solution and that upon reintroduction of extracellular calcium, PAEC [Ca2+]i increased. These results were further validated by experiments wherein the rate at which manganese quenched the fura-2 signal increased with acute normoxia, consistent with an increased rate of entry of extracellular calcium.
Although the initial component of the normoxia-induced increase in PAEC [Ca2+]i is dependent on entry of extracellular calcium, the present data demonstrate that release of Ca2+ from IP3-sensitive stores accounts for the sustained increase in PAEC [Ca2+]i. Pharmacological blockade of calcium release from ryanodine-sensitive stores had no effect on the initial component, but prevented the sustained and progressive elevation in PAEC [Ca2+]i, in response to acute normoxia. Although previous investigators have demonstrated a role for calcium release from ryanodine-sensitive stores in umbilical vein endothelial cells (25), the present data are the first to implicate a role for calcium release from ryanodine-sensitive stores in the normoxia-induced increase in fetal PAEC [Ca2+]i.
At birth, PAECs must contract, increase production of NO (8,26) and prostacylin (27,28), and decrease endothelin production (29) to enable effective gas exchange to occur in the lungs. Changing the exposure of PAECs from normoxia to hypoxia reduces reactive oxygen species (ROS) (30,31) so presumably the reverse is also true. Consequently, we can speculate that as H2O2 can inhibit K+ channels (31), the increase in ROS could cause membrane depolarization. This in turn could lead to calcium release from the endoplasmic reticulum (32). Alternatively, ROS are known to alter the ratio of the small G proteins RhoA and Rac1 leading to Ca2+ release (33).
The observation that endothelial cells from an animal model of PPHN demonstrate no increase in either [Ca2+]i or only a minimal increase in NO production in response to an acute increase in oxygen tension provides the first direct evidence that the chronic intrauterine pulmonary hypertension compromises PAEC oxygen sensing and NO production. The present data link endothelial cell cytosolic calcium and an acute increase in oxygen tension, one of the central perinatal physiologic stimuli (1).
The present study is limited by the absence of a mechanistic link between an increase in oxygen tension, an increase in the rate of calcium entry, and the consequent release of Ca2+ from IP3-sensitive stores and NO production. Exactly how the increase in cytosolic calcium leads to augmented NO production remains unknown. However, the observation that fetal PAECs maintained in culture respond to an acute increase in oxygen tension with an increase in cytosolic calcium, in direct contrast to the response of PAECs derived from the adult pulmonary vasculature (18,34), lends weight to the proposition that maturation-related physiologic differences exist in PAECs. Rigorous measures were undertaken to ensure that PAECs were not subject to dedifferentiation while maintained in culture. PAECs stained positively with endothelial cell–specific (factor VIII; acetylated LDL uptake, griffonia lectin) markers and did not stain positively for smooth muscle cell markers.
In conclusion, the present data indicate that fetal PAECs are able to sense and respond to an acute increase in oxygen tension with an increase in cytosolic calcium and NO production. The acute increase in oxygen tension that occurs at birth may lead to K+ channel inactivation, membrane depolarization, increased entry of extracellular calcium, and augmented NO production. The sustained elevation of PAEC calcium results, in part, from release of calcium from ryanodine-sensitive stores. From a teleologic perspective, the response of the PAECs to an acute increase in oxygen tension is biologically imperative. The present data suggest that compromised PAEC oxygen sensing may underlie the attenuated response of the pulmonary circulation to perinatal vasodilator stimuli, thereby leading to persistent pulmonary hypertension of the newborn.
Abbreviations
- PA:
-
pulmonary artery
- PAECs:
-
pulmonary artery endothelial cells
- PPHN:
-
persistent pulmonary hypertension of the newborn
References
Dawes GS, Mott JC, Widdicombe JG, Wyatt DG 1953 Changes in the lungs of the newborn lamb. J Physiol 121: 141–162
Emmanouilides GC, Moss AJ, Diuffie ER, Adams FH 1964 Pulmonary arterial pressure changes in human newborn infants from birth to 3 days of age. J Pediatr 65: 327–333
Cassin S, Dawes GS, Mott JC, Ross BB, Strang LB 1964 The vascular resistance of the fetal and newly ventilated lung of the lamb. J Physiol 171: 61–79
Cornfield DN, Chatfield BA, McQueston JA, McMurtry IF, Abman SH 1992 Effects of birth-related stimuli on L-arginine-dependent pulmonary vasodilation in ovine fetus. Am J Physiol 262: H1474–H1481
Accurso FJ, Albert B, Wilkening RB, Petersen RG, Meschia G 1986 Time-dependent response of fetal pulmonary blood flow to an increase in fetal oxygen tension. Respir Physiol 63: 43–52
Furchgott RF 1988 Studies on relaxation of rabbit aorta by sodium nitrite: the basis for the proposal that the acid-activatable inhibitory factor from bovine retractor penis is inorganic nitrite and the endothelium-derived relaxing factor is nitric oxide. In: Vanhoutte PM (eds) Vasodilatation. Raven Press, New York, pp 410–414
Yanagisawa M, Kurihara H, Kimura S, Tomobe Y, Kobayashi M, Mitsui Y, Yazaki Y, Goto K, Masaki T 1988 A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 332: 411–415
Abman SH, Chatfield BA, Hall SL, McMurtry IF 1990 Role of endothelium-derived relaxing factor during transition of pulmonary circulation at birth. Am J Physiol 259: H1921–H1927
Ivy DD, Kinsella JP, Abman SH 1994 Physiologic characterization of endothelin A and B receptor activity in the ovine fetal pulmonary circulation. J Clin Invest 93: 2141–2148
Morin FC 3rd, Eagan EA, Ferguson W, Lundgren CE 1988 Development of pulmonary vascular response to oxygen. Am J Physiol 254: H542–H546
Accurso FC 3rd, Wilkening RB 1988 Temporal response of the fetal pulmonary circulation to pharmacologic vasodilators. Proc Soc Exp Biol Med 187: 89–98
Abman SH, Shanley PF, Accurso FJ 1989 Failure of postnatal adaptation of the pulmonary circulation after chronic intrauterine pulmonary hypertension in fetal lambs. J Clin Invest 83: 1849–1858
Le Cras TD, Markham NE, Tuder RM, Voelkel NF, Abman SH 2002 Treatment of newborn rats with a VEGF receptor inhibitor causes pulmonary hypertension and abnormal lung structure. Am J Physiol Lung Cell Mol Physiol 283: L555–L562
Shaul PW, Wells LB 1994 Oxygen modulates nitric oxide production selectively in fetal pulmonary endothelial cells. Am J Respir Cell Mol Biol 11: 432–438
Assali NS, Kirchbaum TH, Dilts PV 1968 Effects of hyperbaric oxygen on utero placental and fetal circulation. Circ Res 22: 573–588
Busse R, Mülsch A, Fleming I, Hecker M 1993 Mechanisms of nitric oxide release from the vascular endothelium. Circulation 87: V18–V25
Villamor E, Le Cras TD, Horan MP, Halbower AC, Tuder RM, Abman SH 1997 Chronic intrauterine pulmonary hypertension impairs endothelial nitric oxide synthase in the ovine fetus. Am J Physiol 272: L1013–L1020
Stevens T, Cornfield DN, McMurtry IF, Rodman DM 1994 Acute reductions in PO2 depolarize pulmonary artery endothelial cells and decrease [Ca2+]i . Am J Physiol 266: H1416–H1421
Cornfield DN, Stevens T, McMurtry IF, Abman SH, Rodman DM 1994 Acute hypoxia causes membrane depolarization and calcium influx in fetal pulmonary artery smooth muscle cells. Am J Physiol 266: L469–L475
Olschewski A, Hong Z, Linden BC, Porter VA, Weir EK, Cornfield DN 2002 The contribution of the KCa channel to membrane potential and oxygen sensitivity is decreased in an ovine model of PPHN. Am J Physiol Lung Cell Mol Physiol 283: L1103–L1109
Porter VA, Reeve HL, Cornfield DN 2000 Fetal rabbit pulmonary artery smooth muscle cell response to ryanodine is developmentally regulated. Am J Physiol Lung Cell Mol Physiol 279: L751–L757
Garcia ML, Hanner M, Knaus HG, Koch R, Schmalhofer W, Slaughter RS, Kaczorowski GJ 1997 Pharmacology of potassium channels. Adv Pharmacol 39: 425–471
North AJ, Lau KS, Brannon TS, Wu LC, Wells LB, German Z, Shaul PW 1996 Oxygen upregulates nitric oxide synthase gene expression in ovine fetal pulmonary artery endothelial cells. Am J Physiol 270: L643–L649
Shaul PW, Yuhanna IS, German Z, Chen Z, Steinhorn RH, Morin FC 1997 Pulmonary endothelial NO synthase gene expression is decreased in fetal lambs with pulmonary hypertension. Am J Physiol 272: L1005–L1012
Frieden M, Graier WF 2000 Subplasmalemmal ryanodine-sensitive Ca2+ release contributes to Ca2+-dependent K+ channel activation in a human umbilical vein endothelial cell line. J Physiol 524: 715–724
Fineman JR, Wong J, Morin FC, Wild LM, Soifer SJ 1994 Chronic nitric oxide inhibition in utero produces persistent pulmonary hypertension in newborn lambs. J Clin Invest 93: 2675–2683
Shaul PW, Farrar MA, Magness RR 1993 Oxygen modulation of pulmonary arterial prostacyclin synthesis is developmentally regulated. Am J Physiol 265: H621–H628
Leffler CW, Hessler JR, Green RS 1984 Mechanism of stimulation of pulmonary prostacyclin synthesis at birth. Prostaglandins 28: 877–887
Rosenberg AA, Kennaugh J, Koppenhafer SL, Loomis M, Chatfield BA, Abman SH 1993 Elevated immunoreactive endothelin-1 levels in newborn infants with persistent pulmonary hypertension. J Pediatr 123: 109–114
Wojciak-Stothard B, Tsang LY, Paleolog E, Hall SM, Haworth SG 2006 Rac1 and RhoA as regulators of endothelial phenotype and barrier function in hypoxia-induced neonatal pulmonary hypertension. Am J Physiol Lung Cell mol Physiol 290: L1173–1182
Reeve HL, Michelakis E, Nelson DP, Weir EK, Archer SL 2001 Alterations in a redox oxygen sensing mechanism in chronic hypoxia. J Appl Physiol 90: 2249–2256
del Valle-Rodriguez A, Lopez-Barneo J, Urena J 2003 Ca2+ channel-sarcoplasmic reticulum coupling: a mechanism of arterial myocyte contraction without Ca2+ influx. EMBO J 22: 4337–4345
Wojciak-Stothard B, Tsang LY, Haworth SG 2005 Rac and Rho play opposing roles in the regulation of hypoxia/reoxygenation-induced permeability changes in pulmonary artery endothelial cells. Am J Physiol Lung Cell mol Physiol 288: L749–L760
Hampl V, Cornfield DN, Cowan NJ, Archer S 1995 Hypoxia potentiates nitric oxide synthesis and transiently increases cytosolic calcium levels in pulmonary artery endothelial cells. Eur Respir J 8: 515–522
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by National Institutes of Health grants RO1 HL60784 (D.N.C.), RO1 HL70628 (D.N.C.), and RO1 HL65322 (E.K.W.); VA Merit Review Funding (E.K.W.); American Heart Association Established Investigator Award (D.N.C.); and Viking Children's Fund (E.R.). D.N.C. is an Established Investigator of the American Heart Association.
The findings were presented in part at the Society for Pediatric Research Meeting on May 5, 2004.
Rights and permissions
About this article
Cite this article
Tirosh, R., Resnik, E., Herron, J. et al. Acute Normoxia Increases Fetal Pulmonary Artery Endothelial Cell Cytosolic Ca2+ Via Ca2+-Induced Ca2+ Release. Pediatr Res 60, 258–263 (2006). https://doi.org/10.1203/01.pdr.0000233077.29866.f0
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000233077.29866.f0