Abstract
Brain damage around birth may cause lifelong neurodevelopmental deficits. We examined the therapeutic potential of human umbilical cord blood–derived mononuclear cells containing multipotent stem cells to facilitate motor recovery after cerebral hypoxic-ischemic damage in neonatal rats. Left carotid artery ligation followed by 8% O2 inhalation for 80 min was performed on postnatal d 7, succeeded by intraperitoneal transplantation of human umbilical cord blood–derived mononuclear cells on postnatal d 8 in a sham-controlled design. Histologic and immunohistochemical analysis on postnatal d 21 revealed that neonates developed severe cerebral damage after the hypoxic-ischemic insult. These animals also suffered from contralateral spastic paresis, as evidenced by their locomotor behavior. After transplantation of human umbilical cord blood–derived mononuclear cells, spastic paresis was largely alleviated, resulting in a normal walking behavior. This “therapeutic” effect was accompanied by the fact that mononuclear cells had entered the brain and were incorporated around the lesion without obvious signs of transdifferentiation. This study demonstrates that intraperitoneal transplantation of human umbilical cord blood–derived mononuclear cells in a rat model of perinatal brain damage leads to both incorporation of these cells in the lesioned brain area and to an alleviation of the neurologic effects of cerebral palsy as assessed by footprint and walking pattern analysis.
Similar content being viewed by others
Main
Each year, thousands of children incur perinatal brain damage that potentially results in lifelong sequelae (1,2). Depending on the extent and location of the insult these children may develop spastic paresis, choreo-athetosis, ataxia, and disorders of sensorimotor coordination (1). In the United States, estimates of the costs to society for treatment and care of these children amount to a total of $11.5 billion per birth year (2).
One of the major causes of perinatal brain damage is severe fetal or neonatal asphyxia (3,4), resulting in cerebral hypoxic-ischemic insults and hemorrhages. Experimental evidence has shown that neuroprotective strategies using pharmacologic agents or moderate cerebral hypothermia may ameliorate perinatal brain damage (5,6). However, limited clinical strategies are available for functional regeneration of damaged nervous structures in the perinatal period (7). Therefore, one of the most urgent tasks for scientists and clinicians will be to explore the enormous potential of cell therapies using stem cells in general and hUCB-derived cells in particular to provide a therapeutic paradigm for perinatal neuronal repair.
For hUCB cell transplantation, a number of promising experimental protocols have been established in sheep (8) and rats (9). The study by Chen et al. (9) provides first experimental evidence in adult rats that intravenous application of umbilical cord blood cells results in the migration of these cells toward brain regions affected by stroke. Furthermore, behavioral studies on those animals revealed an at least partial functional compensation.
The insult resulting from perinatal hypoxic-ischemic brain damage in humans has been reproduced in a neonatal rat model (Levine model) (10–12). Here, we present a study designed to investigate the potential of hUCB-derived mononuclear cells to migrate to a hypoxic-ischemic brain lesion from a distant transplantation site, and to examine their potential to alleviate neurologic deficits in neonatal rats. Our results demonstrate that intraperitoneal transplantation of hUCB-mononuclear cells after a hypoxic-ischemic insult results both in the migration of these cells toward the lesion in the neonatal rat brain and in the recovery from spastic paresis as assessed by walking pattern analysis.
MATERIALS AND METHODS
hUCB-derived mononuclear cells.
Blood from umbilical cord and placenta was obtained from the Department of Gynecology and Obstetrics (Ruhr-University Bochum, Germany), after receiving the mother's informed consent. The umbilical vein was punctured post partum, and the blood was collected in umbilical cord blood collection bags containing citrate phosphate dextrose as an anticoagulant (Maco Pharma, Langen, Germany) and stored at room temperature up to 24 h until further processing.
Preparation of the mononuclear cell fraction was performed by Ficoll Paque (Amersham, Freiburg, Germany) density gradient centrifugation according to the manufacturer's instructions. The mononuclear fraction of cells was collected from the interphase, resuspended in 0.9% sodium chloride, and the cell number was determined. Viability of resuspended mononuclear cells was 97 ± 2%.
Cerebral ischemia.
The Levine model (10,13) was used to achieve reproducible hypoxic-ischemic injury in neonatal rats. Seven-day-old Wistar rat pups were deeply anesthetized by inhalation of 4% halothane and maintained with 1.5% halothane in 50% N2O/50% O2. The left common carotid artery was exposed, double-ligated with 6–0 surgical silk, and severed. The duration of anesthesia and surgery did not exceed 10 min. After surgery, the rat pups were allowed to recover in their home cages for 1 h. To introduce systemic hypoxia, the pups were subsequently placed in an incubator (Incubator 7510; Dräger, Lübeck, Germany) and exposed to a hypoxic gas mixture (8% oxygen, 92% nitrogen) for 80 min. The environmental temperature was strictly maintained at 36°C.
All surgical and experimental protocols were approved by the appropriate institutional review committee (Bezirksregierung Arnsberg, Germany) and met the guidelines of the German animal protection law.
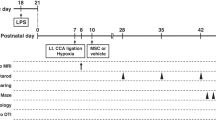
Experimental protocol.
Randomly selected animals were assigned to three different experimental groups: controls (no lesion), lesion (without transplantation), and lesion followed by transplantation of mononuclear cells.
Animals of the lesion group (lesion only, n = 11) were subjected to ligation of the left common carotid artery, followed by systemic hypoxia. Twenty-four hours after the insult, this group received an intraperitoneal injection of 500 μL of 0.9% sodium chloride (sham injection). In the transplantation group (lesion followed by transplantation, n = 14), rats received 1 × 107 hUCB-derived mononuclear cells (in a volume of 500 μL 0.9% sodium chloride) by intraperitoneal injection 24 h after the hypoxic-ischemic insult. The control group (no lesion, n = 11) comprised of animals that did not undergo any treatment or surgery (n = 5), and of sham-operated animals that were anesthetized, the carotid artery exposed but not ligated, and surgery then terminated (n = 6). After initial analysis, these latter two groups were indistinguishable in motor analysis, and therefore combined. Additional control animals (no lesion, n = 10), which received intraperitoneal injection of 1 × 107 hUCB-derived mononuclear cells, were included in motor analysis. There was no use of immunosuppressants or analgesics in any experimental group. Animals were included into subsequent analyses when displaying a severe macroscopic lesion accompanied by cystic changes larger than 4 mm upon hypoxic-ischemic damage without (11 out of 18 animals) or with (14 out of 20 animals) transplantation of hUCB-derived cells, thereby disregarding animals in which the Levine procedure resulted in minor lesions. For the control group, animals were included when displaying an intact brain without pigmentation or cystic changes (11 out of 13 animals).
Analysis of motor abilities.
Footprint analysis was performed on postnatal d 21 in a strictly blinded fashion. The paws were colored consecutively, and the footprints were printed onto paper when the rat walked along a defined gangway which was elevated by 35°. Footprints were then measured and each imprint was analyzed regarding the distance between the first and fifth toe (hind paws) or between the first and the fourth digit (forepaws) (14). In addition, the step length was determined for each paw. A significant decrease in footprint width and/or step length of the limbs contralateral to the lesion compared with that of the ipsilateral site was considered to reflect spastic paresis.
Macroscopic assessment.
Rats were anesthetized by CO2 exposition and decapitated at postnatal d 21. Brains were dissected and brain injury was assessed immediately after dissecting the brains (11). Neonatal rats were considered to have suffered hypoxic-ischemic brain damage when displaying a cystic infarction, similar to a unilateral internal hydrocephalus, on the brain surface ipsilateral to the carotid artery occlusion.
Microscopic assessment.
Brains were covered in tissue freezing medium (Leica, Nussloch, Germany) and frozen in 8% methylcyclohexane in 2-methylbutan (vol/vol) (–80°C). Histology and immunohistochemistry were performed on cryosections of 14-μm thickness, which had been mounted onto Superfrost Plus slides (BDH, London, UK) and heat dried for 1 h at 40°C before fixation.
Precise localization of the lesion areas was assured by histologic staining according to Klüver-Barrera, showing myelinated fiber tracts in light green and cell bodies in blue. The lesion size was determined by measuring the hemisphere areas in histologic sections. Measurements were performed in nine histologic sections at three defined levels in the brain, and in three animals per group (control, lesion, lesion plus transplantation). The extent of brain damage was expressed as area of the left (lesioned) hemisphere as percentage of the area of the right (nonlesioned) hemisphere.
For immunohistochemistry, adjacent cryosections were fixed in –20°C cold ethanol, rinsed in PBS and preincubated in blocking buffer (BB, 10% normal goat serum and 0.1% TritonX-100 in PBS) for 30 min. Primary antibodies were diluted in BB and sections were incubated at 18°C overnight. Samples were rinsed in PBS and incubated in 0.2% BSA in PBS. Incubation with secondary antibodies was performed in BB at 18°C for 2 h. Sections were mounted using the ProLong Antifade Kit (Molecular Probes, Leiden, Netherlands). Fluorescence was documented using confocal imaging microscopy (Zeiss LSM 510 META). Data were collected using the single track scanning module and exported as TIFF files into Adobe Photoshop 7.0 (Adobe Imaging Systems Inc., Mountain View, CA).
Primary antibodies (dilution and supplier in parentheses) were directed against HLA-DR α-chain (1:50; DAKO, Hamburg, Germany), cleaved caspase3 (1:100; New England Biolabs, Frankfurt, Germany), CD68 (ED1; 1:100; Serotec, Düsseldorf, Germany), glial fibrillary acidic protein (GFAP; monoclonal: 1:100, Chemicon, Hofheim, Germany; polyclonal: 1:100, Sigma Chemical Co., Taufkirchen, Germany). Primary antibodies used to determine neuronal differentiation of HLA-DR-labeled hUCB-derived mononuclear cells included the polyclonal GFAP antibody, neurofilament-68 (Chemicon), and synaptophysin antibodies (Diagnostic Biosystems, Pleasanton, CA). Reactivity of these antibodies with human cells had been confirmed in vitro (data not shown).
Secondary antibodies were Alexa Fluor 488 or 546 conjugated goat-anti-rabbit or goat-anti-mouse (1:3,000; Molecular Probes).
Statistical analysis.
The Kolmogorov-Smirnov test was performed to demonstrate that test distributions were normal. Further analysis of intra- and intersample variability was done by two-way ANOVA (SuperANOVA; Abacus Concepts Inc., Berkeley, CA), followed by the appropriate posthoc test (Student-Newman-Keuls). Data are expressed as mean ± SEM. A value of p < 0.05 was considered statistically significant.
RESULTS
Hypoxic-ischemic brain damage in perinatal rats.
Cerebral hypoxia-ischemia resulted in macroscopic changes, including cystic lesions (n = 11). There was no evidence of any brain damage in control rats (n = 12). The rostrocaudal extent of the damage was determined and averaged 6.1 ± 0.6 mm in lesioned brains. Histopathological analysis revealed that hypoxic-ischemic brain damage affected cortex, hippocampus, and periventricular areas (Fig. 1, A–C), and comprised inflammation and neuronal cell death (see below).
Histology of the hypoxic-ischemic brain lesion. (A) The level of coronal sections shown in B and C is indicated in a schematic drawing. (B) Histologic staining (Klüver-Barrera) reveals damage of the left brain hemisphere, i.e. ipsilateral to the carotid artery occlusion. The lesion affects the hippocampus (hc), parietal and temporal cortex (cx), periventricular areas (pv), and results in an enlarged lateral ventricle (v). (C) Schematic representation of the histologic features observed in B. Boxed areas were analyzed immunohistochemically, shown in Figures 2 and 3. Scale bar: 1 mm.
The extent of inflammation was determined by CD68-immunopositive activated microglia (15). Apoptotic neuronal cell death was detected by cleaved-caspase3 immunoreactivity (16). There were activated microglia (green) in a large region of the lesioned hemisphere, whereas the apoptotic neuronal cells were clustered within (red), as depicted in Figure 2, A and B. Intact areas of the ipsilateral hemisphere as well as the contralateral hemisphere were devoid of any immunoreactivity to CD68, indicating the absence of inflammation (Fig. 2, A and C; green). However, weak cleaved-caspase3 immunoreactivity was detectable in intact hemispheres (Fig. 2, A and C; red), as described previously during brain development (17).
Activated microglia and apoptotic neuronal cells are located in the vicinity of the hypoxic-ischemic lesion. (A) Schematic representation of the lesion site as indicated by the presence of CD68-immunopositive cells (green) and cleaved-caspase3 expressing cells (red). Immunohistochemistry is presented for areas B and C. (B) Immunohistochemistry for CD68 (green fluorescence), showing activated microglia, and cleaved-caspase3 immunoreactivity (red fluorescence) indicating apoptosis in the lesioned hemisphere. (C) The nonlesioned hemisphere is devoid of activated microglia (green fluorescence) and shows few weakly labeled caspase3-positive cells as characteristic for neonatal rat brain. Scale bar: 100 μm.
“Homing” of human umbilical mononuclear cells.
Transplantation of human mononuclear cells (1 × 107) derived from umbilical cord blood was performed by intraperitoneal injection 24 h after the hypoxic-ischemic insult, i.e. in postnatal d 8 rats (n = 14), in a sham-controlled fashion. Cells were identified by immunohistochemical detection of human-specific HLA-DR α-chain surface antigens (18). Thus, we demonstrate that transplanted human mononuclear cells migrate from the intraperitoneal cavity to the damaged brain region (Fig. 3, A and B; green). These cells were detectable in the brain as early as 3 d after intraperitoneal transplantation and were still present in the lesioned hemisphere 2 wk after transplantation (Fig. 3, A and B; green). Confocal microscopy revealed that transplanted cells (green immunofluorescence in Fig. 3B) were clearly incorporated into the astrocytic network (red immunofluorescence in Fig. 3, B–D). In contrast, there was no evidence for human cells outside the damaged brain region (Fig. 3C), and there was no HLA immunoreactivity in the lesioned areas of animals that had not received transplantation of hUCB-derived mononuclear cells (Fig. 3D). Interestingly, transplanted human cells found in the brain were strictly confined to the area of activated microglia (compare Fig. 2A; green).
Intraperitoneal transplantation of mononuclear hUCB-derived cells resulted in a specific “homing” of these cells into the CNS and incorporation around the lesioned area. (A) Schematic representation of the distribution of human cells in the lesioned hemisphere. HLA-DR-positive cells (green) are detected in the area of the hypoxic-ischemic lesion. Contralateral hemispheres were devoid of human cells. Immunohistochemistry is demonstrated for boxed areas in B (lesioned hemisphere) and C (nonlesioned hemisphere). (B) HLA-DR-positive mononuclear cells (green) are located within a scaffold of GFAP-positive astrocytes (red) in the area of the hypoxic-ischemic lesion. (C) Nonlesioned parts of the brain, as demonstrated by the absence of inflammatory and apoptotic events (compare Fig. 2), are devoid of human cells (absence of green fluorescence). (D) Lesioned areas of the brain of animals that did not receive transplantation of human cells are devoid of HLA-immunostaining. Note absence of green immunofluorescence (HLA-staining) within the red scaffold of GFAP-positive rat astrocytes. Scale bar in B, C: 100 μm; in D: 20 μm.
Transplantation of hUCB cells did not change the severity of morphologic damage. In control animals, left and right hemisphere comprised approximately the same area. Upon hypoxic-ischemic brain injury, the area of the lesioned hemisphere was 34.99 ± 4.7% of that of the intact hemisphere. In lesioned animals that had received transplantation of hUCB-derived mononuclear cells, the lesioned hemisphere area comprised 35.72 ± 0.4% of the intact hemisphere area, which was not significantly different from nontransplanted animals (p ≥ 0.05). In addition, HLA-DR-immunopositive cells did not display obvious signs of transdifferentiation in vivo, as assessed by their phenotype and the absence of GFAP, an intermediate filament expressed in neural progenitor cells, and neuron-specific proteins like neurofilament-68 and synaptophysin (Fig. 4), although expression of these markers was observed upon cultivation of hUCB-derived mononuclear cells in the presence of nerve growth factor and retinoic acid in vitro (data not shown).
Transplanted HLA-immunopositive human UCB-derived mononuclear cells do not reveal signs of transdifferentiation upon “homing” to the hypoxic-ischemic lesion. (A, B) GFAP (red), characteristic for astrocytes as well as neuroglial progenitor cells, is located in close vicinity to human HLA-DR-positive cells (green), however, there is no obvious overlap between GFAP- and HLA-DR-immunofluorescence. The neuron-specific proteins NF-68 (C, D) and synaptophysin (E, F) are expressed in the brain tissue (red fluorescence), however, HLA-positive cells (green fluorescence) are devoid of NF-68 and synaptophysin immunostaining. Scale bar in A, C, E: 20 μm; B, D, F: 50 μm.
Perinatal brain damage causes spastic paresis. To examine whether transplantation of hUCB-derived mononuclear cells after cerebral hypoxic-ischemic brain damage has beneficial effects on locomotor behavior, we performed a strictly blinded footprint and walking pattern analysis. Our analysis of the toe distance 1 to 5 of the hind paw contralateral to the cerebral damage at 3 wk of age revealed a highly significant reduction (p < 0.001) of this measure after cerebral damage (0.99 ± 0.04 cm; n = 10) compared with controls (1.15 ± 0.04 cm; n = 12), which is characteristic for spastic paresis. As animals after hypoxic-ischemic lesion were smaller (43.2 ± 3.2 g) than control animals (50.3 ± 3.1 g) of the same age, an intraindividual comparison of footprint width was performed. In control animals (without transplantation), there was no significant difference in toe distance between left (1.16 ± 0.03 cm) and right (1.15 ± 0.04 cm; p ≥ 0.05; Fig. 5 A) hind paws. In nonlesioned control animals, transplantation of hUCB cells did not result in significant differences in the toe distance of left (1.19 ± 0.01 cm) and right (1.21 ± 0.01 cm; p ≥ 0.05) hind paws. However, in lesioned animals (without transplantation), the toe distance of the ipsilateral hind paw (1.12 ± 0.03 cm) differed significantly from that of the contralateral hind paw (0.99 ± 0.04 cm; p < 0.05; Fig. 5A), and this difference is independent of the animal's weight.
Transplantation of hUCB-derived mononuclear cells reduces spastic paresis as assessed by footprint analysis of 3-wk-old animals. (A) Hypoxic-ischemic brain damage results in spastic paresis of the distal limb muscles, causing a significant reduction of footprint width (toe distance 1 to 5) of the right hind paw (contralateral to the insult; black columns) compared with the left (ipsilateral; gray columns) hind paw. Intraperitoneal transplantation of hUCB-derived mononuclear cells after hypoxic-ischemic brain damage reduced spastic paresis. In these animals, differences between ipsi- and contralateral hind paws were no longer detectable. Photographs of footprints (right hind paws) illustrate the footprint widths (arrows) of control animals without (left) and with (center left) transplantation, upon hypoxic-ischemic lesion without (center right) and with (right) transplantation of hUCB-derived mononuclear cells. (B) In control animals with and without transplantation, the step length of left and right hind paws is equal. In contrast, hypoxic-ischemic lesion resulted in a significantly reduced step length of the right hind paw (black columns) compared with the left hind paw (gray columns). This reduction in step length of the hind paw contralateral to the lesion, also indicative of spastic paresis, was largely alleviated upon transplantation of hUCB-derived mononuclear cells. Data are presented as mean ± SEM; *p < 0.05; ***p < 0.001.
Furthermore, in animals with hypoxic-ischemic lesion, there was evidence for a reduction of the step length of the right hind paw (contralateral to the lesion; 7.57 ± 0.07 cm) compared with the left hind paw controls (8.26 ± 0.33 cm; p < 0.05; Fig. 5B), which is also characteristic of spastic paresis (19).
Intraperitoneal transplantation of umbilical mononuclear cells reduces spastic paresis.
Most importantly, our results show that these neurologic deficits were eliminated following transplantation of hUCB mononuclear cells. There was a dramatic alleviation of the contralateral spastic paresis for all parameters back to normal (Fig. 5). Upon transplantation, there was no significant difference detected between toe distances 1–5 of the ipsilateral (1.20 ± 0.03 cm) and contralateral (1.21 ± 0.04 cm) hind paws of animals after hypoxic-ischemic lesion and transplantation (p ≥ 0.05). The step length of the ipsilateral (8.46 ± 0.4 cm) hind paws also equaled that measured on the contralateral side (8.40 ± 0.32 cm; p ≥ 0.05). Interestingly, the weight of these animals (51.4 ± 1.4 g) was similar to that of control animals, however, it differed significantly from that of lesioned animals that had not received hUCB-cell transplantation (p < 0.05).
DISCUSSION
In this study, we used a model of perinatal hypoxic-ischemic brain damage in rats. The insult was morphologically characterized by hemorrhage, neuronal death, and inflammation, and functionally by spastic paresis of contralateral fore- and hind limbs. Intraperitoneal transplantation of human UCB-derived mononuclear cells resulted in a) migration of cells from the peritoneal cavity to the CNS, b) incorporation of cells around the cerebral lesion (“homing”), and c) an alleviation of spastic paresis.
Unlike other studies, we used the intraperitoneal cavity for transplantation. The migration of transplanted cells from the intraperitoneal cavity to the damaged region of the brain suggests the presence of very specific and powerful chemoattractant signals. One component of the complex mechanism seems to be the expression of cytokines/chemokines in the brain in response to hypoxic-ischemic brain injury (20). The chemoattractant effect of adult ischemic brain tissue had previously been demonstrated by cell migration assays, in which hUCB-derived cells were shown to migrate towards tissue extract derived from lesioned brain hemispheres (9). In our paradigm, invasion of mononuclear cells was very focused in that it was confined to the hypoxic-ischemic region of the brain. More general patterns of brain damage as observed in human genetic metabolic disorders like Krabbe leukodystrophy lead to a more widespread distribution of damaged neurons, and hence result in a ubiquitous distribution of transplanted human hUCB cells (21,22).
The specificity of “homing” within the hypoxic-ischemic brain may both be linked to specific chemoattractants (20) and to the lack of a functioning blood-brain-barrier in the damaged brain regions (13,23) leading to a facilitated intrusion of human mononuclear cells into damaged regions and to a preferential regional incorporation of these cells. Furthermore, successful “homing” might be related to the early transplantation after the insult, because then concentrations of chemoattractants are likely to be maximal, and, secondly, there is a known optimal point in time for transplantation in rodents within the first 2 wk after the insult (24).
Successful “homing” may be also related to the use of crude, rather than predifferentiated, hUCB-derived mononuclear cells for transplantation in this study, resulting in a minimal manipulation of cells, which was limited to density gradient centrifugation and resuspension in sodium chloride only. Thus, the full potential of cell (sub-) populations and that of cellular responsiveness to sense signals important to entrain migration to the damaged brain region may have been preserved.
Transplantation of human mononuclear cells into neonatal rats also warrants some considerations concerning graft–host interactions. Our results suggest some degree of immune tolerance toward cord blood cells, possibly mediated by diminished generation of cytotoxic responses of the host (25) through IL-10 release by these cells (26).
Neurologic deficits like contralateral spastic paresis and reduced step length are characteristic of pyramidal tract impairment in human newborns. Thus, the most important issue in any therapeutic approach, i.e. functional recovery, was achieved in our model. Footprint analysis represents one of the most sensitive parameters to detect pyramidal motor dysfunction in early neonatal life (19).
Irrespective of the striking “therapeutic” effect of mononuclear cell transplantation that also included the normalization of the weight, the underlying mechanisms remain largely unknown. Interestingly, we produced no evidence for neural differentiation of these transplanted human cells in the rat brain, even though hUCB mononuclear cells in our hands showed expression of a variety of neural markers in vitro using differentiation media (data not shown). This appears in part at variance with observations by Zigova et al. (27). However, this study is not directly comparable due to the methods used by those authors, i.e. predifferentiation of hUCB cells, intracisternal injection of cells, and the use of P1 rats. In our study, there was no change in the phenotype of HLA-positive mononuclear cells or in the expression of glial or neuronal marker proteins even though there was clear structural integration of the human cells into the three-dimensional astrocytic scaffold of the rat brain. None of the neural markers used yielded positive immunohistochemical staining of HLA-positive transplanted human cells. Although we were able to demonstrate a strong therapeutic effect of the transplantation by largely alleviating the neurologic deficits observed in rats after cerebral hypoxic ischemia without transplantation, the beneficial functional outcome appears to be unrelated to true cell replacement by differentiation of transplanted human cells. Thus, a permissive effect is suggested, as observed in the lesioned heart (28) and brain (29). Hence, in our model of hypoxic-ischemic brain damage, we propose secondary mechanisms, which may reduce adverse effects resulting from neural damage per se. Tentative candidates for these secondary mechanisms are increased vascularization, reduced edema, detoxification, prevention of gliosis, and others. Also, “bystander effects” mediated by other trophic factors, including glial cell line–derived neurotrophic factor, brain-derived neurotrophic factor, and nerve growth factor, may contribute to functional recovery caused e.g. by extensive host axonal growth and increased neuronal survival (30). Furthermore, recruitment of endogenous neural stem cells, e.g. elicited through cytokine and growth factor release, ought to be considered.
In summary, we show in a neonatal cerebral hypoxia-ischemia model that hUCB-derived mononuclear cells transplanted intraperitoneally enter the rat brain and incorporate specifically around the lesion (“homing”) in large numbers. Transplantation results in substantial alleviation of spastic paresis as assessed by footprint recordings of the hind paw contralateral to the damaged brain hemisphere and walking track analysis. This study provides important information for the development of therapeutic strategies using hUCB stem cells after perinatal brain damage to reduce potential sensorimotor deficits.
Abbreviations
- GFAP:
-
glial fibrillary acidic protein
- HLA-DR:
-
human leukocyte antigen type DR
- hUCB:
-
human umbilical cord blood
References
Volpe JJ 2001 Neurology of the Newborn. WB Saunders, Philadelphia pp 217–396
Centers for Disease Control and Prevention (CDC) 2003 Economic Costs Associated with Mental Retardation, Cerebral Palsy, Hearing Loss, and Vision Impairment—United States. MMWR Morb Mortal Wkly Rep 53: 57–59
Jensen A, Berger R 1991 Fetal circulatory responses to oxygen lack. J Dev Physiol 16: 181–207
Jensen A, Garnier Y, Middelanis J, Berger R 2003 Perinatal brain damage—from pathophysiology to prevention. Eur J Obstet Gynecol Reprod Biol 110: S70–S79
Hamrick SE, Ferriero DM 2003 The injury response in the term newborn brain: can we neuroprotect?. Curr Opin Neurol 16: 147–154
Vannucci RC, Connor JR, Mauger DT, Palmer C, Smith MB, Towfighi J, Vannucci SJ 1999 Rat model of perinatal hypoxic-ischemic brain damage. J Neurosci Res 55: 158–163
Gluckman PD, Wyatt JS, Azzopardi D, Ballard R, Edwards AD, Ferriero DM, Polin RA, Robertson CM, Thoresen M, Whitelaw A, Gunn AJ 2005 Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet 365: 663–670
Kogler G, Sensken S, Airey JA, Trapp T, Muschen M, Feldhahn N, Liedtke S, Sorg RV, Fischer J, Rosenbaum C, Greschat S, Knipper A, Bender J, Degistirici O, Gao J, Caplan AI, Colletti EJ, Almeida-Porada G, Muller HW, Zanjani E, Wernet P 2004 A new human somatic stem cell from placental cord blood with intrinsic pluripotent differentiation potential. J Exp Med 200: 123–135
Chen J, Sanberg PR, Li Y, Wang L, Lu M, Willing AE, Sanchez-Ramos J, Chopp M 2001 Intravenous administration of human umbilical cord blood reduces behavioral deficits after stroke in rats. Stroke 32: 2682–2688
Levine S 1960 Anoxic-ischemic encephalopathy in rats. Am J Pathol 36: 1–17
Bona E, Johansson BB, Hagberg H 1997 Sensorimotor function and neuropathology five to six weeks after hypoxia-ischemia in seven-day-old rats. Pediatr Res 42: 678–683
Hagberg H, Gilland E, Diemer NH, Andine P 1994 Hypoxia-ischemia in the neonatal rat brain: histopathology after post-treatment with NMDA and non-NMDA receptor antagonists. Biol Neonate 66: 205–213
Rice JE 3rd, Vannucci RC, Brierley JB 1981 The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann Neurol 9: 131–141
de Medinaceli L, Freed WJ, Wyatt RJ 1982 An index of the functional condition of rat sciatic nerve based on measurements made from walking tracks. Exp Neurol 77: 634–643
Ivacko JA, Sun R, Silverstein FS 1996 Hypoxic-ischemic brain injury induces an acute microglial reaction in perinatal rats. Pediatr Res 39: 39–47
Wang X, Karlsson JO, Zhu C, Bahr BA, Hagberg H, Blomgren K 2001 Caspase-3 activation after neonatal rat cerebral hypoxia-ischemia. Biol Neonate 79: 172–179
Hu BR, Liu CL, Ouyang Y, Blomgren K, Siesjo BK 2000 Involvement of caspase-3 in cell death after hypoxia-ischemia declines during brain maturation. J Cereb Blood Flow Metab 20: 1294–1300
Adams TE, Bodmer JG, Bodmer WF 1983 Production and characterization of monoclonal antibodies recognizing the alpha-chain subunits of human ia alloantigens. Immunology 50: 613–624
Hare GM, Evans PJ, Mackinnon SE, Best TJ, Midha R, Szalai JP, Hunter DA 1993 Walking track analysis: utilization of individual footprint parameters. Ann Plast Surg 30: 147–153
Bona E, Andersson AL, Blomgren K, Gilland E, Puka-Sundvall M, Gustafson K, Hagberg H 1999 Chemokine and inflammatory cell response to hypoxia-ischemia in immature rats. Pediatr Res 45: 500–509
Daley GQ, Goodell MA, Snyder EY 2003 Realistic prospects for stem cell therapeutics. Hematology (Am Soc Hematol Educ Program) 1: 398–418
Escolar ML, Poe MD, Provenzale JM, Richards KC, Allison J, Wood S, Wenger DA, Pietryga D, Wall D, Champagne M, Morse R, Krivit W, Kurtzberg J 2005 Transplantation of umbilical-cord blood in babies with infantile Krabbe's disease. N Engl J Med 352: 2069–2081
Muramatsu K, Fukuda A, Togari H, Wada Y, Nishino H 1997 Vulnerability to cerebral hypoxic-ischemic insult in neonatal but not in adult rats is in parallel with disruption of the blood-brain barrier. Stroke 28: 2281–2289
Park KI, Liu S, Flax JD, Nissim S, Stieg PE, Snyder EY 1999 Transplantation of neural progenitor and stem cells: developmental insights may suggest new therapies for spinal cord and other CNS dysfunction. J Neurotrauma 16: 675–687
Risdon G, Gaddy J, Broxmeyer HE 1994 Allogeneic responses of human umbilical cord blood. Blood Cells 20: 566–572
Rainsford E, Reen DJ 2002 Interleukin 10, produced in abundance by human newborn T cells, may be the regulator of increased tolerance associated with cord blood stem cell transplantation. Br J Haematol 116: 702–709
Zigova T, Song S, Willing AE, Hudson JE, Newman MB, Saporta S, Sanchez-Ramos J, Sanberg PR 2002 Human umbilical cord blood cells express neural antigens after transplantation into the developing rat brain. Cell Transplant 11: 265–274
Balsam LB, Wagers AJ, Christensen JL, Kofidis T, Weissman IL, Robbins RC 2004 Haematopoietic stem cells adopt mature haematopoietic fates in ischaemic myocardium. Nature 428: 668–673
Ourednik J, Ourednik V, Lynch WP, Schachner M, Snyder EY 2002 Neural stem cells display an inherent mechanism for rescuing dysfunctional neurons. Nat Biotechnol 20: 1103–1110
Lu P, Jones LL, Snyder EY, Tuszynski MH 2003 Neural stem cells constitutively secrete neurotrophic factors and promote extensive host axonal growth after spinal cord injury. Exp Neurol 181: 115–129
Acknowledgements
The authors thank Nicole-Christiane Kozik, Hans-Werner Habbes, Janet Moers, and Kerstin Schmitz for excellent technical assistance, and Petra Parakenings and Helga Schulze for expertly done photographic work.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants of the Stem Cell Network North Rhine Westphalia (C.M., A.J.) and by the Medical Faculty of Ruhr-University Bochum (FoRUM) (A.J.).
Rights and permissions
About this article
Cite this article
Meier, C., Middelanis, J., Wasielewski, B. et al. Spastic Paresis After Perinatal Brain Damage in Rats Is Reduced by Human Cord Blood Mononuclear Cells. Pediatr Res 59, 244–249 (2006). https://doi.org/10.1203/01.pdr.0000197309.08852.f5
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000197309.08852.f5
This article is cited by
-
Neuroprotective therapies in the NICU in term infants: present and future
Pediatric Research (2023)
-
Autologous cord blood cell therapy for neonatal hypoxic-ischaemic encephalopathy: a pilot study for feasibility and safety
Scientific Reports (2020)
-
Effects of umbilical cord blood cells, and subtypes, to reduce neuroinflammation following perinatal hypoxic-ischemic brain injury
Journal of Neuroinflammation (2018)
-
Umbilical cord blood cells for treatment of cerebral palsy; timing and treatment options
Pediatric Research (2018)
-
From cord to caudate: characterizing umbilical cord blood stem cells and their paracrine interactions with the injured brain
Pediatric Research (2018)







