Abstract
Diamond-Blackfan anemia (DBA) is a constitutional disease characterized by a specific maturation defect in cells of erythroid lineage. We have assembled a registry of 229 DBA patients, which includes 151 patients from France, 70 from Germany, and eight from other countries. Presence of malformations was significantly and independently associated with familial history of DBA, short stature at presentation (before any steroid therapy), and absence of hypotrophy at birth. Two hundred twenty-two patients were available for long-term follow-up analysis (median, 111.5 mo). Of these individuals, 62.6% initially responded to steroid therapy. Initial steroid responsiveness was found significantly and independently associated with older age at presentation, familial history of DBA, and a normal platelet count at the time of diagnosis. Severe evolution of the disease (transfusion dependence or death) was significantly and independently associated with a younger age at presentation and with a history of premature birth. In contrast, patients with a familial history of the disease experienced a better outcome. Outcome analysis revealed the benefit of reassessing steroid responsiveness during the course of the disease for initially nonresponsive patients. Bone marrow transplantation was successful in 11/13 cases; HLA typing of probands and siblings should be performed early if patients are transfusion dependent, and cord blood should be preserved. Incidence of DBA (assessed for France over a 13-y period) is 7.3 cases per million live births without effect of seasonality on incidence of the disease or on malformative status. Similarly, no parental imprinting effect or anticipation phenomenon could be documented in families with dominant inheritance.
Similar content being viewed by others
Main
Since the first description of DBA as a congenital erythroblastopenia in the 1930s (1, 2), numerous cases of this disease have been reported; a comprehensive review covering >200 cases was published in 1988 (3). More recent reports have analyzed clinical data from either a single clinical center or national registries and have provided insights into clinical presentation, biologic features, and outcome of DBA (4–6). In the present study, we present the analysis of clinical data from a series of 229 DBA patients from France, Germany, and other European countries. All of these individuals had regular follow-up, and extensive biologic and clinical information was available for analysis of the progression of the disease and clinical outcome. In the present article, we highlight clinical presentation as well as long-term prognosis and response to the different treatment schedules. A vast majority of the severe complications encountered are of iatrogenic origin, related either to transfusion dependence or to long-term steroid therapy. Alternative treatments including BMT seem appropriate in this group of severely affected individuals.
Epidemiologic evaluation of DBA required a systematic and intensive search to identify all DBA patients born in France since 1983 and resulted in the identification of 72 patients who represent all or almost all French individuals with DBA born since this period. On the basis of this finding, we estimate the incidence of the disease to be 7.3 cases per million live births over the 13-y study period. No significant gender difference was noted in either presentation features or clinical outcome. Prevalence of malformations observed in our study is similar to that reported in previous studies. Importantly, our analysis suggests significant relationships between clinical manifestations, biologic features, familial history, and disease evolution.
METHODS
Registry.
The French DBA registry was initiated in 1984 by the DBA working group of the Société d'Hématologie et d'Immunologie Pédiatrique (SHIP). Since 1995, exhaustive coverage of pediatric French cases has been achieved through distribution of inclusion files to all French hematologists and pediatric departments. Annual notices were sent to collect new cases and follow-up data from previously registered patients. The French registry has been approved by the Commission Nationale Informatique et Libertés. Patients were recruited from 80 pediatric and/or hematology departments throughout France and its overseas territories. One hundred fifty-nine DBA cases were referred to the registry by medical groups from France, whereas eight others were referred by physicians from Belgium (seven patients) and Switzerland (one patient). Seventy German patients were added to the registry in 1998 through the DBA working group of the European Society for Pediatric Hematology and Immunology (ESPHI). Of the 237 patients initially referred for inclusion in the DBA registry, eight were excluded due to ambiguous or erroneous diagnoses (congenital dyserythropoiesis, two; transient erythroblastopenia of childhood, two; aplastic anemia, one; metabolic disease, one; dysmyelopoiesis, two). Thus, 229 DBA patients were finally available for detailed analysis.
A standardized questionnaire was used to collect data on each patient. It included information on birth history, physical examination, hematologic and biochemical data, response to therapeutic procedures, and a standardized clinical assessment of dysmorphic features based on a previously published range of malformations (3). Follow-up information was ascertained on the basis of annual patient clinical checkup and clinical records detailing growth parameters, CBC, all therapeutic procedures since the last evaluation, transfusion program, and treatment complications. Final analysis of the assembled data was performed in September, 1998. Descriptive statistics on clinical presentation, biologic features, evolution data, and prognosis factors were performed on the whole registry population, whereas epidemiologic analysis was restricted to the subgroup of patients born in France.
Diagnosis and presentation.
Diagnosis criteria included aregenerative anemia related to pure erythroblastopenia (≤5% of nucleated cells in the bone marrow are erythroblasts, without dysmorphic features) in an otherwise normal bone marrow. Chronic parvovirus B19 infection was ruled out by serology and/or PCR on blood and/or bone marrow and Fanconi's anemia by chromosome breakage study (7). These analyses were systematically performed before inclusion in the registry for all patients born since 1985; this information is being progressively updated when not available for older patients. Both diagnoses were thus ruled out in 47% of the registry population screened at the time of this analysis. All physical abnormalities were included in the database, enabling us to calculate the number of malformations per organ and the number of malformations for each individual (Table 1). Physical characteristics, when related to either premature birth or maturation delay or when frequently found in otherwise healthy individuals (i.e. foramen ovale persistence, hip dysplasia, testis migration defect), although recorded in the database, were excluded from the determination of the clinical phenotype and from calculations on prevalence of malformations associated with DBA. Weight and height at birth were compared with intrauterine growth charts according to gestational age (8, 9). Hypotrophy was defined as birth weight below the 10th percentile of body weight for gestational age and statural retardation as birth length below the 10th percentile of body length for gestational age.
Growth parameters at diagnosis or during evolution were transformed into SD from the mean [SD score or z score (10)] of the considered variable (body weight, body length, body mass index) according to mean and SD values for age and sex by using reference tables (11, 12). Association between malformations and descriptive variables at diagnosis was searched for by univariate analysis, and all parameters with a level of significance below 0.05 were included in a logistic regression model.
Disease evolution.
Hematologic outcome was assessed after completion of the first steroid course and at last follow-up. An intermediate evaluation of outcome was also used to describe variations in therapeutic response. Patients were classified into the following two groups:1) SR under long-term steroid therapy, making it possible to spare transfusions, and 2) TD patients who were steroid nonresponsive, had experienced a partial response to steroid therapy as previously described (7), or in whom steroid therapy had to be discontinued because of unacceptable side effects. Patients were considered free of treatment when persistently independent from both transfusion and steroid therapy for at least 6 mo. Because BMT dramatically transforms the course of the disease, the 13 patients who received allogenic bone marrow were not considered in the analysis of prognosis factors but consequently were analyzed separately.
Prognosis factors.
As long-term transfusion dependence has been shown to carry an unfavorable prognosis compared with long-term steroid sensitivity, variables in the outcome analysis included 1) outcome after first steroid course (responders versus nonresponders) and 2) a two-classes variable, “long-term prognosis.” Patients either free of treatment or persistently transfusion independent on steroid therapy at the last follow-up were considered the good prognosis group. The poor prognosis group included patients on a regular transfusion program at last follow-up or those who died after several years of transfusion dependence. Univariate association between these two outcome variables and potential explicative parameters included hypotrophy at birth, premature birth, diagnosis evoked before/after age 2, age at presentation, familial history of DBA, presence/absence of any malformation, presence/absence of malformations in each of the following categories: head, eye, neck, thumb, heart, bone, urogenital tract, miscellaneous. Other parameters at diagnosis included hypotrophy and statural delay (z score for, respectively, body weight and body length below/above −2 SD) and thrombocytopenia or thrombocytosis (platelet count below 150 × 109/L or above 450 × 109/L, respectively).
Epidemiology.
Incidence of DBA was calculated by comparing the number of DBA patients born in France between 1983 and 1995 with the total number of live births in France during the same period: 9 777 456 (INSEE, Paris, France). To analyze a possible effect of seasonality on DBA (5), the month of conception was calculated from birth date and term of pregnancy when available (n= 175). To search for a seasonality effect on potentially affected fetuses or maternal miscarriage, the distribution of month of birth of DBA patients was compared with monthly variations in the total number of births in France (INSEE, Paris, France). The observed number of cases for each month of the year was compared with the expected number of cases according to incidence of the disease and monthly rate of birth. Comparison was performed through χ2 analysis. Prevalence of malformations was calculated according to the month of birth and the month of conception. The same analysis was also performed on a 3-mo grouping basis according to all combinations of contiguous months.
Statistical analysis.
Descriptive statistics are presented as percentages and mean ± 1 SD. Crude and specific prevalence rates were calculated as the number of patients with the corresponding feature divided by the total number of patients in the relevant subgroup. The significance of observed differences was tested using the χ2 statistic and, when appropriate for small samples, the Fisher exact test on a bilateral formulation. Kruskal-Wallis H nonparametric test was used for comparison of age at diagnosis, as variance within groups seemed to be different. All p values were 2-sided, and a p value of 0.05 for univariate analysis was considered significant according to the large number of tests performed. A p value of 0.01 was chosen as significant for seasonality analysis, as multiple tests and grouping of data were used. To determine predictive factors for favorable outcome in the whole group or in the subgroup of steroid-resistant patients, multivariate logistic regression models were developed. The models included any variable with univariate relationship with a statistical test below 0.05 to this outcome variable. The results were reported as odds ratios (OR) with 95% confidence interval. Actuarial survival was calculated only for patients born after 1977, because patients included in the registry in adulthood can lead to a recruitment bias and cannot be considered representative of the whole adult DBA population. Survival was analyzed through the Kaplan-Meier technique on the whole group and on two separate groups according to the response to the first steroid course. The difference between steroid-responsiveness groups was assessed by log-rank test. Statistical analysis was performed using Epi-Info 6.04b (13) or Statistica 4.0 B (Statsoft, Inc.) software.
RESULTS
Diagnosis and presentation.
Among the 229 individuals in the registry, diagnosis of DBA could be established at birth in 30 cases (13.1%), before 1 y of age in 202 cases (88.2%), before 2 y of age in 217 patients (94.8%), and before 5 y of age in 226 patients (98.7%). Median age at presentation was 3 mo (Fig. 1). As diagnosis of DBA after the age of 2 is questionable (7), the 12 patients whose anemia was revealed late were specifically studied; one is a familial case from a dominant family in which DBA manifested in other individuals of the family before the age of 2, three are TD, and three others are long-term steroid dependent. After being weaned from both steroids and transfusions, the five remaining patients exhibit a persistent macrocytosis, with one individual also exhibiting a persistent increase in erythrocyte adenosine deaminase activity (eADA). Parvovirus B19 serology and PCR studies did not reveal a viral infection in any of these patients. Thus, biologic features and clinical outcome data are consistent with the diagnosis of DBA in these 12 cases with a delayed diagnosis.
The male:female ratio was not significantly different from 1 (1:1.1). Premature birth (before 37 wk of gestational age) occurred in 19.9% of cases, hypotrophy at birth was observed in 28.4% of the patients, and statural retardation in 22.1% of the patients. Birth weight was <2500 g in 26.5% of the patients. At least one malformation was observed in 93 patients (40.6%), whereas 54 patients were affected with two or more malformations (23.6%). Details on all malformations and prevalence for each group of malformations are shown in Table 1.
CBC was not available for all DBA patients at diagnosis or before the first transfusion. Macrocytosis based on mean corpuscular volume reference values for the appropriate age range was observed at presentation in 22% of the patients for whom the initial data were available but was present in 59.6% of 92 non-TD patients at last follow-up, a feature reported previously (4). Erythrocyte adenosine deaminase activity was found to be elevated in 28 of 34 non-TD patients, as previously described (14). At diagnosis, moderate neutropenia below 1.5 × 109/L was observed in 24.4% of cases, thrombocytopenia with platelet count below 150 × 109/L in 9.4%, and thrombocytosis with platelet count above 450 × 109/L in 41.2%. By univariate analysis, the presence of at least one malformation was significantly associated with two variables: short stature and absence of hypotrophy at diagnosis. We forced the existence of a familial history as a third variable in the regression model. A logistic regression model including these variables showed all three to remain significantly and independently associated with the presence of malformations (n= 118, r= 0.56). Presence of malformations is significantly and independently associated with familial history of DBA, short stature at diagnosis, and absence of hypotrophy at birth. Final stature was observed to be below −2 SD in 51.9% of the patients who reached adulthood.
Familial history.
Of the 229 patients in the registry, 195 were sporadic cases, whereas dominant mode of inheritance was observed for 34 patients from 16 families. Consanguinity was noticed in three pedigrees. Analysis of pedigrees of dominant families did not reveal any modification in sex ratio in affected or obligate carrier parents (male, six; female, five) compared with DBA cases (male, nine; female, 15). In dominant families, comparison of outcome between 23 DBA children and their 11 corresponding affected parents did not show any significant difference between generations. At last follow-up, seven children and seven affected parents were free of treatment; 11 children and four parents were steroid dependent. Although five children were still TD, whereas all parents had reached transfusion independence with age, outcome was not found to be different within generations (p= 0.16, Yates corrected χ2 test, df 1).
Disease evolution.
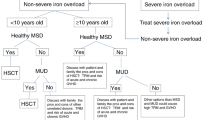
Two hundred twenty-two patients were available for long-term evaluation with a median follow-up of 111.5 mo and a total cumulative follow up of 2716 patient years. Figure 2 summarizes the evolution of the disease. Positive response to the first steroid treatment was obtained in 62.6% of the patients The response rate after the first steroid treatment was 64.7% with prednisone, 69.2% with prednisolone, and 75.5% with other steroids (p= 0.8), indicating that the type of steroid used for this first treatment did not influence the response rate. Steroid treatment had to be discontinued in 15.8% of the responders because of a progressive loss of response or severe side effects. Complications due to steroid therapy were noted in 19.7% of the patients under long-term therapy: osseous complications in 11 patients (5.6%), hypertension in three, diabetes mellitus in four, and growth retardation, presumably aggravated by steroid therapy, in 25 (13%). One infection-related death occurred in the group of SR, a 17-mo-old boy on long-term steroid therapy presenting with a silent peritonitis.
Among the 80 initial steroid nonresponders, eight (10%) could be weaned from transfusions during disease evolution, whereas four others were weaned from any treatment and 22 initially steroid-responsive patients became TD. Long-term follow-up showed a severe evolution in 40.5% of the patients: 65 patients (29.2%) required regular transfusion therapy, 13 (5.8%) required BMT, and 14 died (6.3%) (including two after BMT).
Complications due to transfusion therapy were observed in 69% of the long-term TD patients: iron overload despite regular subcutaneous desferrioxamine therapy occurred in 52 patients (62%), resulting in heart involvement in 12 patients (14.2%), liver dysfunction in 42 (50%), and endocrine deficiency in 21 (25%). Prevalence of hemochromatosis-related complication was significantly higher in TD DBA patients after age 10 compared with younger patients (71 versus 46%, p= 0.02), whereas no significant difference was noted among age-related groups when the cutoff point was set at age 15 (65 versus 54%, p= 0.3). Hepatitis C chronic infection was found in 6.6% of the transfused patients, all but one of whom was born before 1983. Three TD DBA patients were positive for both hepatitis C and HBsAg. Data on hepatitis B immunization were available for 178 patients. Immunization had been performed in only 59% of the TD patients (37.5% in non-TD patients). No significant difference in rate of immunization was observed among age groups (data not shown). No infection due to HIV was noted, nor any Creutzfeldt-Jacob disease. Transfusions and steroid treatment both could be discontinued in 46 of 222 patients (20.7%): 42 of 139 initially SR (30.2%) and four of 80 initially TD patients (5%), respectively. Among patients free of treatment, macrocytosis was observed in 33%, elevation of eADA in 80%, and increase in fetal Hb in 26%.
BMT was performed using HLA identical sibling donors (11 out of 13 patients), and donors were mismatched in two other patients. Overall results were satisfactory: survival, 84.6%; median follow-up, 36 mo (range, 3 to 138 mo) (Table 2). BMT-related deaths occurred in the two oldest patients at the time BMT was performed (15 y 11 mo and 18 y 4 mo, respectively).
Malignancies occurred in three patients, two of whom were TD: femoral osteosarcoma in a 12-y-old girl, Hodgkin's disease in a 23-y-old man, and breast cancer in a 26-y-old transfusion-independent female. Fatal outcome occurred in 15 DBA cases (median age, 17 y 5 mo; range, 1 y 1 mo to 53 y 9 mo) (Table 3). Underlying conditions causing death among 14 of these patients were hemochromatosis in five, severe pancytopenia related to secondary chronic bone marrow failure in three, infections in three, cancer in two (Hodgkin's disease, osteosarcoma), and noninfectious complications of BMT (severe graft versus host disease) in one. More than one cause of death was reported in some patients; for instance, iron overload complications were often associated with infectious complications. Overall survival at 250 mo of age (20.8 y) was 88.6 ± 3.7% (mean ± SD) (Fig. 3). Survival at 250 mo was significantly better among those who initially responded to steroids (95.4 ± 2.7%,) compared with nonresponders (84.6 ± 10.8%) (p= 0.01, log-rank test).
Prognostic factors.
Univariate analysis showed a significant association between absence of response to initial steroid course and four variables at diagnosis: young age at presentation, thrombocytosis above 450 × 109/L at diagnosis, absence of familial history, and presence of heart malformations. Logistic regression was performed with these variables included in the model. Three remained independently included in the model after logistic regression was performed (n= 163, r= 0.59) and were associated with absence of response to the first steroid course: young age at presentation, thrombocytosis at diagnosis, and absence of familial history. Similarly, six prognostic factors tested in univariate analysis against long-term outcome were significantly associated with unfavorable prognosis: neck malformations, thumb malformations, thrombocytosis at diagnosis, young age at presentation, premature birth, and absence of familial history. Among them, young age at presentation, absence of familial history, and premature birth remained the only independently associated variables with unfavorable outcome (n= 130, r= 0.84).
Epidemiology.
Among the 151 patients born in France or in overseas territories, 72 were born between January 1, 1983 and December 31, 1995. The annual incidence of DBA in France remained stable over this 13-y period with 7.3 new cases per million live births. No monthly variation of birth rate of DBA patients was observed in the whole population studied. A slight increase in prevalence of malformations was noted in children born at the end of the summer or in the fall (54.6% for the period September–November, p= 0.02; 50% for the period August–October, p= 0.04). However, these data did not reach the level of significance that was expected for this part of the study (p< 0.01). Further, this variation was not confirmed when the same data were analyzed on a monthly basis. Similarly, prevalence of DBA cases and malformations according to the month of conception did not show statistically any significant difference on a monthly or a 3-mo-period basis (data not shown).
DISCUSSION
The present study highlights the main features of the epidemiology and outcome of DBA through the analysis of a large well-characterized group of patients. Short-term prognosis is found to be dependent on steroid sensitiveness (62.6% of patients), whereas long-term prognosis is influenced by the morbidity encountered with transfusion programs (62% of TD patients) and mortality (18% of TD patients). Interestingly, long-term prognosis is statistically worse in sporadic cases compared with familial cases and in individuals with early onset of the disease, as previously reported (4). Analysis of our data enabled us to define the annual incidence of DBA in France to be 7.3 cases per million live births, without any effect of seasonality.
Presentation.
Our data show that short stature at presentation is significantly associated with malformative syndrome (5) and cannot be explained by other variables such as term of pregnancy or early onset of anemia. We were also able to confirm the variety of malformations and their frequency, as reported in earlier studies (3–5). The occurrence of malformative features among hematologically normal relatives of DBA patients remains a rare situation. Specifically, we observed three healthy relatives in a dominant DBA family who exhibited severe malformation of one hand and one of the two nonaffected children of a DBA mother who presented with Pierre Robin syndrome. Short stature at presentation (before any steroid therapy) seemed to be a true part of the malformative syndrome (4, 5) and raises the question whether or not short stature at adult age could be prevented. Postnatal onset of anemia observed in most of the DBA patients implies that erythropoiesis in utero is adequate in most cases for survival of the fetus. However, the prevalence of prematurity and intrauterine growth retardation is increased in DBA newborns compared with other newborns (19.9 versus 6% and 28.4 versus 10% in France, respectively, p< 0.0001). Malformations are not more frequently encountered in premature than in full-term birth DBA patients (46.8 versus 43.9%, respectively, p= 0.76) and thus do not seem to significantly contribute to premature birth in DBA. CBC was not always available at diagnosis or before transfusion, as initial data were often missing in the records of older patients and, in some patients, severe anemia at birth was followed by a prompt transfusion.
Disease evolution.
Our data also provided new insights into the therapeutic response and outcome in DBA patients. Initial steroid responsiveness is achieved in 61% of the cases. Long-term follow-up highlights time-related variations in response to treatments. Of the patients, 21.8% were finally weaned from any form of treatment. This group was composed mainly of SR (42 of 139, 30.2%) but also included rare individuals who were initially TD (four of 98, 4%). Thus, steroid response/resistance cannot be considered a definitive feature for a patient, as several patients experienced modifications in their status during long-term follow-up (13.5%). Specifically, 22 of 137 patients initially steroid sensitive became steroid resistant, whereas eight of 84 patients initially TD became SR. In some cases, response to steroid was achieved only after several steroid courses, suggesting that repeated steroid courses within the first decade of life should be considered in initially TD patients and are mandatory before major therapeutic decisions such as high-dose methyl prednisolone therapy, initiation of chelation, or BMT (15–20) are considered. Our study, however, does not provide data on the optimal number of steroid courses to perform in initially TD patients, as it was not previously considered a consensual treatment practice. Comprehension of such changes in therapeutic response would be a major step in understanding the pathophysiology of DBA. We also did not observe consistent loss of responsiveness to steroid therapy after interruption of the first course of steroid therapy (9.8% of initially SR and 17.8% of initially steroid-resistant patients changed status, respectively). These results do not support the hypothesis that an interruption of steroid therapy could be followed by a significant reduction in steroid response and favor the suggestion of transient discontinuation of steroid therapy and limited periods of transfusion support to promote catch-up periods for growth in steroid-responsive DBA patients with short stature. The clinical evolution we found in DBA patients after BMT emphasizes the overall good prognosis of this procedure as long as an HLA identical donor is available. The apparent discrepancy between outcome observed in the present study and that reported in the registry of the United States may be explained by the lower prevalence of HLA identical sibling donors (six out of 12 BMT) involved in the registry of the United States. In this earlier report, four out of five fatalities occurred in unrelated or mismatched transplants (6). Unfortunately, our data analysis has not been helpful in defining early and precisely the subset of patients who will remain TD and thus be potential candidates for early BMT. Deciding the optimal time for BMT in TD patients with an available sibling donor is a most distressing problem, as early BMT might be performed in patients who would still have a chance to reach transfusion independence, whereas, if BMT were performed later, transfusion-related complications might compromise the outcome. Yet HLA typing has to be performed during the first years of life in such situations, and cord blood of subsequent pregnancies should be systematically preserved (21).
No actuarial survival prediction can be made for the whole population of DBA patients from such a study design, and we proposed survival data for patients born since 1978. Janov et al. (4) carried out the first detailed study of a cohort of patients in a single clinical center and found a median survival of 31.2 y for patients born since 1960. Our data are consistent with this result, although most of the patients included in our study had not yet reached this age.
The major concern for TD DBA patients remains the complications related to this supportive therapy. Among our patients, 6.6% experienced blood-borne viral infections, and 63% exhibited iron overload-related complications despite regular chelation therapy, which was regularly performed in every TD patient. We did not observe any trend toward reduction in prevalence of iron overload complications among age groups, suggesting difference in compliance. Compliance to desferrioxamine therapy would need to be specifically assessed to further investigate this phenomenon. Importantly, immunization against hepatitis B should be more systematically performed in DBA, as all groups are potentially a population at risk for blood-borne infections.
Occurrence of malignancies in our series deserves further attention because other groups have reported an increased risk for malignancies in this condition (4, 22). The four patients reported by Janov et al. (4) exhibited acute myeloid leukemia after a prolonged period (15 to 30 y) and died between the ages of 24 and 43. Others have reported nonhematologic malignancies, as previously reviewed (22).
Epidemiology.
Early epidemiologic surveys of DBA were based on retrospective studies, leading to an underestimation of the incidence of this disorder [one case per million live births (23)]. Our data showing an incidence of 7.3 cases per million live births in France are in agreement with data from the United Kingdom (five per million), the Netherlands (four per million) (24), and Scandinavian countries [10 per million (L. Wranne, personal communication)]. Although the data on incidence can be considered reliable, disease prevalence data are certainly underestimated because most steroid and transfusion-independent adult patients are lost to follow up after childhood. Inclusion of patients older than 20 y in databases relies usually on new contacts of these individuals with a hematology or internal medicine group because of relapse of anemia, genetic counseling, pregnancy, the birth of an affected child, the occurrence of a malignancy, or through the family associations. Our data do not support the hypothesis of a seasonal factor previously suggested by Ball et al. (5). Indeed, we did not find any significant seasonal variation in incidence of DBA or any significant prevalence of dysmorphic features according to birth or conception date. The moderate increase in prevalence of malformations at the end of the summer or during the fall can be considered nonsignificant due to the large number of statistical tests performed. No gender difference was observed in phenotypic expression of the disease, and evaluation of familial cases did not suggest the existence of an effect of parental imprinting or any anticipation phenomenon in dominant cases.
The present study as well as a number of earlier studies implies that DBA is a heterogeneous clinical condition with regard to existence of malformations, sporadic cases or familial history, and response to steroid therapy. The novelty of our study is that we have been able to document these diverse features as statistically linked, giving strong support to the hypothesis that a common underlying genetic defect or mechanism could explain most of the variations in phenotypic expression of the disorder. To establish the diagnosis of DBA, Fanconi's anemia and parvovirus B19 must be ruled out, as therapeutic options differ (7). Steroid response/resistance does not seem to be a permanent feature in DBA patients, as 13.5% of DBA patients experience modifications in their status. Further, the occurrence of complication during steroid treatment or the existence of a threshold above 0.5 mg·kg−1·d−1 often requires a long-term transfusion program. Repeated attempts of steroid treatment, however, are useful, as they may reveal an improved steroid sensitiveness. Further studies on growth will be needed, as it seemed that growth failure related to steroid treatment requires a short-term transfusion program in some cases to allow for catch-up growth. The prognosis encountered by TD patients remains impaired by complications of iron overload and blood-borne infections. BMT has proven to be an effective treatment option when an intrafamilial genoidentical donor is available. Until results of further therapeutic trials are available, the prognosis for steroid-resistant patients will remain a significant concern. Recent research on genes underlying DBA may help in understanding the phenotypic variations of the disease as well as the mechanism(s) of steroid sensitiveness and, thus, lead to better treatment planning for DBA patients (25–27). At the time this study was completed, identification of mutations in a gene encoding the ribosomal protein S19 had opened interesting fields for research in understanding these features and, hopefully, therapeutic management (28). Genotypic analysis of the patients in the present study may explain some of the prognostic factors that we report here.
Abbreviations
- DBA:
-
Diamond-Blackfan anemia
- BMT:
-
bone marrow transplantation
- CBC:
-
complete blood count
- TD:
-
transfusion dependent
- SR:
-
steroid responder
References
Diamond LK, Blackfan KD 1938 Hypoplastic anemia. Am J Dis Child 56: 464–467
Josephs HW 1936 Anaemia of infancy and early childhood. Medicine 15: 307–451
Alter BP 1980 Childhood red cell aplasia. Am J Pediatr Hematol Oncol 2: 121–139
Janov AJ, Leong T, Nathan DG, Guinan EC 1996 Diamond-Blackfan anemia. Medicine 75: 77–87
Ball SE, McGuckin CP, Jenkins G, Gordon-Smith EC 1996 Diamond-Blackfan anaemia in the U. Br J Haematol 94: 645–653
Vlachos A, Boonyasai R, Abramson J, Samedi J, Alter BP, Buchanan GR, Freedman MH, Glader BE, Lipton JM 1997 Data from the Diamond-Blackfan anemia registry (DBAR) suggests a reevaluation of current treatment practices. Blood 90: 440a
Willig TN, Ball S, Tchernia G 1998 Current concepts and issues in Diamond-Blackfan anemia. Curr Opin Hematol 2: 109–115
Leroy B, Lefort F 1971 A propos du poids et de la taille des nouveau nés à la naissance. Rev Fr Gynécol 66: 391–396
Lubchenco LO, Hansman C, Dressler M, Boyd E 1963 Intrauterine growth as estimated from live-born birth-weight data at 24 to 42 wk of gestation. Pediatrics 32: 793–800
Waterlow JC, Buzina R, Keller W, Lane JM, Nichaman MZ, Tanner JM 1977 The presentation and use of height and weight data for comparing the nutritional status of groups of children under the age of 10 years. Bull World Health Organ 55: 489–498
Sempé M, Pédron G, Roy-Pernot MP 1979 Auxologie Méthodes et Séquences. Theraplix Eds, Paris, pp 30–57
Rolland-Cachera MF, Cole T, Sempé M, Tichet J, Rossignol C, Charraud A 1991 Body mass index variations: centiles from birth to 87 years. Eur J Clin Nutr 45: 13–21
Dean AG, Dean JA, Coulombier D, Brendel KA, Smith DC, Burton AH, Dicker RC, Sullivan K, Fagan RF, Arner TG 1995 Epi Info, Version 6: a Word Processing, Database, and Statistics Program for Public Health on IBM-Compatible Microcomputers. Centers for Disease Control and Prevention, Atlanta, GA, pp 97–108
Willig TN, Pérignon JL, Gustavsson P, Gane P, Draptchinskaya N, Testard H, Girot R, Debré M, Stéphan JL, Chenel C, Cartron JP, Dahl N, Tchernia G, on behalf of the DBA working group of Société d'Hématologie et d'Immunologie Pédiatrique SHIP 1998 High adenosine deaminase level among healthy probands of Diamond Blackfan anemia (DBA) cosegregates with the DBA gene region on chromosome 19q13. Blood 92: 4422–4427
Ozsoylu S 1984 High-dose intravenous corticosteroid for a patient with Diamond-Blackfan syndrome refractory to classical prednisone treatment. Acta Haematol 71: 207–210
Bernini JC, Carillo JM, Buchanan GR 1995 High-dose intravenous methylprednisolone therapy for patients with Diamond-Blackfan anemia refractory to conventional doses of prednisone. J Pediatr 127: 654–659
August CS, King E, Githens JH, McIntosh K, Humbert JR, Greensheer A, Johnson FB 1976 Establishment of erythropoiesis following bone marrow transplantation in a patient with congenital hypoplastic anemia (Diamond-Blackfan syndrome). Blood 48: 491–498
Iriondo A, Garijo J, Baro J, Conde E, Pastor JM, Sabanes A, Hermosa V, Sainz MC, Perez de la Lastra L, Zubizarreta A 1984 Complete recovery of hemopoiesis following bone marrow transplant in a patient with unresponsive congenital hypoplastic anemia (Blackfan-Diamond syndrome). Blood 64: 348–351
Wiktor-Jedrzejczak W, Szczylik C, Pojda Z, Siekierzynski M, Kansy J, Klos M, Ratajczak MZ, Pejcz J, Jaskulski D, Gornas P 1987 Success of bone marrow transplantation in congenital Diamond-Blackfan anaemia: a case report. Eur J Haematol 38: 204–206
Mugishima H, Gale RP, Rowlings PA, Horowitz MM, Marmont AM, McCann SR, Sobocinski KA, Bortin MM 1995 Bone marrow transplantation for Diamond-Blackfan anemia. Bone Marrow Transplant 15: 55–58
Bonno M, Azuma E, Nakano T, Higashikawa M, Kawasaki H, Nishihara H, Obata M, Nagai M, Sakatoku H, Komada Y, Ito M, Sakurai M 1995 Successful hematopoietic reconstitution by transplantation with umbilical cord blood cells in a patient with Diamond-Blackfan anemia. Blood 86: 938a
van Dijken PJ, Verwijs W 1995 Diamond-Blackfan anemia and malignancy. Cancer 76: 517–520
Kynaston JA, West NC, Reid MM 1993 A regional experience of red cell aplasia. Eur J Pediatr 152: 306–308
Bresters D, Bruin MCA, Van Dijken PJ 1991 Congenitale hypoplastische anemie in Nederland 1963–1989. Tijdschr Kindergeneeskd 59: 203–210
Gustavsson P, Willig TN, van Haeringen A, Tchernia G, Dianzani I, Donner M, Elinder G, Henter JI, Nilsson PG, Gordon L, Skeppner G, van't Veer-Korthof L, Kreuger A, Dahl N 1997 Diamond-Blackfan anemia: genetic homogeneity for a gene on chromosome 19q13 restricted to 1:8 Mb. Nat Genet 16: 368–371
Gustavsson P, Garelli E, Draptchinskaia N, Ball S, Willig TN, Tentler D, Punnet H, Schafer F, Cario H, Ramenghi U, Dianziani I, Glomstein A, Pfeiffer RA, Goringe A, Olivieri N, Cotton ES, Tchernia G, Elinder G, Dahl N 1998 Identification of microdeletions spanning the major locus on 19q13 in Diamond-Blackfan anemia and evidence for at least two DBA genes. Am J Hum Genet 63: 1388–1395
Gazda H, Lipton JM, Niemeyer CM, Vlachos A, Rokicka-Milewska R, Ohara A, Ploszynska A, Webber A, Nathan DG, Beggs AH, Sieff CA 1998 Diamond-Blackfan anemia is genetically heterogeneous. Blood 92: 16b
Draptchinskaia N, Gustavsson P, Andersson B, Pettersson M, Willig TN, Dianzani I, Ball S, Tchernia G, Klar J, Mattsson H, Tentler D, Carlsson B, Narla M, Dahl N 1999 The ribosomal protein S19 gene is mutated in Diamond-Blackfan anemia. Nat Genet 21: 169–175
Acknowledgements
The authors acknowledge the DBA working groups of the European Society for Pediatric Hematology and Immunology (ESPHI) and of the Société d'Hématologie et d'Immunologie Pédiatrique (SHIP). We thank Drs. Philippe Gascard and Joel Chasis (LBNL) for their careful help in improving this manuscript. We also thank Dr. Mark Durst (LBNL) for his kind help in reviewing statistical procedures and methodology.
Author information
Authors and Affiliations
Consortia
Additional information
Supported in part by Association Française contre les Myopathies (A.F.M.), Généthon, Direction de la Recherche Clinique (DRC) (grant CRC 950183), Assistance Publique-Hôpitaux de Paris, the Deutsche Forshungsgemeinschaft (SFB).
Preliminary results appeared as an interim analysis during the European Hematology Association Congress, Paris, May 31–June 1, 1996, and the American Society of Hematology, Orlando, Florida, December 6–10, 1996.
APPENDIX
APPENDIX
Participating clinical investigators from France.
A. Babin Boilletot (Strasbourg), C. Bachelot (Grenoble), A. Barruchel (Paris), Berets (Clamart), J. Bernard (Paris), F. Bernaudin (Créteil), Y. Bertrand (Lyon), S. Blanche (Paris), J.F. Boccara (Paris), P. Bordigoni (Nancy), Ph. Bourgeois (Evreux), J.M. Cazauran (Périgueux), C. Chenel (Papeete), B. Coiffier (Lyon), G. Couillault (Dijon), G. Daltroff (Belfort), M. Damay (Le Mans), M. Debre (Paris), F. Deméocq (Clermont-Ferrand), L. De Parscau, R. Despax (Toulouse), A. Deville (Nice), H. Dombret (Paris), J.P. Dommergues (Le Kremlin-Bicêtre), J. Donadieu (Paris), V. Dorvaux (Metz), F. Dreyfus (Paris), C. Edan (Rennes), C. Fagnou (Boulogne Billancourt), M.J. Gaonach (Le Chesnay), Ph. Gestas (Papeete), J.Y. Genot (Caen), R. Girot (Paris), E. Gluckman (Paris), R. Goddon (Montluçon), J.M. Guillard (Bordeaux), M. Guillot (Lisieux), F. Klein (Metz), Z. Klink (Thionville), P. Labrune (Clamart), C. Lajarrige (Laon), J.P. Lamagnere (Tours), A. Lambiliotte (Lille), T. Leblanc (Paris), J.M. Le Fur (Brest), O. Lejars (Tours), Cl. Lejeune (Colombes), G. Leverger (Paris), L. de Lumley (Limoges), G. Margueritte (Montpellier), F. Mechinaud (Nantes), J.L. Mesnil (Flers), M. Micheau (Bordeaux), G. Michel (Marseille), M.J. Milleret Proyart (Sens), M. de Montalembert (Paris), M. Monconduit (Rouen), M. Munzer (Reims), C. Narcy (Saint Germain en Laye), B. Nelken (Lille), H. Orfeuvre (Bourg en Bresse), B. Pautard (Amiens), P.Y. Péaud (Valence), Y. Perel (Bordeaux), H. Perrimond (Marseille), N. Philippe (Lyon), E. Praud (Le Mans), M.P. Pignol (Mont de Marsan), H. Piguet (Rouen), M. Pilliot (Wattrelos), A. Plou (Nantes), E. Plouvier (Besançon), G. Pointecouteau (Angoulême), C. Rey (Le Kremlin-Bicêtre), P. Richard (Angoulême), A. Robert (Toulouse), Cl. Roy (Paris), D. Quillerou (Troyes), G. Souillet (Lyon), H. Testard (Saint Denis de la Réunion), C. Saint-Aimé (Fort de France), B. Salles (Chalon sur Saône), P.J. Sanyas (La Rochelle), G. Schaison (Paris), D. Stamm (Lyon), J.L. Stéphan (Saint Priez en Jarrez), G. Tchernia (Le Kremlin-Bicêtre), Ph. Tron (Rouen), C. Vervel (Compiègne), J.P. Vannier (Rouen), W. Vainchenker (Villejuif), E. Vilmer (Paris), T.N. Willig (Le Kremlin-Bicêtre, Berkeley).
Participating clinical investigators from Germany.
C. Bender-Götze (München), F. Berthold (Köln), U. Bertram (Hanau), R. Blütters-Sawatzki (Giessen), J. Budde (Freiburg), H. Cario (Ulm), B. Dorn (Wuppertal), S. Eber (Göttingen), W. Eberl (Braunschweig), A.K. Gnekow (Augsburg), N. Graf (Homburg), U. Graubner (München), R.J. Haas (München), E. Harms (Münster), G. Henze (Berlin), G. Janka-Schaub (Hamburg), A. Jopke (Nürnberg), N. Jorch (Bielefeld), T. Klingebiel (Tübingen), E. Kohne (Ulm), D. Körholz (Düsseldorf), H.J. Laws (Düsseldorf), R. Mertens (Aachen), S. Müller-Weihrich (München), C. Niekrenz (Delmenhorst), C. Niemeyer (Freiburg), M. Rister (Koblentz), J. Ritter (Münster), W. Scheuerlen (Würzburg), B. Stollman-Gibbels (Essen), K.W. Sykora (Hannover), C. Tiemann (Freiburg), R. Tratzmüller (Augsburg), N. Veelken (Hamburg), H. Wehinger (Kassel), G. Weissbach (Dresden), T. Wiesel (Datteln), F. Zintl (Jena).
Contributors from other countries.
G. Cornu (Bruxelles), J. Otten (Bruxelles), J. Humbert (Genève).
Participating laboratories.
J.P. Cartron (Paris), L. Croisille (Le Kremlin-Bicêtre), L. Coulombel (Villejuif), P. Gane (Paris), J.L. Pérignon (Paris), P.H. Roméo (Créteil).
Rights and permissions
About this article
Cite this article
Willig, TN., Niemeyer, C., Leblanc, T. et al. Identification of New Prognosis Factors from the Clinical and Epidemiologic Analysis of a Registry of 229 Diamond-Blackfan Anemia Patients. Pediatr Res 46, 553 (1999). https://doi.org/10.1203/00006450-199911000-00011
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199911000-00011
This article is cited by
-
Clinical features, mutations and treatment of 104 patients of Diamond-Blackfan anemia in China: a single-center retrospective study
International Journal of Hematology (2016)
-
Disruption of the 5S RNP–Mdm2 interaction significantly improves the erythroid defect in a mouse model for Diamond-Blackfan anemia
Leukemia (2015)
-
PPAR-α and glucocorticoid receptor synergize to promote erythroid progenitor self-renewal
Nature (2015)
-
Ribosomal protein mutations in Korean patients with Diamond-Blackfan anemia
Experimental & Molecular Medicine (2014)
-
VarRanker: rapid prioritization of sequence variations associated with human disease
BMC Bioinformatics (2013)