Abstract
The renal effects of acute hypoxemia and the ability of perindoprilat, a potent angiotensin-converting enzyme inhibitor, to prevent these effects were assessed in 31 anesthesized and mechanically ventilated newborn (5 to 8 d of age) rabbits. Renal blood flow (RBF) and GFR were determined by the clearances of para-aminohippuric acid and inulin, respectively. Each animal acted as its own control. In eight normoxemic rabbits (group 1), the i.v. infusion of saline did not change renal and hemodynamic functions. In eight additional rabbits, acute hypoxemia (Pao2 = 40 mm Hg) induced a significant decrease in mean blood pressure (-8 ± 2%), RBF (-36 ± 3%), and GFR (-31 ± 3%) and an increase in renal vascular resistance (+50 ± 12%). A third group of newborn animals (n = 7) was used to determine the renal effects of perindoprilat administration (20 µg/kg) under normoxemic conditions. RBF significantly increased (+15 ± 2%) and renal vascular resistance significantly decreased (-15 ± 3%), whereas GFR, mean blood pressure, and filtration fraction did not change significantly. In group 4 (n = 7), perindoprilat infusion completely prevented the hypoxemia-induced alterations in GFR and renal vascular resistance and partially prevented the fall in RBF. These results demonstrate that angiotensin II modulates the renal immature microcirculation and that inhibition of its formation effectively prevents the hypoxemia-induced decrease in GFR.
Similar content being viewed by others
Main
In animal models as well as in humans, acute hypoxemia can lead to a state of renal insufficiency(1,2). In the newborn rabbit, renal maturation shows close similarity with that of premature infants(2,3). In this model, acute normocapnic hypoxemia increases the RVR, leading to renal hypoperfusion, and decreases GFR(2–4). The underlying mechanisms of this hypoxemia-induced vasomotor nephropathy are still controversial. The chemoreceptor-mediated reflex and/or the activation of vasoactive factors such as adenosine(4) and nitric oxide(5) have been suggested to play a role. A II has also been implicated in the hypoxemia-induced renal changes, but its role has not yet been clearly demonstrated.
The RAS is known to play an important role in the regulation of systemic arterial pressure, RBF, single nephron GFR, and intrarenal distribution of blood flow in adult as well as immature animals(6). During the neonatal period, the activation of the RAS has been shown to contribute mainly to the hemodynamic adjustments after delivery(7).
Several lines of evidence suggest that A II could be involved in the pathogenesis of the hypoxemia-induced renal vasoconstriction. The hypoxemia-induced changes in renal hemodynamics are very similar to those induced by the intrarenal injection of A II(8). Moreover, hypoxemia and ischemia have been shown to stimulate renin release in adults(9), newborn infants(10), newborn lambs(11), and piglets(12).
The aim of the present study was to define the putative protective effects of perindoprilat, an ACEI, in anesthetized and mechanically ventilated newborn rabbits exposed to normocapnic hypoxemia. Perindoprilat is one of the most potent ACEI presently available(13). It has also been shown to inhibit the degradation of the vasodilator peptide bradykinin(14). If a II activation and/or bradykinin degradation are involved in the pathogenesis of the hypoxemia-induced renal vasoconstriction, perindoprilat administration should prevent or at least blunt the effect of hypoxemia.
METHODS
Experiments were performed in 31 newborn New Zealand White rabbits, 5 to 8 d old, weighing 90 to 174 g. The animals were born by spontaneous vaginal delivery and afterward housed with the maternal rabbit and breast fed. These studies were performed in accordance with the guidelines of the Swiss National Research Foundation.
Experimental Procedures
All Methods have previously been described(4,15). Briefly, the animals were initially anesthetized with sodium pentobarbital (25 mg·kg-1 administered intraperitoneally), supplemented with small doses administered i.v., as required. The trachea was cannulated to allow mechanical ventilation with a mixture of air and oxygen (rodent ventilator, model 683; Harvard, Millis, MA). The femoral vein and artery were catheterized for arterial blood sampling, monitoring of systemic arterial blood pressure (Statham P23 ID pressure transducer recorded on a Grass Polygraph, model 7B, Quincy, MA), and solute and drug infusion; the urinary bladder was catheterized for the collection of urine. Body temperature was maintained at approximately 39°C by an infrared lamp and a heated operating table and was continuously monitored by an intraesophageal thermometer (digital thermometer, Poliak and Gramiger, EPFL, Lausanne, Switzerland). After completion of the surgical procedure, an i.v. priming dose of inulin (80 mg·kg-1) and PAH (1.25 mg·kg-1) was administered and was followed by a continuous infusion to maintain constant plasma inulin and PAH concentrations. Throughout the experiment, an infusate containing 100 mM NaCl, 50 mM NaHCO3, 5 mM KCl, 50 g of mannitol, 3 g of inulin, and 150 mg of PAH per liter was administered. The infusion rate was maintained at 1 mL·h-1·100 g-1 body weight with a constant infusion pump (Perfusor EDL 2, Braun, Melsungen, Germany). Approximately 45 min were spent for animal preparation and 90 min were allowed for subsequent equilibration.
Experimental Protocol
After the equilibration period, the experimental protocol started with a control period (period 1) of 60 min in each group. The remainder of the protocol differed among the four experimental groups (Fig. 1).
Group 1 (control, n = 8; age = 6.4 ± 0.3 d; weight = 135 ± 9 g). The animals were infused throughout the experimental 60-min period (period 2) with the solution described above (1 mL·h-1·100 g-1) and were ventilated under normoxemic conditions. This group was used to evaluate the stability of this model.
Group 2 (hypoxemia, n = 8; age = 6.2 ± 0.3 d; weight = 130 ± 5 g). Fifteen minutes after the end of period 1, hypoxemia was induced (within 45 min) by slowly reducing the fractional inspiratory oxygen concentration with a gas mixture of 10% O2 and 90% N2, maintained throughout the experiment. Renal hemodynamics and blood pressure were assessed during one 60-min period (period 2). This animal group was used to determine the systemic and renal effects of hypoxemia.
Group 3 (perindoprilat, n = 7; age = 5.9 ± 0.4 d; weight = 135 ± 8 g). At the end of period 1, the animals received an i.v. bolus of 20 µg·kg-1 of perindoprilat (Laboratoire Servier, Gidy, France). Renal function and blood pressure were assessed during a 60-min period, which started 1 h after perindoprilat infusion (period 2). This delay after perindoprilat injection was chosen to allow comparison with the other groups. The dose of 20 µg/kg of perindoprilat was considered efficient enough to inhibit A II formation because this dose has been shown to result in an 82.8 ± 4.7% inhibition of the angiotensin I-induced increase in MBP, 1 h after its injection(15).
Group 4 (perindoprilat + hypoxemia, n = 8; age = 6.5 ± 0.4 d; weight = 127 ± 7 g). The animals of this group received the same dose of perindoprilat as that administered to the animals in group 3. Fifteen minutes later, hypoxemia was induced as described above. Measurements were performed during continuous hypoxemia (period 2). This group was used to assess the putative effect of perindoprilat in hypoxemia-induced renal dysfunction.
Each animal acted as its own control. For period 1, two timed urinary collections of 30 min each were obtained with blood sampling (0.4 mL) at midpoint. The results of both 30-min collection periods were averaged. For period 2, blood was sampled at the midpoint of a 60-min urine collection period. Eighty microliters of whole blood were used for blood gases, hematocrit, and protein determinations. The remaining blood was centrifuged, and the red blood cells were reconstituted in 0.4 mL of human albumin and returned to the animal. The plasma and urine samples were kept at -20°C for subsequent analysis of inulin and PAH. At the end of the experiments, the rabbits were given a lethal i.v. dose of pentobarbital.
Analytical Procedures
Urine volume was measured from the change in weight of preweighed tubes, without correction for specific gravity. Arterial blood for pH, Paco2, Pao2, hematocrit, and protein levels was collected anaerobically in heparinized capillary tubes. Blood gas determination was performed with a pH/blood gas analyzer (Gas Analyser 168, Corning, Essex, England). The automatic anthrone(16) and the Bratton and Marshall(17) methods were used for the determination of inulin and PAH concentrations, respectively (Autoanalyser II, Technicon Instrument Corporation, Tarrytown, NY). We estimated plasma protein concentration from the plasma index of refraction, with a temperature-compensated refractometer (AOTS meter, American Optical, Buffalo, NY).
Data Analysis. The renal clearances of inulin (CIn) and PAH (CPAH) were calculated from standard equations and used as indices of GFR and RPF, respectively. A renal PAH extraction ratio (EPAH) of 0.55, as previously determined in our laboratory(2), was used to calculate RBF. In a recent study in adult rabbits, perindoprilat administration did not significantly modify the EPAH(18). RBF, RVR, and FF were calculated from the following equations (where Hct = hematocrit): RBF(ml·kg-1·min-1) = CPAH/[EPAH × (1 - Hct)], RVR(mm Hg·ml-1·kg·min) = MBP/RBF FF(%) = (GFR/RPF) × 100
The data obtained from the two control periods were averaged. The effects of the modified Ringer solution alone (group 1), hypoxemia (group 2), perindoprilat (group 3), and perindoprilat + hypoxemia (group 4) on systemic and renal hemodynamics were analyzed by the Wilcoxon signed-rank test. Comparisons between the control and experimental periods in all groups of animals were performed by the Kruskal-Wallis test. p values <0.05 were considered statistically significant. All data were expressed as means ± SEM.
RESULTS
Postnatal age, body weight, pH, Pao2, Paco2, protein plasma levels, hematocrit, MBP, and renal function during the control period were not statistically different among the four groups of newborn rabbits (text and Tables 1 and 2). Blood pH, Pao2, and Paco2 did not vary significantly throughout the study in groups 1 and 3, whereas, as expected, Pao2 fell from 126 ± 4 to 43 ± 1 mm Hg and from 128 ± 4 to 41 ± 1 mm Hg in groups 2 and 4, respectively (both p < 0.01). As a consequence of repeated blood sampling, the hematocrit decreased slightly, albeit significantly in groups 2 and 4. The plasma levels of protein decreased slightly in group 2 (Table 1). The absolute values observed for the renal parameters in the control and experimental periods in the four groups are shown in Table 2.
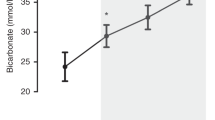
In control normoxemic animals (group 1), the infusion of the standard solution at a rate of 1 mL·h-1·100 g-1 body weight did not induce significant changes in systemic and renal hemodynamics. In group 2, acute hypoxemia was associated with a significant decrease in MBP (-8 ± 2%). Urine flow rate, RBF, and GFR decreased significantly (-21 ± 9%, -36 ± 3%, and -31 ± 3%, respectively). RVR increased dramatically (+50 ± 12%), whereas FF was not significantly affected by hypoxemia. In group 3, the administration of perindoprilat in normoxemic and normocapnic conditions did not significantly modify MBP (Fig. 2). A slight but significant increase in urine flow rate and RBF was observed (+10 ± 0.5% and +15 ± 2%, respectively). RVR significantly decreased (-15.1 ± 3%). GFR and FF were not significantly affected by the administration of perindoprilat.
In perindoprilat-pretreated rabbits (group 4), acute normocapnic hypoxemia induced a slight but significant decrease in MBP and RBF decreased significantly (-8 ± 1% and -12.6 ± 3%, respectively) whereas urine flow rate, GFR, and RVR did not change. FF significantly increased by 13 ± 2%.
When comparing the data of group 4 with those of group 2, the percent changes in RBF, GFR, and RVR were significantly different (p < 0.05). Figure 3 shows the protective effects of perindoprilat on renal functions during hypoxemia.
Comparison of the changes in renal hemodynamics in newborn rabbits with hypoxemia (group 2, white bars) and animals that were pretreated with perindoprilat before hypoxemia was induced (group 4, black bars). The values are expressed in percent changes for each group as compared with the control period. Values are means ± SEM; * = p < 0.05 and ** = p < 0.01 when compared with the control period, and † = p < 0.05 and ‡ = p < 0.01 when compared with group 2. V, urine flow rate.
DISCUSSION
This study was performed to define the putative protective effects of perindoprilat, an ACEI, on the renal functional changes induced by hypoxemia in newborn rabbits. The role of RAS in modulating cardiovascular and renal hemodynamics during pre- and perinatal life has been well documented(19). The RAS seems to play an important role in regulating blood pressure in fetal life(20). The kidneys of fetal and newborn experimental animals are known to synthesize and secrete renin in abundance(6). It has been suggested that the RAS, through a local mechanism, is partially responsible for the vasoconstriction of renal vessels at this age. Systemic administration of A II in fetal lambs decreases RBF without changes in GFR. This suggests that A II acts primarily by increasing the efferent arterial tone and, to a lesser degree, leads to contraction of the glomerular mesangium(21). In fact, the renal vascular response to exogenous administration of A II is lower in fetal lambs than in adult sheep, suggesting that others factors (i.e. α adrenergic tone) could contribute to local vascular resistance in this model(21) or that renal vasoconstriction is already maximal.
Although A II has been shown to be an important vasoconstrictor in the developing renal vasculature, experimental studies with the systemic administration of the A II antagonist saralasin(22) or ACEI [captopril(20,23–25) or enalapril(26)] have shown a variety of responses. Thus, no conclusive specific vasoactive role for A II in the developing kidney has been defined. The conflicting results can probably be explained by the lack of specificity of these drugs and/or the variability of the models in term of species, age, or stage of fetal renal maturation and/or the variability of glomerular A II receptor subtype expression and localization during kidney development(27). However, in recent studies, the intrarenal infusion of an angiotensin receptor antagonist(28) produced a marked increase in RBF in the developing piglet, without affecting GFR. Our results in the animals of group 3, which received only ACEI, support these observations. The administration of perindoprilat to normoxemic newborn rabbits was followed by a significant increase in RBF without any change in GFR. This suggests both afferent and efferent arteriolar vasodilation, as a result of the inhibition of A II formation. The renal vascular action of perindoprilat could in theory also be mediated by bradykinin. Indeed, ACEI also inhibit the degradation of bradykinin into inactive fragments, but previous studies in our laboratory failed to demonstrate a role of bradykinin in the perindoprilat-induced renal changes(15).
As previously described(2–4), acute normocapnic hypoxemia produced a significant fall in RBF and GFR in newborn rabbits (group 2). This occurred concomittantly with a significant increase in RVR, whereas FF remained unchanged. These results suggest both pre- and postglomerular vasoconstriction and are in agreement with previous studies demonstrating that hypoxemic conditions are associated with renal vasoconstriction in a variety of neonatal animal species, such as lambs(11), puppies(29), and rabbits(2,3). These hypoxemia-induced changes in renal hemodynamics are very similar to those induced by intrarenal injection of A II(8). In immature animal models, the plasma renin activity has been shown to rise dramatically as a result of hypoxemia(30). Furthermore, in isolated perfused kidneys, infusion of A II augments medullary hypoxic damages by decreasing RBF and increasing FF(31).
When A II formation was markedly inhibited by perindoprilat (animals of group 4), acute hypoxemia did not alter GFR and the increase in RVR was completely prevented (Fig. 3). The decrease in RBF was significantly blunted. The FF increased slightly, possibly as a result of an increase in the ultrafiltration coefficient. We suggest that perindoprilat prevented the hypoxemia-induced renal dysfunction mainly by the inhibition of the A II-mediated preglomerular vasoconstriction. Alternatively, the maintenance of GFR in rabbits that received perindoprilat could also be due to the accumulation of bradykinin(32) or the local effects of nitric oxide(5,28) or adenosine. Renal adenosine, which is stimulated in hypoxic states, causes predominantly vasodilation of the efferent arteriole(4) but also vasoconstricts the afferent arteriole when the RAS is activated(33). Inhibition of the A II-mediated vasoconstriction could thus give adenosine the opportunity to freely express its vascular action, resulting in an increase in RBF in comparison with untreated hypoxemic rabbits. The potential role of bradykinin accumulation in hypoxemic newborn rabbits pretreated by an ACEI remains to be investigated.
The use of ACEI has been shown to induce deleterious effects in the human fetus. A potential fetal side effect of captopril administration to pregnant women was first reported by Guignard et al.(34) in 1981. The authors described the occurrence of a persistent anuria in a premature neonate born from a mother who received captopril from the 26th to the 29th wk of gestation. Since that report, several cases of anuria or impaired renal function in infants born from mothers who had been given either captopril or enalapril during pregnancy have been reported(35). Because of their potential risk for fetal renal function, as well as other risks (oligoamnios and ossification abnormalities), ACEI are contraindicated during pregnancy. The present study suggests that the postnatal activation of the renin-angiotensin system by hypoxemia can impair renal perfusion and lead to renal insufficiency.
In summary, the present results in newborn rabbits confirm the following: 1) the physiologic role of A II in modulating the renal microcirculation in newborn rabbits, 2) the deleterious renal effect of acute hypoxemia, and 3) the ability of ACEI to prevent the hypoxemia-induced renal changes.
Abbreviations
- RVR:
-
renal vascular resistance
- A II:
-
angiotensin II
- RAS:
-
renin-angiotensin system
- RBF:
-
renal blood flow
- ACEI:
-
angiotensin-converting enzyme inhibitor
- PAH:
-
para-aminohippuric acid
- MBP:
-
mean blood pressure
- RPF:
-
renal plasma flow
- FF:
-
filtration fraction
References
Guignard J-P, Torrado A, Mazouni SM, Gautier E 1976 Renal function in respiratory distress syndrome. J Pediatr 88: 845–850.
Gouyon J-B, Vallotton M, Guignard J-P 1987 The newborn rabbit: a model for studying hypoxemia-induced renal changes. Biol Neonate 52: 115–120.
Vallotton M 1984 Maturation de la fonction rénale chez le lapin nouveau-né: effet de l'hypoxlémie. Thesis Lausanne University Medical School, Switzerland, 34–35.
Gouyon J-B, Guignard J-P 1988 Theophylline prevents the hypoxemia-induced renal hemodynamic changes in rabbits. Kidney Int 33: 1078–1083.
Ballèvre L, Thonney M, Guignard JP 1996 Role of nitric oxide in the hypoxemia-induced renal dysfunction of the newborn rabbit. Pediatr Res 39: 725–730.
Drukker A, Goldsmith DI, Spitzer A, Edelmann CM, Blaufox MD 1980 The renin angiotensin system in newborn dogs: developmental patterns and response to acute saline loading. Pediatr Res 14: 304–307.
Davidson D 1987 Circulating vasoactive substances and hemodynamic adjustments at birth in lambs. J Appl Physiol 63: 676–684.
Navar CG, Rosivall L, Carmines PV, Oparil 1986 Effects of locally formed angiotensin II on renal hemodynamics. Fed Proc 45: 1448–1453.
Tuffley RE, Rubenstein RH, Slater JD, Williams ES 1970 Serum renin activity during exposure to hypoxia. J Endoc 48: 497–510.
Broughton-Pipkin F, Phil P, Smales ORC 1977 A study of factors affecting blood pressure and angiotensin II in newborn infants. J Pediatr 91: 113–119.
Weismann DN, Clarke WR 1981 Postnatal age-related renal responses to hypoxemia in lambs. Circ Res 49: 1332–1338.
Alward CT, Hook JB, Helmrath TA, Bailie MD 1978 Effects of asphyxia on renal function in the newborn piglet. Pediatr Res 12: 225–228.
Morin JP, Moulin B, Borghi H, Fillastre JP 1989 High affinity binding sites for perindopril a new inhibitor of angiotensin I converting enzyme (ACE) in the rabbit kidney. Int J Tiss Reac 11: 81–92.
Erdös EG 1975 Angiotensin I converting enzyme. Circ Res 36: 247–255.
Toth-Heyn P, Mosig D, Guignard JP 1998 Renal effects of angiotensin converting enzyme inhibition in the newborn rabbit: role of bradykinin. Life Sci 62: 309–318.
Wright HK, Gann 1966 An automatic anthrone method for the determination of inulin in plasma and urine. J Lab Clin Med 67: 689–693.
Bratton AC, Marshall EK 1939 A new coupling component for sulfanilamide determination. J Biol Chem 128: 537–550.
Huet F, Gouyon JB, Guignard JP 1997 Prevention of the hypoxemia-induced renal dysfunction by perindoprilat in the rabbit. Life Sci 61: 2157–2165.
Robillard JE, Nakamura KT 1988 Neurohormonal regulation of renal function during development. Am J Physiol 254: F771–F779.
Robillard JE, Weismann DN, Gomez RA, Ayres NA, Lawton WJ, VanOrden DE 1983 Renal and adrenal responses to converting-enzyme inhibition in fetal and newborn life. Am J Physiol 244: R249–R256.
Robillard JE, Gomez RA, VanOrden DE, Smith FG 1982 Comparisonof the adrenal and renal responses to angiotensin II in fetal lambs and adult sheep. Circ Res 50: 140–147.
Osborn JL, Hook JB, Bailie MD 1980 Effect of saralasin and indomethacin on renal function in developing piglets. Am J Physiol 238: R438–R442.
Gomez RA, Robillard JE 1984 Developmental aspects of the renal responses to hemorrhage during converting-enzyme inhibition in fetal lambs. Circ Res 54: 301–312.
Nakamura KT, Ayres NA, Gomez RA, Robillard JE 1985 Renal responses to hypoxemia during renin-angiotensin system inhibition in fetal lambs. Am J Physiol 249: R116–R124.
Lumbers ER, Burrell JH, Menzies RI, Stevens AD 1993 The effects of a converting enzyme inhibitor (captopril) and angiotensin II on fetal renal function. Br J Pharmacol 110: 821–827.
Rose JC, Block SM, Flowe K, Morris M, South S, Sundberg DK, Zimmerman C 1987 Responses to converting-enzyme inhibition and hemorrhage in newborn lambs and adult sheep. Am J Physiol 252: R306–R313.
Ciuffo GM, Viswanathan M, Seltzer AM, Tsutsumi K, Saavedra JM 1993 Glomerular angiotensin II receptor subtypes during development of rat kidney. Am J Physiol 265: F264–F271.
Solhaug MJ, Wallace MR, Granger JP 1996 Nitric oxide and angiotensin II regulation of renal hemodynamics in the developing piglet. Pediatr Res 39: 527–533.
John EG, Bhat R, Zeis PM, Vidyasagar D 1980 Effects of hypoxia, hypocarbia and acidemia on renal functions and hemodynamics in puppies. Int J Pediatr Nephrol 1: 167–171.
Drummond WH, Lindheimer CA 1982 Plasma renin activity during acute ventilatory hypoxia in the ewe and fetal lambs. Biol Neonate 42: 291–298.
Brezis M, Greenfeld Z, Shina A, Rosen S 1990 Angiotensin II augments medullary hypoxia and predisposes to acute renal failure. Eur J Clin Invest 20: 199–207.
Kon V, Fogo A, Ichikawa I 1993 Bradykinin causes selective efferent arteriolar dilation during angiotensin converting enzyme inhibition. Kidney Int 44: 545–550.
Dietrich MS, Endlich MS, Parekh N, Steinhausen 1991 Interaction between adenosine and angiotensin II in renal microcirculation. Microvasc Res 41: 275–288.
Guignard J-P, Burgener F, Calame A 1981 Persistent anuria in a neonate: a side effect of captopril?. Intern J Pediatr Nephrol 2: 133
Broughton-Pipkin F, Baker PN, Symonds EM 1989 ACE inhibitors in pregnancy. Lancet 2: 96–97.
Acknowledgements
The authors thank Michèle Thonney and Olympia Grigoras for technical assistance and A. Drukker for valuable criticisms of the manuscript.
Author information
Authors and Affiliations
Additional information
This study was supported by Grant No. 32-26395.89/2 from the Swiss National Science Foundation.
Rights and permissions
About this article
Cite this article
Huet, F., Semama, D., Gouyon, JB. et al. Protective Effect of Perindoprilat in the Hypoxemia-Induced Renal Dysfunction in the Newborn Rabbit. Pediatr Res 45, 138–142 (1999). https://doi.org/10.1203/00006450-199901000-00023
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199901000-00023
This article is cited by
-
Impact of acute kidney injury on in-hospital outcomes in Chinese patients with community acquired pneumonia
BMC Pulmonary Medicine (2021)
-
Kidney-lung connections in acute and chronic diseases: current perspectives
Journal of Nephrology (2016)
-
Beneficial effect of insulin-like growth factor-1 on hypoxemic renal dysfunction in the newborn rabbit
Pediatric Nephrology (2009)