Abstract
Obstruction of narrow vessels by rigid neutrophils may contribute to ischemic organ injury. In septicemia, a substantial portion of the neutrophils may become activated and the number of circulating immature neutrophils may rise sharply. Volume and deformability of mature (PMN) and immature neutrophils in healthy preterm and full-term infants and in septicemic neonates were studied by means of a micropipette system. Membrane cytoplasm tongues were aspirated into 2.5-µm (diameter) pipettes over a period of 60 s. Volume and tongue growth of mature resting PMN were similar in healthy preterm and full-term neonates and adults. Compared with mature PMN (about 360 fl), the volumes of band cells (415 fl), metamyelocytes (470 fl), and less mature cells (myeloblasts, promyelocytes, and myelocytes; 490 fl) were significantly increased (p < 0.005). Final tongue lengths of band cells, metamyelocytes, and less mature cells were decreased by about 50, 60, and 70%, respectively, when compared with passive mature cells. In septic neonates, the percentage of immature neutrophils was increased, but the deformability and volume of the cell subpopulations were not affected by septicemia. Active PMN were characterized by pseudopod formation. More active PMN were found in group B streptococcal (14% of total PMN), Gram-negative (12%), and Staphylococcus epidermidis septicemia (8%) than in healthy neonates and adults (4%). The main bodies of active PMN were less deformable than passive PMN, and the pseudopods showed very little membrane deformation. The increased number of rigid active and immature neutrophils may contribute to impaired microcirculation and the high risk for organ injury in septic patients.
Similar content being viewed by others
Main
Leukocytes must deform markedly to pass through narrow capillaries with diameters of about 5 µm (1). Both neonatal PMN and erythrocytes have resting diameters of approximately 9 µm (2,3), but mature PMN have a 4 times larger volume (2,3) and 500 times higher flow resistance through 5-µm filter pores (4) than do erythrocytes. Fortunately, leukocytes usually travel through relatively wide capillaries with high flow, thereby requiring little or no deformation (5). At low perfusion pressure, however, leukocytes may enter into narrow capillaries with low flow and obstruct these vessels, thereby further deteriorating flow through ischemic tissues. A major role of PMN accumulation in the development of severe tissue injury has been shown in adult animal models with cardiac (6), cerebral (7), and gastrointestinal (8) ischemia. Capillary leukostasis may also contribute to the "no-reflow" phenomenon after local or general ischemia (9). Recently, PMN accumulation has been shown in brain vessels of the neonatal rat after ligation of the right common carotid artery and systemic hypoxia (10).
Accumulation of leukocytes in low flow tissues is intensified by increased cell rigidity and large cell volume (5,11). Immature granulocytes in neonates and adults are both less deformable and larger than are mature PMN (2,12–14). In neonatal septicemia, up to 100% of the circulating neutrophils may be immature (15). In addition to their impaired function (16), the rigid and large immature neutrophils may more than mature PMN tend to obstruct narrow vessels.
In neonates with septicemia (17) and severe surfactant deficiency (18), a large percentage of neutrophils may become activated. Active PMN are very rigid both in vitro (19) and in vivo (1,20) and may therefore rapidly obstruct narrow vessels (1,6,20).
Previous studies have shown that erythrocyte deformability may markedly decrease in Gram-negative (21) and Gram-positive septicemia (22). Moreover, in adults with septicemia the passage time of isolated PMN may be prolonged by 100-200% (23). Because individual PMN have not been studied in septicemia, it is unclear whether impaired deformability of PMN is a result of increased numbers of rigid immature or activated neutrophils or of increased overall rigidity of the circulating neutrophils. Moreover, no study on the deformability of neutrophils in neonates with septicemia appears to exist in the literature. The present investigation was designed to compare the volume and deformability of passive and active mature PMN and of immature neutrophils in healthy and septicemic neonates.
METHODS
Patients. Six groups (see Table 1) were studied with approval of the ethics committee of the University of Heidelberg Medical Center: 1) 20 healthy nonsmoking adults; 2) 20 healthy full-term infants; 3) 20 healthy preterm infants without signs of infection, respiratory distress, or other disorders and without need of assisted ventilation (28-32 wk of gestation); 4) 9 neonates with GBS septicemia (33-40 wk of gestation); 5) 10 neonates with Gram-negative septicemia (6 Escherichia coli, 2 Enterobacter cloacae; 2 Klebsiella oxytoca; 28-37 wk of gestation); and 6) 7 neonates with Staphylococcus epidermidis septicemia (28-32 wk of gestation). All septic babies showed clinical signs of septicemia, CRP > 20 mg/L (nephelometry), and septicemia was proven by a positive blood culture. The blood samples for the micropipette studies (0.5 mL) were anticoagulated with EDTA (1 mg/mL) (18). All studies on one blood sample were finished within 3 h. The blood samples of the neonates were primarily taken for routine laboratory tests (blood cultures, CRP, leukocyte count, differential blood picture, screening tests, and so forth). None of the infants and adults received antibiotics at the time of blood sampling. Informed consent of the parents was obtained before blood sampling.
Micropipette system. Pipettes with internal diameters of 2.5 µm were used to aspirate membrane-cytoplasm tongues of granulocytes (24–26). Details of the leukocyte preparation, the micropipette system, and the procedure of leukocyte deformation studies have been described elsewhere (2,14). The blood was centrifuged at 350 × g and 4°C for 25 min. Leukocytes were taken directly from the buffy coat. A separation medium was not used. The cells were observed using a light microscope with an optical magnification of X788. The additional electronic magnification of the video system resulted in a final magnification of X4000. The studies were carried out at 22°C. An aspiration pressure of 2 cm H2O was applied. The length of the aspirated tongue was measured from video recording after 5, 10, 20, 30, 40, 50, and 60 s. The diameter (D) of each cell was measured before aspiration. Because passive neutrophils had a spherical shape (Fig. 1), the volume (V) of each individual cell was calculated as V = ([pi]a/6)(D3). Volume of active PMN was calculated only if the cell shape was spherical.
Leukocyte subpopulations. The leukocyte subpopulations were identified during the microscopic deformation studies. Several previous studies have shown that different types of leukocytes, of neutrophils and their precursors as well as activated neutrophils can be distinguished by light microscopy (2,12,14,24–27). Sometimes the granules interfere with the view of the nucleus. But the nucleus always becomes clearly visible upon tongue aspiration (25). Mature neutrophils were distinguished from eosinophils and basophils by their smaller and lighter granules. Mature and immature neutrophils were distinguished by the shape of their nucleus. Myeloblasts and promyelocytes contain a round or oval nucleus. Myelocytes contain an oval or indented nucleus. Because of their small number, we combined the results of myeloblasts, promyelocytes, and myelocytes. Metamyelocytes were defined as cells with a nucleus shaped like a kidney or a rod. In band cells, the nucleus is of uniform thickness and curved throughout. In mature PMN, the nucleus consists of two to five or more distinct lobes.
Activation of neutrophils was assumed if pseudopod projections greater than 0.5 µm were visible (Fig. 1), tongue growth in the pipette abruptly slowed or stopped, or tongues partially retracted from the pipette during aspiration (25–27).
In each blood sample, the distribution of passive and activated mature PMN and of immature neutrophils were initially counted among 100 PMN. Then cells were purposely selected for the deformation studies to yield sufficient numbers for each cell subpopulation. In each sample, 20 passive mature PMN were studied. PMN activated upon contact with the glass surface of the micropipette were added to the number of activated cells showing pseudopods before aspiration into the pipette.
Statistical analysis. Means and SD were calculated for leukocyte counts, percentages of neutrophil subpopulations and CRP (Table 1), and for the neutrophil volumes and tongue lengths (Table 2). Table 2 presents the values for the entire cell populations of each cell type for each of the six groups. Statistical analyses were performed to test for intergroup differences between the combined values of the healthy full-term and preterm infants and each of the three groups of septicemic infants. Moreover, differences of volume and deformation behavior among various neutrophil subpopulations were analyzed separately for each of the six groups (Table 2). Kruskal-Wallis nonparametric analysis of variance was used to calculate significances. Because of the large number of comparisons, significant differences were defined as p < 0.005.
RESULTS
The total leukocyte and neutrophil counts, the percentages of the neutrophil subpopulations, and the CRP values are summarized in Table 1. Neutropenia (neutrophil count <2 × 109/L) was observed in 3 of 9 infants with GBS, 4 of 10 with Gram-negative, and none with S. epidermidis septicemia. One infant with E. coli and two with S. epidermidis septicemia had neutrophilia (neutrophil count >25 × 109/L).
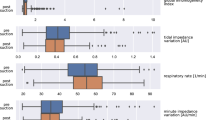
Cellular volume increased progressively with decreasing leukocyte maturity. The volume of each cell type was similar in the six groups and not affected by septicemia (Table 2). Compared with mature PMN, the volumes of immature neutrophils were increased by 14-22% (band cells), 28-36% (metamyelocytes), and 36-42% (myelocytes, promyelocytes, and myeloblasts).
All passive cells showed steady tongue formation in 2.5-µm micropipettes (Table 2; Fig. 2). Immature neutrophils showed diminished tongue growth. Compared with mature passive PMN, final tongue lengths of immature neutrophils were decreased by about 50% (band cells), 60% (metamyelocytes), and 70% (myelocytes, promyelocytes, myeloblasts). Tongue growth of the same cell type was similar in neonates and adults and was not significantly affected by septicemia (Table 2).
In infants with septicemia, a substantial number of the mature neutrophils were active or became activated upon aspiration into glass pipettes. Neonates with GBS (14%) and Gram-negative septicemia (12%) showed more active PMN than infants with S. epidermidis septicemia (8%). Immature neutrophils showed no activation.
We observed three types of active neutrophils among the 88 active PMN studied in septicemic infants and the 56 active PMN in healthy blood donors: 1) cells with visible pseudopods before aspiration of a membrane-cytoplasm tongue into the pipette (32 and 11%, respectively); 2) cells with abrupt stoppage or slowing of tongue growth (42 and 64%), and 3) retraction from the pipette in spite of continuous aspiration (26 and 25%). Most active PMN showed relatively fast tongue growth during the first 5 s, but little or no further tongue growth during the following 55 s (Fig. 3).
The main cell body of PMN with visible activation before aspiration showed similar tongue formation as passive cells during the first 5 s of aspiration. Thereafter, the tongue growth was markedly reduced. Cells activated during aspiration demonstrated a sudden cessation of tongue growth at the time of activation. Passive deformation of pseudopods was studied in 20 PMN from septic neonates. Pseudopods formed small tongues only (Fig. 3), suggesting marked rigidity.
DISCUSSION
During bacterial infection, large numbers of neutrophils are released from the bone marrow into the circulating blood (15). Many of these cells are rapidly sequestered in the vascular bed of infected tissues. If the supply is less than the sequestration, blood neutropenia results. The increase in neutrophil release from the bone marrow is usually associated with the release of immature neutrophils. In our study, one third of the circulating PMN were immature in neonates with GBS and Gram-negative septicemia, whereas in neonates with S. epidermidis septicemia only 17% of the PMN were immature (Table 1).
During septicemia, several inflammatory mediators are activated or released from the infected tissues and cause activation of both blood vessel endothelium and leukocytes (28). Neutrophils are recruited for phagocytosis and microbial killing at the site of infection or injury. The expression of adhesion molecules and their ligands increases, thereby causing local accumulation and adhesion of leukocytes. Due to their elevated adhesion energy, active neutrophils are usually not found in circulating blood (27). However, we observed that in vitro manipulation may cause visible activation of a substantial number of neutrophils in septicemia (Table 1). This suggests that in septicemia circulating neutrophils are more susceptible to activation.
Neutrophils activated in vitro or in vivo with chemoattractants are much stiffer than passive neutrophils (1,19–20). In particular, pseudopods formed during activation are extremely rigid (29). We have shown similar behavior of active PMN and their pseudopods in septic neonates. Pseudopods are formed as a result of polymerization and alignment of actin molecules near the PMN membrane surface. The rigidification of pseudopods may be explained by the change of the physical properties of the membrane cytoplasm from a viscoelastic semifluid to an elastic solid and the loss of excess membrane surface area (29). Because the activated peripheral neutrophils behaved similarly as neutrophils with chemotactic activation (11,20), we assume that the activated peripheral neutrophils are representative of neutrophils that are sequestrated in vivo.
Immature neutrophils are larger and less deformable than mature neutrophils. In spite of their poor deformability, even high counts of immature leukocytes (e.g. in leukemia) rarely cause small vessel obstruction (leukostasis) and organ ischemia, as long as the perfusion pressure is normal (30). In vessels with diameters of less than 200 µm, the large leukocytes travel in the rapid center stream and preferentially flow into relatively wide branches with high flow. Upon reduction of flow, leukocytes are displaced from the center stream to the slowly flowing vessel margin and travel into relatively narrow branches with slow flow, thereby further deteriorating blood flow in these vessels (5). The extent of capillary leukostasis at low perfusion pressure depends on the deformability of the leukocytes (11). Thus, although immature neutrophils show little or no motility and adhesion (16), they may enhance leukostasis and capillary obstruction at low perfusion pressure.
We conclude that increased stiffness of immature and activated leukocytes may play an important role in the development of vessel obstruction in septicemia; immature neutrophils are larger and more rigid than mature PMN and may, therefore, intensify leukocyte sequestration in septicemia. Activated PMN are extremely rigid and readily adhere to endothelium, thereby obstructing small vessels. Sequestration of PMN may contribute to pulmonary hypertension (31), ischemic brain damage (32), and necrotizing enterocolitis (8) in septicemia. We speculate that inhibition of PMN activation by drugs (e.g. pentoxifylline) (33) may ameliorate the circulatory complications of septicemia.
Abbreviations
- CRP:
-
C-reactive protein
- GBS:
-
group B streptococcus
- PMN:
-
polymorphonuclear cells
References
Worthen GS, Schwab B, Elson EL, Downey GP 1989 Mechanics of stimulated neutrophils: cell stiffening induces retention in capillaries. Science 245: 183–186
Ruef P, Böhler T, Linderkamp O 1991 Deformability and volume of neonatal and adult leukocytes. Pediatr Res 29: 128–132
Linderkamp O, Nash GB, Wu PYK, Meiselman HJ 1986 Deformability and intrinsic material properties of neonatal red blood cells. Blood 67: 1244–1250
Chien S, Schmalzer EA, Lee MML, Impelluso T, Skalak R 1983 Role of white blood cells in filtration of blood cell suspensions. Biorheology 20: 11–27
Gaehtgens P 1987 Pathways and interactions of white cells in the microcirculation. Prog Appl Microcirc 12: 51–65
Schmid-Schöbein GW 1987 Capillary plugging by granulocytes and the no-reflow phenomenon in the microcirculation. Fed Proc 46: 2397–2401
Matsuo Y, Onodera H, Shiga Y, Nakamura M, Ninomiya M, Kihara T, Kogure K 1994 Correlation between myeloperoxidase-quantified neutrophil accumulation and ischemic brain injury in the rat: effects of neutrophil depletion. Stroke 25: 1469–1475
Zimmerman BJ, Guillory DJ, Grisham MB, Gaginella TS, Granger DN 1990 Role of leukotriene B4 in granulocyte infiltration into the postischemic feline intestine. Gastroenterology 99: 1358–1363
Hansell P, Borgstrom P, Arfors KE 1993 Pressure-related capillary leukostasis following ischemia-reperfusion and hemorrhagic shock. Am J Physiol 265: H381–H388
Hudome S, Palmer C, Roberts RL, Mauger D, Housman C, Towfighi J 1997 The role of neutrophils in the production of hypoxic-ischemic brain injury in the neonatal rat. Pediatr Res 41: 607–616
Bagge U, Braide P 1985 Microcirculatory effects of white cells in shock. Prog Appl Microcirc 7: 43–50
Lichtman MA 1970 Cellular deformability during maturation of the myeloblast. Possible role in marrow egress. N Engl J Med 283: 943–948
Linderkamp O, Hammer BJ, Miller R 1986 Filterability of erythrocytes and whole blood in preterm and full-term neonates and adults. Pediatr Res 20: 1269–1273
Ruef P, Zilow EP, Linderkamp O 1994 Deformability of peripheral immature and mature neutrophils. Clin Hemorheol 14: 233–236
Christensen RD, Bradley PP, Rothstein G 1981 The leukocyte left shift in clinical and experimental neonatal sepsis. J Pediatr 98: 101–105
Krause PJ, Kreutzer DL, Eisenfeld L, Herson V C, Weisman S, Bannon P, Greca N 1989 Characterization of nonmotile neutrophil subpopulations in neonates and adults. Pediatr Res 25: 519–524
Gessler P, Nebe T, Birkle A, Haas N, Kachel W 1996 Neutrophil respiratory burst in term and preterm neonates without signs of infection and in those with increased levels of C-reactive protein. Pediatr Res 39: 843–848
Brus F, van Oeveren W, Okken A, Bambang Oetomo S 1996 Activation of circulating polymorphonuclear leukocytes in preterm infants with severe idiopathic respiratory distress syndrome. Pediatr Res 39: 456–463
Nash GB, Jones JG, Mikita J, Christopher B, Dormandy JA 1988 Effects of preparative procedures and of cell activation on flow of white cells through micropore filters. Br J Haematol 70: 171–176
Lipowsky HH, Riedel D, Shi GS 1991 In vivo mechanical properties of leukocytes during adhesion to venular endothelium. Biorheology 28: 53–64
Linderkamp O., Klose HJ, Kelson S, Fuhrmann G, Galanos C, Marget W, Riegel KP, Betke K 1981 Effect of endotoxin and exchange transfusion on red cell deformability. Bibl Anat 20: 174–177
Pöschl JMB, Ruef P, Schnauffer M, Pohl S, Sonntag HG, Linderkamp O 1996 Group B streptococcus impairs erythrocyte deformability in neonates more than in adults. Arch Dis Child 74: F187–F190
Drost EM, Fisher TC, Kassabian G, Gelmont D, Meiselman HJ 1995 Altered neutrophil deformability in sepsis syndrome. Biorheology 32: 128( abstr)
Schmid-Schönbein GW, Sung K, Tözeren H, Skalak R, Chien S 1981 Passive mechanical properties of human leukocytes. Biophys J 36: 243–256
Evans E, Kukan B 1984 Passive material behavior of granulocytes based on large deformation and recovery after deformation tests. Blood 64: 1028–1036
Nash GB, Meiselman HJ 1986 Rheological properties of individual polymorphonuclear granulocytes and lymphocytes. Clin Hemorheol 6: 87–97
Chang RRK, Chien NTY, Chen CH, Jan KM, Schmid-Schönbein GW, Chien S 1992 Spontaneous activation of circulating granulocytes in patients with acute myocardial and cerebral diseases. Biorheology 29: 549–561
Zilow G, ZIilow EP, Burger R, Linderkamp O 1993 Complement activation in newborn infants with early onset infection. Pediatr Res 34: 199–203
Dong C, Skalak R, Sung KL, Schmid-Scönbein GW, Chien S 1987 Passive deformation analysis of human leukocytes. J Biomech Eng 110: 27–36
Lichtman MA, Rowe JM 1982 Hyperleukocytic leukemias: rheological, clinical, and therapeutic considerations. Blood 60: 279–283
Engelhardt B, Sandberg K, Bratton D, van den Abbele A, Grogaard J, Hellerqvist C, Sundell H 1987 The role of granulocytes in the pulmonary response to group B streptococcal toxin in young lambs. Pediatr Res 21: 159–165
Faix RG, Donn SM 1985 Association of septic shock caused by early-onset group B streptococcal sepsis and periventricular leukomalacia in the preterm infant. Pediatrics 76: 415–419
del Moral T, Goldberg RN, Urbon J, Suguihara C, Martinez O, Stein-Streilein J, Feuer WJ, Bancalari E 1996 Effects of treatment with pentoxifylline on the cardiovascular manifestations of group B streptococcal sepsis in the piglet. Pediatr Res 40: 469–474
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Linderkamp, O., Ruef, P., Brenner, B. et al. Passive Deformability of Mature, Immature, and Active Neutrophils in Healthy and Septicemic Neonates. Pediatr Res 44, 946–950 (1998). https://doi.org/10.1203/00006450-199812000-00021
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199812000-00021
This article is cited by
-
Characterization of Circulating Low-Density Neutrophils Intrinsic Properties in Healthy and Asthmatic Horses
Scientific Reports (2017)
-
Effects of volume resuscitation on the microcirculation in animal models of lipopolysaccharide sepsis: a systematic review
Intensive Care Medicine Experimental (2016)
-
The diagnostic and prognostic significance of monitoring blood levels of immature neutrophils in patients with systemic inflammation
Critical Care (2015)
-
Microvascular Dysfunction in Sepsis
Microcirculation (2000)