Abstract
Intraischemic reduction in temperature of 2-3 °C (modest hypothermia) has been demonstrated to provide partial neuroprotection in neonatal animals. This investigation determined if modest hypothermia initiated immediately after brain ischemia provides neuroprotection. Piglets were studied with rectal temperature maintained during the 1st h after 15 min of brain ischemia at either 38.3 ± 0.3 °C (normothermia, n = 11) or at 35.8± 0.5 °C (modest hypothermia, n = 11). The severity of brain ischemia was similar between groups as indicated by equivalent reduction in mean blood pressure (90 ± 15 to 24 ± 3 versus 92± 13 to 26 ± 3 mm Hg), and changes in cerebral metabolites and intracellular pH (pHi) measured by magnetic resonance spectroscopy(β-nucleoside triphosphate = 44 ± 9 versus 42 ± 18% of control, control = 100%, pHi: 6.25±.15 versus 6.24 ± 0.22 for normothermic and modestly hypothermic groups, respectively). In the first 90 min after ischemia, there were no differences between groups in the duration and extent of brain acidosis, and relative concentrations of phosphorylated metabolites. Categorical assessment of neurobehavior was evaluated at 72 h postischemia (n = 16), or earlier if an animal's condition deteriorated (n = 6). Postischemic hypothermia was associated with less severe stages of encephalopathy compared with normothermia (p = 0.05). Histologic neuronal injury was assessed categorically in 16 brain regions, and postischemic hypothermia resulted in less neuronal injury in temporal (p = 0.024) and occipital (p = 0.044) cortex at 10 mm beneath the cortical surface, and in the basal ganglia (p = 0.038) compared with that in normothermia. Modest hypothermia for 1 h immediately after brain ischemia provides partial neuroprotection and may represent an adjunct to resuscitative strategies.
Similar content being viewed by others
Main
In 1950 it was reported that deep hypothermia extended the duration in which the brain can tolerate ischemia(1). Approximately 10 y ago, it was recognized that much smaller reductions in brain temperature during ischemia or hypoxia-ischemia can attenuate the extent of subsequent neuronal necrosis(2). A temperature change of 1-4 °C has been termed modest hypothermia, and associated intraischemic neuroprotection has been confirmed in multiple adult species as recently summarized by Ginsberg et al.(3). A limited number of reports have provided similar observations in neonates. During hypoxia-ischemia decreasing axillary temperature by 2.5 °C in 10-d-old Sprague-Dawley rats(4) and lowering brain temperature by 3 °C in 7-d-old Wistar rats(5) were associated with a reduction in brain damage. These observations complement our observation that a 2-3 °C reduction in brain temperature during 15 min of incomplete ischemia provides partial neuroprotection in neonatal swine(6). All of the above investigations used modest hypothermia as a protective strategy (i.e. during ischemia). There is greater potential clinical applicability if modest hypothermia is efficacious as a resuscitative therapy. This is especially pertinent for neonates, because ischemia or hypoxia-ischemia may occur before or during delivery, or unexpectedly in otherwise stable infants within a neonatal intensive care unit. Studies in adult animals that evaluated modest hypothermia initiated in the postischemic interval demonstrated an attenuation of neuropathologic damage(7–10), although no effect has been found in some models(11, 12).
There is less experience with modest hypothermia implemented for resuscitation in neonatal models. At present there are two reports using hypoxia-ischemia in 7-d-old rat pups that provide conflicting results. Yager et al.(5) reported no cerebral protection associated with maintaining brain temperature at either 34 or 31 °C compared with 37 °C for 3 h after hypoxia-ischemia. In contrast, Thoresen et al.(13) found that a 6 °C reduction in rectal temperature for 3 h immediately after hypoxia-ischemia reduced the extent of brain damage. There are important differences between the latter two studies that may contribute to the discrepant results; these include length of hypoxia-ischemia, use of restraints, age of assessment for brain damage, and different normothermic temperatures despite similar temperature differences between normothermic and hypothermic groups. Thus, there is insufficient information in neonatal models to draw conclusions regarding the efficacy of modest hypothermia as a resuscitative strategy. The present report investigated neonatal swine with the following two purposes: 1) is modest hypothermia initiated immediately after brain ischemia associated with less brain damage compared with animals maintained normothermic? and 2) are there changes in brain energy state immediately after brain ischemia that may contribute to putative benefits of modest hypothermia?
METHODS
This investigation was approved by the Institutional Review Board for Animal Research at the University of Texas South-western Medical Center at Dallas. Details concerning the surgical preparation have been reported previously(6). Briefly, 22 piglets were studied in the first 2 wk of life. This age range allowed maximal use of animals in each litter and was similar to our prior report(6) facilitating future comparisons between studies. The brain of newborn swine has been estimated to be comparable to that of a full-term human(14), but accurate developmental correlations over the first 2 wk of life are unavailable. Piglets were aseptically instrumented 24 h before the experiment using ketamine (20 mg/kg) and pentobarbital (20 mg/kg) for anesthesia. Catheters were positioned in the superior vena cava via the internal and external jugular veins, and the left common carotid artery, and then tunneled s.c. to the animal's back to be stored in a pouch. On the day of the experiment animals were intubated after thiopental (20 mg/kg) administration, and mechanically ventilated with inspired gases of 70% N2O and 30% O2. Vecuronium (0.25 mg/kg/h i.v.) and nalbuphine HCl (0.15 mg/kg i.v.) were given for muscle paralysis and analgesia, respectively. Rectal temperature was measured with a thermocouple microprobe, and a blood pressure cuff was positioned around the animal's neck. Animals were then transported to the Magnetic Resonance Laboratory, wrapped in a thermal blanket, and placed supine in a plexiglass cylinder with the head resting on a rectangular 4 × 5 cm double tuned (31P and1 H) surface coil. Animals were allowed to stabilize after positioning the cylinder inside the bore of a superconducting magnet.
The experimental protocol consisted of a 20-min steady-state control period, 15 min of partial brain ischemia, and a 90-min postischemic interval. Brain ischemia was induced by hemorrhage via a venous catheter to a MABP of approximately 30 mm Hg and inflation of a blood pressure cuff around the neck to 300 mm Hg. In 11 piglets rectal temperature was maintained normothermic throughout, and in 11 piglets an identical protocol was followed except that rectal temperature was reduced 2-3 °C (modest hypothermia) immediately after ischemia. Rectal temperature was altered in the modestly hypothermic animals by changing the temperature of the circulating water through the thermal blanket and cooling the hemorrhaged blood (approximately 30 mL/kg) to 30 °C before reinfusion. After the postischemic interval, animals were weaned from the ventilator, extubated, returned to their pens, and maintained for 72 h.
One additional piglet was studied to verify that rectal temperature could be used as an index of brain temperature in the postischemic interval. A 6-d-old piglet was acutely instrumented on the day of the experiment with placement of intravascular catheters, rectal and a brain temperature probe(depth of 2 cm from the cortical surface). The animal was wrapped in a thermal blanket to allow manipulation of rectal temperature and was subjected to two 15-min intervals of normothermic brain ischemia as described above separated by 145 min. After the first episode of brain ischemia, rectal temperature was rapidly reduced to achieve modest hypothermia, which was maintained for 1 h. The piglet was then rewarmed for the second interval of brain ischemia, after which rectal temperature was maintained normothermic.
Heart rate, MABP, and arterial blood samples for blood gases, pH, hematocrit, and plasma concentrations of glucose and lactic acid were measured during steady-state control conditions (in duplicate), at 4 and 12 min during ischemia, and at 5, 30, 60, and 90 min postischemia, and at 24, 48, and 72 h after ischemia. 31P MR spectra of piglet brain were acquired during steady-state control conditions (in duplicate), ischemia (two consecutive spectra), and postischemia (collected in pairs at 30-min intervals to 90 min postischemia) on a Nicolet NT-80 NMR system equipped with a 30-cm diameter bore TMR 32/200 superconducting magnet (Oxford) operating at 32.5 MHz for31 P and 80.3 MHz for 1H as previously described(15). Each 31P MR spectrum (7.5 min) was obtained using acquisition parameters of 45-μs pulse width, 256-ms acquisition time, 1.5 s interpulse delay, sweep width of 2000 Hz, 4K data points per free induction decay, and 256 free induction decay transients per spectrum. Spectra were processed by left shift removal of the first three data points in the accumulated free induction decay and right shifting to reestablish phase integrity of the spectrum, and by application of exponential multiplication(10-Hz line broadening) before Fourier transformation. Baseline straightening was performed with the use of a spline interpolation routine.
Two outcome variables, clinical neurologic assessment and neuronal histology, were assessed. Neurologic assessment was determined by a modification of the OPS described by Leonov et al.(16) and previously adapted in this laboratory(6, 15). The OPS evaluates the state of awareness, ambulation, muscle tone, abnormal movements, presence or absence of hyperventilation and seizures, response to sensory stimuli, and the ability to feed. Piglets were scored daily and categorized as normal or encephalopathic(mild, moderate, severe). Neuronal histology was determined after brain perfusion and fixation at 72 h after ischemia or earlier if animals expired prematurely, as described previously(6). Brains were sectioned in axial orientation at depths of approximately 5, 10, 15, 20, and 25 mm from the cortical surface, processed, and stained with hematoxylin and eosin. Ischemic neuronal damage was determined by a neuropathologist (D.K.B.) blinded to group assignment and was based on the presence of nuclear pyknosis and karyolysis, and cytoplasmic retraction and eosinophilia. Neuronal morphology in 16 predefined brain regions was scored on a scale of 0 to 4 as follows: 0, normal; 1, scattered isolated ischemic neurons; 2, cluster of ischemic neurons; 3, laminar necrosis; and 4, ischemic changes in almost all or all neurons.
MR spectra resonance peaks were quantitated by comparison of peak heights acquired during and after ischemia with values at steady-state control conditions and expressed as a percent of control. pHi was derived from the chemical shift of the Pi resonance peak relative to the PCr peak using the following equation: where χ is the chemical shift of the Pi peak(17). Kost(18) used in vitro calibrations to demonstrate that temperature affects the calculation of pHi using the aboveequation. However, the magnitude of this effect over the temperature range studied (35-38 °C) was negligibly small (i.e. less than 0.01 pH unit). In addition a previous study using this animal model showed that the effect of temperature on pHi in vivo was less than 0.03 unit from 35 to 38 °C(19). An estimate of the total phosphate pool from the area of the 31P spectrum from 10 to-20 ppm was determined as previously reported(20). During preischemia and the final postischemia periods, plots of 31P spectra were cut and weighed; the weight was taken as a measure of the total area. A repeated measures analysis of variance (SAS) was used to compare brain metabolic and systemic variables of the normothermic and modestly hypothermic groups. If significance was achieved (p < 0.05) a Bonferroni-adjusted multiple comparisons to localize significant group-time interaction (p < 0.0016) and time effects (<0.0018-0.0024, depending on the number of comparisons) was used. Comparison of OPS between groups was performed using a one-sided exact linear-by-linear test. Neuronal histologic scores were compared between groups by a one-sided Mann-Whitney test. Spearman's correlation was used to examine the relationship between histologic scores and OPS. All results are mean ± SD.
RESULTS
The measurement of rectal temperature facilitated comparison of animals with a 2-3 °C difference in brain temperature during the immediate postischemic interval without direct measurement of brain temperature in chronically instrumented piglets. To validate the use of rectal temperature as an index of brain temperature, brain and rectal temperature were compared in one piglet during and after two ischemic intervals (Fig. 1). During both intervals of ischemia brain temperature decreased, whereas rectal temperature was maintained constant. In the postischemic interval, rapid reduction or maintenance of a constant rectal temperature resulted in distinct brain temperatures with ranges of 35-36 °C or 37.5-38 °C, respectively.
The relationship between rectal (circle) and brain temperature (square) measured at a depth of 2 cm from the brain surface. Temperatures were recorded during two sequential sequences of control (C), ischemia (Isc), and postischemia(PostIsc). In the first sequence rectal temperature was reduced at the beginning of the postischemic interval and was maintained hypothermic for a 60-min duration (horizontal solid bar), and in the second sequence rectal temperature was maintained normothermic throughout.
Normothermic and modest hypothermia groups were comparable in age and weight (9 ± 4 d and 1.6 ± 0.5 kg and 10 ± 4 d and 1.5± 0.5 kg for normothermic and hypothermic animals, respectively). Different rectal temperatures (Fig. 2) occurred between groups by 4 min postischemia and persisted for 60 min. Although hypothermic animals were rewarmed after 60 min, rectal temperature was still slightly reduced compared with normothermic animals at the completion of the postischemia interval. Changes in MABP were nearly identical between groups, and tests of time effects indicated a lower MABP at 88, 118, and 148 min compared with steady-state control conditions for both groups (p< 0.0018). Heart rate (not shown) was similar between groups during steady-state control conditions, increased comparably during ischemia, but was 25-30 beats/min lower in the modest hypothermia group compared with the normothermia group during postischemia, resulting in a group effect(p = 0.008). Arterial pH was similar between groups, and values at the completion of postischemia did not differ from steady-state control. Arterial Pco2 was similar between groups, but values at the completion of ischemia were moderately decreased from steady-state control (4.7 ± 0.4 versus 4.0 ± 0.7, and 4.4 ± 0.2 versus 3.8 ± 0.5 kPa for normothermic and hypothermic control versus ischemia, p < 0.0024). Arterial Po2 remained above 13 kPa throughout the study for both groups. Arterial lactate and glucose concentration (data not shown) did not differ between groups with similar increases (5 and 10 mM for lactate and glucose, respectively) during ischemia and decreases toward steady-state control values during the 90-min postischemia interval.
Representative 31P MR spectra before, during, and after ischemia are illustrated in Figure 3. Spectral characteristics between groups appeared comparable at steady-state control conditions as indicated by ratios of resonance peak heights (PCr/β-NTP; 1.45 ± 0.13versus 1.53 ± 0.28, and Pi/β-NTP; 1.29 ± 0.11 versus 1.33 ± 0.13 for normothermic versus hypothermic, respectively). Quantitation of changes during and after ischemia(Table 1) revealed no differences between groups for pHi or phosphorylated metabolites for any of the intervals studied. Trends toward group effects were present for β-NTP (p = 0.066) and phosphocreatine (p = 0.086) reflecting small but consistently higher values for the hypothermic group during postischemia. Comparison of the total areas of spectra before and after ischemia did not differ within each group, indicating no net loss of phosphates from brain.
Representative spectra were acquired from a modestly hypothermic piglet and represent data collected during control(bottom), over the last 7.5 min of ischemia (middle), and at the completion of postischemia (top). The horizontal axis represents chemical shift in parts per million (ppm) and the vertical axis represents resonance intensity. Spectra from ischemia and postischemia are offset from the control spectra and chemical shift axis. Seven resonance peaks are identifiable at control: phosphomonoester(PME), inorganic phosphorus (Pi), phosphodiester(PDE), PCr, and γ, α, and β peaks of NTP. During ischemia there was an increase in Pi, decreases in PCr and NTP, and a down field shift in Pi. Changes associated with ischemia were largely resolved by the completion of the postischemic interval.
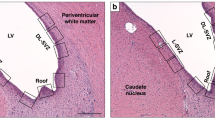
Follow-up assessments on the days after ischemia revealed stable physiologic parameters and no differences between groups. MABP at 24, 48, and 72 h postischemia was 74 ± 16, 76 ± 8, and 70 ± 20 mm Hg for normothermic animals, and 77 ± 9, 73 ± 7, and 82 ± 18 mm Hg for hypothermic piglets. Arterial pH values at the same time intervals were 7.48 ± 0.05, 7.45 ± 0.02, and 7.46 ± 0.03 compared with 7.48 ± 0.03, 7.48 ± 0.03, and 7.46 ± 0.03 for normothermic and hypothermic groups, respectively. The maximal overall performance score for each group (Table 2) indicated that piglets subjected to 1 h of hypothermia immediately after brain ischemia had less severe stages of encephalopathy compared with piglets maintained normothermic. Six animals died before completing the 72-h postischemic interval (normothermic n = 4, hypothermic n = 2). Death occurred 24 h after ischemia in four piglets, and 48 h postischemia in the remaining two piglets; five were severely encephalopathic, and one was moderately encephalopathic (hypothermic). Hypothermic piglets had less severe histologic grades of neuronal injury in the temporal and occipital cortex 10 mm beneath the cortical surface compared with normothermic animals (Fig. 4). Although there were no differences between groups for cortex at 5 mm beneath the cortical surface, the direction of effect for all regions favored less neuronal injury in hypothermic animals. Hypothermic animals also had less neuronal injury in the caudate nucleus(p = 0.038), but there were no group differences in the hippocampus(p = 0.14), thalamus (p = 0.12), midbrain (p = 0.38), and cerebellum (p = 0.12). Damage to the pons and medulla was limited to a cluster of ischemic neurons (grade II) in the pons of one normothermic animal and a grade II lesion in the medulla of a second normothermic piglet. The overall performance score positively correlated with a composite score of the histologic grade (cumulative sum of grades for 16 regions scored) for both groups combined (r = 0.67, p = 0.024).
Histologic grades of cortical regions are plotted for normothermic and hypothermic neonatal swine (closed and open symbols, respectively) within axial sections at depths of 5 and 10 mm beneath the cortical surface. Each symbol represents a different animal. Group comparisons are indicated by the p values.
DISCUSSION
The results of this investigation demonstrate that a reduction in brain temperature of 2-3 °C in neonatal swine initiated immediately after partial global brain ischemia is associated with partial neuroprotection. Both groups were comparable in age and weight at the time of the experiment, and there were no differences between groups in any physiologic or brain metabolic variables before or during ischemia. Partial neuroprotection was substantiated by both clinical neurologic assessment and neuronal histology, the latter being conducted in a blinded fashion. Differences in the extent of ischemic neuronal changes were present in the temporal and occipital cortex at a depth of 10 mm beneath the cortical surface, and in the caudate nucleus.
In evaluating the efficacy of modest hypothermia as a neuroprotective strategy for resuscitation, three critical variables are the time of initiation, the duration, and the extent of hypothermia. Experiments in the present investigation were designed to assess immediate implementation of hypothermia and verified that brain temperature was lowered by 2-3 °C within 5-10 min of the termination of ischemia (Fig. 1). A number of studies using adult animals have examined the effect of different intervals of postischemic normothermic recirculation before initiating hypothermia(9, 21, 22). All demonstrate that postischemic hypothermia is of greatest benefit in attenuating the extent of brain injury when initiated immediately postischemia, and efficacy decreased with an increasing time interval of initiation postischemia. Of equal importance to the time of initiation is the duration of hypothermia. In adult gerbils the percent of CA-1 neurons protected after global cerebral ischemia increased as the duration of immediate postischemic hypothermia was extended from 30 min to 4 h(9). Other studies have demonstrated that increasing the duration of postischemic hypothermia from 12 to 24 h provided greater neuroprotection for hippocampal CA-1 neurons(23). Similarly modest hypothermia initiated immediately after hypoxia-ischemia in 21-d-old rats decreased the frequency and extent of cortical infarction if the interval of hypothermia was 72 h compared with a 6-h regimen or normothermic conditions(24). The extent of brain temperature reduction in the context of modest hypothermia represents a variable which has received little systematic evaluation when ischemic condition, time of initiation, and duration of ischemia are standardized. Only in adult gerbils has there been a comparison of 24 h of hypothermia using 32 or 34 °C initiated 1 h after 5 min of ischemia(25). Both hypothermic regimens provided partial neuroprotection for CA-1 neurons evident by clinical performance and histologic evaluation, and the extent of protection was greater at the lower temperature.
Our decision to employ a 2-3 °C temperature reduction for a 1-h interval immediately after ischemia reflects specific considerations for the care of newborns. The adverse effects of exposure to environmental temperatures below that required for maintenance of a neutral thermal environment has been studied, with results showing an increase in O2 consumption(26, 27). The increase in O2 consumption is responsible for nonshivering thermogenesis, which is accompanied by multiple biochemical changes reflecting attempts to meet increased metabolic demands. The latter potentially includes elevation of lactate with a resultant base deficit(28), hypoglycemia(29), and increases in nonesterified fatty acids(30) and glycerol(31). Norepinephrine has been suggested as the putative mediator of chemical thermogenesis(32), and release of vasoactive compounds such as norepinephrine may account for the observed reduction in arterial O2 tension associated with cold exposure via alterations in pulmonary vascular resistance(33). Evaluation of different ambient temperatures in the care of premature infants during the first 5 d of life indicated that survival is favorably influenced by environments that reduce heat loss(34). Thus, in spite of the evidence that longer durations and greater degrees of modest hypothermia are more efficacious than shorter intervals, we purposely designed a hypothermic regimen that minimized the extent and duration of temperature reduction given the adverse effects of cold exposure in neonates. Even limited exposure to modest reduction in temperature in this study resulted in a lower heart rate compared with that of animals maintained normothermic. This presumably reflects temperature-induced reductions in metabolic rate, which are directly correlated with heart rate(35). Whether a specific hypothermia regimen is of net therapeutic benefit after ischemia or hypoxia-ischemia will ultimately reflect a balance between observed neuroprotection and the hazards from the metabolic/hormonal derangements associated with cold exposure.
The precise mechanism by which modest hypothermia provides neuroprotection remains unclear. When used in a protective strategy small reductions in temperature moderate multiple cellular events that may contribute to the observed reduction of brain damage. Examples of the latter include attenuation of the release of excitatory neurotransmitters(36), depression in protein synthesis(37), extent of brain acidosis(4), rate of energy utilization(19), and free radical production(38, 39). The contribution of these processes to the neuroprotection associated with modest hypothermia used for resuscitation has received little attention. Alternatively, the benefit of modest hypothermia may emanate from avoiding deleterious effects of postischemic hyperthermia that have been observed in some animal models(40). Our preliminary data (Fig. 1) did not suggest that hyperthermia in the first 90 min postischemia was relevant to our partial ischemia model in neonatal swine. The results of this investigation indicate that immediate postischemic modest hypothermia does not attenuate the extent or duration of brain acidosis compared with normothermic animals. In addition there were no differences between groups in relative concentrations of phosphorylated metabolites as indicated by peak height analysis, although there are trends for group effects for β-NTP and PCr. Anesthetic and analgesic agents may have neuroprotective properties. However, pentothal for intubation, N2O for anesthesia, nalbuphine for analgesia, and vecuronium for immobilization were chosen for either their short duration of action (pentothal), or their relative lack of effect on cerebral blood flow and metabolism(41). It seems doubtful that these medications interact with hypothermia and contribute to the observed neuroprotection.
These results demonstrating that a short interval of modest hypothermia initiated immediately after ischemia provides partial neuroprotection raise the possibility that brief temperature manipulation may represent a beneficial adjunct to other potential resuscitative therapies in clinical practice. Delivery room resuscitation may represent the ideal circumstance to evaluate modest hypothermia for neonates, given the ease of inducing temperature reductions in this setting(42). The efficacy of modest hypothermia as a protective and immediate resuscitative strategy is ideal for delivery room stabilization because it is unclear at birth if a hypoxic-ischemic interval has previously occurred, or whether difficulty in the fetal to neonatal transition results in an immediate postnatal hypoxic-ischemic event. These experiments were conducted in animals with a mean postnatal age of 9 d, and extrapolation to conditions at birth needs to be tempered because brain injury mechanisms may change with development. The results of the current investigation clearly justify further investigation of modest hypothermia. Evidence that a short period of 2-3 °C temperature reduction confers neuroprotection when initiated at some interval after ischemia would further enhance the clinical utility of this resuscitative strategy.

Abbreviations
- MABP:
-
mean arterial blood pressure
- MR:
-
magnetic resonance
- pHi:
-
intracellular pH
- PCr:
-
phosphocreatine
- Pi:
-
inorganic phosphorus
- NTP:
-
nucleoside triphosphate
- OPS:
-
overall performance score
References
Bigelow WG, Lindsay WK, Greenwood WF 1950 Hypothermia, its possible role in cardiac surgery: an investigation of factors governing survival in dogs at low body temperatures. Ann Surg 13: 849–866.
Busto R, Dietrich WD, Globus MY-T, Valdes I, Scheinberg P, Ginsberg MD 1987 Small differences in intraischemic brain temperature critically determine the extent of ischemic neuronal injury. J Cereb Blood Flow Metab 7: 729–738.
Ginsberg MD, Sternau LL, Globus MY-T, Dietrich WD, Busto R 1992 Therapeutic modulation of brain temperature: relevance to ischemic brain injury. Cerebrovasc Brain Metab Rev 4: 189–225.
Ikonomidou C, Mosinger JL, Olney JW 1989 Hypothermia enhances protective effect of MK801 against hypoxic-ischemic brain damage in infant rats. Brain Res 487: 184–187.
Yager J, Towfighi J, Vannucci RC 1993 Influence of mild hypothermia on hypoxic-ischemic brain damage in the immature rat. Pediatr Res 34: 525–529.
Laptook AR, Corbett RJT, Sterett R, Burn DK, Tollefsbol G, Garcia D 1994 Modest hypothermia provides partial neuroprotection for ischemic neonatal brain. Pediatr Res 35: 436–442.
Busto R, Dietrich WD, Globus MY-T, Ginsberg MD 1989 Post-ischemic moderate hypothermia inhibits CA1 hippocampal ischemic neuronal injury. Neurosci Lett 101: 299–304.
Chopp M, Chen H, Dereski MO, Garcia JH 1991 Mild hypothermic intervention after graded ischemic stress in rats. Stroke 22: 37–43.
Carroll M, Beek O 1992 Protection against hippocampal CA1 cell loss by postischemic hypothermia is dependent on delay of initiation and duration. Metab Brain Dis 7: 45–50.
Weinrauch V, Safar P, Tisherman S, Kuboyama K, Radovsky A 1992 Beneficial effect of mild hypothermia and detrimental effect of deep hypothermia after cardiac arrest in dogs. Stroke 23: 1454–1462.
Welsh FA, Harris VA 1991 Post-ischemic hypothermia fails to reduce ischemic injury in gerbil hippocampus. J Cereb Blood Flow Metab 11: 617–620.
Chen H, Chopp M, Vande Linde AMQ, Dereski MO, Garcia JH, Welch KMA 1992 The effects of post-ischemic hypothermia on the neuronal injury and brain metabolism after forebrain ischemia in the rat. J Neurol Sci 107: 191–198.
Thoresen M, Bagenholm R, Loberg EM, Apricena F, Kjellmer I 1996 Post-hypoxic cooling of neonatal rats provides protection against brain injury. Arch Dis Child 74:F3–F9.
Tuor UI, Del Bigio MR, Chumas PD 1996 Brain damage due to cerebral hypoxia-ischemia in the neonate: pathology and pharmacological modification. Cerebrovasc Brain Metab Rev 8: 159–193.
Laptook AR, Corbett RJT, Burns D, Sterett R 1995 Neonatal ischemic neuroprotection by modest hypothermia is associated with attenuated brain acidosis. Stroke 26: 1240–1246.
Leonov Y, Sterz F, Safar P, Radovsky A, Oku K, Tisherman S, Stezoski SW 1990 Mild cerebral hypothermia during and after cardiac arrest improves neurologic outcome in dogs. J Cereb Blood Flow Metab 10: 57–70.
Corbett RJT, Laptook AR, Nunnally RL 1987 The use of the chemical shift of the phosphomonoester P-31 magnetic resonance peak for the determination of intracellular pH in the brain of neonates. Neurology 37: 1771–1779.
Kost GJ 1990 pH standardization for phosphorus-31 magnetic resonance heart spectroscopy at different temperatures. Magn Reson Med 14: 496–506.
Laptook AR, Corbett RJT, Sterett R, Garcia D, Tollefsbol G 1995 Quantitative relationship between brain temperature and energy utilization rate measured in vivo using 31P and 1H magnetic resonance spectroscopy. Pediatr Res 38: 919–925.
Laptook AR, Corbett RJT, Ruley J, Olivares E 1992 Blood flow and metabolism during and after repeated partial brain ischemia in neonatal piglets. Stroke 23: 380–387.
Rosomoff HL, Shulman K, Raynor R, Grainger W 1960 Experimental brain injury and delayed hypothermia. Surg Gynecol Obstet 110: 27–32.
Coimbra C, Wieloch T 1994 Moderate hypothermia mitigates neuronal damage in the rat brain when initiated several hours following transient cerebral ischemia. Acta Neuropathol 87: 325–331.
Colbourne F, Corbett D 1994 Delayed and prolonged post-ischemic hypothermia is neuroprotective in the gerbil. Brain Res 654: 265–272.
Sirimanne ES, Blumberg RM, Bossano D, Gunning M, Edwards AD, Gluckman PD, Williams CE 1996 The effect of prolonged modification of cerebral temperature on outcome after hypoxic-ischemic brain injury in the infant rat. Pediatr Res 39: 591–597.
Colbourne F, Corbett D 1995 Delayed postischemic hypothermia: a six month survival study using behavioral and histological assessments of neuroprotection. J Neurosci 15: 7250–7260.
Bruck K 1961 Temperature regulation in the newborn infant. Biol Neonate 3: 65–119.
Hey EN 1969 The relation between environmental temperature and oxygen consumption in the newborn baby. J Physiol 200: 589–603.
Gandy GM, Adamsons K, Cunningham N, Silverman WA, James LS 1964 Thermal environment and acid base homeostasis in human infants during the first few hours of life. J Clin Invest 43: 751–758.
Cornblath M, Schwartz R 1976 Hypoglycemia associated with neonatal cold injury. In: Disorders of Carbohydrate Metabolism in Infancy. WB Saunders, Philadelphia, pp 166–167.
Schiff D, Stern L, Leduc J 1966 Chemical thermogenesis in newborn infants: catecholamine excretion and the plasma non-esterified fatty acid response to cold exposure. Pediatrics 37: 577–582.
Perlstein PH, Hersh C, Glueck CJ, Sutherland JM 1974 Adaptation to cold in the first three days of life. Pediatrics 54: 411–416.
Stern L, Lees MH, Leduc J 1965 Environmental temperature, oxygen consumption, and catecholamine excretion in newborn infants. Pediatrics 36: 367–373.
Stephenson JM, Du JN, Oliver TK 1970 The effect of cooling on blood gas tensions in newborn infants. J Pediatr 76: 848–852.
Silverman WA, Fertig JW, Berger AP 1958 The influence of the thermal environment upon the survival of newly born premature infants. Pediatrics 22: 876–885.
Chessex P, Reichman BL, Verellen GJE, Putet G, Smith JM, Heim T, Swyer PR 1981 Relation between heart rate and energy expenditure in the newborn. Pediatr Res 15: 1077–1082.
Busto R, Globus MY-T, Dietrich D, Martinez E, Valdes I, Ginsberg MD 1989 Effect of mild hypothermia on ischemia-induced release of neurotransmitters and free fatty acids in rat brain. Stroke 20: 904–910.
Bergstedt K, Hu BR, Wieloch T 1993 Postischemic changes in protein synthesis in the rat brain: effects of hypothermia. Exp Brain Res 95: 91–99.
Armstead WM, Mirro R, Busija DW, Leffler CW 1988 Postischemic generation of superoxide anion by newborn pig brain. Am J Physiol 255:H401–H403.
Dempsey RJ, Combs DJ, Maley ME, Cowen DE, Roy MW, Donaldson DL 1987 Moderate hypothermia reduces postischemic edema development and leukotriene production. Neurosurgery 21: 177–181.
Kurowa T, Bonnekoh P, Hossmann KA 1990 Prevention of postischemic hyperthermia prevents ischemic injury of CA-1, neurons in gerbils. J Cereb Blood Flow Metab 10: 550–556.
Smith AL, Wollman H 1972 Cerebral blood flow and metabolism: effects of anesthetic drugs and techniques. Anesthesiology 36: 378–400.
Dahm LS, James LS 1972 Newborn temperature and calculated heat loss in the delivery room. Pediatrics 49: 504–513.
Author information
Authors and Affiliations
Additional information
Supported by the United Cerebral Palsy Research and Educational Foundation, Inc., the Southwestern Biomedical Magnetic Resonance Facility National Institutes of Health Grant P41-RR02584 and the Department of Pediatrics, UT-Southwestern Medical Center at Dallas.
Rights and permissions
About this article
Cite this article
Laptook, A., Corbett, R., Sterett, R. et al. Modest Hypothermia Provides Partial Neuroprotection when Used for Immediate Resuscitation after Brain Ischemia. Pediatr Res 42, 17–23 (1997). https://doi.org/10.1203/00006450-199707000-00004
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199707000-00004
This article is cited by
-
Early assessment of injury with optical markers in a piglet model of neonatal encephalopathy
Pediatric Research (2023)
-
Therapeutic hypothermia translates from ancient history in to practice
Pediatric Research (2017)
-
Brain Energy Metabolism During Experimental Neonatal Seizures
Neurochemical Research (2010)
-
Effect of post-ischemic hypothermia on spinal cord damage induced by transient ischemic insult in rabbits
The Japanese Journal of Thoracic and Cardiovascular Surgery (2002)