Abstract
Study design:
Controlled, repeat-measures study.
Objectives:
To determine if functional electrical stimulation (FES) can affect bone atrophy in early spinal cord injury (SCI), and the safety, tolerance and feasibility of this modality in bone loss remediation.
Setting:
Spinal Injuries Units, Royal Adelaide Hospital and Hampstead Rehabilitation Centre, South Australia.
Methods:
Patients with acute SCI (ASIA A–D) were allocated to FES (n=23, 28±9 years, C4–T10, 13 Tetra) and control groups (CON, n=10, 31±11 years, C5–T12, four Tetra). The intervention group received discontinuous FES to lower limb muscles (15 min sessions to each leg twice daily, over a 5-day week, for 5 months). Dual energy X-ray absorptiometry (DEXA) measured total body bone mineral density (tbBMD), hip, spine BMD and fat mass (FM) within 3 weeks, and 3 and 6 months postinjury.
Results:
FES and CON groups' tbBMD differed significantly at 3 months postinjury (P<0.01), but not thereafter. Other DEXA measures (hip, spine BMD, FM) did not differ between groups at any time. No adverse events were identified.
Conclusion:
Electrically stimulated muscle activation was elicited, and tetanic effects were reproducible; however, there were no convincing trends to suggest that FES can play a clinically relevant role in osteoporosis prevention (or subsequent fracture risk) in the recently injured patient. The lack of an osteogenic response in paralysed extremities to electrically evoked exercise during subacute and rehabilitation/recovery phases cannot be fully explained, and may warrant further evaluation.
Similar content being viewed by others
Introduction
Electrical stimulation has a long history in the diagnosis1, 2, 3 and treatment of disorders4, 5, 6 of the central nervous system. The application of this physical modality in the rehabilitation of people with spinal cord injury (SCI) has been extensively studied as a ‘functional therapy’.4, 5, 6, 7 Clinical and experimental studies indicate that neuromuscular electrical stimulation can both affect and effect changes in muscle fibre contractile properties4, 8 and metabolism,9, 10 as well as responses at physiological5, 6 and functional levels. Although well studied,7, 11, 12, 13 there is conflicting evidence about the efficacy of electrically evoked muscle activation in the stimulation of bone metabolism (bone formation and/or reduction of bone loss), and the clinical role of functional electrical stimulation (FES) in the treatment of osteoporosis resulting from neurological damage. The reason for this conflict may be that bone metabolic abnormalities may be time dependent14, 15, 16 or as-yet-unexplained factors affect the osteogenic response to mechanical strain. Alternatively, as it is well known that exercise-induced bone effects are mode and dose dependent, and the exercise modes or doses used and/or tolerated by the patient with SCI may have been subtherapeutic.
Fracture, and bone densitometry data suggest that early bone loss interventions will be required to prevent SCI osteoporosis.17, 18, 19, 20 Dual energy X-ray absorptiometry (DEXA) (research based and clinical) confirms a rapid decline in lower extremity bone mineral density (BMD) in the initial 6 to 18 months after injury, resulting in osteopenia and susceptibility for fracture.17, 18, 21 Preliminary data suggest that antiresorptive agents (aminobisphosphonates) may ameliorate SCI bone loss.22, 23, 24 However, there are still many clinical uncertainties about the optimal time for the initiation of bone loss prevention protocols, and appropriate avenue(s) for early remediation.
This study aimed to explore the use of FES in the first 6 months following acute SCI, and its potential to alter the well-described course of postinjury bone loss. The data were examined in two phases: acute/subacute (3–12 weeks), and rehabilitation/recovery (3–6 months). The discontinuous FES protocol was safe and well tolerated; however, the low-intensity exercise intervention showed limited potential to delay or prevent bone loss, as measured by DEXA.
An apparent lack of therapeutic efficacy may be explained by protocol inadequacies, or Type 2 error due to low statistical power, or the limited period of observation. A discrepancy between the postulated and observed responses to exercise may also be attributed to technical, or physiological limitations to electrically evoked muscle activation (small amount of muscle mass, axonal degeneration, contractile properties). Further study may be required to explore the underlying mechanisms of SCI bone loss in acute/subacute and recovery phases, and clinically relevant avenues for early intervention.
Methods
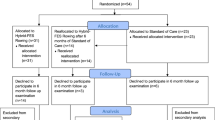
Study design
The study was performed using a nonrandomised, controlled, repeat-measures design.
Methodology
Blinding was rejected for two reasons. Firstly, the electrical stimulus elicits obvious muscle contraction, which cannot be replicated by a ‘placebo’ device. Secondly, there were ethical concerns about intervention and nonintervention patients receiving treatment (or denial of perceived benefit) at the same time in the rehabilitation setting. As a result, intervention and control (CON) groups were enrolled nonconsecutively.
Subject selection
In all, 33 patients were recruited from acute admissions to the Spinal Injuries Unit of the Royal Adelaide Hospital (SIU) between 1997 and 2001. Male and female patients aged 18–55 years with a spinal cord lesion above L1 were eligible for participation. Patients with a deteriorating neurological condition, known osteoporosis, associated lower limb or pelvic fracture(s), medical condition(s) influencing bone metabolism and/or medical contraindications to exercise were excluded. Table 1 shows demographic, injury (lesion) and functional data by study group (FES: n=23; CON: n=10; aged 28.6±9 and 31±11 years, respectively, at arrival). These patients were transferred to the SIU, either directly from the site of injury or via an initial assessment facility, arriving within 2 days of sustaining their injury. Methylprednisolone was administered according to the acute SCI protocol25 and all patients were anticoagulated initially. At 3 weeks postinjury, maximal intensity electrical stimulation tests were performed at quadriceps femoris and anterior tibial motor points to ascertain whether a 30 Hz frequency could evoke tetanic muscle contraction (see below – FES protocol). Patients who satisfied FES stimulation response criteria entered the study.
FES protocol
Electrical stimulation was applied using Respond SELECT stimulators (Empi Inc., Saint Paul, MN, USA), and delivered via surface electrodes (Empi Inc., Axelgaard, Denmark). Electrodes were applied unilaterally at quadriceps femoris and anterior tibial motor points. Blood pressure (BP), heart rate (HR) and O2 saturation (saO2) were monitored (504 US Pulse Oximeter; Criticare Systems) at pretreatment, and during FES application and postexercise sessions during the first 2 weeks of the protocol.
After a 2-week preconditioning period, isotonic, unresisted, inner range quadriceps and ankle dorsiflexor repetitions were performed with a stimulation:rest ratio 4:8 s. The unilateral exercise protocol was performed for 15 min; the procedure then was repeated at the other limb. Patients performed two 15-min FES exercise sessions per limb per day, over a 5-day week, with the limb supported at the knee in 20° flexion, and the patient positioned in a semirecumbent, supine position. A physiotherapist recorded the weekly cumulative exercise sum.
Measurement protocol
Apparatus
BMD measurements were performed using DEXA (GE-Lunar Expert XL, Lunar Corp, Madison, WI, USA). System precision was monitored on a weekly basis using an aluminium spine phantom. Reproducibility was estimated as between 1 and 2% throughout the study period (4 years in total). Coefficient of variability (CV) was estimated as 0.5% for total body BMD, 2% at the hip and 4% at the spine. Total radiation burden to participants was very small (approximately 0.2 uSv). Scans were analysed using Expert 1.92 software by an operator (CS) who was blinded to the protocol.
Measurement parameters
BMD measurements were taken for the total body, lower extremity region, and anteroposterior (AP) lumbar spine (L2–4), femoral neck and proximal femur. The left limb was selected as the preferred side for measurement; laterality was rejected as a confounding variable. Measures were performed at entry (within 3 weeks postinjury), 6 weeks, and 3 and 6 months postinjury.
Clinical measures
Protocol adherence (PA) was calculated as the percentage of cumulated exercise sum (hours per week) from a maximum of two and a half hours per week. Retention to study, reasons for attrition and complication frequency were also determined. The Functional Independence Measure (FIM™)26 and ASIA motor scores27 were obtained at hospital discharge.
Analyses
The ‘intention to treat’ principle was applied. As bone complications, for example, heterotopic ossification, scoliosis, osteomyelitis, arthroses, internal fixation of bone, can influence DEXA precision,28, 29 International Society for Clinical Densitometry (ISCD) scan artefact criteria were applied and scans were extracted accordingly (periarticular hip artefact n=5, two FES, three CON). Percentage change (%) BMD was derived from baseline BMD (g/cm2) and % fat mass (FM) from total body mass (g). Analysis was performed using the Statistical Software for Social Scientists (SPSS) Base 11.5 version. Student's t-tests (two-tailed) were applied at each data point to test for between-group effects. A probability of P<0.05 was taken as statistically significant.
Results
Recruitment and retention
We recruited 33 male and female patients from acute admissions to the SIU 1997–2001. A further 44 eligible candidates declined invitation to take part. Table 1 shows patient characteristics by study group. The average age of FES and CON groups did not differ significantly at admission (FES 28.6±8.6 years, CON 31.0±10.7). Although males were over-represented, the male to female ratio in each group was essentially the same (CON 11:1, FES 10:1). PA together with bone complications accounted for similar within-group attrition (PA FES 17%, CON 13%; complication FES 17%, CON 10%).
In the FES group, four patients were withdrawn owing to medical complications unrelated to the exercise regime, and three for protocol violation (PA). In the CON group, one patient was withdrawn owing to a medical complication, and two noncompliance (PA) with ward protocols. Bone complications did not show apparent group trends (heterotopic ossification (n=5; two FES, three CON), osteomyelitis (n=1; one FES, zero CON) and hypercalcaemia (n=1; one FES, zero CON)).
Stimulation response
The low-intensity (bi-daily) FES exercise protocol was tolerated acutely and well accepted during physical rehabilitation. Patients demonstrated brisk FES-evoked muscle tetany while still showing clinical evidence of spinal shock. Pretreatment, treatment and postexercise observations confirmed that physiological parameters (HR, BP and O2 saturation) remained within medically acceptable ranges. All patients achieved the target exercise interval of 15 min per limb per session within 2 weeks of commencing the FES protocol. Relatively few problems were encountered with skin irritation or muscle trauma (one patient developed a small haematoma that resolved with rest). No serious medical complications were attributed directly to the stimulation protocol or study participation.
Patients averaged 3 h of exercise per week (range 1–5 h per week, or completed 61% of scheduled sessions) throughout their admission. Although all patients with tetraplegia were hospitalised for the study duration (6 months), most with thoracic lesions were discharged (the mean length of stay was 17 weeks). After discharge, two FES subjects withdrew owing to time commitments and another was lost to follow-up.
Bone mineral density
Table 2 shows BMD data for CON and FES groups as percentage change from study baseline. A significant difference was identified between CON and FES groups' total body BMD at the subacute 3-month point (P<0.01), but this early trend did not persist. No between-group differences were identified in lower extremity or hip BMD at the 3- or 6-month points. CON and FES groups lost −4.7±2.7 versus −7.1±3.1%, respectively, of their lower extremity BMD, in the first 6 months of injury (P>0.05). Similar trends were seen at the hip during the same period (CON BMD −8.4±7.6 and FES −10.8±4.6%, P>0.05).
Body fat and lean mass
Table 2 also shows total FM and regional FM for CON and FES groups. Total FM did not significantly differ between FES and CON groups at acute/subacute, or rehabilitation/recovery sample points (at the 6-month point, CON FM 2±9 versus FES 6±6%, P>0.05). Furthermore, although DEXA cannot discriminate intraosseous and extraosseous fat fractions, no significant differences were identified between groups' regional FM (at the 6 month point lower extremity CON FM 6±9% and FES 8±7%, P>0.05). As total body water (TBW) content can vary postinjury, variations in fluid load may affect DEXA LBM and DEXA lean body mass (LBM) estimates include TBW, analysis of LBM data was not meaningful.
Discussion
Pathological fracture risk in the SCI population has directed clinical attention towards fracture diagnostic thresholds, and avenues for osteoporosis prevention22, 30, 31 and treatment.7, 12, 13, 23, 32 Physical modalities (standing, FES cycle ergometry,11, 12, 13 vibration32, 33) and pharmacological agents (amino-bisphosphonates22, 23, 24) have been proposed as measures to slow the rapid loss of lower extremity bone after SCI. Although research data for patients with chronic SCI12, 13 suggest that FES could play an adjunctive role in the early clinical management of SCI bone loss, relatively few studies have evaluated the safety or efficacy of FES in the patient recently injured.30 Furthermore, very little is known about bone responses to exercise stress during the clinically relevant SCI acute/subacute and rehabilitation/recovery phases, and if these responses are time, dose or mode dependent.
Uncertainties about the optimal time for the implementation of bone loss prevention protocols, and the appropriate treatment modality after SCI represents a problem for the clinician tasked with determining ‘best practice’ in rehabilitation medicine. As the implementation of physical modalities can be resource intensive, cost–benefits and effective resource allocation (time and equipment) in the rehabilitation and community setting are also a consideration. This study aimed to address clinical uncertainties about the role of physical modalities in the management of early SCI bone loss, by determining its potential to affect bone atrophy in acute/subacute or rehabilitation/recovery phases; and the therapeutic safety, tolerance and feasibility of this modality in bone loss remediation.
Therapeutic safety and tolerance of lower limb FES during acute/subacute SCI or rehabilitation/recovery
As determined clinically and by physiological measures, the low-intensity FES protocol was well tolerated by patients with early SCI. No problems were encountered, in relation to adverse physiological effects, or tissue trauma in proximity to the electrode interface. Study retention was similar in CON and FES groups, as well as reasons given for attrition. Taken together, these data suggest that FES is well tolerated by patients with early SCI and that it can be applied to condition recently paralysed muscle groups. As muscle conditioning is time dependent,4, 34 there was a delay between initiation of the FES regime and attainment of a relatively modest cumulative exercise sum. Muscle atrophy,8 together with the relatively small amount of muscle mass activated by surface FES protocols4 and hypothalamic-pituitary-axis abnormalities,35, 36, 37 may interact with residual potential for clinically relevant muscle hypertrophy, required for therapeutic efficacy.
Feasibility of lower limb FES as a treatment modality within a rehabilitation programme
Physiological efficacy was substantiated in the phase of spinal shock, thus identifying lesion level (below T12) as the definitive contraindication for clinical FES applications. As the FES protocol was standardised to physiological tolerance in early SCI, intensity, mode (addition of resistance, loading, incremental exercise) and cycle ergometry protocols were not explored. Additionally, ‘novel’ stimulation frequencies,32, 38 physical modalities and pharmacotherapies with osteogenic potential outside the exercise physiology window were not explored. Although the FES-elicited muscle activation pattern was reproducible, an effect sustained in acute/subacute or rehabilitation/recovery phases, potential for ‘habituation’39, 40 to the 30 Hz frequency cannot be ruled out. As shown by compliance statistics, the exercise protocol was well tolerated and integrated into acute and rehabilitation settings. Thus, clinical observations suggest that FES is a feasible treatment modality within a rehabilitation programme; but study data do not support the application of FES in early bone loss remediation, at least not as a single modality.
Potential for lower limb FES to interact with clinical outcomes
Differences in spontaneous recovery and active physical rehabilitation prevented meaningful analysis of the clinical and functional data. However, there was an impression of clinical benefit in the intervention group. The introduction of a ‘placebo stimulus’ was rejected owing to the obvious nature of FES intervention, and the placebo effects of exercise regimes per se.41, 42 Thus, any perception of well being or benefit derived from FES application may be attributed to a ‘placebo effect’.42 Alternatively, perception of benefit may be attributed to social participation41, 42 (opportunities for social interaction or additional clinical attention). As there was also an impression of contrary effects within the CON group (adjustment to injury, possibly explained by a perception of denial of a therapeutic benefit), these preliminary observations suggest that unblinded research in the rehabilitation setting (but not necessarily the FES protocol per se) may interact with the well being of the recently injured patient.
Potential for lower limb FES to affect postinjury bone atrophy
A hip BMD decline of −8.5 and −11% during the first 6 months postinjury in CON and FES groups, respectively, illustrates the relatively low potential for FES exercise to alleviate the early bone atrophy. These DEXA data are in agreement with the annualised hip BMD data reported by cross-sectional studies.17 Several studies12, 13 suggest that FES-evoked repetitive contractions can promote bone adaptation at sites of muscle attachments/insertions, in patients with established osteoporosis. The BMD of the proximal tibia, distal femur and cortical diaphysis were not measured in our study, an acknowledged limitation of commercially available DEXA software. However, although physiologically significant, it is unclear whether small focal BMD increments in response to FES are clinically relevant to fracture prevention. Studies of FES effects upon other bone strength properties (bone size, geometry, architecture) and clinical end points such as SCI fracture frequency and distribution43, 44, 45, 46 may resolve this question.
Effects of fat mass and lean mass upon BMD measures
Although the total body fat mass of both CON and FES groups increased postinjury, there was no evidence that the FES exercise protocol protected participants against fatty involution. Thus, between-group differences in total BMD at 12 weeks postinjury could not be attributed directly to differences in weight loss or gain. Furthermore, there was no indication in these SCI groups of a mechanistic effect in which body fat protects against bone atrophy, as suggested by data for ambulant cohorts.
The DEXA CV for BMD in sites of interest in our study was very low. However, it has been suggested that soft-tissue variation and disproportionate marrow fat fractions47 may increase DEXA's potential for systematic measurement inaccuracies. Although changes to apparent soft-tissue densities39, 48, 49 and marrow constituents are known to occur during the acute/subacute injury phases, FM and BMD did not differentiate FES and CON groups at either subacute or rehabilitation/recovery points. Ex vivo study would be required to determine the potential for systematic DEXA measurement errors to explain these results. DEXA's proven track record was considered from aspects of patient radiation safety and likelihood of ethics approval. As DEXA measurement of bone mineral density is noninvasive, highly reproducible, and radiation dose is low, it was selected in preference to computed tomography (CT). Peripheral quantitative computed tomography (pQCT) was not available, but portable densitometers may offer a means to explore the natural history of bone loss in acute/subacute or rehabilitation/recovery phases.
Effects attributed to pharmacotherapies and motor recovery
Experimental and clinical evidence shows that glucocorticoid exposure has effects upon bone strength; however, it is also known that the magnitude of that effect is dependent on the dose and duration of therapy. Although it is unlikely that transient exposure to methylprednisolone (MP) has clinically significant implications for bone atrophy, the acute intravenous MP protocol may be responsible for corticosteroid myopathy.50 Peripheral nerve damage as a complication of SCI may have implications for muscle activation in the acute/subacute phase of this evaluation. However, patients with absent or inadequate muscle responses to maximal FES stimulation did not enter the study. Quadriceps muscle torque and force–length relationships were not measured (by strain gauge). Although a study by Gerrits et al39 indicates reliability for ‘hand-held’ dynamometers in the evaluation of FES-evoked muscle contractile properties (contractile speed, tetanic tension, fatigue resistance), this technique was validated after the commencement of study. As both FES and CON groups were representative of acute SCI admissions (ASIA A–D), recovery-dependent differences in quadriceps muscle torque and force–length relationships do not fully explain the failure to differentiate between-group effects at acute/subacute or rehabilitation/recovery measurement points that may be attributed to the exercise protocol.
Summary of FES effects upon BMD
Our standardised FES protocol showed low therapeutic efficacy to alleviate bone loss during the critical early window for prevention. Although this apparent lack of therapeutic efficacy may be explained by Type 2 error or protocol inadequacies, the discrepancy between the postulated and observed response to exercise may also be attributed to overlapping behavioural, physical, endocrine35, 36, 37, 51 or physiological effects52, 53, 54 relative to acute/subacute or rehabilitation/recovery phases. Further study is warranted to explore the mechanisms underlying the low therapeutic efficacy of FES to promote clinically relevant bone remodelling in the present study. Taken together, physiological evidence for ‘blunted’ bone responses to low-intensity exercise stress could suggest a multifactorial aetiology in this therapeutic window, thus raising questions about clinical requirements for combined approaches to remediation.
Conclusion
In summary, the low-intensity, discontinuous FES protocol was safe and well tolerated, but the protocol did not appear to delay or prevent early lower extremity bone loss, as measured by DEXA. An apparent lack of therapeutic efficacy may be explained by protocol inadequacies or Type 2 error due to low statistical power. Modest between-group differences were identified in total BMD at the subacute sample point, which may be attributed to Type 1 error. Taken together, these DEXA data do not indicate a clinically relevant role for exercise, as elicited by FES, in the remediation of early SCI bone loss.
Lastly, there were no convincing BMD trends to suggest that FES after acute SCI forestalled or reversed the onset or postinjury progression of lower extremity bone loss or subsequent pathological fracture risk. The data could indicate that the early period is not conducive to an osteogenic response, which cannot be fully explained. Alternatively, the data may indicate that FES-induced bone effects are mode or dose dependent, and that the modes or doses used and/or tolerated in this critical early window were sub-therapeutic. Although there are still many uncertainties about safe, efficacious, well-tolerated and cost-effective avenues for osteoporosis treatment, as well as the optimal time for the implementation of bone loss prevention protocols, these data do not substantiate a clinically relevant role for FES in the early prevention of osteoporosis. As discrepancies between the observed and expected responses to exercise are consistent with a complex pathogenesis, at least initially, the lack of a therapeutic effect could suggest a requirement for multimodal bone loss prevention and treatment avenues.
References
Basmajian JV . Muscles Alive. Their Functions Revealed by Electromyography, 5th edn. Williams and Wilkins 1985.
Wallin BG, Fagius J . The sympathetic nervous system in man-aspects derived from micro-electrode recordings. Trends Neurosci 1986; 9: 63–67.
Woolsey CN . Cortical localisation as defined by evoked potential and electrical stimulation studies. In: Schaltenbrand G, Woolsey CN (eds). Cerebral Localisation and Organisation. University of Wisconsin Press: Wisconsin, MI 1964, pp 17–32.
Baldi JC, Jackson RD, Morallie R, Mysiw WJ . Muscle atrophy is prevented in patients with acute spinal cord injury using functional electrical stimulation. Spinal Cord 1998; 36: 463–469.
Nash MS et al. Reversal of adaptive left ventricular atrophy following electrically-stimulated exercise training in human tetrataplegics. Paraplegia 1991; 29: 590–599.
Mohr T, Anderson JL, Beiring-Sorensen F, Galbo H, Wagner A, Kjaer M . Long term adaptation to electrically induced cycle training in severe spinal cord injured individuals. Spinal Cord 1997; 35: 1–16.
Hangartner TN, Rodgers MM, Glaser RM, Barre PS . Tibial bone density loss in spinal cord injured patients: effects of FES exercise. J Rehab Res Dev 1994; 31: 50–61.
Talmadge RJ, Castro MJ, Apple Jr DF, Dudley GA . Phenotypic adaptations in human muscle fibres 6 and 24 weeks after spinal cord injury. J Appl Physiol 2002; 92: 142–154.
Hjeltnes N et al. Exercise-induced overexpression of key regulatory proteins involved in glucose uptake and metabolism in tetraplegic persons: molecular mechanisms for improved glucose homeostasis. FASEB J 1998; 12: 1701–1712.
Kler M et al. Regulation of glucose turnover and hormonal responses during electrical cycling in tetraplegic patients. Am J Physiol 1996; 271: R191–R199.
De Bell KK, Scremin AM, Perell KL, Kunkel CF . Effects of functional electrical stimulation-induced lower extremity cycling on bone density of spinal cord-injured patients. Am J Phys Med Rehab 1996; 75: 29–34.
Mohr T, Podenphant J, Biering-Sorensen F, Galbo H, Thamsborg G, Kjaer M . Increased bone mineral density after prolonged electrically induced cycle training of paralysed limbs in spinal cord injured man. Calcif Tiss Int 1997; 61: 22–25.
Eser P, de Bruin ED, Telley I, Lechner HE, Knecht H, Stussi E . Effect of electrical stimulation-induced cycling on bone mineral density in spinal cord injured patients. Eur J Clin Invest 2003; 33: 412–419.
Maimoun L et al. Changes in osteoprotegerin /RANKL system, bone mineral density, and bone biochemical markers in patients with recent spinal cord injury. Calcif Tissue Int 2005; 76: 404–411.
Roberts D et al. Longitudinal study of bone turnover after acute spinal cord injury. J Clin Endocrinol 1998; 83: 415–422.
Mechanick JI, Pomerantz F, Flanagan S, Atein A, Gordon WA, Ragnarsson KT . Parathyroid hormone suppression in spinal cord injury patients is associated with degree of neurologic impairment and not the level of impairment. Arch Phys Med Rehab 1997; 78: 692–696.
Garland DE et al. Osteoporosis after spinal cord injury. J Orthop Res 1992; 10: 371–378.
Eser P et al. Relationship between the duration of paralysis and bone structure: a pQCT study of spinal cord injured individuals. Bone 2004; 34: 869–880.
Garland DE, Foulkes GD, Adkins RH, Stewart CA, Yakura JS . Regional osteoporosis following incomplete spinal cord injury. Contemp Orthop 1994; 28: 134–139.
Dauty M, Verbe BP, Maugars Y, Dubois C, Mathe JF . Supralesional and sublesional bone mineral density in spinal cord-injured patients. Bone 2000; 27: 305–309.
Zhender Y et al. Prevention of bone loss in paraplegics over 2 years with alendronate. J Bone Miner Res 2004; 19: 1067–1074.
Pearson EG, Nance PW, Leslie WD, Ludwig S . Cyclical etidronate: its effect on bone density in patients with acute spinal cord injury. Arch Phys Med Rehab 1997; 79: 269–273.
Chen B, Mechanick JI, Nierman DM, Stein A . Combined calcitriol–pamidronate therapy for bone hyper-resorption in spinal cord injury. J Spinal Cord Med 2001; 24: 235–240.
Moran de Brito CM, Battistella LR, Saito ET, Sakamoto H . Effect of alendronate on bone mineral density in spinal cord injury patients: a pilot study. Spinal Cord 2005; 43: 341–348.
Bracken MB et al. A randomized controlled trial of methylprednisolone or naloxone in the treatment of acute spinal cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med 1990; 322: 1405–1411.
The Uniform Data System for Medical Rehabilitation. The Functional Independence Measure (FIM sm) Participant Manual, Version 5. 0 (Australia). State University of New York: Buffalo, NY 1999.
Stover SL, Apple DF, Donovan WH, Maynard FM (eds). International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association: Chicago, IL 1996.
Jones LM, Goulding A, Gerrard DF . DEXA: A practical and accurate tool to demonstrate total and regional bone loss, lean tissue loss and fat mass gain in paraplegia. Spinal Cord 1998; 36: 637–640.
Jaovisidha S, Sarotis DJ, Martin EME, Foldes K, Szollar SM, Deftos LJ . Influence of heterotopic ossification of the hip on bone densitometry: a study in spinal cord injured patients. Spinal Cord 1998; 36: 647–653.
De Bruin ED, Frey-Rindova P, Herzog RE, Deitz V, Dambacher MA, Stuhl E . Changes to tibia bone properties after spinal cord injury: effects of early intervention. Arch Phys Med Rehab 1999; 80: 214–220.
Warden SJ, Bennell KL, Matthews B, Brown DJ, McMeeken JM, Wark L . Efficacy of low-intensity pulsed ultrasound in the prevention of osteoporosis following spinal cord injury. Bone 2001; 29: 431–436.
Alsop WK, Caulton J, Rubin C, Admans J, Mughal Z . Low magnitude mechanical loading is osteogenic in children with disabling conditions. J Bone Miner Res 2004; 19: 360–369.
Rubin C et al. Quality and quantity of trabecular bone in the femur are enhanced by a strongly anabolic, noninvasive mechanical intervention. J Bone Miner Res 2002; 17: 349–357.
Bizzarini E, Saccavini M, Lipanje F, Magrin P, Malisan C, Zampa A . Exercise prescription in subjects with spinal cord injuries. Arch Phys Med Rehab 2005; 86: 1170–1175.
Huang TS, Wang YH, Chiang HS, Lien YN . Pituitary-testicular and pituitary–thyroid axes in spinal cord-injured males. Metabolism 1993; 42: 516–521.
Wang YH, Huang TS, Lien IN . Hormone changes in men with spinal cord injuries A. J Phys Med Rehab 1992; 71: 328–332.
Tsitouros PD, Zhang YG, Spungen AM, Baumann WA . Serum testosterone and growth hormone/insulin-like growth factor-1 in adults with spinal cord injury. Horm Metab Res 1995; 27: 287–292.
Yang L, Blumbergs PC, Jones NR, Manavis J, Sarvestini GT, Ghabriel MN . Early expression and cellular localization of proinflammatory cytokines interleukin-1-beta, interleukin-6 and tumor necrosis factor-alpha in human traumatic spinal cord injury. Spine 2004; 29: 966–971.
Gerrits HL, Hopman MT, Sargent AJ, De Haan A . Reproducibility of contractile properties of the human paralysed and non-paralysed quadriceps muscle. Clin Physiol 2001; 21: 105–113.
Bolotin HH, Sievanen H . Inaccuracies inherent in dual-energy X-ray absorptiometry in vivo bone mineral density can seriously mislead diagnostic/prognostic interpretations of patient-specific bone fragility. J Bone Miner Res 2001; 16: 799–805.
La Porte RE, Montoyne HJ, Casperson CJ . Assessment of physical activity in epidemiological research: problems and prospects. Public Health Report 1985; 100: 131–146.
Desharnais R, Jobin J, Cote C, Levesque L, Godin G . Aerobic exercise and the placebo effect: a controlled study. Psychosomatic Med 1993; 55: 149–155.
Freehafer AA, Mast WA . Lower extremity fractures in patients with spinal cord injury. J Bone Joint Surg 1965; 47-A: 683–694.
Frisbie J . Fractures after myelopathy: the risk quantified. J Spinal Cord Med 1997; 20: 66–69.
Vestergaarde P, Krogh K, Rejnmark L, Modekilde L . Fracture rates and risk factors for fractures in patients with spinal cord injury. Spinal Cord 1998; 36: 790–796.
Ragnarsson KT, Sell GH . Lower extremity fractures of patients with spinal cord injuries. Arch Phys Med Rehab 1981; 62: 418–423.
Minaire P, Edouard C, Arlot M, Meunier PJ . Marrow changes in paraplegic patients. Calcif Tiss Int 1984; 36: 338–340.
Gu Y, Genever PG, Skerry TM, Publicover SJ . The NMDA type glutamate receptors expressed by primary rat osteoblasts have the same electrophysiological characteristics as neuronal receptors. Calcif Tiss Int 2002; 70: 194–203.
Kooijman M, Rongen GA, Smits P, Hopman MTE . Preserved alpha-adrenergic tone in the leg vascular bed of spinal cord injured individuals. Circulation 2003; 108: 2361–2363.
Quin T, Guo X, Levi AD, Vanni S, Shebert RT, Sipski ML . High-dose methylprednisolone may cause myopathy in acute spinal cord injury patients. Spinal Cord 2005; 43: 199–203.
Huang TS, Wang YH, Lee SH, Lai JS . Impaired hypothalamic–pituitary–adrenal axis in men with spinal cord injuries. Am J Phys Med Rehab 1998; 77: 108–112.
DeGroot PCE, Van Kuppevelt DHJM, Snoek G, Van Der Woude LHV, Hopman MTE . Time course of arterial vascular adaptations to inactivity and paralyses in humans. Med Sci Sports Exerc 2003; 35: 1977–1985.
Hopman MT, van Ansten WN, Oeseburg B . Changes in blood flow in the common femoral artery related to inactivity and muscle atrophy in individuals with long- standing paraplegia. Adv Exp Med Biol 1996; 388: 379–383.
Boot CR, Groothuis JT, Van Langen H, Hopman MT . Shear stress levels in paralyzed legs of spinal cord-injured individuals with and without nerve degeneration. J App Physiol 2002; 92: 2335–2340.
Acknowledgements
We acknowledge the excellent technical support of Ms Trish Wesley, of the Department of Nuclear Medicine, Royal Adelaide Hospital and Ms Sheelagh Donohoe, Ms Julie Wheeler, Ms Marie Hogg and Ms Annette van den Broek of the FES Clinic, Hampstead Rehabilitation Centre. The study was funded by a grant from the Motor Accident Commission of South Australia and the State Government of South Australia. The protocol was approved by the Royal Adelaide Hospital Human Research Ethics Committee, and conducted in accordance with the guidelines of the Declaration of Helsinki.
Author information
Authors and Affiliations
Additional information
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research
Rights and permissions
About this article
Cite this article
Clark, J., Jelbart, M., Rischbieth, H. et al. Physiological effects of lower extremity functional electrical stimulation in early spinal cord injury: lack of efficacy to prevent bone loss. Spinal Cord 45, 78–85 (2007). https://doi.org/10.1038/sj.sc.3101929
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101929
Keywords
This article is cited by
-
Motorless cadence control of standard and low duty cycle-patterned neural stimulation intensity extends muscle-driven cycling output after paralysis
Journal of NeuroEngineering and Rehabilitation (2022)
-
Selective neural stimulation methods improve cycling exercise performance after spinal cord injury: a case series
Journal of NeuroEngineering and Rehabilitation (2021)
-
Evidence-based prevention and treatment of osteoporosis after spinal cord injury: a systematic review
European Spine Journal (2018)
-
Fabrication and in vitro biological properties of piezoelectric bioceramics for bone regeneration
Scientific Reports (2017)
-
Musculoskeletal Health in the Context of Spinal Cord Injury
Current Osteoporosis Reports (2017)