Abstract
Study design:
Prospective comparative study.
Objective:
To compare the efficacy of the ASIA scoring system and Tuli's classification for assessment of neurological status in a typical case of Pott's paraplegia/tetraplegia and suggest a suitable classification.
Setting:
Department of Orthopaedics of University College of Medical Sciences and GTB Hospital, Delhi, India.
Methods:
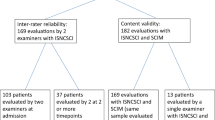
A total of 33 cases of tuberculosis of the spine with paraplegia were evaluated serially for the severity of the neurological deficit by grading systems as suggested by Tuli and ASIA score, during the course of treatment. A total of 111 readings of neurological status were recorded and analysed.
Results:
Tuli's grading was found to be sensitive for detection of early stage (grade I) of neurological deficit. The rest of the grades (grade II, III, IV) of Tuli's classification have a wide range of sensory-motor deficit and hence are insensitive to early detection of any deterioration/improvement in the neurological status. The ASIA score failed to grade all types of neurological deficit associated with the Pott's spine. The sensory-motor score obtained by the ASIA scale depends on the level of involvement of the spinal cord. The higher the level of the cord damage, the poorer is the score.
Conclusion:
Neither Tuli's grading nor the ASIA scale alone can effectively grade all stages of neurological deficit in tuberculosis of the spine. The neurological deficit in tuberculosis of the spine should be described in stages and each stage should have sensory and motor scoring. A new staging system of Pott's tetraplegia/paraplegia is suggested.
Similar content being viewed by others
Introduction
The first recorded evidence of paraplegia is in Edwin Smith's book that was copied by an unknown scribe around 1700 BC. The author is thought to be Imhotep, the physician to Pharaoh Joser III of Egypt. Many centuries later, Galen (AD130–200) first recognized different levels of injury and since then numerous classifications of paraplegia have been proposed.1
Neurological deficit is a dreadful complication of tuberculosis of the spine.2 The grading of neurological deficit is an indirect indicator of the severity of cord compression or spinal cord injury. During the course of treatment, serial neurological assessment is done to detect improvement or deterioration. This assessment is an important tool for prognostication as well as comparison of results with other cases.
The classifications used for traumatic tetraplegia/paraplegia are Frankel classification3 and the ASIA scale.4 Konstam and Blesovsky5 and Tuli and co-workers have classified the neurological deficit resulting from tuberculosis of the spine.2, 6
An ideal classification should not only quantify the severity of the neurological deficit as a result of cord compression but should also be sensitive enough to detect subtle changes in the neurological status of the patient. It should be simple, objective and reproducible with minimum inter- and intraobserver variation.
The aim of the present study is the comparative evaluation of the efficacy of the ASIA scoring system and Tuli's classification for tubercular tetraplegia/paraplegia.
Methods
A total of 33 cases of paraplegia secondary to tuberculosis of the spine (13 male and 20 female subjects), between 6 and 70 years of age (average of 35 years), are the subjects of the present study. Seven patients had caries of the spine between D1 and D6, 12 had caries between D6 and D9 and 14 had D10–L1 involvement. A total of 24 cases had disease of two vertebrae and nine cases had disease of three or more vertebrae. The neurological deficit was recorded using Tuli's classification as well as the ASIA scale at admission, and subsequently during the course of treatment (Table 1).
Tuli's classification2, 6 divides neural deficit in Pott's spine in four grades (Table 2).
On the ASIA scale, motor power of 10 muscle groups for the left and right sides (C5-T1 in upper limb and L2-S1 in lower limb) is measured on a six-point scale (0–5) and the total score is expressed as x/100. Sensory scoring (2 for normal, 1 for impaired, 0 for absent) is done for light touch and pin-prick in each dermatome from C2 to S5, and the total score is expressed as y/112 (28 dermatomes on each side).
The neural deficit was recorded by an independent observer who was blinded to the aim of the study and therapeutic outcome. A total of 12 patients responded to nonoperative management while 21 patients underwent anterolateral decompression. In these 33 patients, 111 readings of neurological status were recorded using Tuli's classification and the ASIA score simultaneously. The ASIA motor and sensory scores were categorized according to their respective Tuli's grades and one-way analysis of variance was carried out for Tuli's grades.
Results
Tuli's grade-I group had 24 out of 111 readings. Of the 24 readings, 20 did not have motor deficit and had an ASIA motor score (AM) of 100/100. The mean motor score was 99.14 (range 98–100). In the above group, 20/24 readings had no sensory loss. The mean sensory score for light touch (ASL) and pin-prick (ASP) was 107.73 (range 82–112). Such cases having a motor score of 100 and a sensory score of 112 with extensor plantar response and exaggerated deep tendon reflexes are considered essentially normal by the ASIA scale but Tuli's classification labels these as grade-I paraparesis.
Tuli's grade-II group had 25 readings. The range of AM score was 72–96 (mean 84.87), ASL score was 82–112 (mean 97.52) and ASP score was 82–112 (mean 102.136).
Tuli's grade-III group had 10 readings. The range of AM score in this group was 50–82 (mean 65.4). All patients had sensory loss. The ASL range was 60–112 (mean 94). The ASP ranged from 64 to 112 (mean 94.6).
Tuli's grade-IV group had 52 readings. The range of AM score was 50–80 with a mean of 58. In all, 40% patients in this group had an AM score of 50 (no power in lower limbs). The ASL range was 52–112 (mean of 83.82). Similarly, ASP ranged 52–112 (mean 84.69). There were cases that had some motor power but were included in Tuli's grade IV (case nos. 3, 23, 25, 30) as they had bladder and bowel involvement. The third reading of case no. 3, had an AM score of 50, but was included in Tuli's grade III because the patient regained bladder/bowel control. The sensory score in 38 out of 52 readings in this group was closer to a normal value of 112 due to the distal level of cord damage.
Multiple comparisons
In Tuli's grade I cases, 83.8% readings had an AM score of 100 (no motor deficit). The lowest AM score in this group was 98, while the lowest value of ASL and ASP was 82. All ASL and ASP readings in Tuli's grade II, 80% in Tuli's grade III and 73.1% ASL and ASP readings in Tuli's grade IV were more than 82. On analysis, it is clear that there is no overlap of AM readings of Tuli's grade 1 cases on Tuli's grade II, III and IV cases. However, for sensory scores, Tuli's grade 1 readings overlap on Tuli's grade II, III and IV readings.
The lowest AM score in Tuli's grade II cases was 72. In all, 20% of AM scores in Tuli's grade III cases and 7.3% of AM scores in Tuli's grade IV cases had values of more than 72. This signifies an overlap of AM scores of Tuli's grade II cases over Tuli's grade III and IV cases. The lowest ASL and ASP score in Tuli's grade II cases was 82. The ASL and ASP scores of more than 82 were recorded in 80% of Tuli's grade III cases and 73.5% of Tuli's grade IV cases.
In Tuli's grade III and IV cases, the lowest AM score was 50 and the range of AM score was nearly identical. ASL and ASP readings of all cases in Tuli's grade III and 47/52 readings in Tuli's grade IV cases had values of more than 60 and were in the same range. Despite a similar sensory motor score as Tuli's grade III, Tuli's grade IV cases had sphincter involvement/flexor spasm/ flaccidity/pressure sores indicating severe cord compression.
Thus, there is a significant overlap of AM, ASL and ASP scores of Tuli's grade II, III and IV cases. With similar AM, ASL and ASP scores, Tuli's grade may differ according to functional status of the patient (Table 3).
Discussion
In a typical lesion of Pott's spine, the compression starts anterior to the cord.7 The earliest manifestation is a gradual increase in spasticity, which may not be appreciated by the patient as he has only clumsiness of gait. The clinician detects exaggerated reflexes and extensor plantar responses. As compression increases, the anterior column of the cord is more affected and the patient starts losing motor power gradually, going from partial weakness to complete loss of power. By the time compression is severe enough to cause a complete block of conduction in the anterior column, the lateral column is also affected partially, thus producing some reduction of sensation (pain, temperature and crude touch). With further increase in compression, the posterior column is also affected, leading to complete loss of sensation and disturbances of sphincter control. In long-standing compression, spasticity is replaced by flaccidity and flexor spasms.
Frankel et al3 divided a broad spectrum of neurological deficit into five discrete groups in acute spinal injury, which was modified and incorporated in the ASIA impairment scale.
The ASIA scale does not classify all types of neurological deficit associated with Pott's spine, such as the following: (a) cases where the patient does not appreciate weakness but the clinician detects signs of upper motor neuron lesion. There are 20 readings of normal ASIA motor and sensory score with ASIA impairment scale (AIS) as ‘E’ (Table 4), despite increased tone and extensor plantar response. Hence, Tuli's classification is more sensitive for early detection of neurological deficit.
(b) Paraplegia with bladder and bowel involvement. The ASIA impairment scale was ‘C’ in 7/10 readings in Tuli's grade III and 32/52 in Tuli's grade IV. The bladder/bowel involvement is not an integral feature of AIS. Thus, in spite of severe cord compression with the involvement of sphincters (Tuli's grade IV), AIS may be ‘C’. This depicts the inability of the ASIA scale to show increasing severity of cord compression.
(c) Paraplegia in flexion/flaccidity. (d) Paraplegia with flexor spasms.
In the ASIA scale, the severity of impairment reflected by the score depends upon the level of involvement in addition to the severity of the compression at the involved level. In Tuli's grade-III, few ASIA sensory score readings (case nos. 6 and 13) were very close to the normal value of 112. This can occur in paraplegic patients where the damage to the cord is at a relatively distal level and there are 10–15 uninvolved root segments above the damaged segment. In such a situation, the summation of values for the uninvolved and the involved segments on the ASIA scale may reach near the normal value.
In the ASIA scale, a case with severe cord compression at the distal level may have a motor and sensory score (AM, ASL, ASP) similar to a case with lesser magnitude of compression, but at a proximal level. For example, case no. 5 in our series had D9-10 disease with Tuli's grade IV paraplegia; the ASL and ASP were 88 and 92, respectively. On the other hand, case 14 had D5-6 disease with Tuli's grade IV paraplegia; the ASL and ASP were 56 and 63, respectively. Both cases had an AM score of 50. Both cases had paraplegia of similar severity, but the case with distal lesion showed a better sensory score.
As the assessment of the severity of compression at the involved segment is important for prognostication, the numerical value of the score should be directly proportional to the severity of cord compression. In Pott's spine, there may be complete block of conduction below the involved segment, yet the patient may have good sensory-motor score according to the ASIA scale if the level of involvement is lower. The natural course of neural deficit in a typical lesion of TB of the spine is progressive due to increasing anterior extradural compression in contrast to the traumatic spinal cord injury where the severity of insult to the cord is maximum at the time of injury. In TB of the spine, it starts as spasticity and progresses to partial and total motor loss with gradual sensory deficit. At any stage, spinal shock and areflexia may lead to sphincter involvement. In this category, there were patients who also had some motor power, but were included in Tuli's grade IV (case nos. 3, 23, 25, 30) as they had bladder and bowel involvement. In a long-standing case, flaccidity and flexor spasm may appear. Instability of the vertebral column or vascular catastrophe can hasten the process. Increasing neural deficit reflects increasing cord compression while decreasing neural deficit is an indicator of disease regression.
In Tuli's classification, the spectrum of neurological deficit is divided into four discrete grades. Tuli's grade II takes into consideration motor deficit only. Results show that the majority of cases in this group have some sensory loss also. Each grade has a broad range of sensory-motor deficit, especially in grade III and grade IV. Moreover, lack of numeric sensory-motor scoring renders it less sensitive to subtle changes in neurological status of the case during the course of treatment, but it is more sensitive for early detection of neurological deficit. For example, case no. 33 remained in Tuli's grade IV in three subsequent readings, although the sensory scores show gradual improvement in all the assessments (ASL scores 70, 83, 92, respectively).
The differentiating feature between Tuli's grade III and IV is the quantum of sensory deficit, but multiple comparisons show that III and IV are inseparable as far as the sensory deficit is concerned. After evaluating both the classifications, it is obvious that neither is a complete classification for neural deficit in tuberculosis of the spine.
Proposed classification
In TB of the spine, the usual course of disease and development of neurological deficit is a gradual process. Typically, it progresses more or less in a definite pattern. Hence tetraplegia/paraplegia should be classified in stages.
An ideal classification system should assess the functional status of the paraplegic/tetraplegic patient and should reflect the severity of cord compression. Each stage should have numeric sensory-motor scoring to show early deterioration or improvement of neurological status. The motor scoring should be done according to the ASIA scale. Sensory deficit at each root level should be recorded as:
Grade 0 – complete loss of sensation; Grade 1 – impairment of lateral as well as posterior column sensations; Grade 2 – impairment of lateral column sensations; Grade 3 – normal sensory appreciation.
The use of a four-point sensory scoring system instead of the ASL and ASP of the ASIA scale is proposed as lateral column sensations are decreased before posterior column sensations in a typical lesion of Pott's spine. The four-point sensory scale of the proposed classification will be carefully tested for reliability in the future.
The paraplegia/tetraplegia in TB of the spine should be classified into five stages.
Stage I – is the same as Tuli's grade I.
Stage II – The patient has spasticity with motor deficit but is a walker. He is able to lift the upper limb against gravity in tetraparesis. The anticipated motor score in tetraparesis would be between 60 and 100. In paraparesis, it would be between 80 and 100.The sensory impairment of the lateral column is present at all root levels. The sensory score is a summation of sensations at all root levels at and below the level of cord involvement.
The sensory score for a particular level of involvement can be calculated by using the formula: Total sensory score=no. of involved root segments × grade of sensation × 2 (for both sides). The sensory score of a patient is expressed as total sensory score/maximum sensory score.
Stage III – Bedridden spastic patient. Anticipated motor score for quadriplegia is 0–30, and for paraplegia it is 50–80. Sensory scoring is the same as in stage II.
Stage IV – Bedridden patient with severe sensory loss, and/or pressure sores. Anticipated motor score in tetraplegia is 0 and in paraplegia is 50. There is impairment of both lateral and posterior column sensations.
Stage V – Same as stage IV and/or bladder and bowel involvement, and/or flexor spasms/flaccid tetraplegia/paraplegia. There is usually no motor power below the involved cord segment. There are no sensations distal to the level of involvement. If the bladder/bowel are affected or flexor spasm is present, then in spite of some preservation of motor power or sensation it will be considered as stage V.
The proposed classification will need to be further evaluated in a population of individuals with TB of the spine. Waters et al8 reported in traumatic SCI that paraplegic subjects with lower extremity motor scores of 30 were able to ambulate in the community. It needs to be evaluated whether it is different in subjects with spastic paraparesis due to TB of the spine.
References
Lucas JT, Ducker TB . Motor classification of spinal cord injuries with mobility, morbidity and recovery indices. Am Surg 1979; 45: 151–158.
Jain AK, Kumar S, Tuli SM . Tuberculosis of spine (C1–D4). Spinal cord 1999; 37: 362–369.
Frankel HL et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia 1969; 7: 179–192.
Ditunno Jr JF et al. The international standards booklet for neurological and functional classification of spinal cord injury. Paraplegia 1994; 32: 70–80.
Konstam PG, Blesovsky A . The ambulant treatment of spinal tuberculosis. Br J Surg 1962; 50: 26–38.
Tuli SM . Tuberculosis of Skeletal System 2nd edn. Japee Brothers Medical Publications (p) Ltd: New Delhi 1996, p 220.
Jain AK . Treatment of tuberculosis of the spine with neurologic deficit. Clin Orthop 2002; 398: 75–84.
Waters RL, Adkins R, Yakura J, Vigil D . Prediction of ambulatory performance based on motor scores derived from standards of the American Spinal Injury Association. Arch Phys Med Rehabil 1994; 75: 756–760.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Jain, A., Sinha, S. Evaluation of systems of grading of neurological deficit in tuberculosis of spine. Spinal Cord 43, 375–380 (2005). https://doi.org/10.1038/sj.sc.3101718
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101718
Keywords
This article is cited by
-
Incidence and Patterns of Drug Resistance in Patients with Spinal Tuberculosis: a Prospective, Single-Center Study from a Tuberculosis-Endemic Country
Indian Journal of Orthopaedics (2023)
-
Phoenixin-20 ameliorates brain infarction by promoting microglia M2 polarization in an ischemic stroke model
Metabolic Brain Disease (2022)
-
The spectrum of tuberculosis of the spine in pediatric age group: a review
Child's Nervous System (2018)
-
Tuberculosis of spine: neurological deficit
European Spine Journal (2013)