Abstract
Schizophrenia is a disease syndrome with major public health implications. The primary advance in pharmacotherapeutics was in 1952 with the introduction of antipsychotic medications (ie, chlorpromazine, dopamine D2 antagonism). Barriers to progress have been substantial, but many will be subject to rapid change based on current knowledge. There are attractive psychopathology indications for drug discovery (eg, impaired cognition and negative symptoms), and drugs with efficacy in these domains may have application across a number of disease classes. These pathologies are observed prior to psychosis raising the possibility of very early intervention and secondary prevention. Success in drug discovery for cognition and negative symptom pathologies may bring forth issues in ethics as the potential for enhancing normal function is explored.
Similar content being viewed by others
INTRODUCTION
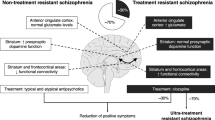
Schizophrenia is a clinical syndrome, perhaps comprising several disease entities. Cases are observed worldwide with some variation in incidence and life-long prevalence, but afflicting 0.5–0.8 percent of the world's population (Saha et al, 2005). The onset of some aspects of the disease may be observed from birth onward, but psychotic symptoms generally become manifest in late adolescence and early adulthood in males, with an extended onset period in females. Psychotic symptoms such as hallucinations, delusions, and disorganization of thought can impair function, and are stigmatizing. These symptoms lead to diagnosis, but are usually preceded by trait dysfunctions in cognition, affect, and motivation. These aspects of schizophrenia account for substantial decrements in social and occupational functioning and appear to be primary determinants of long-term morbidity (Matza et al, 2006; Velligan et al, 2006; Green et al, 2004; Harvey et al, 2006). Psychotic symptoms may persist from disease onset, but the general trend is a pattern of remission/exacerbation or partial remission/exacerbation. The combination of early onset, poor function, and stigmatizing symptoms lead to failure in many human pursuits. Patients with schizophrenia are over-represented among the non-married, childless, unemployed, underemployed, and low academic achievers. Homelessness, extensive hospitalization, joblessness, time in jail, disability support, supervised living arrangements, dependence on family, excess tobacco, and substance abuse, social isolation, poor health, victims of crime, and early death are all associated with schizophrenia. The cost of schizophrenia in human and financial terms is great to both society and to families (Murray and Lopez, 1996; Wyatt et al, 1995; Mauskopf et al, 2002). Schizophrenia is a leading public health challenge (Rupp and Keith, 1993; Murray and Lopez, 1996; Lopez et al, 2006). Critical therapeutic advances have been associated with humane care, specialized forms of psychosocial treatments, electroconvulsive therapy, community-based care, and rehabilitation. Although some patients do well off medication (Bola, 2006) pharmacotherapy is generally considered the essential component for reducing psychotic symptoms and relapse rates. Among the first pharmacological agents used in schizophrenia was the antihypertensive agent, reserpine. This drug acts to reduce synaptic dopamine release and its beneficial effects in schizophrenia preceded the discovery of the antipsychotic properties of chlorpromazine (for review see Seeman, 2002; Kapur and Mamo, 2003). Since chlorpromazine was introduced in 1952, about 50 additional antipsychotic drugs have been developed for the treatment of schizophrenia. Each of these drugs exerts therapeutic action at the dopamine D2 receptor and all but aripiprazole, are antagonists at the D2 receptor (Carlsson and Lindqvist, 1963; Kapur and Mamo, 2003; Davies et al, 2004). Aripiprazole, on the other hand, is a partial agonist at the D2 receptor (for review see Tamminga and Carlsson, 2002). Clozapine, the only antipsychotic approved with a superiority claim for treatment-resistant and refractory patients, is also a D2 antagonist (Conley, 1998; Wahlbeck et al, 1999). Clozapine is distinguished from other antipsychotic drugs in several ways including a broad profile of receptor affinities and ‘rapid-on, rapid-off’ kinetics at the D2 receptor (Seeman, 2002). However, the basis for clozapine superiority is not known, and has not been replicated by other new generation drugs.
Despite the ability of dopamine antagonists to reduce psychosis and delay symptom exacerbations, the long-term outcome of schizophrenia has remained poor. During the 1950–1960s, two major changes occurred in the way schizophrenia was treated. The first was a shift in treatment focus from long-term custodial to community-based care. The second change was the introduction of efficacious pharmacotherapy. However, Hegarty et al (1994) found little evidence that these two major revolutions altered the outcome of schizophrenia during the twentieth century. Changing methodologies during this period make before and after antipsychotic drug therapy comparisons difficult, but schizophrenia remains a chronic illness with substantial functional impairments for most cases. A probable explanation will be found below when considering the diverse nature of schizophrenia pathology, and the association of functional outcomes with pathological domains that are not responsive to antipsychotic medication.
The majority of currently approved pharmacological agents for the treatment of schizophrenia target psychotic symptoms as their primary effects. In this critical aspect, the drugs are extensively similar in efficacy and effectiveness. Only clozapine has been documented to be modestly more effective in treatment resistant/refractory cases (Kane et al, 1988; Lewis et al, 2006; McEvoy et al, 2006; Conley, 1998; Wahlbeck et al, 1999). The first generation antipsychotic drugs, often termed neuroleptics, have robust adverse effects. Dysphoria, dystonia, akathisia, dyskinesia, and Parkinsonian motor symptoms are the most notable of these effects. First generation antipsychotic drugs also may increase or prolong the depressive/demoralization aspects of illness course, impair learning, and slow information processing, and akathisia may increase hostility, aggression, and suicidality (Conley and Kelly, 2002; Awad and Voruganti, 2004; Weickert and Goldberg, 2005). These adverse effects have been exaggerated in clinical practice where excess dosing and under utilization of prophylactic antiparkinsonian drugs is common. Second generation antipsychotic drugs are similar to first generation drugs in their profile of therapeutic efficacy for core schizophrenia pathology (see cochrane reports http://www.mrw.interscience.wiley.com/cochrane/). Many of the adverse effects of first-generation antipsychotic drugs are diminished or absent in the second-generation antipsychotic medications, and this may account for advantages observed in some comparison studies. These advantages observed in some, but not all, studies include improvement in measures of negative symptoms, cognitive test performance, depression, adherence, time to relapse, aggression, and suicide. A few studies using low doses of first-generation antipsychotic drugs, and recent head-to-head comparisons with public sponsorship in the United States and United Kingdom fail to support the superiority of second generation drugs (Jones et al, 2006, Lieberman et al, 2003a, 2003b, 2005; Geddes et al, 2005; Schooler et al, 2005; Lieberman, 2007). Some second-generation antipsychotic drugs cause very substantial adverse effects. Among these metabolic syndrome, already a concern in persons with schizophrenia based on life style risk factors, is a major concern with drugs that cause increased body mass index, hyperlipidemia, reduced insulin sensitivity, and are associated with an increased incidence of diabetes. Reduction in life span is great, and expected to worsen with increased exposure to pharmacological adverse effects (Hennekens et al, 2005; Auquier et al, 2006; Seeman, 2007; Colton and Manderscheid, 2006; Newcomer and Hennekens, 2007). In most respects, drug development for schizophrenia has not progressed appreciably since the introduction of chlorpromazine, a point which recently found emphasis in a large first episode clinical trial in Beijing comparing the original antipsychotic drug, chlorpromazine, with the only second generation drug with documented superiority, clozapine. This trial reported little therapeutic difference between these two drugs (Lieberman et al, 2003a). While not denying the clozapine superiority in treatment-resistant cases, these data reinforce the view that dopamine D2 receptor antagonists share a mechanism of action that produces similar efficacy.
The clinical trials data to date justify the following conclusions.
-
1)
Discovery platforms for schizophrenia have repeatedly produced drugs with the same or similar mechanism of action. In spite of fifty years of development, virtually no new drugs have achieved superior efficacy for psychosis. The traditional discovery pathway has not produced drugs that address the cognitive impairments or negative symptom pathology.
-
2)
Quality of life and functional outcomes are not adequately addressed by antipsychotic drug development.
Impaired cognition and negative symptom pathology remain unmet treatment needs, and substantially account for long-term morbidity, and poor functional outcomes associated with this disease (Buchanan et al, 2005; Green et al, 2004; Kirkpatrick et al, 2000, 2006; Matza et al, 2006).
History of the Concept and A Paradigm Shift: Relevance to Drug Discovery
In the late nineteenth century medical progress was facilitated by the power of the disease entity model, which identified similarities across patients in onset, manifestations, and course of illness. Distinctive patterns had been elusive among the insane, and the substantial heterogeneity between patients was sometimes resolved by identifying very narrow and specific proposed disease entities. Syphilitic insanity was common in that era, and manifestations included psychosis. When the cause was determined and these cases were recognized and separated from other forms of madness, it was possible for Kraepelin to distinguish the illness patterns on which he proposed the two major forms of chronic psychotic illness (Kraepelin, 1919). The manic-depressive psychoses were described and separated from dementia praecox. The latter combined paranoia, hebephrenia, and catatonia disease classes based on similarities in age and type of onset, symptomatic manifestations, and course of illness. Parenthetically, discovery of the spirochete as causative of a common and severe form of insanity and the subsequent treatment and prevention is one of the remarkable therapeutic triumphs in medicine.
Bleuler (1950), working in the era of associative psychology, identified dissociative pathology as fundamental to dementia praecox, and coined the term schizophrenia to denote mental splitting within thought, and between thought, affect, and behavior. Introduced in 1911, the concept of schizophrenia as a single disease entity with a unifying pathology has been the dominant paradigm for almost 100 years. The influence of this paradigm can be seen in most studies in that the design addresses schizophrenia as a class and views heterogeneity of manifestations as representing the same latent structure. Kraepelin described two maladies within dementia praecox: the dissociative pathology of Bleuler and the weakening of the well-springs of volition (today's negative symptom concept). But he viewed these as two different phenomena arising from the same disease. The key question is whether schizophrenia is a disease or a syndrome (Carpenter, 2006). Consider dementia research and the importance of identifying specific disease entities rather than investigating a heterogeneous dementia syndrome.
The title of Bleuler's text, Dementia Praecox or the Group of Schizophrenias, suggests heterogeneity, but the traditional subtypes such as paranoid schizophrenia, hebephrenic schizophrenia and catatonic schizophrenia were not validated as separate disease entities. Rather, by the mid-twentieth century, influential proposals from Schneider (1959) and Langfeldt (1937, 1939) focused on symptoms with critical diagnostic importance proposing to distinguish true schizophrenia from pseudoschizophrenia and other forms of psychotic illness. During this time much of American psychiatry neglected classification in favor of psychodynamic formulations. The introduction of efficacious drugs for depression, psychosis, and mania gave impetus to classification. And the growing psychiatric research community needed classification criteria that were specific, valid, and reliable. Studies documenting a broader definition of schizophrenia in the US compared to the UK gave urgency to restructuring classification. The resulting DSM-III, influenced by the European concept of nuclear schizophrenia and the primacy of Schneider's First Rank Symptoms, resulted in an unintended but dramatic change in the concept of schizophrenia (Tamminga and Carpenter, 1982; Eysenck et al, 1983). Symptoms such as hallucinations and delusions, considered secondary by Bleuler, became the foremost defining criteria, and special forms such as voices commenting on behavior or discussing the patient in third person pronouns became critical to the diagnosis of schizophrenia. They also became, if combined with duration and dysfunction criteria, sufficient to define a case as schizophrenia. Consequently, the schizophrenia concept was redefined as psychosis, with emphasis on reality distortion pathology.
During this time, clinical trials of antipsychotic drugs used primary endpoints that were weighted toward psychotic symptoms as defining therapeutic response. Hence, time to discharge, time to relapse, and rating scales using total scores or psychosis scores were used to assess change in drug treatment trials.
Taken together, the effect of these trends was to treat schizophrenia as a unitary disease entity, to equate psychosis (at least special psychotic phenomena) with schizophrenia, to measure treatment effects by measuring effects on psychosis, and to generally regard antipsychotic drugs as antischizophrenia drugs. Drug development models favored compounds based on their ability to block or reverse ‘hyperdopaminergic’ models. The result is 50 years of dopamine antagonists with a partial agonist as the only variation on the theme (Adams et al, 2005).
A Paradigm Shift to Facilitate Drug Discovery
Heterogeneity in the manifestations and course of schizophrenia has long been observed. Within the disease entity paradigm, various aspects of pathology were viewed as emerging from the same latent structure. A unifying pathophysiology was expected, with neuroanatomic locations of the pathology perhaps determining symptom expression. The syphilitic insanities provided a compelling model, and knowledge of brain–behavior relations could account for different symptom patterns between cases. This view was challenged by work in the early 1970s suggesting an almost orthogonal relationship between symptom complexes and a lack of predictive relationships between symptom domains (Strauss et al, 1974). Further, pathologic manifestations within a domain were closely linked across time so that negative symptoms predicted future negative symptoms, past social functioning predicted future functioning, etc (Carpenter et al, 1978; Strauss and Carpenter, 1977). On the basis of these data, schizophrenia was reconceptualized as a tripartite construct with positive psychotic symptoms, negative symptoms, and pathology in interpersonal relating, constituting separate domains. It was envisioned that each domain would be a separate target for etiologic and treatment discovery (Strauss et al, 1974).
This tripartite domains model, proposed in 1974, has been modified in important ways that are highly relevant to new drug discovery. First, positive psychotic symptoms involve two domains: reality distortion (ie, hallucinations and delusions) and disorganization of thought and behavior. Although both are responsive to antipsychotic drugs, they separate repeatedly in factor analytic studies (Buchanan and Carpenter, 1994) and may have different associated biologic features. Second, impaired cognition as measured in various psychological and neuropsychological test procedures, is now viewed as central to the early manifestations of schizophrenia and critically related to functional outcomes. The impaired cognitive pathology is not significantly associated with the symptom domains (Gold and Harvey, 1993; Berman et al, 1997; Harvey et al, 2006; Cohen et al, 2007) but is comprised of seven independent areas of impairment, which were identified by the academic/pharmaceutical/governmental MATRICS initiative (Table 1). The specificity of these concepts should facilitate developing animal and human experimental models. Third, a number of endophenotypes have been proposed (Table 2), often based on physiologic measures of information processing. This is especially critical in the post-genomic era since genotype/endophenotype relations are likely to be far more robust than genotype/schizophrenia relations (Braff and Light, 2005; Braff et al, 2007; Thaker, 2007). Here too, facilitation of animal (Table 3) and human experimental models useful in drug development are promising so long as phenotypes can be translated from one species to the other. Tables 2 and 3 provide evidence that human phenotypes can be translated into non-human experimental endpoints and that these endpoints, ultimately, can be used to inform about the human disease. Fourth, the negative symptom construct derived from Kraepelin's avolitional malady, is being revised to provide a more specific definition. Clinical ratings in treatment trials during the past 20 years have failed to differentiate primary (to the disease) from secondary (eg, paranoid social withdrawal, drug-induced anergia or akinesia, or depressive anhedonia) negative symptoms. Here too, animal and human models will be facilitated by currently evolving constructs and measurement. A consensus view, developed in a National Institute of Mental Health (NIMH) workshop, proposes anhedonia, blunted affect, alogia, avolition, and asociality as components of this construct (Kirkpatrick et al, 2006).
The domains of pathology paradigm, in contrast to the disease entity paradigm, identifies several aspects of schizophrenia as pathology targets for treatment development. The paradigm suggests separate developmental pathways for treatment discovery for each domain. Cognitive impairment and negative symptoms are the domains with the most compelling case as unmet treatment needs. If the domains of pathology paradigm proves robust in treatment discovery, other domains will be defined.
Animal Preparations and their use in Schizophrenia Drug Discovery
Advances in schizophrenia have been retarded not only by the complexities of the disease and a lack of consensus about the central features of the disease phenotype but also by inconsistencies in the neurochemical and molecular signatures of the disease and the dearth of informative animal models. The lack of useful animal preparations for schizophrenia can also be linked to the uniquely human nature of schizophrenia, which reflects the inability of animals to experience hallucinations and delusions, or even to convey the presence of these disease features. However, recent research is beginning to change thinking about the utility of animal preparations to generate useful information to understand the pathophysiology of schizophrenia, the identification of new treatment targets or conduct early evaluations of putative antischizophrenia drugs. A feature of critical importance to any of these uses of animal models is the relevance of the behavioral endpoints being analyzed in animals to the array of disease symptoms. The translation of some endpoints is immediately obvious, example, amphetamine-induced locomotion compared to amphetamine-induced displacement of radiolabeled raclopride in the human striatum (Laruelle et al, 1996), prepulse inhibition of the acoustic startle response (Swerdlow et al, 1994, 2000), spatial and working memory (Robbins, 1998) or even episodic memory (Eichenbaum and Fortin, 2005). These comparisons require accurate knowledge about both human and animal behaviors and the relationship to the disease process. Given the spectrum of phenotypes associated with schizophrenia, this is not always easily assessed. Articulated in Table 2 are human phenotypes that might be translatable to animal modeling.
Animal preparations that may be informative about some aspect of either the schizophrenia phenotype or etiology can be divided into four categories: (1) genetic-based preparations, (2) environmental-based preparations, (3) drug-induced preparations, and (4) lesion models. Much of the information driving the creation of these animal preparations was generated from either post-mortem human brain analysis using chemical, molecular or neuroanatomical techniques or epidemiological findings. Table 3 lists many of the animal preparations that have been reported to have phenotypic overlaps with either a behavioral component of schizophrenia or an identified molecular characteristic of the disease (Table 3).
Because of the diverse nature of the disease, generation of reliable and informative animal models has proven to be a difficult task. It is, however, fair to say that the models based solely on genetic modifications do not recreate the spectrum of schizophrenia-related phenotypes. Developmental models appear to better recapitulate the breadth of the behavior diversity of schizophrenia. Lesion models also are able to address the diverse nature of the disease. This said, several of the models may prove useful for generating an increased understanding of the pathophysiology of schizophrenia. Arguably, the most informative genetic models appear to be the calcineurin conditional knockout mouse, the neuregulin hypomorphic mouse, and the recently described DISC1 mutant mouse (Stefansson et al, 2002; Miyakawa et al, 2003; Hikida et al, 2007). There are two drawbacks to the currently available genetic models that must be mentioned. First, postmortem findings in schizophrenic brain tissue never reported the complete absence of any protein or mRNA in the human brain. Therefore, most of the current genetic knockout models create artificial voids in protein expression that do not exist in patients, although the use of heterozygous animals and some conditional knockout strategies are beginning to address this concern. Second, schizophrenia is considered a polygenic disease and it is overly simplistic to think that knocking out a single gene will recreate the diverse phenotype manifest in schizophrenic patients. With regard to other models, the rat prenatal stress model has strong face and construct validity based on epidemiological findings associated with schizophrenia (Kinnunen et al, 2003; Koenig et al, 2005; Lee et al, 2007) and the rat neonatal ventral hippocampal lesion model appears to recreate many of the behaviors associated with schizophrenia. However, the limitation to this later preparation is the void created during the lesion process, the consequences of which have yet to be fully established (Lipska, 2004). Nonetheless, the advent of these models, will likely streamline the creation new antischizophrenia drugs by facilitating (1) identification of new targets for drug discovery programs and (2) evaluation of the usefulness of new drugs based on new targets for the treatment of the symptoms of schizophrenia. Arguably, the greatest potential of these models maybe the identification of the pathophysiology underlying the disease and the identification of mechanisms to reverse that pathophysiology. However, because of the recent advent of many of the more useful animal models, there is only limited information available regarding the translation of findings in animal models to the treatment of schizophrenic human beings.
As mentioned above, the molecular pathology of schizophrenia remains obscure. However, investigators have developed genetic animal models for schizophrenia based on information gained from a variety of genetic linkage and DNA microarray studies. The genes most widely accepted to be involved in schizophrenia are summarized in Table 4. At the present time, the animal models based on these genetic findings do not recapitulate the breadth of the schizophrenia clinical profile. Several issues continue to confound attempts to advance further in this area. First, schizophrenia is a complex disease and multigenic. Continuing to pursue single genes as causal agents for the disease is overly simplistic and more efforts need to be directed toward understanding how multiple genes or genes and the environment interact to generate the disease phenotype. A second conundrum is parsing primary effects from compensatory effects. Post-mortem human studies are of great value, but only limited information can be gained about primary vs compensatory genetic changes in this system. Animal models may prove exceedingly valuable in addressing these particularly problematic issues. Finally, the deletion of genes and hence, proteins, from the brain's normal milieu does not accurately capture the molecular profiles generated in schizophrenic patients. It may be necessary to explore the utility of temporal or spatial genetic knockdowns to gain information about the importance of a number of genes in schizophrenia. Recent work with DISC1 confirms the value of this approach (Hikida et al, 2007; Pletnikov et al, 2007).
Three Conceptual Approaches to Drug Discovery for Pathological Domains
The disease model of schizophrenia's core pathologies presumes pathophysiologies that are distinguished from normal brain function. Nonetheless, the observed behaviors are on a continuum with normal human function. Patients exhibit impairments or decrements in normal functions, not the absence of these functions. Therapeutic interventions are intended to ‘normalize’ these functions. With this in mind, drug discovery can be based on three conceptual approaches. First, cognitive enhancing drugs could be developed that do not depend on the specific pathophysiology for effect. Pathways of normal cognitive processing, for example, may represent final common pathways for therapeutic effect. An example is the pro-cognitive effect of dopamine agonists in normal volunteers and patients with hyperactivity/attention disorder. A second conceptual approach is the direct correction of the pathophysiology underlying the impaired function. Animal models based on induced impairments could be useful screening tools for determining restitutive or restorative effects of drugs. A third construct involves compensatory mechanisms. Cognitive behavioral therapy appears more likely to be effective if it focuses on compensatory rather than restorative techniques (Bellack, 2003). This third possibility brings a new dimension to the discovery of cognitive enhancing compounds because molecular targets in compensatory pathways would now present an alternative to molecular targets involved in the pathology of schizophrenia per se.
A drug that acts in the pathways involved in compensatory effects may be more effective if the pathological domain is a longstanding trait, at least if functional outcome is the treatment target. The proposition here parallels analgesic development where a drug may target the analgesic pathways (eg, where morphine has its effect) or may target the expectancy pathways where placebo has its effect (Colloca and Benedetti, 2005).
Nine Items Impeding Drug Discovery in 2007 and Recommendations for Future Developments
The synopsis of schizophrenia research provided above, generates a variety of concerns about the current status of drug development for schizophrenia and possibly other neuropsychiatric disorders. Below is a list of nine points, which appear to represent significant hurdles in the current drug-development scheme. Attention to these nine points may lead to more rapid identification and development of new therapeutic agents for schizophrenia. This list of impediments is by no means exhaustive and more significant hurdles may be identified by others. Nonetheless, this list provides a starting point to focus attention on the logjam in drug development for schizophrenia, and to contribute to a discussion of methods for breaking the logjam.
1. The single-disease paradigm with psychosis-defining schizophrenia. Considering schizophrenia as a single-disease entity has skewed drug development to focus solely on psychosis. However, positive psychotic symptoms comprising disorganized thought and behavior, hallucinations, and delusions are only one aspect of schizophrenia pathology. Key domains of pathology-affecting course and functional outcomes are negative symptoms and impaired cognition. Focus on these domains and the critical components encapsulated by these domains will potentially generate endophenotypic markers that will be useful for drug discovery. This paradigm shift is beginning to be employed by many investigators in academic and industrial settings.
2. Failure to identify key molecular pathologic elements as treatment targets. Basic knowledge at the level of molecular etiology and pathophysiology is insufficient to define molecular targets for drug development with high predictive validity for therapeutic success. The study of etiology and pathophysiology at the syndrome level fails to address heterogeneity. It is increasingly imperative to develop information on the molecular basis of each aspect of the disease to perform definitive studies about the illness and generate models that are more informative (Carpenter et al, 1993).
3. Failure to develop and apply animal and human models for specific attributes to enhance early evaluation of candidate compounds. Early proof of concept or proof of principle studies would greatly streamline the flow of drugs through the developmental pipeline. Investment in creating and validating model systems for the specific pathologic domains is essential.
4. A complex multi-factorial, polygenetic brain disorder without known, specific neuropathology/pathophysiology; and limited approaches to identifying novel molecular targets. Sophisticated bioinformatic approaches combined with molecular and neuroanatomical studies are needed to identify the causes and pathologic changes for each symptom domain. The bioinformatic resources to accomplish this task combined with the nucleic acid- and protein-based investigations that will be needed to break the drug discovery logjam are expensive. At present, conducting the studies needed to generate reliable information on the molecular level requires large resources, usually located in labs at pharmaceutical companies. An additional contribution to the logjam is the limited transmission of such molecular information from industry into the public sector. Facilitating this transfer of information without harming the intellectual property of the companies will be essential if discovery of molecular targets is to be maximized. A final consideration in this regard is the development of consistent information about putative molecular targets. Abundant DNA microarray data are available about the disease but understanding the limitations of working with disease-related post-mortem human brain tissue is an under-appreciated aspect of data interpretation. It may be that informative animal models based on etiological considerations may create new opportunities to identify molecular pathophysiology of the disease domains.
5. Substantial profit associated with marketing of new drugs without regard for novel mechanism or therapeutic advance, thus using discovery pathways that result in D2-active drugs. Developing antipsychotic drugs is relatively inexpensive and low risk for pharmaceutical companies, in part because the pathway for regulatory approval and marketing is clear. Potential profits are large, and a substantial advance over current drugs is not required. This results in resources being devoted to the development of ‘me too’ antipsychotic drugs that neglect novel mechanisms and pathologic targets other than psychosis. Appreciation of the potential market, especially for a pro-cognitive drug, combined with greater feasibility for proof of concept testing, will facilitate development. At the policy level, raising the bar for approval of drugs which are based on the same therapeutic mechanism and which fail to document superior efficacy would shift incentives toward more effective therapies.
6. A general neglect of schizophrenia by society. Schizophrenia remains highly stigmatizing with most patients being impoverished, unemployed and unmarried. Moreover, the burden on affected families is high. Clinical care is inadequately funded, and society's willingness to pay high costs for drugs is becoming increasingly doubtful. Addressing the lack of public understanding of schizophrenia and the need for supporting additional care costs are beyond the scope of this report, but the reaction to the greatly increased cost of new drugs combined with public attention to the minimal advances in efficacy may create another cycle of neglect.
7. Industry bias against drug discovery for complex diseases affecting impoverished populations. A major impediment to developing new schizophrenia drugs is the idea that schizophrenia is too complex, and there is inadequate knowledge upon which to base rational drug discovery. This perception is based on the heterogeneity of a disease syndrome and a realistic appreciation of current knowledge of molecular pathophysiology. However, we propose that investing in appropriate animal models, molecular tools, Bioinformatics, and neuroimaging for the study of pathologic domains will result in accelerated progress. A complex neuropsychiatric syndrome may be resolved at the level of pathologic domains, each with specific pathways that can be targeted for new drug development. Industry needs to accept the challenge of discovery in the context of a multi-factorial, polygenic syndrome and apply new concepts. A similar statement could be made about other neuropsychiatric disorders. Resolving pathophysiology at the level of pathological domain rather than syndrome may also address the overlap between psychiatric illnesses, and present drug development opportunities that cut across present diagnostic categories.
8. A failure to appreciate the broad market likely for drugs, which effect specific pathologic domains (not disease specific). Schizophrenia is a disease that has symptoms, which overlap with other disease entities. For example, gating sensory information deficits have been identified in a variety of other diseases, as have cognitive impairments. Once a drug is shown to have beneficial effects in one disease entity, there is a high probability that that drug may also have beneficial effects in another entity with a similar phenotype. The development of adjunctive therapies that have utility in several disease entities could provide pharmaceutical companies with other outlets for their products. These include but are not limited to attention, motivation, reward response, affect disturbance, processing speed, and social cognition. New approaches to FDA for approval for a domain indication rather than a schizophrenia indication may facilitate exploration of efficacy across disease classes.
9. The FDA's system of disease as an indication. Until now, the FDA has reviewed applications for a schizophrenia class indication. This works well for antipsychotic drug applications. However, the FDA can review applications for an indication that may cross disease lines. For example, analgesic drugs. The FDA is prepared to take the first step in recognizing non-psychotic domains as indications in schizophrenia. Representatives of the FDA have participated in developing clinical trials guidelines for addressing an indication for cognition and for negative symptoms (Buchanan et al, 2005; Kirkpatrick et al, 2006).
Attention to these nine issues will facilitate the development of drugs with efficacy for pathological domains other than psychosis. Success is likely to substantially improve functional outcomes, a challenge not met by current drugs. Particularly encouraging in this regard is the progress associated with the NIMH MATRICS project (Stover et al, 2007), the identification of potential molecular targets for therapeutic development in schizophrenia (Gray and Roth, 2007), and involvement of industry in these developments (Breier et al, 2007). Information about the molecular targets and approaches being taken with these trials can also be obtained from the Schizophrenia Research Forum website (http://www.schizophreniaforum.org).
General Summary
The era of psychopharmacology developed in the same time frame as international emphasis on disease classification and highly specifiable diagnostic criteria. The single-disease paradigm was dominant, and differential diagnosis came to rely very extensively on psychotic symptoms, especially reality distortion symptoms. Treatment effects in schizophrenia clinical trials have been mainly evaluated in relation to psychosis, or to global or total scores on rating instrument. This encouraged the development of antipsychotic drugs while neglecting other pathological domains. Despite unequivocal antipsychotic efficacy using this approach, the long-term functional outcomes have not changed much. The treatment discovery process has produced a series of drugs acting at the D2 receptor, and no drug has been approved for marketing with a novel molecular target. This has been noted as a general problem for the pharmaceutical industry (Drews, 2000; Dutta and Garner, 2003; Mills, 2006; Norrby et al, 2005; Carpenter, 2004; Scolnick, 2004; Korn and Stanski, 2005) and applies also to developing drugs for depression and other mental illnesses.
An alternative paradigm identifies domains of pathology within the schizophrenia construct and proposes independent therapeutic development for each domain. The two leading unmet therapeutic needs in schizophrenia, cognition impairment and primary negative symptoms, come into focus in this paradigm. This moves the challenge from developing drugs for schizophrenia to developing drugs for pathological domains within the schizophrenia syndrome. A shift in regulatory focus is also required, but substantial progress has been made within the FDA in preparation to evaluate a drug for an indication within schizophrenia. Clinical trial designs for this purpose relating to cognition and to negative symptoms have been presented with FDA involvement (Buchanan et al, 2005; Kirkpatrick et al, 2006). Therapeutic discovery for these domains will be based on different developmental models, will require new approaches to early drug evaluations and proof of concept testing, and new designs for randomized clinical trial. Specifying elements of these domains can facilitate animal and human model development. The current status in these fields has been explored in recent NIMH workshops (Buchanan et al, 2005; Geyer and Heinssen, 2005; Kirkpatrick et al, 2006). New knowledge on genotype/endophenotype relationships will create another paradigm in which to conceptualize novel drug development (Braff and Light, 2005; Braff et al, 2007; Thaker, 2007).
Polypharmacy is a prevalent and worrisome practice in schizophrenia therapeutics. At present this usually involves add-on administration of more than one drug from the dopamine antagonist class (assuring increased adverse effects without evidence of increased efficacy). If drugs are discovered for pathological aspects of schizophrenia other than psychosis, the approach would be comedication with each drug having a different mechanism of action and administered for a different clinical target. The issue is not polypharmacy or add-on therapy. Rather, independent domains of pathology will require novel drugs, which specifically target an aspect of schizophrenia. If successful, the field would evolve comedication strategies with antipsychotic drugs for psychosis, anti-negative symptom drugs for this pathology, cognition-enhancing drugs for cognition, and so forth. Whether a drug developed for one domain will be cross-reactive with other domains, or whether synergism between mechanisms occurs must await the development of efficacious compounds.
A practical question remains as to whether domains of pathology replace or augment current syndrome classes. There is insufficient evidence at present to determine whether, for example, anergia observed in cases drawn from schizophrenia and major depressive disorder will share the same causal pathway. Or whether cognitive impairment in bipolar disorder and schizophrenia share the same latent structure. Nonetheless, these and other pathological features cut across current diagnostic boundaries at the clinical manifestation level. Therapeutic efficacy may follow the pathological domains rather than being syndrome specific. This is clearly the case for antipsychotic efficacy. However, in the absence of evidence for domain pathophysiological similarity across diagnostic classes, the current syndrome nosology is likely to continue in DSM-V and ICD-11. What will be new is an effort to deconstruct psychotic illnesses (Allardyce et al, 2007; Dutta et al, 2007; Keller et al, 2007; Vieta and Phillips, 2007; Owen et al, 2007; Tamminga and Davis, 2007) into key dimensions or domains, and identify these dimensions as therapeutic targets. The FDA may grant an indication for a domain within a syndrome, and may still require evidence of efficacy for the same domain in another syndrome. In this regard, pathological domains remain disease-class bound in initial development. Unlike pain, where an analgesic with efficacy can be marketed for pain in various disease conditions, a pathological domain indication may be restricted to cases in the parent syndrome who manifest the domain. But testing efficacy hypotheses in other syndromes will be facilitated. It seems likely that a therapeutic mechanism related to final common pathways, will have efficacy across syndrome boundaries. It is also possible that the therapeutic mechanism may relate to specific pathophysiology, which is unique to a syndrome. Advancing therapeutic discovery for domains of pathology will greatly enhance our understanding of the pathologies, which are disease-specific and the pathologies, which define the porous boundaries of our present classification system.
References
Adams CE, Rathbone J, Thornley B, Clarke M, Borrill J, Wahlbeck K et al (2005). Chlorpromazine for schizophrenia: a Cochrane systematic review of 50 years of randomised controlled trials. BMC Med 17: 15.
Agid Y, Buzsaki G, Diamond DM, Frackowiak R, Giedd J, Girault J-A et al (2007). How can drug discovery for psychiatric disorders be improved? Nature Rev Drug Discovery 6: 189–201.
Allardyce J, Gaebel W, Zielasek J, van Os J (2007). Deconstructing psychosis conference February 2006: the validity of schizophrenia and alternative approaches to the classification of psychosis. Schizophr Bull 33: 863–867.
Amar S, Jones BC, Nadri C, Kozlovsky N, Belmaker RH, Agam G (2004). Genetic correlational analysis of glycogen synthase kinase-3 beta and prepulse inhibition in inbred mice. Genes Brain Behav 3: 178–180.
Aokhin AP, Heath AC, Myers E, Ralano A, Wood S (2003). Genetic influences on prepulse inhibition of startle reflex in humans. Neurosci Lett 353: 45–48.
Arolt V, Lencer R, Nolte A, Muller-Myhsok B, Purmann S, Schurmann M et al (1996). Eye tracking dysfunction is a putative phenotypic susceptibility marker of schizophrenia and maps to a locus on chromosome 6p in families with multiple occurrence of the disease. Am J Med Genet 67: 564–579.
Auquier P, Lancon C, Rouillon F, Lader M, Holmes C (2006). Mortality in schizophrenia. Pharmacoepidemiol Drug Saf 15: 873–879.
Awad AG, Voruganti LN (2004). New antipsychotics, compliance, quality of life, and subjective tolerability—are patients better off? Can J Psychiatry 49: 297–302.
Ballmaier M, Zoli M, Leo G, Agnati LF, Spano P (2002). Preferential alterations in the mesolimbic dopamine pathway of heterozygous reeler mice: an emerging animal-based model of schizophrenia. Eur J Neurosci 15: 1197–1205.
Bannerman DM, Deacon RM, Brady S, Bruce A, Sprengel R, Seeburg PH et al (2004). A comparison of GluR-A-deficient and wild-type mice on a test battery assessing sensorimotor, affective, and cognitive behaviors. Behav Neurosci 118: 643–647.
Beaulieu JM, Sotnikova TD, Marion S, Lefkowitz RJ, Gainetdinov RR, Caron MG (2005). An Akt/beta-arrestin 2/PP2A signaling complex mediates dopaminergic neurotransmission and behavior. Cell 122: 261–273.
Beglopoulos V, Montag-Sallaz M, Rohlmann A, Piechotta K, Ahmad M, Montag D et al (2005). Neurexophilin 3 is highly localized in cortical and cerebellar regions and is functionally important for sensorimotor gating and motor coordination. Mol Cell Biol 25: 7278–7288.
Bellack AS (2003). Psychosocial rehabilitation. In: Tasman A, Lieberman J, Kay J (eds). Psychiatry, 2nd edn. Wiley: London, pp 1853–1864.
Berman I, Viegner B, Merson A, Allan E, Pappas D, Green AI (1997). Differential relationships between positive and negative symptoms and neuropsychological deficits in schizophrenia. Schizophr Res 25: 1–10.
Berretta S, Munno DW, Benes FM (2001). Amygdalar activation alters the hippocampal GABA system: ‘partial’ modelling for postmortem changes in schizophrenia. J Comp Neurol 431: 129–138.
Bielsky IF, Hu SB, Ren X, Terwilliger EF, Young LJ (2005). The V1a vasopressin receptor is necessary and sufficient for normal social recognition: a gene replacement study. Neuron 47: 503–513.
Bleuler E (1950). Dementia Praecox or the Group of Schizophrenias Zinkin J (trans.) International Universities Press: New York.
Boksa P (2004). Animal models of obstetric complications in relation to schizophrenia. Brain Res Brain Res Rev 45: 1–17.
Bola JR (2006). Medication-free research in early episode schizophrenia: evidence of long-term harm? Schizophr Bull 32: 288–296.
Borrell J, Vela JM, Arevalo-Martin A, Molina-Holgado E, Guaza C (2002). Prenatal immune challenge disrupts sensorimotor gating in adult rats. Implications for the etiopathogenesis of schizophrenia. Neuropsychopharmacology 26: 204–215.
Braff DL, Freedman R, Schork NJ, Gottesman II (2007). Deconstructing schizophrenia: an overview of the use of endophenotypes in order to understand a complex disorder. Schizophr Bull 33: 21–32.
Braff DL, Light GA (2005). The use of neurophysiological endophenotypes to understand the genetic basis of schizophrenia. Dialogues Clin Neurosci 7: 125–135.
Breier A, Alphs L, Binneman B (2007). Wayne Fenton's impact on industry. Schizophr Bull 33: 1154–1155.
Brody SA, Conquet F, Geyer MA (2003). Disruption of prepulse inhibition in mice lacking mGluR1. Eur J Neurosci 18: 3361–3366.
Brody SA, Dulawa SC, Conquet F, Geyer MA (2004). Assessment of a prepulse inhibition deficit in a mutant mouse lacking mGlu5 receptors. Mol Psychiatry 9: 35–41.
Buchanan RW, Carpenter WT (1994). Domains of psychopathology: an approach to the reduction of heterogeneity in schizophrenia. J Nerv Ment Dis 182: 193–204.
Buchanan RW, Davis M, Goff D, Green MF, Keefe RSE, Leon AC et al (2005). A summary of the FDA-NIMH-MATRICS workshop on clinical trial design for neurocognitive drugs for schizophrenia. Schizophr Bull 31: 5–19.
Carlsson A, Lindqvist M (1963). Effect of chlorpromazine and haloperidol on formation of 3-methoxytyramine and normetanephrine in mouse brain. Acta Pharmacol Toxicol 20: 140–144.
Carpenter Jr WT (2004). Clinical constructs and therapeutic discovery. Schizophr Res 72: 69–73.
Carpenter WT (2006). The schizophrenia paradigm: a hundred-year challenge (editorial). J Nerv Ment Dis 194: 639–643.
Carpenter WT, Bartko JJ, Strauss JS, Hawk AB (1978). Signs and symptoms as predictors of outcome: a Report from the International Pilot Study of Schizophrenia. Am J Psychiatry 135: 940–945.
Carpenter WT, Buchanan RW, Kirkpatrick B, Tamminga CA, Wood F (1993). Strong inference, theory falsification, and the neuroanatomy of schizophrenia. Arch Gen Psychiatry 50: 825–831.
Clapcote SJ, Lipina TV, Millar JK, Mackie S, Christie S, Ogawa F et al (2007). Behavioral phenotypes of Disc1 missense mutations in mice. Neuron 54: 387–402.
Cohen AS, Saperstein AM, Gold JM, Kirkpatrick B, Carpenter Jr WT, Buchanan RW (2007). Neuropsychology of the deficit syndrome: new data and meta-analysis of findings to date. Schizophr Bull 33: 1201–1212.
Colloca L, Benedetti F (2005). Placebos and painkillers: is mind as real as matter? Nat Rev Neurosci 6: 545–552.
Colton CW, Manderscheid RW (2006). Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis 3: A42.
Conley RR (1998). Optimizing treatment with clozapine. J Clin Psychiatry 59 (Suppl 3): 44–48.
Conley RR, Kelly DL (2002). Current status of antipsychotic treatment. Curr Drug Targets CNS Neurol Disord 1: 123–128.
Costa E, Davis J, Pesold C, Tueting P, Guidotti A (2002). The heterozygote reeler mouse as a model for the development of a new generation of antipsychotics. Curr Opin Pharmacol 2: 56–62.
DAdamo P, Welzl H, Papadimitriou S, Raffaele di Barletta M, Tiveron C, Tatangelo L et al (2002). Deletion of the mental retardation gene Gdi1 impairs associative memory and alters social behavior in mice. Hum Mol Genet 11: 2567–2580.
Daenen EW, Wolterink G, Gerrits MA, Van Ree JM (2002). The effects of neonatal lesions in the amygdala or ventral hippocampus on social behaviour later in life. Behav Brain Res 136: 571–582.
Daenen EW, Wolterink G, Van Der Heyden JA, Kruse CG, Van Ree JM (2003). Neonatal lesions in the amygdala or ventral hippocampus disrupt prepulse inhibition of the acoustic startle response; implications for an animal model of neurodevelopmental disorders like schizophrenia. Eur Neuropsychopharmacol 13: 187–197.
Davies MA, Sheffler DJ, Roth BL (2004). Aripiprazole: a novel atypical antipsychotic drug with a uniquely robust pharmacology. CNS Drug Rev 10: 317–336.
Dirks A, Groenink L, Westphal KG, Olivier JD, Verdouw PM, van der Gugten J et al (2003). Reversal of startle gating deficits in transgenic mice overexpressing corticotropin-releasing factor by antipsychotic drugs. Neuropsychopharmacol 28: 1790–1798.
Drews J (2000). Drug discovery: a historical perspective. Science 287: 1960–1964.
Duan X, Chang JH, Ge S, Faulkner RL, Kim JY, Kitabatake Y et al (2007). Disrupted-in-schizophrenia 1 regulates integration of newly generated neurons in the adult brain. Cell 130: 1146–1158.
Dutta AS, Garner A (2003). The pharmaceutical industry and research in 2002 and beyond. Drug News Perspect 16: 637–648.
Dutta R, Greene T, Addington J, McKenzie K, Phillips M, Murray RM (2007). Biological, life course, and cross-cultural studies all point toward the value of dimensional and developmental ratings in the classification of psychosis. Schizophr Bull 33: 868–876.
Eichenbaum H, Fortin NJ (2005). Bridging the gap between brain and behavior: cognitive and neural mechanisms of episodic memory. J Exp Analysis Behav 84: 619–629.
Ellenbroek BA, Cools AR (2002). Apomorphine susceptibility and animal models for psychopathology: genes and environment. Behav Genet 32: 349–361.
Ellenbroek BA, van den Kroonenberg PT, Cools AR (1998). The effects of an early stressful life event on sensorimotor gating in adult rats. Schizophr Res 30: 251–260.
Elmer GI, Sydnor J, Guard H, Hercher E, Vogel MW (2004). Altered prepulse inhibition in rats treated prenatally with the antimitotic Ara-C: an animal model for sensorimotor gating deficits in schizophrenia. Psychopharmacology (Berl) 174: 177–189.
Erbel-Sieler C, Dudley C, Zhou Y, Wu X, Estill SJ, Han T et al (2004). Behavioral and regulatory abnormalities in mice deficient in the NPAS1 and NPAS3 transcription factors. Proc Natl Acad Sci USA 101: 13648–13653.
Eyles D, Almeras L, Benech P, Patatian A, Mackay-Sim A, McGrath J et al (2007). Developmental vitamin D deficiency alters the expression of genes encoding mitochondrial, cytoskeletal and synaptic proteins in the adult rat brain. J Steroid Biochem Mol Biol 103: 538–545.
Eyles DW, Rogers F, Buller K, McGrath JJ, Ko P, French K et al (2006). Developmental vitamin D (DVD) deficiency in the rat alters adult behaviour independently of HPA function. Psychoneuroendocrinol 31: 958–964.
Eysenck HJ, Wakefield Jr JA, Friedman AF (1983). Diagnosis and clinical assessment: the DSM III. Annu Rev Psychol 34: 167–193.
Fatemi SH, Emamian ES, Kist D, Sidwell RW, Nakajima K, Akhter P et al (1999). Defective corticogenesis and reduction in reelin immunoreactivity in cortex and hippocampus of prenatally infected neonatal mice. Mol Psychiatry 4: 145–154.
Fatemi SH, Pearce DA, Brooks AI, Sidwell RW (2005). Prenatal viral infection in mouse causes differential expression of genes in brains of mouse progeny: a potential animal model for schizophrenia and autism. Synapse 57: 91–99.
Featherstone RE, Rizos Z, Nobrega JN, Kapur S, Fletcher PJ (2007). Gestational methylazoxymethanol acetate treatment impairs select cognitive functions: parallels to schizophrenia. Neuropsychopharmacol 32: 483–492.
Ferguson JN, Aldag JM, Insel TR, Young LJ (2001). Oxytocin in the medial amygdala is essential for social recognition in the mouse. J Neurosci 21: 8278–8285.
Flagstad P, Mork A, Glenthoj BY, van Beek J, Michael-Titus AT, Didriksen M (2004). Disruption of neurogenesis on gestational day 17 in the rat causes behavioral changes relevant to positive and negative schizophrenia symptoms and alters amphetamine-induced dopamine release in nucleus accumbens. Neuropsychopharmacol 29: 2052–2064.
Fradley RL, O'Meara GF, Newman RJ, Andrieux A, Job D, Reynolds DS (2005). STOP knockout and NMDA NR1 hypomorphic mice exhibit deficits in sensorimotor gating. Behav Brain Res 163: 257–264.
Freedman R, Coon H, Myles-Worsley M, Orr-Urtreger A, Olincy A, Davis A et al (1997). Linkage of a neurophysiological deficit in schizophrenia to a chromosome 15 locus. Proc Natl Acad Sci USA 94: 587–592.
Geddes J, Freemantle N, Harrison P, Bebbington P, National Schizophrenia Guideline Development Group (2005). Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis. BMJ 321: 1371–1376.
Geschwind DH, Miller BL, DeCarli C, Carmelli D (2002). Heritability of lobar brain volumes in twins supports genetic models of cerebral laterality and handedness. Proc Natl Acad Sci USA 99: 3176–3181.
Geyer MA, Heinssen R (2005). New approaches to measurement and treatment research to improve cognition in schizophrenia. Schizophr Bull 31: 806–809.
Geyer MA, Wilkinson LS, Humby T, Robbins TW (1993). Isolation rearing of rats produces a deficit in prepulse inhibition of acoustic startle similar to that in schizophrenia. Biol Psych 34: 361–372.
Gisabella B, Bolshakov VY, Benes FM (2005). Regulation of synaptic plasticity in a schizophrenia model. Proc Natl Acad Sci USA 102: 13301–13306.
Glynn D, Drew CJ, Reim K, Brose N, Morton AJ (2005). Profound ataxia in complexin I knockout mice masks a complex phenotype that includes exploratory and habituation deficits. Hum Mol Genet 14: 2369–2385.
Gogos JA, Morgan M, Luine V, Santha M, Ogawa S, Pfaff D et al (1998). Catechol-O-methyltransferase-deficient mice exhibit sexually dimorphic changes in catecholamine levels and behavior. Proc Natl Acad Sci 95: 9991–9996.
Gogos JA, Santha M, Takacs Z, Beck KD, Luine V, Lucas LR et al (1999). The gene encoding proline dehydrogenase modulates sensorimotor gating in mice. Nat Genet 21: 434–439.
Gold JM, Harvey PD (1993). Cognitive deficits in schizophrenia. Psychiatr Clin North Am 16: 295–312.
Golub MS, Germann SL, Lloyd KC (2004). Behavioral characteristics of a nervous system-specific erbB4 knock-out mouse. Behav Brain Res 153: 159–170.
Gourevitch R, Rocher C, Le Pen G, Krebs MO, Jay TM (2004). Working memory deficits in adult rats after prenatal disruption of neurogenesis. Behav Pharmacol 15: 287–292.
Gray JA, Roth BL (2007). Molecular targets for treating cognitive dysfunction in schizophrenia. Schizophr Bull 33: 1100–1119.
Green MF, Kern RS, Heaton RK (2004). Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res 72: 41–51.
Grillet N, Pattyn A, Contet C, Kieffer BL, Goridis C, Brunet JF (2005). Generation and characterization of Rgs4 mutant mice. Mol Cell Biol 25: 4221–4228.
Haller J, Szirmai M, Varga B, Ledent C, Freund TF (2005). Cannabinoid CB1 receptor-dependent effects of the NMDA antagonist phencyclidine in the social withdrawal model of schizophrenia. Behav Pharmacol 16: 415–422.
Hanlon FM, Sutherland RJ (2000). Changes in adult brain and behavior caused by neonatal limbic damage: implications for the etiology of schizophrenia. Behav Brain Res 107: 71–83.
Hans A, Bajramovic JJ, Syan S, Perret E, Dunia I, Brahic M et al (2004). Persistent, noncytolytic infection of neurons by Borna disease virus interferes with ERK 1/2 signaling and abrogates BDNF-induced synaptogenesis. FASEB J 18: 863–865.
Harrison PJ, Weinberger DR (2004). Schizophrenia genes, gene expression, and neuropathology: on the matter of their convergence. Mol Psychiatry 10: 40–68.
Harvey PD, Koren D, Reichenberg A, Bowie CR (2006). Negative symptoms and cognitive deficits: what is the nature of their relationship? Schizophr Bull 32: 250–258.
Hegarty JD, Baldessarini RJ, Tohen M, Waternaux C, Oepen G (1994). One hundred years of schizophrenia: a meta-analysis of the outcome literature. Am J Psychiatry 151: 1409–1416.
Heidbreder CA, Weiss IC, Domeney AM, Pryce C, Homberg J, Hedou G et al (2000). Behavioral, neurochemical and endocrinological characterization of the early social isolation syndrome. Neuroscience 100: 749–768.
Hennah W, Tuulio-Henriksson A, Paunio T, Ekelund J, Varilo T, Partonen T et al (2005). A haplotype within the DISC1 gene is associated with visual memory functions in families with a high density of schizophrenia. Mol Psychiatry 10: 1097–1103.
Hennekens CH, Hennekens AR, Hollar D, Casey DE (2005). Schizophrenia and increased risks of cardiovascular disease. Am Heart J 150: 1115–1121.
Hikida T, Jaaro-Peled H, Seshadri S, Oishi K, Hookway C, Kong S et al (2007). From the cover: dominant-negative DISC1 transgenic mice display schizophrenia-associated phenotypes detected by measures translatable to humans. Proc Natl Acad Sci USA 104: 14501–14506.
Hong LE, Mitchell BD, Avila MT, Adami H, McMahon RP, Thaker GK (2006). Familial aggregation of eye tracking endophenotypes in schizophrenia families. Arch Gen Psychiatry 63: 259–264.
Huotari M, Garcia-Horsman JA, Karayiorgou M, Gogos JA, Mannisto PT (2004). D-amphetamine responses in catechol-O-methyltransferase (COMT) disrupted mice. Psychopharmacology (Berl) 172: 1–10.
Jentsch JD, Roth RH (1999). The neuropsychopharmacology of phencyclidine: from NMDA receptor hypofunction to the dopamine hypothesis of schizophrenia. Neuropsychopharmacol 20: 201–225.
Jones PB, Barnes TR, Davies L, Dunn G, Lloyd H, Hayhurst KP et al (2006). Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry 63: 1079–1087.
Kane J, Honigfeld G, Singer J, Meltzer M (1988). Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry 45: 789–796.
Kapur S, Mamo D (2003). Half a century of antipsychotics and still a central role for dopamine D2 receptors. Prog Neuropsychopharmacol Biol Psychiatry 27: 1081–1090.
Keller J, Schatzberg AF, Maj M (2007). Current issues in the classification of psychotic major depression. Schizophr Bull 33: 877–885.
Kesby JP, Burne TH, McGrath JJ, Eyles DW (2006). Developmental vitamin D deficiency alters MK 801-induced hyperlocomotion in the adult rat: an animal model of schizophrenia. Bio Psych 60: 591–596.
Kinney GG, Burno M, Campbell UC, Hernandez LM, Rodriguez D, Bristow LJ et al (2003). Metabotropic glutamate subtype 5 receptors modulate locomotor activity and sensorimotor gating in rodents. J Pharmacol Exp Ther 306: 116–123.
Kinnunen AK, Koenig JI, Bilbe G (2003). Repeated variable prenatal stress alters pre- and postsynaptic gene expression in the rat frontal pole. J Neurochem 86: 736–748.
Kirkpatrick B, Fenton WS, Carpenter Jr WT, Marder SR (2006). The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull 32: 214–219.
Kirkpatrick B, Kopelowicz A, Buchanan RW, Carpenter Jr WT (2000). Assessing the efficacy of treatments for the deficit syndrome of schizophrenia. Neuropsychopharmacology 22: 303–310.
Koenig JI, Elmer GI, Shepard PD, Lee PR, Mayo C, Joy B et al (2005). Prenatal exposure to a repeated variable stress paradigm elicits behavioral and neuroendocrinological changes in the adult offspring: potential relevance to schizophrenia. Behav Brain Res 156: 251–261.
Koike H, Arguello PA, Kvajo M, Karayiourgou M, Gogos JA (2006). Disc 1 is mutated in the 129S6/SvEv strain and modulates working memory in mice. Proc Natl Acad Sci USA 103: 3693–3697.
Korn D, Stanski DR (eds) (2005). Drug Development Science. Obtstacles and opportunities for collaboration among academia, industry and government. Report of an Invitational Conference Organized by The Association of American Medical Colleges, Food and Drug Administration, Center for Drug Development Science, at the University of California, San Francisco. January 13–14, 2005 Washington, DC.
Kraepelin E (1919). Translated by Barclay RM, Edinburgh E & Livingstone S Dementia Praecox and Paraphrenia.
Krezel W, Ghyselinck N, Samad TA, Dupe V, Kastner P, Borrelli E et al (1998). Impaired locomotion and dopamine signaling in retinoid receptor mutant mice. Science 279: 863–867.
Kruger DD, Howell JL, Hebert BF, Olausson P, Taylor JR, Nairn AC (2006). Assessment of cognitive function in the heterozygous reeler mouse. Psychopharmacology 189: 95–104.
Lacroix L, Spinelli S, White W, Feldon J (2000). The effects of ibotenic acid lesions of the medial and lateral prefrontal cortex on latent inhibition, prepulse inhibition and amphetamine-induced hyperlocomotion. Neuroscience 97: 459–468.
Langfeldt G (1937). The Prognosis in Schizophrenia and the Factors Influencing the Course of the Disease. E Munksgaard: Copenhagen.
Langfeldt G (1939). The Schizophrenic States. E Munksgaard: Copenhagen.
Laruelle M, Abi-Dargham A, van Dyck CH, Gil R, D'Souza CD, Erdos J et al (1996). Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proc Natl Acad Sci USA 93: 9235–9240.
Lee PR, Brady D, Shapiro RA, Dorsa DM, Koenig JI (2005). Social interaction deficits caused by chronic phencyclidine administration are reversed by oxytocin. Neuropsychopharmacology 30: 1883–1894 (published online 1882/1816/1805).
Lee PR, Brady D, Shapiro RA, Dorsa DM, Koenig JI (2007). Prenatal stress generates deficits in rat social behavior: reversal by oxytocin. Brain Res (available at http://dx.doi.org/10.1016/j.brainres.2007.04.042).
Leonard S, Gault J, Hopkins J, Logel J, Vianzon R, Short M et al (2002). Association of promoter variants in the alpha7 nicotinic acetylcholine receptor subunit gene with an inhibitory deficit found in schizophrenia. Arch Gen Psychiatry 59: 1085–1096.
Lewis SW, Barnes TRE, Davies L, Murray RM, Dunn G, Hayhurst KP et al (2006). Randomized controlled trial of effect of prescription of clozapine versus other second-generation antipsychotic drugs in resistant schizophrenia. Schizophr Bull 32: 715–723.
Lieberman JA (2007). Effectiveness of antipsychotic drugs in patients with chronic schizophrenia: efficacy, safety and cost outcomes of CATIE and other trials. J Clin Psychiatry 68: e04.
Lieberman JA, Phillips M, Gu H, Stroup S, Zhang P, Kong L et al (2003a). Atypical and conventional antipsychotic drugs in treatment-naïve first-episode schizophrenia: A 52-week randomized trial of clozapine vs chlorpormazine. Neuropsychopharmacology 28: 995–1003.
Lieberman JA, Stroup TS, mcEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al., CATIE Investigators (2005). Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 353: 1209–1223.
Lieberman JA, Tollefson G, Tohen M, Green AI, Gur RE, Kahn R, et al., HGDH Study Group (2003b). Comparative efficacy and safety of atypical and conventional antipsychotic drugs in first-episode psychosis: a randomized, double-blind trial of olanzapine versus haloperidol. Am J Psychiatry 160: 1396–1404.
Lijam N, Paylor R, McDonald MP, Crawley JN, Deng CX, Herrup K et al (1997). Social interaction and sensorimotor gating abnormalities in mice lacking Dvl1. Cell 90: 895–905.
Lipska BK (2004). Using animal models to test a neurodevelopmental hypothesis of schizophrenia. J Psychiatry Neurosci 29: 282–286.
Lipska BK, al-Amin HA, Weinberger DR (1998). Excitotoxic lesions of the rat medial prefrontal cortex. Effects on abnormal behaviors associated with neonatal hippocampal damage. Neuropsychopharmacology 19: 451–464.
Lipska BK, Weinberger DR (2000). To model a psychiatric disorder in animals: schizophrenia as a reality test. Neuropsychopharmacology 23: 223–239.
Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL (eds) (2006). Global Burden of Disease. The World Bank/Oxford University Press: Washington DC/New York, NY.
Madras BK, Miller GM, Fischman AJ (2005). The dopamine transporter and attention-deficit/hyperactivity disorder. Biol Psychiatry 57: 1397–1409.
Matthysse S, Holzman PS, Gusella JF, Levy DL, Harte CB, Jorgensen A et al (2004). Linkage of eye movement dysfunction to chromosome 6p in schizophrenia: additional evidence. Am J Med Genet B Neuropsychiatr Genet 128: 30–36.
Matza LS, Buchanan R, Purdon S, Brewster-Jordan J, Zhao Y, Revicki DA (2006). Measuring changes in functional status among patients with schizophrenia: the link with cognitive impairment. Schizophr Bull 32: 666–678.
Mauskopf J, Muroff M, Gibson PJ, Grainger DL (2002). Estimating the costs and benefits of new drug therapies: atypical antipsychotic drugs for schizophrenia. Schizophr Bull 28: 619–635.
McEvoy JP, Lieberman JA, Stroup TS, Davis SM, Meltzer HY, Rosenheck RA, et al., CATIE Investigators (2006). Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone patients with chronic schizophernia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry 163: 600–610.
Metz GA, Schwab ME (2004). Behavioral characterization in a comprehensive mouse test battery reveals motor and sensory impairments in growth-associated protein-43 null mutant mice. Neuroscience 129: 563–574.
Meyer U, Feldon J, Schedlowski M, Yee BK (2005). Towards an immuno-precipitated neurodevelopmental animal model of schizophrenia. Neurosci Biobehav Rev 29: 913–947.
Meyer U, Schwendener S, Feldon J, Yee BK (2006). Prenatal and postnatal maternal contributions in the infection model of schizophrenia. Exp Brain Res 173: 243–257.
Mills SD (2006). When will the genomics investment pay off for antibacterial discovery? Biochem Pharmacol 71: 1096–1102.
Miner LA, Ostrander M, Sarter M (1997). Effects of ibotenic acid-induced loss of neurons in the medial prefrontal cortex of rats on behavioral vigilance: evidence for executive dysfunction. J Psychopharmacol 11: 169–178.
Miyakawa T, Leiter LM, Gerber DJ, Gainetdinov RR, Sotnikova TD, Zeng H et al (2003). Conditional calcineurin knockout mice exhibit multiple abnormal behaviors related to schizophrenia. Proc Natl Acad Sci USA 100: 8987–8992.
Mohn AR, Gainetdinov RR, Caron MG, Koller BH (1999). Mice with reduced NMDA receptor expression display behaviors related to schizophrenia. Cell 98: 427–436.
Moore H, Jentsch JD, Ghajarnia M, Geyer MA, Grace AA (2006). A neurobehavioral systems analysis of adult rats exposed to methylazoxymethanol acetate on E17: implications for the neuropathology of schizophrenia. Biol Psych 60: 253–264.
Murray CJL, Lopez AD (eds) (1996). The global burden of disease and injury series, vol 1: a comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Harvard University Press: Cambridge, MA.
Newcomer JW, Hennekens CH (2007). Severe mental illness and risk of cardiovascular disease. JAMA 298: 1794–1796.
Norrby SR, Nord CE, Finch R, European Society of Clinical Microbiology and Infectious Diseases (2005). Lack of development of new antimicrobial drugs: a potential serious threat to public health. Lancet Infect Dis 5: 115–119.
Owen MJ, Craddock N, Jablensky A (2007). The genetic deconstruction of psychosis. Schizophr Bull 33: 905–911.
Palmer AA, Printz DJ, Butler PD, Dulawa SC, Printz MP (2004). Prenatal protein deprivation in rats induces changes in prepulse inhibition and NMDA receptor binding. Brain Res 996: 193–201.
Paterlini M, Zakharenko SS, Lai WS, Qin J, Zhang H, Mukai J et al (2005). Transcriptional and behavioral interaction between 22q11.2 orthologs modulates schizophrenia-related phenotypes in mice. Nat Neurosci 8: 1586–1594.
Paunio T, Tuulio-Henriksson A, Hiekkalinna T, Perola M, Varilo T, Partonen T et al (2004). Search for cognitive trait components of schizophrenia reveals a locus for verbal learning and memory on 4q and for visual working memory on 2q. Hum Mol Genet 13: 1693–1702.
Paylor R, McIlwain KL, McAninch R, Nellis A, Yuva-Paylor LA, Baldini A et al (2001). Mice deleted for the DiGeorge/velocardiofacial syndrome region show abnormal sensorimotor gating and learning and memory impairments. Hum Mol Genet 10: 2645–2650.
Petryshen TL, Kirby A, Hammer Jr RP, Purcell S, Singer JB, Hill AE et al (2005). Two QTLs for prepulse inhibition of startle identified on mouse chromosome 16 using chromosome substitution strains. Genetics 171: 1895–1904.
Pieper AA, Wu X, Han TW, Estill SJ, Dang Q, Wu LC et al (2005). The neuronal PAS domain protein 3 transcription factor controls FGF-mediated adult hippocampal neurogenesis in mice. Proc Natl Acad Sci USA 102: 14052–14057.
Pletnikov MV, Ayhan Y, Nikolskaia O, Xu Y, Ovanesov MV, Huang H et al (2007). Inducible expression of mutant human DISC1 in mice is associated with brain and behavioral abnormalities reminiscent of schizophrenia. Mol Psychiatry, published on-line September 11, 2007.
Pletnikov MV, Rubin SA, Vogel MW, Moran TH, Carbone KM (2002). Effects of genetic background on neonatal Borna disease virus infection-induced neurodevelopmental damage. I. Brain pathology and behavioral deficits. Brain Res 944: 97–107.
Podhorna J, Didriksen M (2004). The heterozygous reeler mouse: behavioural phenotype. Behav Brain Res 153: 43–54.
Rapoport JL, Addington AM, Frangou S, Psych MR (2005). The neurodevelopmental model of schizophrenia: update 2005. Mol Psychiatry 10: 434–449.
Reed TM, Repaske DR, Snyder GL, Greengard P, Vorhees CV (2002). Phosphodiesterase 1B knock-out mice exhibit exaggerated locomotor hyperactivity and DARPP-32 phosphorylation in response to dopamine agonists and display impaired spatial learning. J Neurosci 22: 5188–5197.
Rijsdijk FV, van Haren NE, Picchioni MM, McDonald C, Toulopoulou T, Pol HE et al (2005). Brain MRI abnormalities in schizophrenia: same genes or same environment? Psychol Med 35: 1399–1409.
Robbins TW (1998). Homology in behavioral pharmacology: an approach to animal models of human cognition. Behav Pharmacol 9: 509–519.
Rodriguiz RM, Chu R, Caron MG, Wetsel WC (2004). Aberrant responses in social interaction of dopamine transporter knockout mice. Behav Brain Res 148: 185–198.
Rojas P, Joodmardi E, Hang Y, Perlmann T, Ogren SO (2007). Adult mice with reduced Nurr1 expression: an animal model for schizophrenia. Mol Psychiatry 12: 756–766.
Rupp A, Keith S (1993). The costs of schizophrenia: assessing the burden. Psychiat Clin NA 16: 413–423.
Rybakowski JK, Borkowska A, Czerski PM, Hauser J (2001). Dopamine D3 receptor (DRD3) gene polymorphism is associated with the intensity of eye movement disturbances in schizophrenic patients and healthy subjects. Mol Psychiatry 6: 718–724.
Saha S, Chant D, Welham J, McGrath J (2005). A systematic review of the prevalence of schizophrenia. PLoS Med 2: e141.
Sams-Dodd F (1999). Phencyclidine in the social interaction test: an animal model of schizophrenia with face and predictive validity. Rev Neurosci 10: 59–90.
Schneider K (1959). Clinical Psychopathology Hamilton MW (trans.) Grune & Stratton Inc.: New York.
Schooler N, Rabinowitz J, Davidson M, Emsley R, Harvey PD, Kopala L, et al., Early Psychosis Global Working Group (2005). Risperidone and haloperidol in first-episode psychosis: a long-term randomized trial. Am J Psychiatry 162: 947–953.
Scolnick E (2004). Program to improve cognitive functioning in patients with schizophrenia: reflections. Schizophr Res 72: 75–77.
Seeman MV (2007). An outcome measure in schizophrenia: mortality. Can J Psychiatry 52: 55–60.
Seeman P (2002). Atypical antipsychotics: mechanism of action. Can J Psychiatry 47: 27–38.
Selemon LD, Wang L, Nebel MB, Csernansky JG, Goldman-Rakic PS, Rakic P (2005). Direct and indirect effects of fetal irradiation on cortical gray and white matter volume in the macaque. Biol Psychiatry 57: 83–90.
Shi L, Fatemi SH, Sidwell RW, Patterson PH (2003). Maternal influenza infection causes marked behavioral and pharmacological changes in the offspring. J Neurosci 23: 297–302.
Solbrig MV, Koob GF, Parsons LH, Kadota T, Horscroft N, Briese T et al (2000). Neurotrophic factor expression after CNS viral injury produces enhanced sensitivity to psychostimulants: potential mechanism for addiction vulnerability. J Neurosci 20: RC104.
Stefansson H, Sigurdsson E, Steinthorsdottir V, Bjornsdottir S, Sigmundsson T, Ghosh S et al (2002). Neuregulin 1 and susceptibility to schizophrenia. Am J Hum Genet 71: 877–892.
Stevens KE, Kem WR, Mahnir VM, Freedman R (1998). Selective alpha7-nicotinic agonists normalize inhibition of auditory response in DBA mice. Psychopharmacology (Berl) 136: 320–327.
Stover EL, Brady L, Marder SR (2007). New paradigms for treatment development. Schizophr Bull 33: 1093–1099.
Strauss JS, Carpenter JS, Bartko JJ (1974). Speculations on the processes that underlie schizophrenic symptoms and signs. Schizophr Bull 61–69, Winter.
Strauss JS, Carpenter WT (1977). Prediction of outcome in schizophrenia. III. Five-year outcome and its predictors: A Report from the International Pilot Study of Schizophrenia. Arch Gen Psychiatry 34: 159–163.
Swerdlow NR, Braff DL, Geyer MA (2000). Animal models of deficient sensorimotor gating: what we know, what we think we know, and what we hope to know soon. Behav Pharmacol 11: 185–204.
Swerdlow NR, Braff DL, Taaid N, Geyer MA (1994). Assessing the validity of an animal model of deficient sensorimotor gating in schizophrenic patients. Arch Gen Psych 51: 139–154.
Szumlinski KK, Lominac KD, Kleschen MJ, Oleson EB, Dehoff MH, Schwartz MK et al (2005). Behavioral and neurochemical phenotyping of Homer1 mutant mice: possible relevance to schizophrenia. Genes Brain Behav 4: 273–288.
Takayanagi Y, Yoshida M, Bielsky IF, Ross HE, Kawamata M, Onaka T et al (2005). Pervasive social deficits, but normal parturition, in oxytocin receptor-deficient mice. Proc Natl Acad Sci USA 102: 16096–16101.
Tamminga CA, Carlsson A (2002). Partial dopamine agonists and dopaminergic stabilizers in the treatment of psychosis. Curr Drug Targets CNS Neurol Disord 1: 141–147.
Tamminga CA, Carpenter Jr WT (1982). The DSM-III diagnosis of schizophrenic-like illness and the clinical pharmacology of psychosis. JNerv Ment Dis 170: 744–751.
Tamminga CA, Davis JM (2007). The neuropharmacology of psychosis. Schizophr Bull 33: 937–946.
Thaker GK (2007). Endophenotypic studies in schizophrenia: promise and challenges. Schizophr Bull 33: 1–2.
Thaker GK, Wonodi I, Avila MT, Hong LE, Stine OC (2004). Catechol-O-methyltransferase polymorphism and eye tracking in schizophrenia: a preliminary report. Am J Psychiatry 161: 2320–2322.
Thompson P, Cannon TD, Toga AW (2002). Mapping genetic influences on human brain structure. Ann Med 34: 523–536.
Trinh JV, Nehrenberg DL, Jacobsen JP, Caron MG, Wetsel WC (2003). Differential psychostimulant-induced activation of neural circuits in dopamine transporter knockout and wild type mice. Neuroscience 118: 297–310.
Tsai G, Ralph-Williams RJ, Martina M, Bergeron R, Berger-Sweeney J, Dunham KS et al (2004). Gene knockout of glycine transporter 1: characterization of the behavioral phenotype. Proc Natl Acad Sci USA 101: 8485–8490.
Tuulio-Henriksson A, Haukka J, Partonen T, Varilo T, Paunio T, Ekelund J et al (2002). Heritability and number of quantitative trait loci of neurocognitive functions in families with schizophrenia. Am J Med Genet 114: 483–490.
Varty GB, Geyer MA (1998). Effects of isolation rearing on startle reactivity, habituation, and prepulse inhibition in male Lewis, Sprague–Dawley, and Fischer F344 rats. Behav Neurosci 112: 1450–1457.
Velligan DI, Kern RS, Gold JM (2006). Cognitive rehabilitation for schizophrenia and the putative role of motivation and expectancies. Schizophr Bull 32: 474–485.
Vieta E, Phillips ML (2007). Deconstructing bipolar disorder: a critical review of its diagnostic validity and a proposal for DSM-V and ICD-11. Schizophr Bull 33: 886–892.
Wahlbeck K, Cheine M, Essali A, Adams C (1999). Evidence of clozapine's effectiveness in schizophrenia: a systematic review and meta-analysis of randomized trials. Am J Psychiatry 156: 990–999.
Weickert TW, Goldberg TE (2005). First- and second-generation antipsychotic medication and cognitive processing in schizophrenia. Curr Psychiatry Rep 7: 304–310.
Weiner I (2003). The ‘two-headed’ latent inhibition model of schizophrenia: modeling positive and negative symptoms and their treatment. Psychopharmacology (Berl) 169: 257–297.
Weiss IC, Di Iorio L, Feldon J, Domeney AM (2000). Strain differences in the isolation-induced effects on prepulse inhibition of the acoustic startle response and on locomotor activity. Behav Neurosci 114: 364–373.
Wersinger SR, Ginns EI, O'Carroll A-M, Lolait SJ, Young WSI (2002). Vasopressin V1b receptor knockout reduces aggressive behavior in male mice. Mol Psychiatry 7: 975–984.
Wilkinson LS, Dias R, Thomas KL, Augood SJ, Everitt BJ, Robbins TW et al (1997). Contrasting effects of excitotoxic lesions of the prefrontal cortex on the behavioural response to D-amphetamine and presynaptic and postsynaptic measures of striatal dopamine function in monkeys. Neuroscience 80: 717–730.
Wolinsky TD, Swanson CJ, Smith KE, Zhong H, Borowsky B, Seeman P et al (2007). The trace amine 1 receptor knockout mouse: an animal with relevance to schizophrenia. Genes Brain Behav 6: 628–639.
Wood GK, Tomasiewicz H, Rutishauser U, Magnuson T, Quirion R, Rochford J et al (1998). NCAM-180 knockout mice display increased lateral ventricle size and reduced prepulse inhibition of startle. Neuroreport 9: 461–466.
Wyatt RJ, Henter I, Leary MC, Taylor E (1995). An economic evaluation of schizophrenia—1991. Soc Psychiatry Psychiatr Epidiol 30: 196–205.
Yamauchi Y, Qin LH, Nishihara M, Sawada K, Kato K, Inoue S (2005). Vulnerability of synaptic plasticity in the complexin II knockout mouse to maternal deprivation stress. Brain Res 1056: 59–67.
Yee BK, Keist R, von Boehmer L, Studer R, Benke D, Hagenbuch N et al (2005). A schizophrenia-related sensorimotor deficit links a3-containing GABAA receptors to a dopamine hyperfunction. Proc Natl Acad Sci USA 102: 17154–17159.
Young DA, Waldo M, Rutledge III JH, Freedman R (1996). Heritability of inhibitory gating of the P50 auditory-evoked potential in monozygotic and dizygotic twins. Neuropsychobiology 33: 113–117.
Zhao Z, Ksiezak-Reding H, Riggio S, Haroutunian V, Pasinetti GM (2006). Insulin receptor deficits in schizophrenia and in cellular and animal models of insulin receptor dysfunction. Schizophr Res 84: 1–14.
Acknowledgements
The authors declare that over the past 3 years WTC has received compensation from Lilly, Janssen, Pfizer, Solvay/Wyeth, Merck, McNeil, and Astra Zeneca and JIK has received no compensation from any pharmaceutical company over the past 3 years, but received an investigator initiated grant from Janssen Pharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCLOSURE/CONFLICT OF INTEREST
The authors declare that this work was commissioned by the Institute of Medicine and partially funded by NIH P30 MH068580 (WTC) and NIH R01 MH073826 (JIK). VA Capitol Network (VISN 5) Mental Illness Research, Education, and Clinical Center (MIRECC), and USPHS Grants DA09406 and DA 76013 from the National Institute of Drug Abuse (WTC).
Rights and permissions
About this article
Cite this article
Carpenter, W., Koenig, J. The Evolution of Drug Development in Schizophrenia: Past Issues and Future Opportunities. Neuropsychopharmacol 33, 2061–2079 (2008). https://doi.org/10.1038/sj.npp.1301639
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301639
Keywords
This article is cited by
-
Psychosis superspectrum I: Nosology, etiology, and lifespan development
Molecular Psychiatry (2024)
-
Methylation pattern and mRNA expression of synapse-relevant genes in the MAM model of schizophrenia in the time-course of adolescence
Schizophrenia (2022)
-
GABAA and NMDA receptor density alterations and their behavioral correlates in the gestational methylazoxymethanol acetate model for schizophrenia
Neuropsychopharmacology (2022)
-
Assessing olfactory, memory, social and circadian phenotypes associated with schizophrenia in a genetic model based on Rim
Translational Psychiatry (2021)
-
Study of the chromatographic behavior of selected antipsychotic drugs on RP-TLC based on quantitative structure–retention relationships
Journal of the Iranian Chemical Society (2019)