Abstract
Previously the NMDA (N-methyl-D-aspartate) receptor (NMDAR) antagonist ketamine was shown to disrupt generation of the auditory event-related potential (ERP) mismatch negativity (MMN) and the performance of an ‘AX’-type continuous performance test (AX-CPT)—measures of auditory and visual context-dependent information processing—in a similar manner as observed in schizophrenia. This placebo-controlled study investigated effects of the 5-HT2A receptor agonist psilocybin on the same measures in 18 healthy volunteers. Psilocybin administration induced significant performance deficits in the AX-CPT, but failed to reduce MMN generation significantly. These results indirectly support evidence that deficient MMN generation in schizophrenia may be a relatively distinct manifestation of deficient NMDAR functioning. In contrast, secondary pharmacological effects shared by NMDAR antagonists and the 5-HT2A agonist (ie disruption of glutamatergic neurotransmission) may be the mechanism underlying impairments in AX-CPT performance observed during both psilocybin and ketamine administration. Comparable deficits in schizophrenia may result from independent dysfunctions of 5-HT2A and NMDAR-related neurotransmission.
Similar content being viewed by others
INTRODUCTION
Neurocognitive deficits represent an integral feature of schizophrenic pathology and include deficits in higher cognitive functions such as attention, executive functions, and memory (Bilder, 1998; Cornblatt and Keilp, 1994; Pantelis et al, 1998; Saykin et al, 1994). Patients are also impaired in simple tasks probing sensory memory across different modalities (Javitt et al, 1997, 1999; Strous et al, 1995). For example, schizophrenic patients show deficits in auditory sensory (echoic) memory, which encodes and maintains representations of simple physical features of auditory stimuli (eg pitch, intensity) for up to 30 s following stimulus presentation (Lu et al, 1992). These deficits are manifested in an impaired ability to match tones following a brief delay (Javitt et al, 1997; Strous et al, 1995; Wexler et al, 1998) and most likely represent dysfunction at the level of the auditory sensory cortex (Rabinowicz et al, 2000). Consequently, these deficits can also be demonstrated in an abnormal reduction of an event-related potential (ERP) component that is generated in auditory sensory areas (Alho, 1995; Frodl-Bauch et al, 1997; Korzyukov et al, 1999; Näätänen and Alho, 1995a; Tiitinen et al, 1993). This ERP component constitutes an index of echoic memory and is termed mismatch negativity (MMN) (Näätänen, 1995; Ritter et al, 1995). MMN is an auditory ERP that is automatically generated whenever features of a presented stimulus differ from features of previously presented standard stimuli (Näätänen, 1995; Näätänen et al, 1993; Ritter et al, 1995). MMN is thus the manifestation of a preattentive process that compares the deviant stimulus to the transient sensory memory trace of the standard stimulus (Näätänen, 1990; Novak et al, 1990; Ritter et al, 1995). In the absence of such a memory trace, a deviant stimulus does not elicit MMN (Näätänen, 1990). Furthermore, MMN is also generated when a stimulus violates a more abstract regularity that has been extracted from previously presented stimuli (Näätänen and Winkler, 1999; Schröger, 1997). For instance, in a series of stimuli of increasingly higher frequency, a stimulus of previously presented, but lower, frequency will elicit an MMN, because it violates the regularity of a stepwise increase in frequency (Schröger, 1997). Similarly, infrequent repetition of one tone in a regular alternation of two tones will elicit MMN (Alain et al, 1994). Thus, MMN is an electrophysiological index of context-sensitive information processing at the level of the auditory sensory memory (Dehaene-Lambertz, 1997; Näätänen, 1992; Näätänen and Alho, 1995b; Näätänen and Winkler, 1999).
Out of 15 studies in schizophrenia, deficits in MMN generation were found in 13 studies (Alain et al, 1998; Catts et al, 1995; Hirayasu et al, 1998; Javitt et al, 1993, 1995, 2000; Kreitschmann-Andermahr et al, 1999; Oades et al, 1997; Shelley et al, 1991; Shutara et al, 1996; Umbricht et al, 1998, 1999) demonstrating deficits in context-dependent information processing of auditory stimuli at a preattentive automatic level. Schizophrenic patients also exhibit deficient performance in complex tasks that engage the prefrontal cortex (Barch et al, 2001) and require utilization of contextual information for correct task performance (Cohen et al, 1999; Javitt et al, 2000; Servan-Schreiber et al, 1996). Such a task is a modified version of an ‘AX’-type continuous performance task (AX-CPT), in which subjects are required to press a button whenever the letter X follows the letter A. The AX sequences are presented with a high probability, to set up a strong response bias in subjects. Thus, whenever a letter other than A (denoted as ‘B’) precedes an X, access to and use of this contextual information is required to inhibit the tendency to respond to the X. Schizophrenic patients specifically commit more BX errors, suggesting a deficient use of contextual information (Cohen et al, 1999; Javitt et al, 2000; Servan-Schreiber et al, 1996).
A growing body of evidence implicates deficient NMDA (N-methyl-D-aspartate) receptor (NMDAR)-dependent neurotransmission in these deficits. In nonhuman primates, NMDAR antagonists selectively abolish the generation of MMN without affecting sensory ERPs such as N1 (Javitt et al, 1992, 1994, 1996). Likewise, we recently demonstrated that the NMDAR antagonist ketamine induces a significant reduction of MMN, but not of N1, in healthy volunteers (Umbricht et al, 2000). Similarly, ketamine and other NMDAR antagonists significantly reduced MMNm (the magnetic counterpart of MMN) and MMN, respectively, in healthy volunteers (Jääskeläinen et al, 1995a,1995b, Jääskeläinen et al, 1996; Kreitschmann-Andermahr et al, 2001; Pang and Fowler, 1999). In addition, subanesthetic doses of ketamine induce a pattern of deficits in AX-CPT performance in healthy volunteers that is characterized by a specific increase of context-dependent (BX) errors and closely resembles the deficits observed in schizophrenia (Umbricht et al, 2000). Thus, the available evidence suggests that in schizophrenia NMDAR-related dysfunction may contribute significantly to abnormalities in context-dependent information processing both at preattentive automatic and at attention-dependent controlled levels.
There is, however, evidence that abnormalities in 5-HT2A receptor-dependent neurotransmission may also play a role in some symptoms and cognitive deficits in schizophrenia. Some of this evidence comes from the observation that indoleamine hallucinogens such as LSD or psilocybin can induce—among a wide array of behavioral effects—psychotic symptoms that resemble symptoms of schizophrenia (Vollenweider, 1998; Vollenweider et al, 1998). The affinity of indoleamine hallucinogens at the 5-HT2A receptor is highly correlated with their hallucinogenic potency in humans (Aghajanian and Marek, 1999a). A recent study demonstrated that psilocybin not only induced psychotic symptoms, but also impaired spatial working memory in a similar fashion as observed in schizophrenia (Geyer, 1998; Park and Holzman, 1992; Vollenweider et al, 1997, 1998). These cognitive and behavioral effects seem primarily mediated through the agonist action of psilocybin at the 5-HT2A receptor, in that they are blocked in a dose-dependent fashion by ketanserin and risperidone but not haloperidol (Vollenweider et al, 1998). Dysfunctional 5-HT2A receptors may also play a role in abnormal gating mechanisms in schizophrenia; in animals administration of 5-HT2A receptor agonists disrupts prepulse inhibition (PPI), a measure of gating mechanisms (Geyer, 1998). In healthy volunteers, however, psilocybin failed to reduce PPI (Gouzoulis-Mayfrank et al, 1998), possibly because doses were substantially lower than those used in rodents. Furthermore, the 5-HT2A antagonist effect shared by atypical antipsychotic drugs may play a role in their, albeit modest, ameliorative effects on certain cognitive deficits in schizophrenia that are not affected by classical D2 receptor-blocking antipsychotics (Green et al, 1997; Meltzer and McGurk, 1999; Purdon et al, 2000; Stip and Lussier, 1996; Umbricht et al, 1998, 1999).
In humans, administration of psilocybin is, like ketamine, associated with increased dopamine release (Vollenweider et al, 1999), a putative model of dysfunctional dynamics of the dopaminergic system in schizophrenia. Recently, 5-HT2A agonists have also been reported to induce excessive release of glutamate that can be blocked by group II metabotropic receptor agonists (Aghajanian and Marek, 1999b). A similar excessive glutamate release has also been reported after administration of NMDAR antagonists (Moghaddam and Adams, 1998). Indeed, it has been suggested that this shared effect may be the mechanism mediating similar psychomimetic and cognitive effects of both NMDAR antagonists and 5-HT2A agonists, and that comparable disturbances in the dynamics of the glutamate system possibly due to dysfunction of NMDA and/or 5-HT2A receptor-dependent neurotransmission may be operative in schizophrenia (Aghajanian and Marek, 2000). In summary, there is evidence consistent with the hypothesis that dysfunctional 5-HT2A signaling may be an important factor in cognitive deficits in schizophrenia.
The primary aim of this study was to investigate the effects of a 5-HT2A agonist, psilocybin, on the generation of MMN and sensory ERPs and on AX-CPT performance in healthy volunteers using identical test procedures as used previously in our ketamine study (Umbricht et al, 2000) and to address the potential role of the 5-HT2A receptor in both these cognitive operations. We wanted to investigate if dysfunctional 5-HT2A receptor-dependent neurotransmission might also contribute to deficits in MMN generation and AX-CPT performance, and thus address the hypothesis that abnormalities of this receptor may play a role in comparable deficits in schizophrenia. Given both the direct action at distinct receptors and yet some overlap of secondary pharmacological effects of NMDAR antagonists and 5-HT2A receptor agonists, we were also interested in addressing another question—whether such shared pharmacological effects indeed constitute an important mechanism by which these psychotomimetics achieve their effects at both the preattentive and attention-dependent level. We thus assumed that a similar pattern of deficits would point to shared pharmacological effects as an important mechanism, while different effects would indicate main mechanisms of action more closely related to the divergent pharmacological characteristics of ketamine and psilocybin.
Psilocybin (O-phosphoryl-4-hydroxy-N,N-dimethyltryptamine) is a naturally occurring indoleamine hallucinogen. After ingestion it is metabolized to psilocin (Hasler et al, 1997). In rats, psilocin has been demonstrated to bind with high affinity to the 5-HT2A (Ki=6.0 nM) and with moderate affinity to the 5-HT1A receptor (Ki=190 nM) (McKenna et al, 1990). Although indoleamine hallucinogens bind to various subtypes of serotonin receptors, the hallucinogenic and cognitive effects are primarily mediated through agonist action at the 5-HT2A receptor (Aghajanian and Marek, 1999a; Vollenweider et al, 1998). At the doses used, psilocybin has no medical side effects.
METHODS
The study was approved by the ethics committee of the Psychiatric University Hospital Zurich and conducted in the Research Department of the Psychiatric University Hospital Zurich in accordance with the Helsinki declaration. The use of psilocybin was approved by the Swiss Federal Health Office (BAG), Department of Pharmacology and Narcotics (DPN), Bern, Switzerland. Psilocybin was obtained from the BAG–DPN and was prepared as capsules (1 and 5 mg) at the pharmacy of the Kantonsspital Luzern, Switzerland.
Subjects
Normal subjects were recruited from the local university and technical college through advertisement. The rationale and the goal of the study were explained in lay terms to the subjects during the initial screening interview by the principal investigator (DU). In addition, the expected psychotomimetic and hallucinogenic effects were reviewed in detail and described as accurately as possible. Subjects were informed that they would be under constant supervision during both sessions. All potential study candidates were thus fully informed about the goal and the risks of the study both orally and in writing, and all signed informed consent. After signing informed consent, subjects underwent a screening that included a structured clinical interview (Composite International Clinical Interview: CIDI) (Wittchen and Semler, 1996) assessing present and past personal psychiatric history, a semistructured interview covering family psychiatric history, a physical examination, and laboratory tests that included a complete blood count, routine blood chemistry and an electrocardiogram. Exclusion criteria were (a) a history of present or past history of Axis I disorders, (b) a history of drug dependence or present drug abuse, (c) a family history of Axis I disorders extending to second-degree relatives, and (d) the presence of any medical disorder. Intelligence was assessed using the Hamburg-Wechsler Intelligence Scale, revised version (Tewes, 1994). Handedness was determined using the handedness scale by Chapman and Chapman (1987). A total of 18 right-handed subjects (10 men/and eight women) were enrolled in the study. Their mean age was 25.1±4.3 years. Of these, 16 were currently university students; two had completed an apprenticeship and were employed at the time of the study. Their mean verbal and performance IQs were 114±11 and 117±9, respectively. None of the female study subjects was pregnant. Study subjects received a financial remuneration for participation.
Procedures
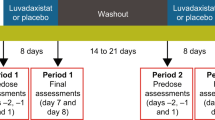
Psilocybin/Placebo administration
Each subject participated in both a psilocybin and a placebo session on two separate days in a randomized and counterbalanced order. Subjects were blind to drug order. On both days, subjects arrived in the laboratory around 0900 h after an overnight fast. After an initial baseline ERP recording, subjects were given psilocybin at a dose of 0.28 mg/kg in 1- and 5-mg capsules or an equal number of capsules containing placebo. A second ERP recording was obtained 70 min after ingestion of psilocybin or placebo. Afterwards subjects stayed under constant supervision until all drug effects had worn off. After an examination by the principal investigator, subjects were released into the custody of a partner or immediate relative.
Behavioral ratings
At the end of each ERP recording session, behavioral effects were assessed using the Brief Psychiatric Rating Scale (scale points: 1–7) (Woerner et al, 1988). Orientation to person, place, and time were assessed with three items from the Modified Mini-Mental State interview (Teng and Chui, 1987): ‘Date and Place of Birth’, ‘Temporal Orientation’, and ‘Spatial Orientation’, with a maximum score of 25 indicating full orientation.
Auditory test paradigm
ERP recordings were acquired during the presentation of auditory stimuli. Auditory stimuli consisted of 100-ms, 1000-Hz standard stimuli intermixed with 100-ms, 1500-Hz frequency deviants and 250-ms, 1000-Hz duration deviants. Stimuli were presented in a fixed order (nine standards, one frequency deviant, nine standards, one duration deviant) with a stimulus onset asynchrony (SOA) of 300 ms and presented through foam insert earphones at a nominal intensity of 75 dB sound pressure level (SPL). Rise–fall time was 5 ms for all stimuli. Stimuli were presented in four blocks, with a total of 1517 stimuli. Subjects performed the AX-CPT during presentation of the auditory test paradigm.
EEG recordings
EEG recordings, acquired with a Neuroscan system (Neuroscan Labs, Sterling, VA, USA), were obtained from 28 scalp locations, consisting of standard 10/20 placements plus right and left mastoid placements, along with right vertical and horizontal electro-oculogram (EOG) electrodes. An electrode placed on the nose served as reference. Electrode impedance was kept below 5 kΩ. Activity was amplified with a band pass of 0.1–100 Hz (6 dB down) and digitized continuously at a sampling rate of 500 Hz. Digital tags were obtained to all auditory stimuli.
Epochs were constructed that consisted of a 100-ms prestimulus baseline and a 500-ms poststimulus interval. After correction for vertical eye movements and blinks using the algorithm provided by Neuroscan software, epochs with amplitudes exceeding ±75 μV at any electrode except the vertical eye leads were excluded from averaging. Following artifact rejection, epochs were averaged off-line for each subject, session, phase and stimulus type, and were digitally filtered with a low-pass filter of 15 Hz (24 dB down).
Analyses focused on the generation of N1 and P2 to the standard stimuli and MMN generation to frequency and duration deviant stimuli. MMN waveforms were obtained by subtracting waveforms elicited by standards from waveforms elicited by frequency- or duration-deviant stimuli. Waveforms were mathematically referenced to an average-mastoid reference prior to peak detection. For N1, amplitude was defined as peak negativity within the 50–150 ms latency; for P2, amplitude was defined as peak positivity within the 150–250 ms latency. For frequency MMN, amplitude was defined as the peak negativity within the 100–225 ms latency window. For duration MMN, amplitude was defined as the peak negativity within the 200–300 ms range.
In one subject, the number of sweeps available for computing the MMN average both in the frequency deviant and duration deviant condition during psilocybin administration was below the threshold of 100 (set because of signal-to-noise concerns). Thus, only 17 subjects were included in the analyses of MMN. The mean number of sweeps available for computing MMN to frequency deviants was not significantly lower during psilocybin administration (infusion×time interaction F1,16=3.59, p=0.08). It was significantly lower for computing MMN to duration deviants (infusion×time interaction F1,16=4.55, p=0.05) and the sensory ERPs N1 and P2 (infusion×time interaction F1,17=5.78, p=0.03). In all instances, however, the mean number of sweeps was sufficiently high to ensure a satisfactory signal-to-noise ratio (see Table 1).
AX continuous performance test
Visual stimuli consisted of individual letters and were presented sequentially on a computer screen for 250 ms each. Subjects were instructed to press a button whenever the letter A (correct cue) was followed by the letter X (correct target). All other sequences were to be ignored, including sequences in which an incorrect cue (designated ‘B’, but comprising all letters other than A or X) was followed by the target letter (X) or sequences in which a correct cue (A) was followed by an incorrect target (designated ‘Y’, but comprising all letters other than A or X). Stimuli were presented in four blocks of 280 stimuli (140 pairs) each. Within each block, 50% of the cue–target sequences were presented with short (0.8 s) interstimulus interval (ISI) and 50% with long ISI (4 s). Short and long ISIs were pseudorandomly intermixed. The time between stimulus pairs was constant at 0.8 s. Of the stimulus pairs, 70% were AX sequences; all other sequences (BX, AY, BY) occurred with a probability of 0.1 each.
One subject completely stopped performing the task during psilocybin administration; in another subject, registration of response codes during the psilocybin administration failed due to computer problems. Thus, data of 16 subjects were included in the analysis.
Statistical Analysis
For ERP analyses, the primary dependent measures consisted of (a) amplitude and latency of N1 and P2 at Fz to the standard stimulus, and (b) amplitude and latency of frequency and duration MMN at FCz. Effects of psilocybin were evaluated using repeated-measures ANOVAs with session (psilocybin vs placebo) and time (baseline vs psilocybin/placebo administration) as repeated measures. For the analysis of MMN, an additional within-subject two-level factor denoting MMN type (frequency vs duration condition) was included. Paired t-tests were performed for post hoc analysis if indicated.
For the analyses of performance of AX-CPT, dependent measures consisted of hit rate (correct detection of AX sequences) and false alarm rates to BX, AY, or BY sequences. Effects of psilocybin on hit rate were evaluated with 2×3×2 factorial repeated-measures ANOVAs with session (psilocybin vs placebo), time (baseline vs psilocybin/placebo administration), and ISI (short vs long) as repeated measures. For analyses of false alarm rates, an additional within-subject factor with three levels denoting false alarm type (BX vs AY vs BY) was included. Differences between rates of BX errors and AY and BY errors, respectively, during the two phases of both sessions were evaluated with simple within-subject contrasts involving session (contrast: psilocybin vs placebo), time (contrast: baseline vs psilocybin/placebo administration), and false alarm type (contrast: BX vs AY; BX vs BY). Post hoc paired t-tests were used to assess specific differences if indicated. Furthermore, the discrimination index d′ and response bias Br were calculated using hit rates and total false alarm rates for the long and short ISI condition (Snodgrass and Corwin, 1988). Effects of psilocybin administration were evaluated with repeated-measures ANOVAs similarly as outlined above.
For behavioral analyses, we used the BPRS total score and five factors that can be derived from the BPRS items: (a) psychosis factor—conceptual disorganization, suspiciousness, hallucinatory behavior, unusual thought content; (b) activation factor—tension, mannerism and posturing, excitement; (c) anxiety/depression factor—somatic concern, anxiety, guilt feelings, depressive mood; (d) anergia factor—emotional withdrawal, motor retardation, blunted affect; and (e) hostility factor—hostility, suspiciousness, uncooperativeness. Effects of psilocybin were evaluated with 2×3 factorial repeated-measures ANOVAs with session (psilocybin vs placebo) and time (baseline vs psilocybin/placebo administration) as repeated measures.
Alpha levels of 0.05 were considered significant throughout.
RESULTS
Effects of Psilocybin on Behavior and Orientation
The BPRS total score increased from 18.9±1.5 to 28.1±9.9 (infusion×time interaction: F1,17=16.00, p=0.001). In addition, significant increases of the BPRS psychosis factor scores (baseline: 4.0±0.0; psilocybin administration: 7.5±2.9; infusion×time interaction: F1,17=24.79, p<0.001) were observed. There were also significant, but less pronounced increases of the BPRS anergia factor score (baseline: 3.2±0.5; psilocybin administration: 4.7±2.7; infusion×time interaction: F1,17=5.30, p<0.05), activation factor score (baseline: 3.2±0.5; psilocybin administration: 4.7±2.5; infusion×time interaction: F1,17=6.82, p<0.05), and hostility factor score (baseline: 3.1±0.5; psilocybin administration: 4.4±1.9; infusion×time interaction: F1,17=8.00, p<0.05) during psilocybin administration. In all subjects, psilocybin did not change autobiographic, temporal, or spatial orientation.
Effects of Psilocybin on Auditory ERPs
N1/P2
During the baseline of both sessions, mean amplitudes and latencies of N1 and P2 were in the range expected for an SOA of 300 ms (Table 1), with maxima at Fz. Psilocybin administration was associated with a significant decrease of N1 peak amplitude (session × time interaction: F1,17=6.03, p<0.05) (Table 1 and Figure 1). Post hoc paired t-tests demonstrated a significantly smaller N1 peak amplitude during psilocybin than session baseline (t=−2.09, df=17, p=0.05). Psilocybin administration did not affect N1 peak latency. An analysis of the effects of psilocybin administration on N1 topography was performed with selected electrode sites (F3, F4, C3, C4, P3, P4) using a repeated-measures ANOVA with five within-subject factors: left vs right location, anterior–posterior location (frontal vs central vs parietal electrodes), time (baseline phase vs psilocybin/placebo administration) and session (psilocybin vs placebo). This analysis demonstrated a significant infusion×time interaction owing to the decrease of the mean N1 amplitude during psilocybin administration (F1,17=6.14, p=0.03). The interactions involving the left vs right location or anterior–posterior location factors were not significant, indicating no change in topography of N1. Psilocybin did not affect the amplitude or latency of P2.
MMN
In both baseline sessions, robust MMN amplitudes to frequency and duration deviants were recorded, with MMN maxima at FCz. MMN to frequency deviants was larger than MMN to duration deviants (see Table 1 and Figure 2). The MMN to frequency deviants peaked at 121±9 and 128±19 ms in the placebo and psilocybin baseline phases, respectively. As expected, the corresponding latencies for MMN to duration deviants occurred with a delay of approximately 100 ms at 234±17 and 230±21 ms in the placebo and psilocybin sessions, respectively. During both placebo and psilocybin administration, MMN amplitudes decreased slightly, and this decrease was more pronounced for the MMN to frequency deviants during psilocybin administration; however, repeated-measures ANOVA failed to demonstrated a significant effect of psilocybin administration on MMN peak amplitudes in the frequency and duration condition (session×time interaction: F1,16=2.22, p=0.16; session×time×MMN type interaction: F1,16=0.14, p=0.7) (Table 1 and Figure 2). In general, MMN to duration deviants was smaller than MMN to frequency deviants (main effect of MMN type: F1,16=4.86, p<0.1). Repeated-measures ANOVAs of MMN performed separately for each condition demonstrated a stronger effect on MMN to frequency than MMN to duration deviants during psilocybin administration (session×time interaction: F1,16=3.20, p=0.09 for frequency condition and F1,16=0.36, p=0.6 for duration condition).
Psilocybin administration did not affect MMN peak latencies (session×time interaction: F1,16=0.71, p=0.4). As expected, there was a highly significant effect of MMN type (F1,16=452.96, p<0.000) due to the consistently longer peak latency of MMN to duration deviants.
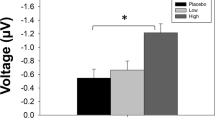
Effects of Psilocybin on AX-CPT Performance
Subjects performed the AX-CPT during the collection of ERP data. Psilocybin administration was associated with a significant decline of the hit rate at both ISIs (infusion×time interaction: F1,15=23.92, p<0.001) (Figure 3) The infusion×time×ISI interaction was not significant, indicating no differential impairment of performance at the two ISIs (F1,15=0.72, p=0.4). Post hoc paired t-tests confirmed significantly lower hit rates during psilocybin administration than during the baseline of the psilocybin infusion (short ISI: t=−5.03, df=15, p<0.001; long ISI: t=−4.96, df=15, p<0.001).
Psilocybin administration was associated with an increase of false alarms, which was most pronounced for false alarms to BX sequences at both short and long ISIs. A repeated-measures ANOVA demonstrated a significant three-way interaction of infusion×time×false alarm type (F2,14=13.51, p=0.001). The infusion type×ISI×time×false alarm type effect was not significant, indicating a similar increase of false alarms across both delays (F2,16=0.63, p=0.5). When we contrasted BX error rates with rates of AY and BY errors, a significantly greater increase of BX errors than both AY and BY errors was observed during psilocybin administration as compared with baseline and placebo administration (contrasts—psilocybin vs placebo session, baseline vs infusion phase, BX vs AY error rates: F1,15=16.03, p=0.001; contrasts—psilocybin vs placebo session, baseline vs infusion phase, BX vs AY error rates: F1,15=28.30, p<0.001). Paired t-tests confirmed significantly higher BX error rates during psilocybin administration than during baseline of the psilocybin session for both ISIs (short ISI: t=5.95, df=15, p<0.001; long ISI: t=5.23, df=15, p<0.001).
Similarly, when we used d′ as the dependent measure, a repeated-measures ANOVA demonstrated a significant decrease of d′ during psilocybin administration that was independent of ISI (interaction of session×phase: F1,16=52.49, p<0.001; interaction of session×phase×ISI: F1,16=1.43, p=0.2) (Table 2). This decrease was not because of a more liberal response bias induced by psilocybin, as mean Br decreased in both ISI conditions during psilocybin administration (data not shown; repeated-measures ANOVA session×phase interaction: F1,16=2.34, p=0.13).
DISCUSSION
In a previous study, we have shown that the NMDAR antagonist ketamine reduced MMN generation and AX-CPT performance in a fashion similar to the deficits observed in schizophrenic patients, thus providing supporting evidence for the NMDA/glutamate hypothesis of schizophrenia (Umbricht et al, 2000). The present study investigated the effects of the 5-HT2A agonist psilocybin on these measures, to explore the potential role of 5-HT2A receptor dysfunction in such deficits and to address the question of whether abnormalities in 5-HT2A receptor-dependent neurotransmission might also contribute to similar deficits in schizophrenia. Administration of the 5-HT2A agonist psilocybin induced a significant reduction of the sensory ERP N1, but was not associated with significant decreases of MMN to frequency and duration deviants. In contrast, psilocybin administration was associated with deficits in AX-CPT performance that were particularly characterized by a failure to use contextual information (BX errors), whereas the rates of other possible errors where contextual information is not important were not significantly altered. Furthermore, the absence of a delay effect indicates that psilocybin did not adversely affect the maintenance of contextual information.
The significant reduction of N1, but not of MMN, during administration of psilocybin differs from the pattern of effects (significant reductions of MMN, but not of N1) during ketamine administration (Umbricht et al, 2000). In contrast, the profile of psilocybin-induced deficits in AX-CPT performance is remarkably similar to the deficits observed in healthy volunteers during ketamine administration and in schizophrenic patients (Cohen et al, 1999; Javitt et al, 2000; Servan-Schreiber et al, 1996; Umbricht et al, 2000). To the extent that these differences and similarities reflect the underlying mechanisms, our results indicate that the pharmacological properties unique to ketamine and psilocybin (ie the NMDAR antagonist and 5-HT2A receptor agonist action, respectively) are the important factor determining their effects on MMN and N1 generation. Thus, together with the findings of our previous study, the results of this investigation support the conclusion that the generation of MMN indeed depends strongly on NMDAR functioning, whereas the 5-HT2A receptor plays a lesser role. Conversely, deficits in AX-CPT performance induced by both ketamine and psilocybin may result not only from their direct antagonist and agonist actions at their respective receptor sites, but also from secondary pharmacological effects that appear to be similar in nature for both drugs and take place downstream to these receptor sites in dopamine and glutamate systems.
Both NMDA and 5-HT2A receptors exert strong modulatory effects on dopaminergic and glutamatergic systems in rodents and humans. The blockade or activation, respectively, of these receptors leads to changes that seem to affect the dynamic properties of these neurotransmitter systems. In animals, the administration of NMDAR antagonists leads to target-specific disruption of the normal functioning of ascending dopaminergic pathways (Takahata and Moghaddam, 1998). Both activation and blockade of 5-HT2A receptors have been demonstrated to exert strong modulatory effects on dopaminergic neurotransmission (Lucas et al, 2000; Yan, 2000). In humans, ketamine administration increases spontaneous and amphetamine-induced dopamine release (Breier et al, 1998; Kegeles et al, 2000; Vollenweider et al, 2000). Similarly, administration of psilocybin in healthy volunteers is associated with increased dopamine release (Vollenweider et al, 1999). In addition, both NMDAR antagonists and 5-HT2A agonists induce excessive release of glutamate in rodents, an effect that can be blocked in both cases by group II metabotropic receptor agonists (Adams and Moghaddam, 1998; Aghajanian and Marek, 1999b; Moghaddam et al, 1997; Moghaddam and Adams, 1998). Consistently, in human volunteers lamotrigine, a drug that inhibits glutamate release, attenuates the cognitive effects of ketamine (Anand et al, 2000). Thus, NMDAR antagonists and 5-HT2A agonists share some secondary pharmacological effects. Besides these similar effects, 5-HT2A receptors have been shown to modulate NMDAR-dependent effects (Arvanov et al, 1999), and even antagonize effects of NMDAR antagonists (Farber et al, 1998).
In healthy volunteers, ketamine-induced cognitive deficits are ameliorated by haloperidol (a dopamine D2 receptor blocker) and lamotrigine (Anand et al, 2000; Krystal et al, 1999). In contrast, psilocybin-induced cognitive deficits are only ameliorated by 5-HT2A antagonists, but not by dopamine D2 antagonists (Vollenweider et al, 1998). Hence, increased glutamatergic tone (ie, abnormal dynamics of this system) may be the common denominator underlying overlapping aspects of the cognitive effects of dissociative NMDAR antagonists and hallucinogenic 5-HT2A agonists in humans (Aghajanian and Marek, 2000).
To the extent that deficits induced by acute drug challenges in healthy volunteers inform us about pathophysiological mechanisms underlying comparable deficits in schizophrenia, the findings of this and our previous study (Umbricht et al, 2000) have several implications for the investigation, pathophysiology, and treatment of cognitive deficits in schizophrenia. First of all, they suggest that deficits of long-latency ERPs such as N1 and MMN may provide potentially useful markers of specific receptor-related abnormalities, whereas abnormal performance in tasks such as the AX-CPT may be similar in patients whose primary abnormality lies within quite different receptor systems (such as independent abnormalities in both NMDA receptor and 5-HT2A receptor-dependent neurotransmission). Thus, profiling patients with regard to their performance on neuropsychological tests may not permit specifying etiologically heterogeneous subgroups. Conversely, using markers of early information processing such as ERPs may provide indices that are closer to suspected abnormalities in NMDAR and 5-HT2A receptor-dependent neurotransmission.
Second, neurocognitive deficits have become a major treatment focus in recent years, with the growing realization that they constitute an important limiting factor for rehabilitation and outcome (Bilder, 1997; Bilder et al, 2000; Green, 1996). If indeed excessive glutamate release (ie abnormal dynamics of the glutamate system, whether as a result of NMDA receptor hypofunction or excessive signaling through the 5-HT2A receptor) plays a role in these deficits, then 5-HT2A receptor antagonists, but not dopamine D2 receptor antagonists, would be expected to exert beneficial effects: In the scenario of a primary deficit in NMDAR-dependent neurotransmission, 5-HT2A antagonists may counteract its secondary effects on the glutamate system, whereas in the case of 5-HT2A receptor-related dysfunction their effect may be direct. Both scenarios would predict that atypical but not typical antipsychotic drugs improve cognitive deficits that result from secondary disturbances due to NMDAR hypofunction, such as deficits in AX-CPT and possibly other cognitive tasks that tax attention and working memory. In contrast, neither atypical nor typical antipsychotics would be expected to affect those deficits hypothesized to be a direct manifestation of NMDAR hypofunction such as deficient MMN generation. Indeed, there is accumulating evidence that atypical antipsychotics, in contrast to typical compounds, improve deficits in tasks assessing verbal memory, immediate recall, and attention (Green et al, 1997; Meltzer and McGurk, 1999; Purdon et al, 2000; Stip and Lussier, 1996). In addition, we and others have previously reported exactly such effects of clozapine and, to a lesser extent, risperidone in studies evaluating their effects on MMN and the attention-dependent ERP P3 (Schall et al, 1998; Umbricht et al, 1998, 1999). Clozapine and risperidone, but not typical antipsychotics, significantly improved the deficient generation of P3 (an attention-dependent ERP) in schizophrenia; like typical antipsychotics, however, clozapine and risperidone failed to affect MMN deficits (Ford et al, 1994; Schall et al, 1998; Umbricht et al, 1998, 1999). Consistent with these observations, we have found that both ketamine and psilocybin significantly reduce auditory P3 generation (Umbricht et al, 2001).
The finding of a significant decrease of N1 amplitude during psilocybin administration is consistent with studies demonstrating a tight modulation of the so-called N1 intensity dependence by the serotonergic system (Hegerl and Juckel, 1993, 1994a). N1 intensity dependence refers to the increase of N1 amplitude with increasing stimulus intensity (Hegerl and Juckel, 1994b). There is considerable evidence that a low serotonergic tone is associated with an increased N1 intensity dependence (Gottfries et al, 1976; Hegerl et al, 1995; Juckel et al, 1999; Perris et al, 1979; Tuchtenhagen et al, 2000; von Knorring and Perris, 1981; Wang et al, 1996), an effect mediated in particular through the 5-HT1A and 5-HT2A receptor (Juckel et al, 1997). One would therefore expect a 5-HT2A agonist to reduce N1 intensity dependence or, with intensity kept constant, to reduce N1 amplitude. The latter is exactly the observation in this study. We note that early ERP studies reported a reduced N1 intensity dependence in schizophrenic patients (Buchsbaum, 1977; Landau et al, 1976; Roth et al, 1991; Schooler et al, 1976). This abnormality, if confirmed in studies using modern ERP methodology, might thus relate to dysfunction in 5-HT2A receptor-dependent neurotransmission.
Psilocybin administration was associated with a small but nonsignificant decrease of MMN. It is conceivable that psilocybin reduces MMN, but that our study lacked the power to detect significant changes. In our study on the effects of ketamine, however, a similar number of subjects (20) was investigated and significant effects were observed. Furthermore, a significant effect on N1 was observed in this study. Thus, any reducing effect of 5-HT2A agonism on MMN generation would be much smaller than the effect of NMDA blockade on MMN or the effect of psilocybin on N1 generation. Furthermore, psilocybin had a more pronounced effect on MMN to frequency deviants. This may actually reflect its reducing effect on N1, given that MMN elicited with the particular paradigm used in this study is confounded with an N1 to the deviant stimulus. Such a confound is not present in the MMN to duration deviants, where the effect of psilocybin was not even close to significance.
It is possible that the dose of psilocybin was not comparable to the ketamine dose used in our previous study; however, the cognitive and behavioral effects were of similar magnitude as observed in our previous ketamine study. Thus, at a dose that induced significant deficits in higher cognitive function, psilocybin had no effect on MMN. This could mean that the 5-HT2A receptor indeed plays no role in MMN generation or, alternatively, that the processes underlying MMN generation may be more impervious to abnormal 5-HT2A signaling, requiring a much higher dose for their disruption.
In conclusion, in healthy volunteers the 5-HT2A agonist psilocybin was associated with significant deficits in the AX-CPT performance similar to those previously observed during ketamine administration and in schizophrenia, but failed to reduce MMN generation. These findings suggest that deficits in higher cognitive functions in schizophrenia may result from independent abnormalities in both NMDA and 5-HT2A receptor systems. The disruption of normal glutamatergic signaling may be a candidate mechanism mediating these shared effects. In addition, the results of this study provide further, albeit circumstantial, support for the hypothesis that deficits in MMN generation in schizophrenia may be a relatively direct manifestation of deficient NMDAR functioning. Atypical antipsychotic drugs may affect NMDAR and 5-HT2A receptor-related dysfunctions similarly through their 5-HT2A antagonism.
References
Adams B, Moghaddam B (1998). Corticolimbic dopamine neurotransmission is temporally dissociated from the cognitive and locomotor effects of phencyclidine. J Neurosci 18: 5545–5554.
Aghajanian GK, Marek GJ (1999a). Serotonin and hallucinogens. Neuropsychopharmacology 21: 16S–23S.
Aghajanian GK, Marek GJ (1999b). Serotonin, via 5-HT2A receptors, increases EPSCs in layer V pyramidal cells of prefrontal cortex by an asynchronous mode of glutamate release. Brain Res 825: 161–171.
Aghajanian GK, Marek GJ (2000). Serotonin model of schizophrenia: emerging role of glutamate mechanisms. Brain Res Brain Res Rev 31: 302–312.
Alain C, Hargrave R, Woods DL (1998). Processing of auditory stimuli during visual attention in patients with schizophrenia. Biol Psychiatry 44: 1151–1159.
Alain C, Woods DL, Ogawa KH (1994). Brain indices of automatic pattern processing. Neuroreport 6: 140–144.
Alho K (1995). Cerebral generators of mismatch negativity (MMN) and its magnetic counterpart (MMNm) elicited by sound changes. Ear Hear 16: 38–51.
Anand A, Charney DS, Oren DA, Berman RM, Hu XS, Cappiello A et al (2000). Attenuation of the neuropsychiatric effects of ketamine with lamotrigine: support for hyperglutamatergic effects of N-methyl-D-aspartate receptor antagonists. Arch Gen Psychiatry 57: 270–276.
Arvanov VL, Liang X, Magro P, Roberts R, Wang RY (1999). A pre- and postsynaptic modulatory action of 5-HT and the 5-HT2A,2C receptor agonist DOB on NMDA-evoked responses in the rat medial prefrontal cortex. Eur J Neurosci 11: 2917–2934.
Barch DM, Carter CS, Braver TS, Sabb FW, MacDonald A III, Noll DC et al (2001). Selective deficits in prefrontal cortex function in medication-naive patients with schizophrenia. Arch Gen Psychiatry 58: 280–288.
Bilder RM (1997). Neurocognitive impairment in schizophrenia and how it affects treatment options. Can J Psychiatry 42: 255–264.
Bilder RM (1998). The neuropsychology of schizophrenia: what, when, where, how? In: Fleischhacker WW, Hinterhuber H, Meise U (eds). Schizophrene Störungen: State of the Art II, Ursachen—Behandlung—Verlauf. 1st edn. Verlag Integrative Psychiatrie: Innsbruck, pp 155–171.
Bilder RM, Goldman RS, Robinson D, Reiter G, Bell L, Bates JA, Pappadopulos E et al (2000). Neuropsychology of first-episode schizophrenia: initial characterization and clinical correlates. Am J Psychiatry 157: 549–559.
Breier A, Adler CM, Weisenfeld N, Su TP, Elman I, Picken L et al (1998). Effects of NMDA antagonism on striatal dopamine release in healthy subjects: application of a novel PET approach. Synapse 29: 142–147.
Buchsbaum MS (1977). The middle evoked response components and schizophrenia. Schizophr Bull 3: 93–104.
Catts SV, Shelley AM, Ward PB, Liebert B, McConaghy N, Andrews S et al (1995). Brain potential evidence for an auditory sensory memory deficit in schizophrenia. Am J Psychiatry 152: 213–219.
Chapman LJ, Chapman JP (1987). The measurement of handedness. Brain Cogn 6: 175–183.
Cohen JD, Barch DM, Carter C, Servan-Schreiber D (1999). Context-processing deficits in schizophrenia: converging evidence from three theoretically motivated cognitive tasks. J Abnorm Psychol 108: 120–133.
Cornblatt BA, Keilp JG (1994). Impaired attention, genetics, and the pathophysiology of schizophrenia. Schizophr Bull 20: 31–46.
Dehaene-Lambertz G (1997). Electrophysiological correlates of categorical phoneme perception in adults. Neuroreport 8: 919–924.
Farber NB, Hanslick J, Kirby C, McWilliams L, Olney JW (1998). Serotonergic agents that activate 5-HT2A receptors prevent NMDA antagonist neurotoxicity. Neuropsychopharmacology 18: 57–62.
Ford JM, White PM, Csernansky JG, Faustman WO, Roth WT, Pfefferbaum A (1994). ERPs in schizophrenia: effects of antipsychotic medication. Biol Psychiatry 36: 153–170.
Frodl-Bauch T, Kathmann N, Moller HJ, Hegerl U (1997). Dipole localization and test-retest reliability of frequency and duration mismatch negativity generator processes. Brain Topogr 10: 3–8.
Geyer MA (1998). Behavioral studies of hallucinogenic drugs in animals: implications for schizophrenia research. Pharmacopsychiatry 31(Suppl 2): 73–79.
Gottfries CG, von Knorring L, Perris C (1976). Neurophysiological measures related to levels of 5-hydroxyindoleacetic acid, homovanillic acid and tryptophan in cerebrospinal fluid of psychiatric patients. Neuropsychobiology 2: 1–8.
Gouzoulis-Mayfrank E, Heekeren K, Thelen B, Lindenblatt H, Kovar KA, Sass H et al (1998). Effects of the hallucinogen psilocybin on habituation and prepulse inhibition of the startle reflex in humans. Behav Pharmacol 9: 561–566.
Green MF (1996). What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 153: 321–330.
Green MF, Marshall Jr BD, Wirshing WC, Ames D, Marder SR, McGurk S, Kern RS, Mintz J (1997). Does risperidone improve verbal working memory in treatment-resistant schizophrenia? Am J Psychiatry 154: 799–804.
Hasler F, Bourquin D, Brenneisen R, Bar T, Vollenweider FX (1997). Determination of psilocin and 4-hydroxyindole-3-acetic acid in plasma by HPLC-ECD and pharmacokinetic profiles of oral and intravenous psilocybin in man. Pharm Acta Helv 72: 175–184.
Hegerl U, Juckel G (1993). Intensity dependence of auditory evoked potentials as an indicator of central serotonergic neurotransmission: a new hypothesis. Biol Psychiatry 33: 173–183.
Hegerl U, Juckel G (1994a). Auditory evoked dipole source activity: indicator of central serotonergic dysfunction in psychiatric patients? Pharmacopsychiatry 27: 75–78.
Hegerl U, Juckel G (1994b). Auditory evoked dipole source activity: indicator of central serotonergic dysfunction in psychiatric patients? Pharmacopsychiatry 27: 75–78.
Hegerl U, Lipperheide K, Juckel G, Schmidt LG, Rommelspacher H (1995). Antisocial tendencies and cortical sensory-evoked responses in alcoholism. Alcohol Clin Exp Res 19: 31–36.
Hirayasu Y, Potts GF, O’Donnell BF, Kwon JS, Arakaki H, Akdag SJ et al (1998). Auditory mismatch negativity in schizophrenia: topographic evaluation with a high-density recording montage. Am J Psychiatry 155: 1281–1284.
Javitt DC, Doneshka P, Grochowski S, Ritter W (1995). Impaired mismatch negativity generation reflects widespread dysfunction of working memory in schizophrenia. Arch Gen Psychiatry 52: 550–558.
Javitt DC, Doneshka P, Zylberman I, Ritter W, Vaughan Jr HG (1993). Impairment of early cortical processing in schizophrenia: an event-related potential confirmation study. Biol Psychiatry 33: 513–519.
Javitt DC, Liederman E, Cienfuegos A, Shelley AM (1999). Panmodal processing imprecision as a basis for dysfunction of transient memory storage systems in schizophrenia. Schizophr Bull 25: 763–775.
Javitt DC, Schroeder CE, Steinschneider M, Arezzo JC, Vaughan Jr HG (1992). Demonstration of mismatch negativity in the monkey. Electroencephalogr Clin Neurophysiol 83: 87–90.
Javitt DC, Shelley AM, Silipo G, Lieberman JA (2000). Deficits in auditory and visual context-dependent processing in schizophrenia: defining the pattern. Arch Gen Psychiatry 57: 1131–1137.
Javitt DC, Steinschneider M, Schroeder CE, Arezzo JC (1996). Role of cortical N-methyl-D-aspartate receptors in auditory sensory memory and mismatch negativity generation: implications for schizophrenia. Proc Natl Acad Sci USA 93: 11962–11967.
Javitt DC, Steinschneider M, Schroeder CE, Vaughan HG, Arezzo JC (1994). Detection of stimulus deviance within primate primary auditory cortex: intracortical mechanisms of mismatch negativity (MMN) generation. Brain Res 667: 192–200.
Javitt DC, Strous RD, Grochowski S, Ritter W, Cowan N (1997). Impaired precision, but normal retention, of auditory sensory (‘echoic’) memory information in schizophrenia. J Abnorm Psychol 106: 315–324.
Jääskeäläinen IP, Lehtokoski A, Alho K, Kujala T, Pekkonen E, Sinclair JD, Näätänen R, Sillanaukee P (1995a). Low dose of ethanol suppresses mismatch negativity of auditory event-related potentials. Alcoholism Clin Exp Res 19: 607–610.
Jääskeäläinen IP, Pekkonen E, Alho K, Sinclair JD, Sillanaukee P, Näätänen R (1995b). Dose-related effect of alcohol on mismatch negativity and reaction time performance. Alcohol 12: 491–495.
Jääskeäläinen IP, Pekkonen E, Hirvonen J, Sillanaukee P, Näätänen R (1996). Mismatch negativity subcomponents and ethyl alcohol. Biol Psychol 43: 13–25.
Juckel G, Hegerl U, Molnar M, Cs V, Karmos G (1999). Auditory evoked potentials reflect serotonergic neuronal activity: a study in behaving cats administered drugs acting on 5-HT1A autoreceptors in the dorsal raphe nucleus. Neuropsychopharmacology 21: 710–716.
Juckel G, Molnar M, Hegerl U, Cs V, Karmos G (1997). Auditory-evoked potentials as indicator of brain serotonergic activity: first evidence in behaving cats. Biol Psychiatry 41: 1181–1195.
Kegeles LS, Abi-Dargham A, Zea-Ponce Y, Rodenhiser-Hill J, Mann JJ, Van Heertum RL et al (2000). Modulation of amphetamine-induced striatal dopamine release by ketamine in humans: implications for schizophrenia. Biol Psychiatry 48: 627–640.
Korzyukov O, Alho K, Kujala A, Gumenyuk V, Ilmoniemi RJ, Virtanen J et al (1999). Electromagnetic responses of the human auditory cortex generated by sensory-memory based processing of tone-frequency changes. Neurosci Lett 276: 169–172.
Kreitschmann-Andermahr I, Rosburg T, Demme U, Gaser E, Nowak H, Sauer H (2001). Effect of ketamine on the neuromagnetic mismatch field in healthy humans. Brain Res Cogn Brain Res 12: 109–116.
Kreitschmann-Andermahr I, Rosburg T, Meier T, Volz HP, Nowak H, Sauer H (1999). Impaired sensory processing in male patients with schizophrenia: a magnetoencephalographic study of auditory mismatch detection. Schizophr Res 35: 121–129.
Krystal JH, D’Souza DC, Karper LP, Bennett A, Abi-Dargham A, Abi-Saab D et al (1999). Interactive effects of subanesthetic ketamine and haloperidol in healthy humans. Psychopharmacology (Berl) 145: 193–204.
Landau SG, Buchsbaum MS, Carpenter W, Strauss J, Sacks M (1976). Schizophrenia and stimulus intensity control. Arch Gen Psychiatry 32: 1239–1245.
Lu ZL, Williamson SJ, Kaufman L (1992). Behavioral lifetime of human auditory sensory memory predicted by physiological measures. Science 258: 1668–1670.
Lucas G, De Deurwaerdere P, Porras G, Spampinato U (2000). Endogenous serotonin enhances the release of dopamine in the striatum only when nigro-striatal dopaminergic transmission is activated. Neuropharmacology 39: 1984–1995.
Lucas G, Spampinato U (2000). Role of striatal serotonin2A and serotonin2C receptor subtypes in the control of in vivo dopamine outflow in the rat striatum. J Neurochem 74: 693–701.
McKenna DJ, Repke DB, Lo L, Peroutka SJ (1990). Differential interactions of indolealkylamines with 5-hydroxytryptamine receptor subtypes. Neuropharmacology 29: 193–198.
Meltzer HY, McGurk SR (1999). The effects of clozapine, risperidone, and olanzapine on cognitive function in schizophrenia. Schizophr Bull 25: 233–255.
Moghaddam B, Adams B, Verma A, Daly D (1997). Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J Neurosci 17: 2921–2927.
Moghaddam B, Adams BW (1998). Reversal of phencyclidine effects by a group II metabotropic glutamate receptor agonist in rats. Science 281: 1349–1352.
Näätänen R (1990). The role of attention in auditory information processing as revealed by event-related potentials and other brain measures of cognitive function. Behav Brain Sci 13: 201–288.
Näätänen R (1992). Attention and Brain Function. Lawrence Erlbaum Associates: Hillsdale, NJ.
Näätänen R (1995). The mismatch negativity: a powerful tool for cognitive neuroscience. Ear Hear 16: 6–18.
Näätänen R, Alho K (1995a). Generators of electrical and magnetic mismatch responses in humans. Brain Topogr 7: 315–320.
Näätänen R, Alho K (1995b). Mismatch negativity to change in complex spectrotemporal sound pattern: a new way to study neural learning in the human brain. Electroencephalogr Clin Neurophysiol 44(Suppl): 179–184.
Näätänen R, Paavilainen P, Tiitinen H, Jiang D, Alho K (1993). Attention and mismatch negativity. Psychophysiology 30: 436–450.
Näätänen R, Winkler I (1999). The concept of auditory stimulus representation in cognitive neuroscience. Psychol Bull 125: 826–859.
Novak GP, Ritter W, Vaughan HG, Wiznitzer ML (1990). Differentiation of negative event-related potentials in an auditory discrimination task. Electroencephalogr Clin Neurophysiol 75: 255–275.
Oades RD, Dittmann-Balcar A, Zerbin D, Grzella I (1997). Impaired attention-dependent augmentation of MMN in nonparanoid vs paranoid schizophrenic patients: a comparison with obsessive-compulsive disorder and healthy subjects. Biol Psychiatry 41: 1196–1210.
Pang EW, Fowler B (1999). Dissociation of the mismatch negativity and processing negativity attentional waveforms with nitrous oxide. Psychophysiology 36: 552–558.
Pantelis C, Nelson HE, Barnes TRE (1998). Schizophrenia: A Neuropsychological Perspective. 1st edn. John Wiley & Sons: New York.
Park S, Holzman PS (1992). Schizophrenics show spatial working memory deficits. Arch Gen Psychiatry 49: 975–982.
Perris C, Gottfries CG, von Knorring L (1979). Visual averaged evoked responses in psychiatric patients: relationship to levels of 5-hydroxy-indoleacetic acid, homovanilic acid and tryptophan in cerebrospinal fluid. J Psychiatr Res 15: 175–181.
Purdon SE, Jones BD, Stip E, Labelle A, Addington D, David SR et al (2000). Neuropsychological change in early phase schizophrenia during 12 months of treatment with olanzapine, risperidone, or haloperidol. The Canadian Collaborative Group for research in schizophrenia. Arch Gen Psychiatry 57: 249–258.
Rabinowicz EF, Silipo G, Goldman R, Javitt DC (2000). Auditory sensory dysfunction in schizophrenia. Arch Gen Psychiatry 57: 1149–1155.
Ritter W, Deacon D, Gomes H, Javitt DC, Vaughan Jr HG (1995). The mismatch negativity of event-related potentials as a probe of transient auditory memory: a review. Ear Hear 16: 52–67.
Roth WT, Goodale J, Pfefferbaum A (1991). Auditory event-related potentials and electrodermal activity in medicated and unmedicated schizophrenics. Biol Psychiatry 29: 585–599.
Saykin AJ, Shtasel DL, Gur RE, Kester DB, Mozley LH, Stafiniak P, Gur RC (1994). Neuropsychological deficits in neuroleptic naive patients with first-episode schizophrenia. Arch Gen Psychiatry 51: 124–131.
Schall U, Catts SV, Chaturvedi S, Liebert B, Redenbach J, Karayanidis F, Ward PB (1998). The effect of clozapine therapy on frontal lobe dysfunction in schizophrenia: neuropsychology and event-related potential measures. Int J Neuropsychopharmacol 1: 19–29.
Schooler C, Buchsbaum MS, Carpenter W (1976). Evoked response and kinesthetic measures of augmenting/reducing in schizophrenics: replications and extensions. J Nerv Ment Dis 163: 221–232.
Schr E (1997). On the detection of auditory deviations: a pre-attentive activation model. Psychophysiology 34: 245–257.
Servan-Schreiber D, Cohen JD, Steingard S (1996). Schizophrenic deficits in the processing of context. A test of a theoretical model. Arch Gen Psychiatry 53: 1105–1112.
Shelley AM, Ward PB, Catts SV, Michie PT, Andrews S, McConaghy N (1991). Mismatch negativity: an index of a preattentive processing deficit in schizophrenia. Biol Psychiatry 30: 1059–1062.
Shutara Y, Koga Y, Fujita K, Takeuchi H, Mochida M, Takemasa K (1996). An event-related potential study on the impairment of automatic processing of auditory input in schizophrenia. Brain Topogr 8: 285–289.
Snodgrass JG, Corwin J (1988). Pragmatics of measuring recognition memory: applications to dementia and amnesia. J Exp Psychol 117: 34–50.
Stip E, Lussier I (1996). The effect of risperidone on cognition in patients with schizophrenia. Can J Psychiatry 41(Suppl 2): S35–S40.
Strous RD, Cowan N, Ritter W, Javitt DC (1995). Auditory sensory (‘echoic’) memory dysfunction in schizophrenia. Am J Psychiatry 152: 1517–1519.
Takahata R, Moghaddam B (1998). Glutamatergic regulation of basal and stimulus-activated dopamine release in the prefrontal cortex. J Neurochem 71: 1443–1449.
Teng EL, Chui HC (1987). The modified Mini-Mental State (3MS) examination. J Clin Psychiatry 48: 314–318.
Tewes U (1994). HAWIE-R: Hamburg-Wechsler-Intelligenztest für Erwachsene, Revision 1991. 2nd edn. Hans Huber AG: Bern.
Tiitinen H, Alho K, Huotilainen M, Ilmoniemi RJ, Simola J, Näätänen R (1993). Tonotopic auditory cortex and the magnetoencephalographic (MEG) equivalent of the mismatch negativity. Psychophysiology 30: 537–540.
Tuchtenhagen F, Daumann J, Norra C, Gobbele R, Becker S, Pelz S et al (2000). High intensity dependence of auditory evoked dipole source activity indicates decreased serotonergic activity in abstinent ecstasy (MDMA) users. Neuropsychopharmacology 22: 608–617.
Umbricht D, Javitt DC, Novak GP, Bates JA, Pollack S, Lieberman J et al (1998). Effects of clozapine on auditory event-related potentials in schizophrenia. Biol Psychiatry 44: 716–725.
Umbricht D, Javitt DC, Novak GP, Bates JA, Pollak S, Lieberman J, Kane J (1999). Effects of risperidone on auditory event-related potentials in schizophrenia. Int J Neuropsychopharmacol 2: 229–304.
Umbricht D, Schmid L, Koller R, Vollenweider FX, Hell D, Javitt DC (2000). Ketamine-induced deficits in auditory and visual context-dependent processing in healthy volunteers: implications for models of cognitive deficits in schizophrenia. Arch Gen Psychiatry 57: 1139–1147.
Vollenweider FX (1998). Advances and pathophysiological models of hallucinogenic drug actions in humans: a preamble to schizophrenia research. Pharmacopsychiatry 31(Suppl 2): 92–103.
Vollenweider FX, Leenders KL, Scharfetter C, Maguire P, Stadelmann O, Angst J (1997). Positron emission tomography and fluorodeoxyglucose studies of metabolic hyperfrontality and psychopathology in the psilocybin model of psychosis. Neuropsychopharmacology 16: 357–372.
Vollenweider FX, Vollenweider-Scherpenhuyzen MF, Babler A, Vogel H, Hell D (1998). Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action. Neuroreport 9: 3897–3902.
Vollenweider FX, Vontobel P, Hell D, Leenders KL (1999). 5-HT modulation of dopamine release in basal ganglia in psilocybin-induced psychosis in man: a PET study with [11C]raclopride. Neuropsychopharmacology 20: 424–433.
Vollenweider FX, Vontobel P, Oye I, Hell D, Leenders KL (2000). Effects of (S)-ketamine on striatal dopamine: a [11C]raclopride PET study of a model psychosis in humans. J Psychiatr Res 34: 35–43.
von Knorring L, Perris C (1981). Biochemistry of the augmenting-reducing response in visual evoked potentials. Neuropsychobiology 7: 1–8.
Wang W, Timsit-Berthier M, Schoenen J (1996). Intensity dependence of auditory evoked potentials is pronounced in migraine: an indication of cortical potentiation and low serotonergic neurotransmission? Neurology 46: 1404–1409.
Wexler BE, Stevens AA, Bowers AA, Sernyak MJ, Goldman-Rakic PS (1998). Word and tone working memory deficits in schizophrenia. Arch Gen Psychiatry 55: 1093–1096.
Wittchen H, Semler G (1996). Composite International Diagnostic Interview (CIDI). Germany, Beltz-Test, GmbH, Psychologie Verlags Union: Weinheim.
Woerner MG, Manuzza S, Kane JM (1988). Anchoring the Brief Psychiatric Rating Scale: an aid to improve reliability. Psychopharmacol Bull 24: 112–117.
Yan QS (2000). Activation of 5–HT2A/2C receptors within the nucleus accumbens increases local dopaminergic transmission. Brain Res Bull 51: 75–81.
Acknowledgements
This work was supported by grants from the Swiss National Science Foundation to Dr Umbricht (SNF 32-050957.97) and Dr Vollenweider (SNF 3200-040900.94 and the Heffter Research Institute (USA). The results of this study were presented in part at the 54th Annual Convention of the Society of Biological Psychiatry, 13–15 May, 1999, Washington, DC, USA. We thank Dr Daniel C Javitt for his helpful and critical review of an earlier draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Umbricht, D., Vollenweider, F., Schmid, L. et al. Effects of the 5-HT2A Agonist Psilocybin on Mismatch Negativity Generation and AX-Continuous Performance Task: Implications for the Neuropharmacology of Cognitive Deficits in Schizophrenia. Neuropsychopharmacol 28, 170–181 (2003). https://doi.org/10.1038/sj.npp.1300005
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300005
Keywords
This article is cited by
-
Functional connectivity signatures of NMDAR dysfunction in schizophrenia—integrating findings from imaging genetics and pharmaco-fMRI
Translational Psychiatry (2023)
-
Low-dose LSD and the stream of thought: Increased Discontinuity of Mind, Deep Thoughts and abstract flow
Psychopharmacology (2022)
-
A Research Domain Criteria (RDoC)-Guided Dashboard to Review Psilocybin Target Domains: A Systematic Review
CNS Drugs (2022)
-
Spontaneous and deliberate creative cognition during and after psilocybin exposure
Translational Psychiatry (2021)
-
Psychedelic drugs: neurobiology and potential for treatment of psychiatric disorders
Nature Reviews Neuroscience (2020)