Abstract
Background:
With obesity rampant, methods to achieve sustained weight loss remain elusive.
Objective:
To compare the long-term weight-loss efficacy of 2 cal and fat-restricted diets, standard (omnivorous) versus lacto–ovo–vegetarian, and to determine the effect of a chosen diet versus an assigned diet.
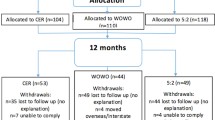
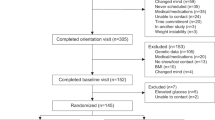
Design, subjects:
A randomized clinical trial was conducted with 176 adults who were sedentary and overweight (mean body mass index, 34.0 kg/m2). Participants were first randomly assigned to either receive their preferred diet or be assigned to a diet group and second, were given their diet of preference or randomly assigned to a standard weight-loss diet or a lacto–ovo–vegetarian diet. Participants underwent a university-based weight-control program consisting of daily dietary and exercise goals plus 12 months of behavioral counseling followed by a 6-month maintenance phase.
Measurements:
Percentage change in body weight, body mass index, waist circumference, low- and high-density lipoprotein, glucose, insulin and macronutrient intake.
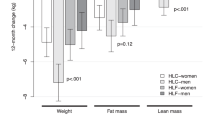
Results:
The program was completed by 132 (75%) of the participants. At 18 months, mean percentage weight loss was greater (P=0.01) in the two groups that were assigned a diet (standard, 8.0% (s.d., 7.8%); vegetarian, 7.9% (s.d., 8.1%)) than in those provided the diet of their choice (standard, 3.9% (s.d., 6.1%); vegetarian, 5.3% (s.d., 6.2%)). No difference was observed in weight loss between the two types of diet. Over the 18-month program, all groups showed significant weight loss.
Conclusions:
Participants assigned to their dietary preference did not have enhanced treatment outcomes. However, all groups lost weight with losses ranging from 4 to 8% at 18 months.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ogden C, Carroll M, Curtin L, McDowell M, Tabak C, Flegal K . Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006; 295/13: 1549–1555.
Wing RR . Behavioral interventions for obesity: Recognizing our progress and future challenges. Obes Res 2003; 11 (Supp): 3S–5S.
Wadden TA, Butryn ML, Byrne KJ . Efficacy of lifestyle modification for long-term weight control. Obes Res 2004; 12 (Suppl): 151S–162S.
Wing RR . Behavioral approaches to the treatment of obesity. In: Bray GA, Bourchard C, James WPT (eds). Handbook of Obesity: Clinical Applications. Marcel Dekker: NY, USA, 2004; 147–167.
Janelle KC, Barr SI . Nutrient intakes and eating behavior scores of vegetarian and nonvegetarian women. J Am Diet Assoc 1995; 95/2: 180–189.
White RF, Seymour J, Frank E . Vegetarianism among US women physicians. J Am Diet Assoc 1999; 99/5: 595–598.
Smith C, Burke LE, Wing R . Vegetarian and weight loss diets among young adults. Obes Res 2000; 8/2: 123–129.
Ornish D . Avoiding revascularization with lifestyle changes: The Multicenter Lifestyle Demonstration Project. Am J Cardio 1998; 82: 72T–76T.
Ornish D, Scherwitz LW, Billings JH, Gould L, Merritt TA, Sparler S et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA 1998; 280: 2001–2007.
Newby PK, Tucker KL, Wolk A . Risk of overweight and obesity among semivegitarian, lactovegitarian, and vegan women. Am J Clin Nutr 2005; 81: 1267–1274.
Burke LE, Smith CF, Wing RR . Efficacy of a vegetarian diet for weight loss. Obes Res 1999; 7 (Suppl 1): 18S.
Phillips F, Hackett A, Stratton G, Billington D . Effect of changing to a self-selected vegetarian diet on antropometric measurements in UK adults. J Hum Nutr Diet 2004; 17: 249–255.
Rosell M, Appleby P, Spencer E, Key T . Weight gain over 5 years in 21 966 meat-eating, fish-eating, vegetarian, and vegan men and woman in EPIC-Oxford. Int J Obes Relat Metab Disord 2006; 1–8.
Barnard ND, Scialli AR, Turner-McGrievy G, Lanou AJ . Acceptability of a low-fat vegan diet compares favorably to a step II Diet in a randomized controlled trial. J Cardiopulm Rehabil 2004; 24: 229–235.
Barnard N, Scialli A, Turner-McGrievy G, Lanou A, Glass J . The effect of low-fat, plant-based dietary intervention on body weight, metabolism, and insulin sensitivity. Am J Med 2005; 118: 991–997.
Murray DC . Preferred versus nonpreferred treatment, and self-control training versus determination raising as treatments of obesity: a pilot study. Psychol Rep 1976; 38: 191–198.
Mendonca PJ, Brehm SS . Effects of choice on behavioral treatment of overweight children. J Soc Clin Psychol 1983; 1/4: 343–358.
Renjilian DA, Perri MG, Nezu AM, McKelvey WF, Shermer RL, Anton SD . Individual versus group therapy for obesity: Effects of matching participants to their treatment preferences. J Consult Clin Psychol 2001; 69/4: 717–721.
King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M et al. Impact of participant and physician intervention preferences on randomized trials: a systematic review. JAMA 2005; 293/9: 1089–1099.
Epstein LH . Role of behavior theory in behavioral medicine. J Consult Clin Psychol 1992; 60/4: 493–498.
Burke LE, Choo J, Music E, Warziski M, Styn MA, Kim Y et al. PREFER study: a randomized clinical trial testing treatment preference and two dietary options in behavioral weight management—rationale, design and baseline characteristics. Contemp Clin Trials 2006; 27/1: 34–48.
Pocock SJ, Simon RM . Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trials. Biometrics 1975; 31: 103–115.
Wing RR . Behavioral approaches to the treatment of obesity. In: Bray GA, Bourchard C, James WPT (eds). Handbook of Obesity. Marcel Dekker: NY, USA, 1998 pp 855–877.
Friedewald WT, Levy RI, Fredickson DA . Estimation of the concentration of low-density cholesterol in plasma without the use of the preparative ultracentrifuge. Clin Chem 1972; 18: 499–502.
Jakicic J, Winters C, Lang W, Wing R . Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss, and fitness in overweight women: a randomized trial. JAMA 1999; 282/16: 1554–1560.
Daby R . Expressed preference for, and assignment to one of two weight loss programs: effects on weight loss and weight loss maintenance. Psychology 1988. Tennessee, Vanderbilt 113.
Fuller TC . The role of patient preferences for treatment type in the modification of weight loss behavior. Unpublished Dissertation 1988; Michigan State University.
Osterberg L, Blaschke TF . Adherence to medication. N Engl J Med 2005; 353/5: 487–497.
Golin CE, DiMatteo MR, Gelberg L . The role of patient participation in the doctor visit: implications for adherence to diabetes care. Diabetes Care 1996; 19/10: 1153–1164.
Feldman R, Bacher M, Campbell N, Drover A, Chockalingam A . Adherence to pharmacologic management of hypertension. Can J Public Health 1998; 89/5: I16–I18.
Smith CF, Burke LE, Wing RR . Young adults remain on vegetarian diets longer than on weight loss diets. Ann Behav Med 1999; 21 (Supp): 90.
Tate DF, Jackvony EH, Wing RR . Effects of internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA 2003; 289/14: 1833–1836.
Bish CL, Blanck HM, Serdula MK, Marcus M, Kohl III HW, Khan LK . Diet and physical activity behaviors among Americans trying to lose weight: 2000 Behavioral risk factor surveillance system. Obes Res 2005; 13/3: 596–607.
Weiss EC, Galuska DA, Khan LK, Serdula MK . Weight-control practices among US adults, 2001–2002. Am J Prev Med 2006; 31/1: 18–24.
Acknowledgements
This study was supported by National Institutes of Health grants NIH, NIDDK, no. RO1-DK58631. The conduct of the study was also supported by the Data Management Core of the Center for Research in Chronic Disorders NIH-NINR no. P30-NR03924, the Obesity and Nutrition Research Center NIH-NIDDK no. DK-046204, the Heinz Nutrition Laboratory and the General Clinical Research Center, NIH-NCRR-GCRC no. 5MO1-RR00056 at the University of Pittsburgh. We thank the study participants who graciously shared their time and information with us.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burke, L., Warziski, M., Styn, M. et al. A randomized clinical trial of a standard versus vegetarian diet for weight loss: the impact of treatment preference. Int J Obes 32, 166–176 (2008). https://doi.org/10.1038/sj.ijo.0803706
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803706
Keywords
This article is cited by
-
The Behavioral Intervention with Technology for E-Weight Loss Study (BITES): Incorporating Energy Balance Models and the Bite Counter into an Online Behavioral Weight Loss Program
Journal of Technology in Behavioral Science (2021)
-
Effect of Treatment Preference in Randomized Controlled Trials: Systematic Review of the Literature and Meta-Analysis
The Patient - Patient-Centered Outcomes Research (2019)
-
Does Giving Parents Their Choice of Interventions for Child Behavior Problems Improve Child Outcomes?
Prevention Science (2019)
-
Estimation of treatment preference effects in clinical trials when some participants are indifferent to treatment choice
BMC Medical Research Methodology (2017)
-
Vegetarian Diets and Weight Reduction: a Meta-Analysis of Randomized Controlled Trials
Journal of General Internal Medicine (2016)