Abstract
Objective:
To evaluate the effects of weight loss on the risk of having metabolic syndrome after 1 year of treatment with lifestyle modification alone, pharmacotherapy alone (sibutramine) or the combination of the two.
Design:
Randomized, controlled, 1-year clinical trial.
Patients:
One hundred and eighty women and 44 men, 18–65 years of age, with a body mass index of 30–45 kg/m2, free of uncontrolled hypertension or type 1 or 2 diabetes.
Intervention:
Fifteen milligrams of sibutramine per day alone, lifestyle modification counseling alone, sibutramine plus lifestyle modification counseling or sibutramine plus brief lifestyle modification counseling.
Measurements:
The metabolic syndrome, as defined by the Adult Treatment Panel III.
Results:
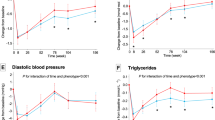
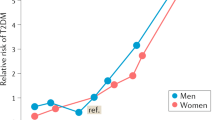
Before treatment, 34.8% of the participants had the metabolic syndrome. Metabolic syndrome was more prevalent in Caucasians than African Americans (42.5 vs 20.3%; P<0.03), in males than females (65.1 vs 34.9%; P<0.002) and in older (>44 years) than younger (⩽44 years) participants (47.5 vs 20.8%; P<0.0001). After 1 year of treatment, a moderate decrease in weight (8.0±8.7 kg) resulted in significant reductions in the prevalence of metabolic syndrome from 34.8 to 27.2% of all participants (P<0.02). Logistic regression analyses indicated that for each 1 kg of weight lost, the odds of metabolic syndrome were reduced by 8% (CI=0.89–0.97; P<0.003). Lifestyle modification either alone (P<0.04), or in combination with sibutramine (P<0.05), significantly reduced the prevalence of metabolic syndrome compared with sibutramine alone. The group effect was removed after controlling for weight loss.
Conclusions:
The metabolic syndrome was prevalent in over one-third of obese individuals who sought weight loss treatment, and the prevalence differed by age, sex and ethnicity. Moderate weight loss markedly reduced the odds of metabolic syndrome in this sample.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ford ES, Giles WH, Dietz WH . Prevalence of the metabolic syndrome among US adults: Findings from the Third National Health and Nutrition Examination Survey. JAMA 2002; 287: 356–359.
Lakka HM, Laaksonen DE, Lakka TA . The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2002; 288: 2709–2716.
Onat A, Ceyhan K, Basar O, Erer B, Toprak S, Sansoy V . Metabolic syndrome: major impact on coronary risk in a population with low cholesterol levels – a prospective and cross-sectional evaluation. Atherosclerosis 2002; 165: 285–292.
Laaksonen DE, Lakka HM, Niskanen LK, Kaplan GA, Salonen JT, Lakka TA . Metabolic syndrome and development of diabetes mellitus: Application and validation of recently suggested definitions of the metabolic syndrome in a prospective cohort study. Am J Epidemiol 2002; 156: 1070–1077.
Resnick HE, Jones K, Ruotolo G . Insulin resistance, the metabolic syndrome, and risk of incident cardiovascular disease in nondiabetic American Indians: The Strong Heart Study. Diab Care 2003; 26: 861–867.
Grundy SM, Becker D, Clark LT, Cooper RS, Denke MA, Howar DWJ et al. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Lofgren IE, Herron KL, West KL, Zern TL, Brownbill RA, Ilich JZ et al. Weight loss favorably modifies anthropometrics and reverses the metabolic syndrome in premenopausal women. J Am Coll Nutr 2005; 24: 486–493.
Poppitt SD, Keogh GF, Prentice AM, Williams DEM, Sonnemans HMW, Valk WJ et al. Long-term effects of ad libitum low-fat, high-carbohydrate diets on body weight and serum lipids in overweight subjects with metabolic syndrome. Am J Clin Nutr 2002; 75: 11–20.
Case CC, Jones PH, Nelson K, Smith EO, Ballantyne CM . Impact of weight loss on the metabolic syndrome. Diab Obes Metab 2002; 4: 407–414.
Xydakis AM, Case CC, Jones PH, Hoogoveen RC, Liu M, Smith EO et al. Adiponectin, inflammation, and the expression of the metabolic syndrome in obese individuals: The impact of rapid weight loss through caloric restriction. J Clin Endocrin Metab 2004; 89: 2697–2703.
Assali AR, Ganor A, Beigel Y, Shafer Z, Hershcovici T, Fainaru M . Insulin resistance in obesity: body weight or energy balance? J Endocrinol 2001; 171: 293–298.
Nicklas B, Dennis KE, Berman DM, Sorkin J, Ryan AS, Goldberg AP . Lifestyle intervention of hypocaloric dieting and walking reduces abdominal obesity and improves coronary heart disease risk factors in obese, postmenopausal, African-American and Caucasian women. J Gerontol A: Biol Sci Med Sci 2003; 58: 181–189.
Orchard TJ, Temprosa M, Goldberg RB, Haffner S, Ratner R, Marcovina S et al. The effect of metformin and intensive lifestyle intervention on the metabolic syndrome: The Diabetes Prevention Program Randomized Trial. Ann Int Med 2005; 142: 611–619.
Despres JP, Golay A, Sjostrom L, Rimonabant in Obesity-Lipids Study Group. Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia. N Engl J Med 2005; 353: 2121–2134.
Pi-Sunyer FX, Aronne LJ, Heshmati HM, Devin J, Rosenstock J, RIO-North America Study Group. Effect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: a randomized controlled trial. JAMA 2006; 295: 761–765.
Van Gaal L, Rissanen AM, Scheen AJ, Ziegler O, Rossner S, RIO-Europe Study Group. Effects of the cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-year experience from the RIO-Europe study. Lancet 2005; 365: 1389–1397.
Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK et al. Randomized trial of lifestyle modification and pharmacotherapy for obesity. N Engl J Med 2005; 353: 2111–2120.
Brownell KD, Rodin J . The Weight Maintenance Survival Guide. Brownell & Hager: Dallas, 1990.
Brownell KD, Wadden TA . The LEARN Program for Weight Control: Special Medication Edition. American Health Publishing: Dallas, 1999.
Haffner SM, Kennedy E, Gonzalez C, Stein MP, Miettinen H . A prospective analysis of the HOMA model. The Mexico City Diabetes Study. Diab Care 1996; 19: 1138–1141.
Hall WD, Clark LT, Wenger NK, Wright JT, Kumanyika SK, Watson K et al. The metabolic syndrome in African Americans: a review. Ethn Dis 2003; 13: 414–428.
Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB . Prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994. Arch Int Med 2003; 163: 427–436.
Kukkonen-Harjula KT, Borg PT, Nenonen AM, Fogelholm MG . Effects of a weight maintenance program with or without exercise on the metabolic syndrome: a randomized trial in obese men. Prev Med 2005; 41: 784–790.
Fogelholm M, Kukkonen-Harjula K, Nenonen A, Pasanen M . Effects of walking training on weight maintenance after a very-low-energy diet in premenopausal obese women: a randomized controlled trial. Arch Int Med 2000; 160: 2177–2184.
Norris SL, Zhang X, Avenell A, Gregg E, Schmid CH, Kim C et al. Efficacy of pharmacotherapy for weight loss in adults with type 2 diabetes mellitus. Arch Int Med 2004; 164: 1395–1404.
Arterburn DE, Crane PK, Veenstra DL . The efficacy and safety of sibutramine for weight loss: a systematic review. Arch Int Med 2004; 164: 994–1003.
Kim SH, Lee YM, Jee SH, Nam CM . Effect of sibutramine on weight loss and blood pressure: A meta-analysis of controlled trials. Obes Res 2003; 11: 1116–1123.
Zhu S, St-Onge M, Heshka S, Heymsfield SB . Lifestyle behaviors associated with lower risks of having the metabolic syndrome. Metabolism 2004; 53: 1503–1511.
Acknowledgements
Funding agencies were not involved in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. Drs Wadden and Phelan designed the study. Drs Berkowitz, Sarwer, Womble and Cato treated the patients and contributed to the revision of the paper with critical input from the other authors. Ms Rothman provided administrative, technical and logistic support and assembled the data. Dr Phelan analyzed the data and prepared the first draft of the manuscript, which was revised with the critical input from Dr Wadden and the other coauthors. All authors have approved the submission of the manuscript. Dr Phelan, as the principal investigator of this secondary study, had full access to all the data in the investigation and takes responsibility for the integrity of the data, the accuracy of the data analysis and acknowledgement of all author contributions. This research was supported by grants DK56124 and DK065018 from the National Institutes of Diabetes Digestive and Kidney Disease. Abbott Laboratories provided the medication used in the study. Drs Wadden and Berkowitz have served as consultants to Abbott laboratories, which manufacture sibutramine.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Phelan, S., Wadden, T., Berkowitz, R. et al. Impact of weight loss on the metabolic syndrome. Int J Obes 31, 1442–1448 (2007). https://doi.org/10.1038/sj.ijo.0803606
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803606
Keywords
This article is cited by
-
In Silico Development of Combinatorial Therapeutic Approaches Targeting Key Signaling Pathways in Metabolic Syndrome
Pharmaceutical Research (2022)
-
Metabolic Syndrome and Cognitive Function
Current Cardiology Reports (2021)
-
Antihypertensive medication needs and blood pressure control with weight loss in the Diabetes Remission Clinical Trial (DiRECT)
Diabetologia (2021)
-
Quantifying the Effects of Different Treadmill Training Speeds and Durations on the Health of Rat Knee Joints
Sports Medicine - Open (2018)
-
A calorie-restriction diet supplemented with fish oil and high-protein powder is associated with reduced severity of metabolic syndrome in obese women
European Journal of Clinical Nutrition (2015)