Abstract
All gamma herpesviruses and a few other viruses encode at least one homologue of the mammalian cell death inhibitor BCL-2. Gamma herpesviruses are associated with human and animal lymphoid and epithelial tumours. However, the role of these viral BCL-2 homologues in the virus replication cycle or in human disease is not known, though recent developments show progress in this area. The structure of viral BCL-2 family protein, KSBcl-2, is similar to that of cellular family members, but viral BCL-2 proteins differ functionally from the cellular proteins, apparently escaping the regulatory mechanisms to which their cellular counterparts are subjected. Thus, exploring the biochemical and biological functions of the viral BCL-2 family proteins will increase our understanding of their role in virus infections and will undoubtedly teach us something about their cellular kin.
Similar content being viewed by others
Introduction
We assume that the large family of mammalian BCL-2 proteins exists because the individual members serve at least some non-overlapping functions and/or because they can be regulated independently by different mechanisms in different cells and tissues. Cellular BCL-2 proteins are generally lumped into subgroups of anti-apoptotic, pro-apoptotic, or BH3-only proteins. This categorization is widely used, though it is now apparent that at least some of these proteins exhibit both pro- and anti-apoptotic activities under different circumstances.1,2,3 Interestingly, all three subclasses of the cellular proteins as well as viral BCL-2 exhibit striking 3-dimensional structure similarity,4 raising the possibility that all family members share at least one common biochemical function. Structurally, BCL-2 family members resemble the bacterial colicins or toxins that have been shown to form pores in membranes and/or facilitate translocation of a toxin moiety across membranes.5 The pro-apoptotic cellular BCL-2 proteins BAX and BAK are thought to induce translocation of pro-apoptotic mitochondrial factors across the outer mitochondrial membrane into the cytosol.6 While the mechanisms involved are still debated, BAX has been suggested to form or induce membrane channels following oligomerization. However, the mechanism by which bacterial toxins translocate peptides is not fully understood, and our model of BAX is likely not yet complete. The mechanisms by which anti-apoptotic BCL-2 proteins protect cells from programmed cell death are even less well understood. They appear to bind and sequester BH3-only proteins to prevent these BH3 proteins from activating the pro-apoptotic functions of BAX and BAK, but do they have additional functions in blocking cell death? Do they also induce channels that support cell survival? Do they act independently of other BCL-2 family proteins to regulate cellular bioenergetics? Interestingly, those central alpha helices in BCL-2 proteins that are thought to insert into membranes and perhaps form pores are also conserved in the structure of viral BCL-2.4 But because viral BCL-2 proteins preserve only the anti-apoptotic function and not the pro-apoptotic function of the BCL-2 family, their membrane active forms are presumably only for the purpose of cell survival.
Epstein–Barr virus (EBV) is an etiologic factor in B cell lymphomas (e.g. Burkitt's lymphoma) and epithelial tumours (e.g. nasopharyngeal carcinoma) and encodes two BCL-2 homologues, at least one of which is produced abundantly during productive virus replication. Overexpression of viral BCL-2 proteins protects a wide variety of cell types from a broad spectrum of death stimuli implying that they function at the point of convergence of many different death signals similar to cellular BCL-2.7,8,9,10,11,12,13.14,15,16 When cellular BCL-2 is overexpressed in the lymphoid compartment, these transgenic animals develop lymphoproliferations that can lead to malignant lymphoma.17,18,19 Although this provides an interesting correlation between EBV-associated tumours and the presumed oncogenic role of cellular BCL-2 in follicular B cell lymphomas,18,20,21,22 the role of viral BCL-2 in any virus-associated tumour is not known (see below). Elevation of cellular BCL-2 in EBV-associated tumours has also been reported.23,24 This is curious since EBV encodes its own BCL-2 homologue (discussed below). Nevertheless, anti-sense strategies that target cellular BCL-2 (or the viral regulators of cellular BCL-2 expression) in herpesvirus-associated tumours are showing some promise.25,26
Viral BCL-2 proteins differ in important ways from cellular BCL-2 family members. For example, the viral proteins escape regulation by proteolysis and phosphorylation (see below). However, viruses have devised other strategies to regulate their BCL-2 homologues. Epstein-Barr virus encodes two homologues of BCL-2, the anti-apoptotic BHRF1 protein [BamHI H fragment (in alphabetical order by size) Rightward reading Frame no.1] and a second BCL-2 family member, BALF1.27 Surprisingly, BALF1 has little or no ability to inhibit cell death in many assay systems.27,28 In contrast, BALF1 antagonizes the anti-apoptotic BCL-2 protein of EBV in that it suppresses the protective effects of BHRF1.28 Interestingly, this interference activity of BALF1 is most likely not due to direct binding of BALF1 to BHRF1, similar to the actions of BAX/BAK and BCL-2/BCL-xL.29 These and other details are explored below.
Homology between cellular and viral BCL-2 family
Cellular BCL-2 family proteins are conserved from worms and flies to humans,30 but family members even within the same species generally share low amino acid sequence homology (∼20–45%). Bcl-2 homologues encoded by alpha and gamma herpesviruses and the African swine fever virus (an unrelated large DNA virus) generally share 20–30% homology with one another and with their cellular counterparts (Figure 1). E1B 19K encoded by adenovirus is a functional homologue of the BCL-2 family. Though E1B 19K lacks significant overall amino acid sequence similarity with members of the BCL-2 family, E1B 19K does appear to preserve some of the defining motifs of the BCL-2 family31 and may possess additional functions not yet ascribed to other BCL-2 proteins32 as recently reviewed by Cuconati and White.33 The low level of homology among BCL-2 family members delayed the discovery of BCL-2 homologues in the genomes of some herpesviruses that had been sequenced several years earlier. Cleary et al.34 were the first to recognize amino acid sequence homology between cellular BCL-2 and BHRF1 encoded by EBV. Henderson et al.35 were the first to demonstrate that BHRF1 possesses anti-apoptotic activity similar to cellular BCL-2. Subsequently, we and others have shown that essentially all gamma herpesviruses encode a functional BCL-2 homologue.36,37,38,39,40,41,42
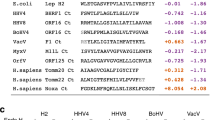
Amino acid sequence alignment of viral BCL-2 proteins with human BCL-2 and BAK. Shown are Epstein-Barr virus (EBV) homologues BHRF1 and BALF1, Kaposi's sarcoma-associated herpesvirus BCL-2 (KSBcl-2) and the BCL-2 homologues encoded by the herpesviruses rhesus rhadinovirus (RRV) open reading frame (ORF) 16, herpesvirus saimiri (HVS) ORF16, equine herpesvirus 2 (EHV2) ORF E4, bovine herpesvirus 4 (BHV4) BORFB2, and murine gamma herpesvirus 68 (γgHV68) M11, and the LMW5-HL ORF of unclassified African swine fever virus. Homologous sequences in over 50% of the entries are shaded. Bold lines indicate the BCL-2 homology (BH) and transmembrane (TM) domains of the cellular proteins, and the shaded bars indicate the positions of the alpha helices in the 3-dimensional structure of KSBcl-2. Amino acid numbers are indicated on the right
The 3-dimensional structure of KSBcl-2 (KSHV) is strikingly similar to the cellular proteins, in that it shares the same fold even though there are differences in the length of some helices and loops.4,5,43 The amphipathic alpha helix 5 together with helix 6, postulated to insert into lipid membranes, are also preserved in KSBcl-2 (Figure 1). In addition, viral BCL-2 proteins contain many of the recognizable amino acid sequence motifs present in the cellular family members (Figure 1). All viral homologues contain a recognizable BH1 sequence motif, though this motif is poorly conserved in BALF1, the non-protective EBV homologue. The BH2 motif is also conserved in the viral homologues except for murine gamma herpesvirus 68 (γHV68). Interestingly, the BH3 domain, thought to be important for killing cells, is poorly conserved in the viral homologues, though the pattern of bulky hydrophobic and charged residues is retained in most viral proteins. Little homology is shared among the viral homologues in the N-terminal BH4 domain, consistent with the fact that this domain is poorly conserved among the cellular proteins as well (perhaps reflecting novel functions). However, an alpha helix corresponding in position to the BH4 domain is preserved in the viral protein, except that it is two turns shorter than the cellular proteins. The non-homologous loop between BH4 and BH3 differs greatly in length among viral homologues just as it does among the cellular proteins. All viral BCL-2 proteins have at least one positively charged amino acid at or near the C-terminus, and most have a putative hydrophobic membrane anchor domain near the C-terminus. However, like some cellular homologues, this hydrophobic tail is lacking from the BCL-2 homologue of equine herpesvirus 2 (EHV2) and the African swine fever virus homologue LMW5-HL, and is shortened in other viral homologues. Viral KSBcl-2 also has a cleft similar to other BCL-2 family proteins.4 This cleft was suggested to serve as a binding pocket for BH3 domains of partner BCL-2 proteins. Indeed, a peptide corresponding to the BH3 domain of BAK binds KSBcl-2 efficiently. However, the relative affinities of KSBcl-2 for BH3 peptides derived from various cellular proteins (BAK>BAX>BAD) are distinct from those of cellular BCL-2 (BAD>BAX>BAK) and BCL-xL (BAD>BAK>BAX). The significance of these interactions with KSBcl-2 is not clear given that KSBcl-2 does not appear to bind BAX or BAK in co-immunoprecipitation experiments.41 Based on the structure of BAX, the only protein for which the structure of the C-terminus is known, the cleft of KSBcl-2 may also be occupied by its own hydrophobic C-terminal tail.43 The subcellular localization of BAX is likely determined by whether or not the hydrophobic tail of BAX is bound in its cleft or is free to bind intracellular membranes. The intracellular distribution of all viral BCL-2 proteins has not been studied in detail, but like their cellular counterparts, viral BCL-2 proteins can be localized diffusely in the cytosol or anchored to intracellular membranes including outer mitochondrial membranes, and these localizations are not necessarily predicted by their C-terminal sequences (unpublished data).44,45
Regulation of cellular but not viral BCL-2 by proteolysis
While cellular BAX and BAK are generally considered to be pro-apoptotic BCL-2 family members, under some circumstances they exhibit potent anti-apoptotic activity1 (Fannjiang and Hardwick, unpublished). Furthermore, the anti-apoptotic family members BCL-2 and BCL-xL can be converted into potent killers.2,3 BCL-2 and BCL-xL are cleaved in their loop domains near the N-terminus by caspase-3 or calpain during programmed cell death in a variety of cell types.2,3,46,47,48 The resulting C-terminal cleavage product is a potent BAX-like pro-apoptotic factor.3,49,50 Mutation of the caspase cleavage sites causes BCL-2 and BCL-xL to become more potently protective than wild type proteins, arguing that cleavage is an important intracellular event for regulating cell survival/death.2,3 Cleavage of BCL-2 may be important in chemotherapy-induced death of leukemia/lymphoma cells,51,52 and in the death of hepatocytes in mice treated with an antibody to activate the Fas death receptor pathway.52 This phenomenon, where the pro-death function of BCL-2 family members is activated by proteolysis, is now known to occur for many BCL-2 family members. Cleavage of BID, BAX and BAD by caspases, calpain, lysosomal enzymes and/or granzyme B potentiates their cell killing activity.53,54,55,56,57,58 Therefore, we suggest a model where all BCL-2 family members may have anti-apoptotic (or possibly null) activity that is converted by proteolysis or other mechanisms into pro-apoptotic activity upon receiving the right death stimulus (Figure 2).
Alternate view of the BCL-2 family. Many cellular anti-apoptotic (or possibly inactive) family members can be converted into pro-apoptotic factors following proteolysis or by other potential mechanisms. Non-proteolytic events are theoretically reversible. In contrast to cellular family members, herpesvirus BCL-2 homologues fail to be converted into pro-apoptotic factors suggesting that they escape regulatory mechanisms that govern their cellular counterparts. BHRF1 (Epstein–Barr virus), KSBcl-2 (Kaposi's sarcoma-associated herpesvirus), HVS (herpesvirus saimiri of monkeys), BHV4 (bovine herpesvirus), γHV68 (murine herpesvirus)
In contrast to the cellular BCL-2 proteins, the herpesvirus BCL-2 homologues have retained only the anti-apoptotic functions of the BCL-2 family and fail to be converted into killer factors.42 Viral BCL-2 homologues from several gamma herpesviruses, including EBV, KSHV/HHV8 (Kaposi's sarcoma-associated herpesvirus/human herpesvirus 8), herpesvirus saimiri (HVS) and bovine herpesvirus 4 (BHV4) fail to be cleaved by caspases in vitro or by other proteases present in apoptotic cell extracts. The only viral BCL-2 protein tested that could be cleaved was that encoded by γHV68.42 However, even if the viral proteins could be cleaved, their C-terminal fragments are unable to kill cells, with the exception of the C-terminal fragment of KSBcl-2 encoded by KSHV. But KSBcl-2 is apparently not susceptible to caspases or other proteases that are activated during cell death. Therefore, all of the viral BCL-2 homologues studied to date fail to be converted into killer proteins because they are either not cleaved by proteases or their C-termini lack pro-apoptotic activity, or both. In this manner, viral BCL-2 proteins escape cellular control mechanisms. This observation with the viral proteins supports the model in Figure 2. After all, if the killing function of cleaved cellular BCL-2 were a fortuitous event or a dominant negative effect of a truncation mutant, then the viruses would presumably not bother to eliminate this pro-death function. Furthermore, viruses are notorious for disabling the regulatory components that govern their cellular counterparts. This escape mechanism presumably allows the viral factors to avoid the regulatory mechanisms to which the cellular factors are subjected. Thus, the herpesvirus BCL-2 homologues are deregulated versions of their cellular progenitors. Where might this be important? Though it remains unproven, the loss of cellular apoptosis inhibitors in virus-infected cells that have an activated cell death pathway could be subverted if the virus provides a protease resistant apoptosis inhibitor. In addition, Ojala et al.59 have shown that a cyclin homologue encoded by KSHV directs cellular cyclin-dependent kinase (cdk) 6 to phosphorylate cellular BCL-2, resulting in destabilization of cellular BCL-2. But the BCL-2 family member encoded by KSHV, KSBcl-2, is not a substrate for viral-cyclin-cdk6, thereby escaping degradation. Substitution of the viral BCL-2 for cellular BCL-2 could side step the cell cycle inhibitory activity, proapoptotic function or other undesirable feature of cellular BCL-2.
Viral and cellular BCL-2 family heterodimerization (or lack of)
Shortly after the discovery that cellular BCL-2 was an inhibitor of apoptosis, it was reported that BCL-2 binds directly to the related cellular protein BAX.60 Furthermore, BCL-2 could suppress the killing function of BAX and it was proposed that heterodimerization was the mechanism by which BCL-2 blocks cell death (Figure 3A), leading to a flood of papers describing the ratios of anti- and pro-apoptotic factors found in cells of various states. Therefore, it was an attractive hypothesis that KSBcl-2 encoded by the human virus KSHV could suppress apoptosis by binding directly to BAX (based on its ability to bind BCL-2 in a yeast two-hybrid analysis).36 However, using co-immunoprecipitation experiments we failed to detect heterodimer formation between KSBcl-2 and the cellular homologues BCL-2, BCL-xL, BAX and BAK, even though KSBcl-2 binds efficiently to the novel cellular protein Aven (described below), to the unrelated cellular PRA1 protein and to the BCL-2-related protein Diva using both yeast two-hybrid and co-precipitation assays.28,41,61,62,63 There are also mixed reports on the ability of BHRF1 to form heterodimers with cellular family members. Again using the yeast two-hybrid strategy, one group found that BHRF1 interacted with BOK, BAX, BAK and BIK.64,65 Although they confirmed the interaction of BHRF1 with BOK by co-precipitation of in vitro translated proteins, we and others have failed to detect dimerization of BHRF1 with BAX, BAK, BAD (BH3-only protein) and Bcl-rambo by co-precipitation of transfected cell lysates or in GST pull-downs.28,40,66,67 However, in these same experiments, the viral BCL-2 proteins from HVS and γHV68 were found to bind BAX.28,40 Therefore, no consistent theme prevails, possibly suggesting that viral BCL-2 proteins may specifically target only one or possibly a subset of cellular pro-death factors to inhibit cell death. However, we favour the idea that viral BCL-2 proteins may protect cells by alternate mechanisms. Despite the apparent inability of BHRF1 and KSBcl-2 to stably interact with BAX in transfected mammalian cells, BHRF1 and KSBcl-2 are potently protective against BAX-induced cell death in these cells, dissociating the ability to protect cells from the capacity to bind BAX.28
Evolution of proposed models for how BCL-2 family members regulate cell survival/apoptosis. (A) BCL-2 inhibits BAX-induced apoptosis by direct heterodimerization with BAX.109(B) Mutants of cellular Bcl-2 and BCL-xL as well as viral BCL-2 proteins that fail to dimerize with BAX and BAK still protect cells from apoptosis,29 suggesting an alternate mechanism for promoting cell survival, perhaps by interacting with Aven.61 (C) Recently revised model suggests that anti-apoptotic BCL-2 proteins prevent BH3-only members of the cellular BCL-2 family from activating the cellular death effector molecules BAX and BAK.70,71,72
This heterodimerization model was also challenged by generating mutants of cellular BCL-xL and BCL-2 that fail to bind BAX and BAK but still protect cells,29 and by the observation that BAX and BCL-2 do not dimerize or co-localize inside cells68,69 (Figure 3B). Several other labs have also pointed out similar discordance between dimerization and function. This suggests that cellular BCL-2 and BCL-xL have alternate strategies for protecting cells, or that they possibly target the same cellular factor(s) as the pro-death BCL-2 family proteins. More recently the heterodimerization model has been revised to suggest that anti-apoptotic members of the BCL-2 family bind to and inhibit the pro-apoptotic BH3-only proteins instead of BAX and BAK70,71,72,73 (Figure 3C). That is, BH3-only proteins such as BID bind and activate BAX and BAK, and force the inactive (or possibly anti-apoptotic) forms of BAX and BAK to assume their pro-apoptotic function. In this model, the proposed function of anti-apoptotic BCL-2 family members is to block BH3-only proteins by directly binding to BH3-only proteins.70 This hypothesis is consistent with the observation that the cellular BH3-only proteins fail to kill cells that are deficient in both BAX and BAK, further implying that BH3-only proteins work by activating BAX and BAK.72 Though this concept has not been formally tested for herpesvirus BCL-2 homologues, BHRF1 was reported to interact with Bik/Nbk and Nip3, members of the BH3-only subgroup.63,74 Furthermore, a functional mutant of cellular BCL-xL that fails to bind BAX or BAK is still competent to bind the BH3-only protein BAD.75 Undoubtedly, we still have much to learn about the role of heterodimerization between BCL-2 family members.
In particular, it is interesting to note that in some situations overexpression of BCL-2 may enhance cell death triggered by BH3.75a,75b
Viral and cellular BCL-2 proteins bind Aven
Although no stable heterodimers are detected between the protective viral proteins KSBcl-2/BHRF1 and the cellular killer proteins BAX/BAK in mammalian cells, all of the viral BCL-2 homologues tested thus far, including KSBcl-2, BHRF1 and the BCL-2 homologue from γHV68, bind directly to a novel cell death regulator Aven61 (Figure 3B). Aven was originally identified in a yeast two-hybrid screen using a heterodimerization-defective mutant of BCL-xL as bait, in hopes of identifying downstream effectors of BCL-xL. Aven forms stable complexes with several viral and cellular BCL-2 proteins both in vitro and inside cells. Aven also binds to Apaf-1, a regulator of caspase-9 activation61 and perhaps other components of the apoptosome. Purified recombinant Aven protein also inhibits caspase activation in vitro (P Irusta and JM Hardwick, unpublished). Although the Apaf-1 homologue in C. elegans (CED-4) appears to bind directly to the C. elegans BCL-2 homologue (CED-9) to suppress caspase activation and cell death, several labs have reported that mammalian Apaf-1 fails to bind cellular BCL-2 family members. Therefore, Aven may be an important intermediate between Apaf-1 and BCL-2 family members as both viral and cellular anti-apoptotic BCL-2 proteins bind to Aven.
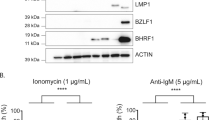
Viral BCL-2 regulation, BALF1 inhibits BHRF1 without dimerizing
Epstein–Barr virus (EBV) and the EBV-like primate viruses encode a second obvious BCL-2 homologue based on amino acid sequence homology.27,28 Surprisingly, BALF1 fails to protect Rat-1 cells, Hela cells, epidermal 308 cells and DG75 B cells from virus-induced apoptosis or BAX overexpression, while BHRF1 protects in all of these paradigms. Interestingly, BALF1 inhibits the anti-apoptotic function of the viral proteins BHRF1 and KSBcl-2 but not cellular BCL-xL. That is, co-transfection of BALF1 reduces the ability of the viral but not the cellular BCL-2 factors to inhibit apoptosis. Again it would be attractive to think that BALF1 suppresses the function of BHRF1 through a direct interaction. However, co-immunoprecipitation experiments are inconsistent with this idea.28 Furthermore, BALF1 and BHRF1 do not colocalize in cells. Therefore, BALF1 most likely interferes with BHRF1 through an indirect mechanism, and unpublished work in our lab suggests a role for Aven.
Could viral BCL-2 protect by other mechanisms?
One key structural feature of both viral and cellular BCL-2 family members, is that central pair of alpha helices stretching between the BH1 and BH2 domains that are postulated to insert into membranes to form a channel (helix 5 and 6, Figure 1).4 Although any link between channel activity and anti-apoptotic activity remains obscure, the possibility that viral BCL-2 proteins may possess ion channel activity is intriguing, and analysis of viral proteins in this regard will provide or dispel any correlation with anti-apoptotic function. The anti-apoptotic protein BCL-xL was reported to regulate the transport of ATP across the outer mitochondrial membrane by altering mitochondrial membrane permeability.76,77,78 Based on experimental evidence, this hypothesis suggests that ATP levels build up in the mitochondrial intermembrane space of apoptotic cells because ATP fails to reach the cytosol where ATP levels fall below critical levels required for the cell to survive. BCL-xL was proposed to maintain cytosolic levels of ATP following a death stimulus perhaps by regulating the activity of VDAC, the abundant voltage-dependent anion channel present on outer mitochondrial membranes.79 In this model, BCL-xL keeps VDAC open to export ATP from mitochondria into the cytosol.80 If this mechanism is a fundamental property of anti-apoptotic BCL-2 family members, then viral proteins might be expected to preserve this function.
Biology of oncogenic herpesviruses
Based on genome sequence analysis, gamma herpesviruses have been subdivided into the gamma 1 subgroup that includes Epstein–Barr virus (EBV or human herpesvirus 4/HHV4) and the gamma 2 subgroup that includes Kaposi's sarcoma-associated herpesvirus (KSHV/HHV8). While EBV infections have a much higher incidence rate in the human population than KSHV, both are associated with specific tumours that arise in individuals with specific types of immunosuppression or other environmental or genetic factors.81,82,83
EBV was discovered over 50 years ago in association with Burkitt's lymphoma and more recently was found in close association with several other tumours of both lymphoid origin (B-lymphoproliferative disease, Hodgkin's lymphoma, some T-cell lymphomas) and epithelial origin (nasopharyngeal carcinoma, stomach cancers).84 Because over 90% of the world's adult population is persistently infected with EBV, additional conditions obviously must be met to develop EBV-associated malignancies. It is generally believed that EBV persists in latently infected B cells and that lytic replication in the oral (or genital) epithelia serves to transmit the virus to susceptible individuals.85 Cytotoxic T cells are important in controlling/restricting EBV infections in healthy individuals. Patients on immunosuppressive anti-cancer therapy and individuals with malaria or HIV infections have an increased propensity to develop EBV-associated lymphomas. In addition, children with mutations in SAP that affect signaling pathways in cytotoxic T cells develop a fatal X-linked lymphoproliferative syndrome (XLPS) upon primary infection with EBV.86,87
KSHV was identified in the Kaposi's sarcoma skin lesions of AIDS patients, and infection with KSHV is a significant risk factor in developing KS (Kaposi's sarcoma), primary effusion lymphomas (PEL) and Castleman's disease.81,83,88 KS develops from latently infected spindle cells and 80–100% of KS lesions have detectable KSHV genomes. While KS is associated with immunosuppression due to HIV infection and kidney transplant regimes, KS also occurs in areas of the world where KSHV is endemic (classic KS). In some parts of the world, KS cases constitute a significant portion of the cancer patients. The virus can be transmitted by semen or saliva, but less is known about sites of viral latency and transmission.
Herpesviruses have both lytic (production of infectious virus resulting in cell death) and latent (non-cytolytic persistence of viral genomes that are replicated with the cell division cycle) phases of their life cycle. Both EBV and KSHV can express a variety of different genes during latent infections that are believed to contribute to the tumours associated with these viruses. For example, EBV encodes LMP1 that functions as a constitutive growth factor-independent pseudo receptor and can upregulate cellular BCL-2 expression. KSHV also encodes several genes implicated in tumour formation including a transmembrane protein designated K1 that interacts with the B cell receptor and induces changes in cell morphology and focus formation.89,90,91,92,93 K7 of KSHV was reported to be an anti-apoptotic bridging factor between BCL-2 and caspase-3, by virtue of its homology to the BH2 domain of cellular BCL-2 and to the BIR domain of a novel splice variant of Survivin, though point mutants of K7 to confirm the significance of this limited homology have not yet been reported.94 It should be kept in mind that virus-induced cell transformation and oncogenesis are fortuitous events that do not serve to maintain these viruses in the environment. Therefore, the function of these genes is foremost to benefit the virus life cycle.
What does viral BCL-2 do for the virus?
Although herpesvirus BCL-2 homologues are not generally believed to be directly causal in virus-associated tumorigenesis, a functional BCL-2 homologue of adenovirus, E1B-19K, is important for both virus production and E1A-induced transformation.95,96,97 Furthermore, the conservation of herpesvirus BCL-2 homologues among primary virus isolates and in the genomes of all gamma 1 and gamma 2 viruses sequenced to date indicates that viral BCL-2 is important in the biology of these viruses.28,40,42,98 However, the biology of herpesvirus BCL-2 proteins or the BCL-2 homologue encoded by African swine fever virus99 is poorly understood in part due to the difficulty in manipulating these viruses genetically and the lack of convenient cell culture systems and/or animal models, though recent advances have proven fruitful.
Most gamma herpesviruses including EBV and KSHV appear to express their BCL-2 homologues early in the lytic replication cycle, raising the possibility that herpesvirus BCL-2 proteins serve the virus by prolonging cell survival to allow production of greater numbers of progeny as shown previously for adenovirus.35,41 However, γHV68 also expresses its BCL-2 gene during latency.100 In addition, several labs have identified and cloned latent-style EBV transcripts containing the BHRF1 open reading frame, suggesting that BHRF1 may also be expressed during EBV latency, and therefore possibly contribute directly to immortalization of cells.101,102,103 However, evidence is lacking for viral BCL-2 protein expression during latency, though antibody reagents are limited. Mutant EBV viruses lacking BHRF1 apparently behave normally in cultured B cells though these assays are limited in scope.104,105 Recent studies with γHV68 virus have uncovered phenotypes for the BCL-2-defective virus in mice.106,107 While deletion of viral BCL-2 had no effect on acute virus replication in lung tissue, replication in the spleen was suppressed. Mutant virus was also impaired for establishment of latency in the spleen but only in animals that had received an intranasal inoculation, and not those animals inoculated intraperitoneally. Therefore, viral BCL-2 appears to be important when the animal acquires the virus by a natural route of infection. Unfortunately, this mouse model has not permitted the study of tumorigenesis, as tumours in γHV68-infected mice are rare.
Even if BHRF1 and KSBcl-2 function only during the lytic replication cycle, they may also play a key role in tumorigenesis, not only for the obvious purpose of supporting virus replication that is essential for virus transmission, but also for increasing viral load that may be important for tumour development. Elevated levels of anti-viral antibodies, viral antigen, viral DNA and/or viral transcripts correlate with development of lymphoproliferative disease (EBV), nasopharyngeal carcinoma (EBV) and Kaposi's sarcoma (KSHV). Therefore, the role of reactivation of latent virus to lytic replication, versus proliferation of latently infected cells in tumor development is an important issue in the field.85
Role of virus production versus proliferation of infected cells in tumorigenesis
In healthy individuals a balance is maintained between EBV latency, EBV replication and immune control of infection. A decrease in EBV-specific cytotoxic T cell function permits an increase in EBV replication and a new set-point is reached in this balance.108 However, some fraction of immunocompromised individuals develop EBV-positive lymphoproliferative disorders. Increased viral loads during immunosuppressive therapy could be due to either increased lytic replication of EBV and subsequent infection of new B cells, or increased proliferation of B cells already infected with EBV. While these two hypotheses are not mutually exclusive, Crawford and colleagues have suggested that de novo infections following reactivation of lytic virus serves to increase the size of the memory B cell compartment and that this is a key prerequisite event leading to tumour formation. That is, increased production of virus may be critical for subsequent tumorigenic events. Reactivation of the lytic cycle was evident in a cohort of immunosuppressed cardiothoracic transplant patients by the finding of high viral loads and detection of lytic cycle transcripts for the EBV glycoprotein gp350 in peripheral blood mononuclear cells of 26% of patients.85 However, the latent cycle proteins LMP1 and a transactivator EBNA2, which are responsible for proliferation of latently infected cells, were not detected, arguing against an expansion of latently infected cells. Although the patients in this study remained healthy, presumably a secondary event allowing escape of an EBV-immortalized cell to resist other anti-tumour controls could result in oncogenesis. Thus, control of lytic EBV replication will be key to controlling both latent infections and the subsequent occasional oncogenic step. Experiments in animals are beginning to explore some of these issues. Interestingly, a BCL-2-deficient γHV68 virus is defective for reactivation from latency, persistent replication and virulence during a chronic infection of a immunocompromised mice (IFNγ-/-).107 Surprisingly, this mutant virus was competent for acute replication not only in cell culture cells, but also in an acute infection in mice. This combination of findings is consistent with a role for viral BCL-2 in human disease as individuals with persistent infections will develop EBV-associated lymphomas upon immune suppression or other event some years after their primary infection. Much more work will be required to understand the molecular basis of EBV-associated tumorigenesis and the role of viral BCL-2. Unfortunately, the answers to the important questions regarding pathogenesis are the hardest to address experimentally.
Abbreviations
- Abbreviations::
-
Abbreviations for viruses and their BCL-2 homologues are all found in the legend to Figure 1
References
Lewis J, Oyler GA, Ueno K, Fannjiang Y, Chau BN, Vornov J, Korsmeyer SJ, Zou S & Hardwick JM (1999) Inhibition of virus-induced neuronal apoptosis by Bax. Nature Medicine 5: 832–835.
Cheng EHY, Kirsch DG, Clem RJ, Ravi R, Kastan MB, Bedi A, Ueno K & Hardwick JM (1997) Conversion of Bcl-2 to a Bax-like death effector by caspases. Science 278: 1966–1968.
Clem RJ, Cheng EHY, Karp CL, Kirsch DG, Ueno K, Takahashi A, Kastan MB, Griffin DE, Earnshaw WC, Veliuona MA & Hardwick JM (1998) Modulation of cell death by Bcl-xL through caspase interaction. Proc. Natl. Acad. Sci. U.S.A. 95: 554–559.
Huang Q, Petros AM, Virgin HW, Fesik SW & Olejniczak ET (2002) Solution structure of a Bcl-2 homolog from Kaposi sarcoma virus. Proc. Natl. Acad. Sci. U.S.A. 99: 3428–3433.
Muchmore SW, Sattler M, Liang H, Meadows RP, Harlan JE, Yoon HS, Nettesheim D, Chang BS, Thompson CB, Wong S-L, Ng S-C & Fesik SW (1996) X-ray and NMR structure of human Bcl-xL, an inhibitor of programmed cell death. Nature (London) 381: 335–341.
Martinou JC & Green DR (2001) Breaking the mitochondrial barrier. Nat. Rev. Mol. Cell. Biol. 2: 63–67.
Adams JM & Cory S (1998) The Bcl-2 protein family: arbiters of cell survival. Science 281: 1322–1326.
Tarodi B, Subramanian T & Chinnadurai G (1994) Epstein-Barr virus BHRF1 protein protects against cell death induced by DNA-damaging agents and heterologous viral infection. Virology 201: 404–407.
Theodorakis P, D'Sa-Eipper C, Subramanian T & Chinnadurai G (1996) Unmasking of a proliferation-restraining activity of the anti-apoptosis protein EBV BHRF1. Oncogene 12: 1707–1713.
Kawanishi M (1997) Epstein-Barr virus BHRF1 protein protects intestine 407 epithelial cells from apoptosis induced by tumor necrosis factor alpha and anti-Fas antibody. J. Virol. 71: 3319–3322.
Foghsgaard L & Jaattela M (1997) The ability of BHRF1 to inhibit apoptosis is dependent on stimulus and cell type. J. Virol. 71: 7509–7517.
Huang H, Pan XH, Zhou JH, Yu L, Kong XT, Zhou SM, Li ZJ, Fu Q & Sun XY (1998) The effect of Epstein-Barr virus gene BHRF1 expression on radioresistance of nasopharyngeal carcinoma cells. ORL J Otorhinolaryngol Relat Spec 60: 329–333.
Derfuss T, Fickenscher H, Kraft MS, Henning G, Lengenfelder D, Fleckenstein B & Meinl E (1998) Antiapoptotic activity of the herpesvirus saimiri-encoded Bcl-2 homolog: stabilization of mitochondria and inhibition of caspase-3-like activity. J. Virol. 72: 5897–5904.
Fanidi A, Hancock DC & Littlewood TD (1998) Suppression of c-Myc-induced apoptosis by the Epstein-Barr virus gene product BHRF1. J. Virol. 72: 8392–8395.
Sutton VR, Davis JE, Cancilla M, Johnstone RW, Ruefli AA, Sedelies K, Browne KA & Trapani JA (2000) Initiation of apoptosis by granzyme B requires direct cleavage of bid, but not direct granzyme B-mediated caspase activation. J. Exp. Med. 192: 1403–1414.
Hardwick JM (1998) Viral interference with apoptosis. Sem.in Cell and Develop.Biol. 9: 339–349.
Tsujimoto Y (1989) Overexpression of the human bcl-2 gene product results in growth enhancement of Epstein-Barr virus-immortalized B cells. Proc. Natl. Acad. Sci. 86: 1958–1962.
McDonnell TJ, Deane N, Platt FM, Núñez G, Jaeger U, McKearn JP & Korsmeyer SJ (1989) bcl-2-immunoglobulin transgenic mice demonstrate extended B cell survival and follicular lymphoproliferation. Cell 57: 79–88.
McDonnell TJ & Korsmeyer SJ (1991) Progression from lymphoid hyperplasia to high-grade malignant lymphoma in mice transgenic for the t(14;18). Nature (London) 349: 254–256.
Tsujimoto Y, Cossman J, Jaffe E & Croce CM (1985) Involvement of the bcl-2 gene in human follicular lymphoma. Science 228: 1440–1443.
Tsujimoto Y, Bashir MM, Givol I, Cossman J, Jaffe E & Croce CM (1987) DNA rearrangements in human follicular lymphoma can involve the 5′ or the 3′ region of the bcl-2 gene. Proc. Natl. Acad. Sci. 84: 1329–1331.
Korsmeyer SJ (1992) Bcl-2 initiates a new category of oncogenes: Regulators of cell death. Blood 80: 879–886.
Camilleri-Broet S, Feuillard J, Bourgeois C, Seihean D, Hauw JJ & Raphael M (1995) High expression of latent membrane protein 1 of Epstein-Barr virus and BCL-2 oncoprotein in acquired immunodeficiency syndrome-related primary brain lymphomas. Blood 86: 432–435.
Sgadari C, Toschi E, Palladino C, Barillari G, Carlei D, Cereseto A, Ciccolella C, Yarchoan R, Monini P, Sturzl M & Ensoli B (2000) Mechanism of paclitaxel activity in Kaposi's sarcoma. J. Immunol. 165: 509–517.
Guinness ME, Kenney JL, Reiss M & Lacy J (2000) Bcl-2 antisense oligodeoxynucleotide therapy of Epstein-Barr virus-associated lymphoproliferative disease in severe combined immunodeficient mice. Cancer Res. 60: 5354–5358.
Kenney JL, Guinness ME, Reiss M & Lacy J (2001) Antisense to the Epstein-Barr virus (EBV)-encoded latent membrane protein 1 (LMP-1) sensitizes EBV-immortalized B cells to transforming growth factor-beta and chemotherapeutic agents. Int. J. Cancer 91: 89–98.
Marshall WL, Yim C, Gustafson E, Graf T, Sage DR, Hanify K, Williams L, Fingeroth F & Finberg RW (1999) Epstein-Barr virus encodes a novel homolog of the bcl-2 oncogene that inhibits apoptosis and associates with Bax and Bak. J. Virol. 73: 5181–5185.
Bellows DS, Howell M, Pearson C, Hazlewood (formerly Henderson) SA & Hardwick JM (2002) Epstein-Barr virus BALF1 is a BCL-2-like antagonist of the herpesvirus anti-apoptotic BCL-2 proteins. J. Virol. 76: 2469–2479.
Cheng EHY, Levine B, Boise LH, Thompson CB & Hardwick JM (1996) Bax-independent inhibition of apoptosis by Bcl-xL . Nature (London) 379: 554–556.
Hengartner MO (2000) The biochemistry of apoptosis. Nature 407: 770–776.
Subramanian T, Tarodi B & Chinnadurai G (1995) Functional similarity between adenovirus E1B 19-kDa protein and proteins encoded by bcl-2 proto-oncogene and Epstein-Barr virus BHRF1 gene. Curr. Topics Micro. Immunol. 199: 153–161.
Sundararajan R, Cuconati A, Nelson D & White E (2001) Tumor necrosis factor-alpha induces Bax-Bak interaction and apoptosis, which is inhibited by adenovirus E1B 19K. J. Biol. Chem. 276: 45120–45127.
Cuconati A & White E (2002) Viral homologs of BCL-2: role of apoptosis in the regulation of virus infection. Genes & Develop. 16: 2465–2478.
Cleary ML, Smith SD & Sklar J (1986) Cloning and structural analysis of cDNAs for bcl-2 and a hybrid bcl-2/immunoglobulin transcript resulting from the t(14;18) translocation. Cell 47: 19–28.
Henderson S, Hue D, Rowe M, Dawson C, Johnson G & Rickinson A (1993) Epstein-Barr virus-coded BHRF1 protein, a viral homologue of bcl-2, protects human B cells from programmed cell death. Proc. Natl. Acad. Sci. 90: 8479–8483.
Sarid R, Sato T, Bohenzky RA, Russo JJ & Chang Y (1997) Kaposi's sarcoma-associated herpesvirus encodes a functional bcl-2 homologue. Nature Med. 3: 293–298.
Wang GH, Garvey TL & Cohen JI (1999) The murine gammaherpesvirus-68 M11 protein inhibits Fas- and TNF- induced apoptosis. J Gen Virol 80: 2737–2740.
Meseda CA, Arrand JR & Mackett M (2000) Herpesvirus papio encodes a functional homologue of the Epstein-Barr virus apoptosis suppressor, BHRF1. J. Gen. Virol. 81: 1801–1805.
Williams T, Sale D & Hazlewood SA (2000) BHRF1 is highly conserved in primate virus analogues of Epstein-Barr virus. Intervirol. 44: 55–58.
Nava VE, Cheng EHY, Veliuona M, Zou S, Clem RJ, Mayer ML & Hardwick JM (1997) Herpesvirus saimiri encodes a functional homolog of the human bcl-2 oncogene. J. Virol. 71: 4118–4122.
Cheng EHY, Nicholas J, Bellows DS, Hayward GS, Guo H-G, Reitz MS & Hardwick JM (1997) A Bcl-2 homolog encoded by Kaposi's sarcoma-associated virus, human herpesvirus 8, inhibits apoptosis but does not heterodimerize with Bax or Bak. Proc. Natl. Acad. Sci. U.S.A. 94: 690–694.
Bellows DS, Chau BN, Lee P, Lazebnik Y, Burns WH & Hardwick JM (2000) Anti-apoptotic herpesvirus Bcl-2 homologues escape caspase-mediated conversion to pro-apoptotic proteins. J. Virol. 74: 5024–5031.
Suzuki M, Youle RJ & Tjandra N (2000) Structure of Bax: coregulation of dimer formation and intracellular localization. Cell 103: 645–654.
Hardwick JM, Lieberman PM & Hayward SD (1988) A new Epstein-Barr virus transactivator, R, induces expression of a cytoplasmic early antigen. J. Virol. 62: 2274–2284.
Hickish T, Robertson D, Clarke P, Hill M, di Stefano F, Clarke C & Cunningham D (1994) Ultrastructural localization of BHRF1: An Epstein-Barr virus gene product which has homology with bcl-2. Can. Res. 54: 2808–2811.
Nakagawa T & Yuan J (2000) Cross-talk between two cysteine protease families: activation of caspase-12 by calpain in apoptosis. J. Cell. Biol. 150: 887–894.
Grandgirard D, Studer E, Monney L, Belser T, Fellay I, Borner C & Michel MR (1998) Alphaviruses induce apoptosis in Bcl-2-overexpressing cells: evidence for a caspase-mediated, proteolytic inactivation of Bcl-2. EMBO J. 17: 1268–1278.
Fujita N, Nagahashi A, Nagashima K, Rokudai S & Tsuruo T (1998) Acceleration of apoptotic cell death after the cleavage of Bcl-xL protein by caspase-3-like proteases. Oncogene 17: 1295–1304.
Kirsch DG, Doseff A, Chau BN, Lin D-S, de Souza-Pinto NC, Hansford R, Kastan MB, Lazebnik YA & Hardwick JM (1999) Caspase-3-dependent cleavage of Bcl-2 promotes release of cytochrome c. J. Biol. Chem. 274: 21155–21161.
Basanez G, Zhang J, Chau BN, Maksaev GI, Frolov V, Brandt TA, Burch J, Hardwick JM & Zimmerberg J (2001) Pro-apoptotic cleavage products of Bcl-xL form cytochrome c-conducting pores in pure lipid bilayers. J. Biol. Chem. 276: 31083–31091.
Fadeel B, Hassan Z, Hellstrom-Lindberg E, Henter JI, Orrenius S & Zhivotovsky B (1999) Cleavage of Bcl-2 is an early event in chemotherapy-induced apoptosis of human myeloid leukemia cells. Leukemia 13: 719–728.
Fadeel B, Zhivotovsky B & Orrenius S (1999) All along the watchtower: on the regulation of apoptosis regulators. FASEB J. 13: 1647–1657.
Li H, Zhu H, Xu C & Yuan J (1998) Cleavage of BID by caspase 8 mediates the mitochondrial damage in the Fas pathway of apoptosis. Cell 94: 491–501.
Luo X, Budihardjo I, Zou H, Slaughter C & Wang X (1998) Bid, a Bcl-2 interacting protein, mediates cytochrome c release from mitochondria in response to activation of cell surface death receptors. Cell 94: 481–490.
Wood DE & Newcomb EW (2000) Cleavage of Bax enhances its cell death function. Exp. Cell Res. 256: 375–382.
Alimonti JB, Shi L, Baijal PK & Greenberg AH (2001) Granzyme B induces BID-mediated cytochrome c release and mitochondrial permeability transition. J. Biol. Chem. 276: 6974–6982.
Condorelli F, Salomoni P, Cotteret S, Cesi V, Srinivasula SM, Elnemri ES & Calabretta B (2001) Caspase cleavage enhances the apoptosis-inducing effects of BAD. Mol. Cell. Biol. 21: 3025–3036.
Stoka V, Turk B, Schendel SL, Kim TH, Cirman T, Snipas SJ, Ellerby LM, Bredesen D, Freeze H, Abrahamson M, Bromme D, Krajewski S, Reed JC, Yin XM, Turk V & Salvesen GS (2001) Lysosomal protease pathways to apoptosis. Cleavage of bid, not pro-caspases, is the most likely route. J. Biol. Chem. 276: 3149–3157.
Ojala PM, Yamamoto K, Castaños-Vélez E, Biberfeld P, Korsmeyer SJ & Mäkelä TP (2000) The apoptotic v-cyclin-CDK6 complex phosphorylates and inactivates BCL-2. Nature Cell Biol. 2: 819–825.
Oltvai ZN, Milliman CL & Korsmeyer SJ (1993) Bcl-2 heterodimerizes in vivo with a conserved homolog, bax, that accelerates programmed cell death. Cell 74: 609–619.
Chau BN, Cheng EHY, Kerr DA & Hardwick JM (2000) Aven, a novel inhibitor of caspase activation, binds Bcl-xL and Apaf-1. Molec. Cell 6: 31–40.
Li IY, Shih HM, Liu MY & Chen JY (2001) The cellular protein PRA1 modulates the anti-apoptotic activity of Epstein-Barr virus BHRF1, a homologue of Bcl-2, through direct interaction. J. Biol. Chem. 276: 27354–27362.
Inohara N, Gourley TS, Carrio R, Muniz M, Merino J, Garcia E, Koseki T, Hu Y, Chen S & Nunez G (1998) Diva, a Bcl-2 homologue that binds directly to Apaf-1 and induces BH3-independent cell death. J. Biol. Chem. 273: 32479–32486.
Hsu SY, Kaipia A, McGee E, Lomeli M & Hsueh AJW (1997) Bok is a pro-apoptotic Bcl-2 protein with restricted expression in reproductive tissues and heterodimerizes with selective anti-apoptotic Bcl-2 family members. Proc. Natl. Acad. Sci. U.S.A. 94: 12401–12406.
Hsu SY & Hsueh AJ (1998) A splicing variant of the Bcl-2 member Bok with a truncated BH3 domain induces apoptosis but does not dimerize with antiapoptotic Bcl-2 proteins in vitro. J. Biol. Chem. 273: 30139–30146.
Moriishi K, Koura M & Matsuura Y (2002) Induction of Bad-mediated apoptosis by Sindbis virus infection: involvement of pro-survival members of the Bcl-2 family. Virology 292: 258–271.
Pellizzoni L, Kataoka N, Charroux B & Dreyfuss G (1998) A novel function for SMN, the spinal muscular atrophy disease gene product, in pre-mRNA splicing. Cell 95: 615–624.
Hsu YT & Youle RJ (1997) Nonionic detergents induce dimerization among members of the Bcl-2 family. J. Biol. Chem. 272: 13829–13834.
Wolter KG, Hsu Y-T, Smith CL, Nechushtan A, Xi X-G & Youle RJ (1997) Movement of Bax from the cytosol to mitochondria during apoptosis. J. Cell. Biol. 139: 1281–1292.
Zong WX, Lindston T, Ross AJ, MacGregor GR & Thompson CB (2001) BH3-only proteins that bind pro-survival Bcl-2 family members fail to induce apoptosis in the absence of Bax and Bak. Genes Dev. 15: 1481–1486.
Bouillet P, Cory S, Zhang LC, Strasser A & Adams JM (2001) Degenerative disorders caused by Bcl-2 deficiency prevented by loss of its BH3-only antagonist Bim. Dev. Cell 1: 645–653.
Cheng EHYA, Wei MC, Weiler S, Flavell RA, Mak TW, Lindsten T & Korsmeyer SJ (2001) BCL-2, Bcl-xL sequester BH3 domain-only molecules preventing BAX- and BAK-mediated mitochondrial apoptosis. Molec. Cell 8: 705–711.
Lee J-M, Zipfel GJ & Choi DW (1999) The changing landscape of ischaemic brain injury mechanisms. Nature 399: A7–A14.
Boyd JM, Gallo GJ, Elangovan B, Houghton AB, Malstrom S, Avery BJ, Ebb RG, Subramanian T, Chittenden T, Lutz RJ & Chinnadurai G (1995) Bik, a novel death-inducing protein shares a distinct sequence motif with Bcl-2 family proteins and interacts with viral and cellular survival-promoting proteins. Oncogene 11: 1921–1928.
Ottilie S, Diaz JL, Horne W, Chang J, Wang Y, Wilson G, Chang S, Weeks S, Fritz LC & Oltersdorf T (1997) Dimerization properties of human BAD. Identification of a BH-3 domain and analysis of its binding to mutant BCL-2 and BCL-XL proteins. J. Biol. Chem. 272: 30866–30872.
Vieira HL, Boya P, Cohen IEI, Hamal C, Haouzi D, Druillenec S, Balzacq AS, Brenner C, Roques B & Kroemer G (2002) Cell permeable BH3-peptides overcome the cytoprotective effect of Bcl-2 and Bcl-X(L). Oncogene 21: 1963–1977.
Letai A, Bassik MC, Walensky LD, Sorcinelli MD, Weiler S & Korsmeyer SJ (2002) Distinct BH3 domains either sensitize or activate mitochondrial apoptosis, serving as prototype cancer therapeutics. Cancer Cell 2: 183–192.
Vander Heiden MG, Chandel NS, Williamson EK, Schumacker PT & Thompson CB (1997) Bcl-xL regulates the membrane potential and volume homeostasis of mitochondria. Cell 91: 627–637.
Vander Heiden MG, Chandel NS, Schumacker PT & Thompson CB (1999) Bcl-xL prevents cell death following growth factor withdrawal facilitating mitochondrial ATP/ADP exchange. Molec. Cell 3: 159–167.
Vander Heiden MG & Thompson CB (1999) Bcl-2 proteins: regulators of apoptosis or of mitochondrial homeostasis?. Nat. Cell Biol. 1: E209–E216.
Vander Heiden MG, Li XX, Gottleib E, Hill RB, Thompson CB & Colombini M (2001) Bcl-xL promotes the open configuration of the voltage-dependent anion channel and metabolite passage through the outer mitochondrial membrane. J. Biol. Chem. 276: 19414–19419.
Vander Heiden MG, Plas DR, Rathmell JC, Fox CJ, Harris MH & Thompson CB (2001) Growth factors can influence cell growth and survival through effects on glucose metabolism. Mol. Cell. Biol. 21: 5889–5912.
Ensoli B, Sgadari C, Barillari G, Sirianni MC, Sturzl M & Monini P (2001) Biology of Kaposi's sarcoma. Eur. J. Can. 37: 1251–1269.
Sgadari C, Barillari G, Toschi E, Carlei D, Bacigalupo I, Baccarini S, Palladino C, Leone P, Bugarini R, Malavasi L, Cafaro A, Falchi M, Valdembri D, Rezza G, Bussolino F, Monini P & Ensoli B (2002) HIV protease inhibitors are potent anti-angiogenic molecules and promote regression of Kaposi sarcoma. Nat. Med. 8: 225–232.
Boshoff C & Weiss RA (2001) Epidemiology and pathogenesis of Kaposi's sarcoma-associated herpesvirus. Phil. Trans. R. Soc. Lond. B 356: 517–534.
de The G, Geser A, Day NE, Tukei PM, Williams EH, Beri DP, Smith PG, Dean AG, Bronkamm GW, Feorino P & Henle W (1978) Epidemiological evidence for causal relationship between Epstein-Barr virus and Burkitt's lymphoma from Ugandan prospective study. Nature (London) 274: 756–761.
Crawford DH (2001) Biology and disease associations of Epstein-Barr virus. Phil. Trans. R. Soc. Lond. B 356: 461–473.
Lewis J, Eiben LJ, Nelson DL, Cohen JI, Nichols KE, Ochs HD, Notarangelo LD & Duckett CS (2001) Distinct interactions of the X-linked lymphoproliferative syndrome gene product SAP with cytoplasmic domains of members of the CD2 receptor family. Clin. Immunol. 100: 15–23, See commentary on page 2 of the same issue
Latour S, Gish G, Helgason CD, Humphries RK, Pawson T & Veillette A (2001) Regulation of SLAM-mediated signal transduction by SAP, the X-linked lymphoproliferative gene product. Nat Immunol 8: 681–690.
Chang Y, Cesarman E, Pessin MS, Lee F, Culpepper J, Knowles DM & Moore PS (1994) Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi's sarcoma. Science 266: 1865–1869.
Wang D, Liebowitz D & Kieff E (1985) An EBV membrane protein expressed in immortalized lymphocytes transforms established rodent cells. Cell 43: 831–840.
Eliopoulos AG & Young LS (2001) LMP1 structure and signal transduction. Sem. Cancer Biol. 11: 435–444.
Bornkamm GW & Hammerschmidt W (2001) Molecular virology and Epstein-Barr virus. Phil. Trans. R. Soc. Lond. B 356: 437–459.
Lee H, Veazey R, Williams K, Li M, Guo J, Neipel F, Fleckenstein B, Lackner A, Desrosiers RC & Jung JU (1998) Deregulation of cell growth by the K1 gene of Kaposi's sarcoma-associated herpesvirus. Nat. Med. 4: 435–440.
Choi J-K, Means RE, Damania B & Jung JU (2001) Molecular piracy of Kaposi's sarcoma associated herpesvirus. Cytok. & Growth Factor Rev. 12: 245–257.
Wang HW, Sharp TV, Koumi A, Koentges G & Boshoff C (2002) Characterization of an anti-apoptotic glycoprotein encoded by Kaposi's sarcoma-associated herpesvirus which resembles a spliced variant of human survivin. EMBO J 21: 2602–2615.
Horner D, Lewis M & Farrell PJ (1995) Novel hypotheses for the roles of EBNA-1 and BHRF1 in EBV-related cancers. Intervirology 38: 195–205.
White E, Sabbatini P, Debbas M, Wold WSM, Kusher DI & Gooding LR (1992) The 19-kilodalton adenovirus E1B transforming protein inhibits programmed cell death and prevents cytolysis by tumor necrosis factor alpha. Mol. Cell. Biol. 12: 2570–2580.
Rao L, Debbas M, Sabbatini P, Hockenbery D, Korsmeyer S & White E (1992) The adenovirus E1A proteins induce apoptosis, which is inhibited by the E1B 19-kDa and Bcl-2 proteins. Proc. Natl. Acad. Sci. 89: 7742–7746.
Khanim F, Dawson C, Meseda CA, Dawson J, Mackett M & Young LS (1997) BHRF1, a viral homologue of the Bcl-2 oncogene, is conserved at both the sequence and functional level in different Epstein-Barr virus isolates. J. Gen. Virol. 78: 2987–2999.
Afonso CL, Neilan JG, Kutish GF & Rock DL (1996) An African swine fever virus Bcl-2 homolog, 5-HL, suppresses apoptotic cell death. J. Virol. 70: 4858–4863.
Virgin HW, Presti RM, Li X-Y, Liu C & Speck SH (1999) Three distinct regions of the murine gammaherpesvirus 68 genome are transcriptionally active in latently infected mice. J. Virol. 73: 2321–2332.
Austin PJ, Flemington E, Yandava CN, Strominger JL & Speck SH (1988) Complex transcription of the Epstein-Barr virus BamHI fragment H rightward open reading frame 1 (BHRF1) in latently and lytically infected B lymphocytes. Proc. Natl. Acad. Sci. U.S.A. 85: 3678–3682.
Bodescot M & Perricaudet M (1986) Epstein-Barr virus mRNAs produced by alternative splicing. Nucl. Acids Res. 14: 7103–7114.
Pearson GR, Luka J, Petti L, Sample J, Birkenbach M, Braun D & Kieff E (1987) Identification of an Epstein-Barr virus early gene encoding a second component of the restricted early antigen complex. Virology 160: 151–161.
Lee M-A & Yates JL (1992) BHRF1 of Epstein-Barr virus, which is homologous to human proto-oncogene bcl-2, is not essential for transformation of B cells or for virus replication in vitro. J. Virol. 66: 1899–1906.
Marchini A, Tomkinson B, Cohen JI & Kieff E (1991) BHRF1, the Epstein-Barr virus gene with homology to Bcl-2, is dispensable for B-lymphocyte transformation and virus replication. J. Virol. 65: 5991–6000.
Jacoby MA & Virgin HW4SSH (2002) Disruption of the M2 gene of murine gammaherpesvirus 68 alters splenic latency following intranasal, but not intraperitoneal, inoculation. J. Virol. 76: 1790–1801.
Gangappa S, van Dyk LF, Jewett TJ, Speck SH & Virgin HW4 (2002) Identification of the in vivo role of a viral bcl-2. J. Exp. Med. 195: 931–940.
Haque T, Thomas JA, Parratt R, Hunt BJ, Yacoub MH & Crawford DH (1997) A prospective study in heart and lung transplant recipients correlating persistent Epstein-Barr virus infection with clinical events. Transplant. 64: 1028–1034.
Yin X-M, Oltvai ZN & Korsmeyer SJ (1994) BH1 and BH2 domains of Bcl-2 are required for inhibition of apoptosis and heterodimerization with Bax. Nature (London) 369: 321–323.
Acknowledgements
The work from our lab summarized here was supported by grants CA73581, NS37402 and NS34175 (JMH) from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by M Piacentini
Rights and permissions
About this article
Cite this article
Hardwick, J., Bellows, D. Viral versus cellular BCL-2 proteins. Cell Death Differ 10 (Suppl 1), S68–S76 (2003). https://doi.org/10.1038/sj.cdd.4401133
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4401133
Keywords
This article is cited by
-
Contrasting roles for G-quadruplexes in regulating human Bcl-2 and virus homologues KSHV KS-Bcl-2 and EBV BHRF1
Scientific Reports (2022)
-
Differences in DNA Repair Capacity, Cell Death and Transcriptional Response after Irradiation between a Radiosensitive and a Radioresistant Cell Line
Scientific Reports (2016)
-
Disruption of Bcl-2 and Bcl-xL by viral proteins as a possible cause of cancer
Infectious Agents and Cancer (2014)
-
Cytomegaloviruses inhibit Bak- and Bax-mediated apoptosis with two separate viral proteins
Cell Death & Differentiation (2010)
-
BH3 domains define selective inhibitory interactions with BHRF-1 and KSHV BCL-2
Cell Death & Differentiation (2008)