Abstract
To investigate the aetiological role of human papillomavirus (HPV) in breast cancer, we examined the presence, genotype, viral load, and physical status of HPV in 124 Japanese female patients with breast carcinoma. Human papillomavirus presence was examined by PCR using SPF10 primers, and primer sets targeting the E6 region of HPV-16, -18, and -33. The INNO-LiPA HPV genotyping kit was used to determine genotype. Human papillomavirus DNA was detected in 26 (21%) breast carcinomas. The most frequently detected HPV genotype was HPV-16 (92%), followed by HPV-6 (46%), HPV-18 (12%), and HPV-33 (4%). In 11 normal epithelium specimens adjacent to 11 HPV-16-positive carcinomas, 7 were HPV-16-positive. However, none of the normal breast tissue specimens adjacent to HPV-negative breast carcinomas were HPV-positive. The real-time PCR analysis suggested the presence of integrated form of viral DNA in all HPV-16-positive samples, and estimated viral load was low with a geometric mean of 5.4 copies per 104 cells. In conclusion, although HPV DNA was detected in 26 (21%) breast carcinomas and, in all HPV-16-positive cases, the HPV genome was considered integrated into the host genome, their low viral loads suggest it is unlikely that integrated HPV is aetiologically involved in the development of Japanese breast carcinomas that we examined.
Similar content being viewed by others
Main
Breast cancer is one of the most prevalent malignancies throughout the world. It is the leading female cancer worldwide and comes second after stomach cancer in Japan (Parkin et al, 1999). Recent studies have suggested that some types of viruses, especially human papillomavirus (HPV), might be involved in the pathogenesis of breast cancer (Liu et al, 2001; Tsai et al, 2007).
Molecular and epidemiological studies have shown that a persistent infection with high-risk HPV is the most important risk factor for both cervical cancer and its precursors (Cuschieri et al, 2005; Steenbergen et al, 2005). A number of studies have reported HPV DNA detection in extragenital cancers, although the aetiological involvement of HPV in those malignancies is still controversial (Gillison and Shah, 2003). Recently, it has been shown that HPV types 16 and 18 can immortalize normal breast epithelium (Band et al, 1990; Wazer et al, 1995). This raised the possibility that HPV may be aetiologically related to some cases of breast cancer. However, unlike cervical carcinoma, which is almost always associated with HPV, the causal role of HPV infection in the development of breast carcinoma remains controversial.
Di Lonardo et al (1992) were the first to report the relationship between HPV and breast cancer, demonstrating HPV-16 DNA in 29.4% of breast carcinomas, using PCR with primer sets specific for HPV-11, -16, and -18 genotypes. A study in Norway, which used primers specific for HPV-11, -16, -18, and -33, in addition to GP5+/6+ primers, detected HPV in 46% of breast carcinomas. In this previous study, only HPV-16 was detected (Hennig et al, 1999). Another European study showed the presence of high-risk HPVs in 15% of invasive breast carcinomas in Greece (Kroupis et al, 2006). A Chinese study also found that 35% of breast carcinomas examined were HPV-16-positive, using type-specific primers for HPV-16 and consensus primers for the HPV L1 gene (Liu et al, 2001). In addition, a study in Korea reported HPV DNA presence in breast carcinomas (6.5%) but not in intraductal papilloma (Choi et al, 2007). Furthermore, a study in Brazil demonstrated HPV-16 and HPV-18 in 14 and 10% of breast carcinomas, respectively, using genotype-specific primers (Damin et al, 2004). In addition, an Australian study reported by Kan et al (2005) used primers specific for HPV-16, -18, and -33, and demonstrated the presence of HPV-18 in 48% of breast cancer specimens. However, neither HPV-16 nor HPV-33 was detected in their study. Another study conducted in China and Japan, which used primers for HPV-16, -18, and -33, detected HPV-33 in 41.7 and 11.1% of breast carcinomas in two countries, respectively (Yu et al, 1999). By examining nipple and breast cancer specimens, de Villiers et al (2005) detected high-risk and low-risk HPVs in 86% of them. They used GP5+/6+, FAP primers for cutaneous-type HPVs, and CP primers. In contrast, several other studies failed to demonstrate HPV DNA in tumors of the breast (Wrede et al, 1992; Lindel et al, 2007).
In malignant transformation of the uterine cervical epithelia, the integration of high-risk HPV DNA into the host genome is considered an important step (zur Hausen, 1991). Viral DNA integration leads to frequent disruption of the HPV-16 E2 gene (Kalantari et al, 1998), a negative regulator of the E6/E7 promoter, resulting in the upregulation of the transcription of the E6 and E7 oncogenes. Human papillomavirus-16 E6 and E7 oncogenes interfere with the normal cell cycle by targeting the p53 and pRb tumor suppressor proteins, respectively (Vousden, 1993). Human papillomavirus-16 DNA integration into the host genome possibly provides a selective growth advantage to the host cell (Jeon et al, 1995; Jeon and Lambert, 1995).
When considering the aetiological role of HPV in non-genital cancers, an important question that should be addressed is the integration of HPV into the host genome. Venuti et al (2000) found that 43% of HPV-16-positive laryngeal carcinomas had HPV-16 DNA integrated into the host genome. Koskinen et al (2003) also reported that 65% of HPV-16-positive head and neck carcinomas had integrated HPV-16 DNA. Recent studies conducted by our laboratory also showed that most HPV-16-positive esophageal and lung carcinomas had integrated HPV-16 DNA (Aguayo et al, 2007; Shuyama et al, 2007). To our knowledge, however, none of the published studies have investigated the possibility of integration of HPV in breast cancer tissues.
Considering the controversial reports on the aetiology of HPV in breast carcinomas, the aim of this study was to examine the presence, genotype, viral load, and physical status of HPV, particularly high-risk HPV, among breast carcinomas in Japan, where breast cancer risk is low when compared with Europe and North America (Parkin et al, 2002), and to investigate its aetiological role.
Materials and methods
Study subjects
A total of 124 formalin-fixed and paraffin-embedded breast cancer specimens consisting of 42 cases from Sagara Hospital (Kagoshima, Japan), diagnosed during the period between 2000 and 2001, and 82 cases from Kagoshima University Hospital (Kagoshima, Japan), diagnosed during the period between 2000 and 2006, were examined in this study. In addition, as positive controls, we examined formalin-fixed and paraffin-embedded specimens from six cervical cancer cases diagnosed at Kagoshima University Hospital. Clinicopathological information, including the expression of oestrogen and progesterone receptors, reproductive histories, and family history of breast cancer, was obtained from medical and pathological records. Histological classification for breast cancer was made using the guidelines determined by the Japanese Breast Cancer Society (2004). With regard to cervical cancer, we also applied the guidelines determined by the Japan Society of Obstetrics and Gynaecology, The Japanese Society of Pathology, and the Japan Radiological Society (1999). The Institutional Review Board of Kagoshima University Graduate School of Medical and Dental Sciences (Japan) approved this study.
DNA extraction
Sections of 10 μm thickness were cut and collected in sterile tubes. To avoid contamination between samples, a cutter blade was changed between each sample cutting. For DNA extraction from paraffin-embedded tissue, each sample was treated with 0.8 ml of lemosol and 0.2 ml of ethanol, and subsequently washed with 1 ml of ethanol. After centrifugation and air-drying, the pellet was resuspended in digestion buffer (50 mM Tris-HCl pH 8.0, 1 mM EDTA, pH 8.0, and 0.5% Tween 20) containing 200 μg ml−1 of proteinase K (Invitrogen Corp., Carlsbad, CA, USA) and incubated for 24 h at 56°C. The solution was then heated at 100°C for 10 min, followed by phenol–chloroform extraction and ethanol precipitation of DNA. DNA quality and the absence of PCR inhibitors in samples were tested by PCR for β-globin using PCO3 5′-ACACAACTGTGTTCACTAGC-3′ and PCO4 5′-CAACTTCATCCACGTTCACC-3′ primers under the following PCR conditions: initial denaturation at 95°C for 15 min, 40 cycles with the cycling profile of 95°C for 1 min, 52°C for 1 min, 72°C for 1 min, and final extension for 5 min at 72°C.
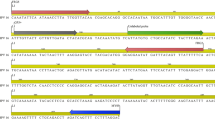
HPV detection and genotyping
The HPV genome was detected with a broad-spectrum SPF10-biotinylated primer PCR. The PCR products, 65 bp of the L1 gene, were run on a 4% agarose gel and visualized with ethidium bromide staining by electrophoresis. Human papillomavirus typing of the HPV DNA-positive samples was performed using the INNO-LiPA HPV Genotyping v2 test (Innogenetics, Ghent, Belgium) (Ketler et al, 1999). In addition, we also analysed all samples through additional type-specific PCR using primer sets targeting the E6 regions of HPV-18 and HPV-33 (Yu et al, 1999). These type-specific primers could detect 140 bp in the E6 region of HPV-18 and HPV-33.
Paraffin sections without tissue and distilled water were used as negative controls for procedures of DNA extraction and PCR, respectively. Full genomes of HPV-16 and HPV-18 cloned in pUC19 plasmid (kindly given by Dr Massimo Tommasino, IARC, Lyon, France), and HPV-33-positive cervical cancer specimens were used as positive controls for amplification.
Quantitative real-time PCR
To determine the presence and physical status, as well as estimate the viral load of HPV-16, real-time PCR was performed with the ABI Prism 7700 Sequence Detection System (Applied Biosystems, Foster City, CA, USA) and 2 × QuantiTect SYBR Green PCR kit (Qiagen, Hilden, Germany). The HPV-16 primers for E6 ORF amplification were as follows: E6F: 5′-GAGAAACTGCAATGTTTCAGGACC-3′ and E6R: 5′-TGTATAGTTGTTTGCAGCTCTGTGC-3′. The HPV-16 primers for E2 ORF amplification were as follows: E2F: 5′-AACGAAGTATCCTCTCCTGAAATTATTAG-3′ and E2R: 5′-CCAAGGCGACGGCTTTG-3′. The PCR amplification conditions were 2 min at 50°C, 15 min at 95°C, and a two-step cycle of 95°C for 15 s, and 60°C for 60 s for a total of 40 cycles (Peitsaro et al, 2002). The sizes of the E6 and E2 products were 81 and 76 bp, respectively.
Serial dilutions of the full-length HPV-16 genome, containing equivalent amounts of E2 and E6 genes from 86 to 862 million copies per reaction, served as a standard control. Numbers of the threshold cycle obtained from E2 PCR and E6 PCR were equivalent in each run. Linear plots of the log of copy number vs numbers of threshold cycle were consistently obtained for both genes.
Real-time PCR for the β-globin gene was performed by the 2 × QuantiTect SYBR Green PCR kit (Qiagen) using PC03/PC04 to adjust the differences in the amount of input genomic DNA between samples. A seven-fold dilution series of a human DNA control (Dynal, UK Ltd, Bromborough, Wirral, Merseyside, UK) was used to generate the standard curve. The amount of β-globin DNA present in each sample was divided by the weight of one genome equivalent (that is, 6.6 pg per cell) and a factor of 2 (as there are two copies of β-globin DNA/genome equivalent or cell) to obtain the number of genome equivalents or cell in the sample. Viral loads in each specimen were expressed as the number of HPV copies per 104 cells.
Immunohistochemistry for HER2/neu overexpression
HER2/neu overexpression was examined, using the Hercep Test kit (Dako, Carpinteria, CA, USA) following the manufacturer's instructions. Control cell lines provided by the manufacturer (Dako) were used as negative and positive controls. The data on its oevererexpression for 17 HPV-positive breast carcinomas (16 invasive carcinomas and 1 non-invasive carcinoma) and 42 HPV-negative carcinomas (40 invasive carcinomas and 2 non-invasive carcinoma) were obtained from medical records. In the HPV-positive cases, HER2/neu expression was additionally examined in seven cases. Following the Hercep Test criteria, the immunoreaction was scored as follows: 3+, complete and intense membrane staining of >10% tumor cells; 2+, complete but moderate staining of >10% tumor cells; 1+, weak and incomplete staining in >10% tumor cells; and 0, no membrane staining or staining in <10% tumor cells. We defined cases with a score 3+ as HER2/neu overexpression.
Statistical analysis
Fisher's exact test was conducted to test statistical significance using STATA (version 8.5, Stata Corporation, College Station, TX, USA). All the P-values presented are two-sided.
Results
We examined 124 female breast cancer cases, aged from 23 to 90 years with a mean of 55 years. β-globin amplification was carried out to check the quality of DNA in formalin-fixed and paraffin-embedded specimens. All samples were positive for β-globin gene amplification, indicating that DNA was available for molecular analysis.
First, we examined all samples using novel, broad-spectrum SPF10 primers for HPV detection. Human papillomavirus DNA was positive in 24 out of 124 (19%) breast cancer specimens. As an alternative approach, we examined all specimens using primer sets targeting the E6 region of HPV genotypes 16, 18, and 33. By using genotype-specific primers, HPV-16 was detected in two new cases. No additional cases of HPV-18 and HPV-33 were detected by genotype-specific approach. Thus, in total, HPV DNA was detected in 26 (21%) breast cancer specimens.
Table 1 presents the HPV frequency according to various clinicopathological features. There was no significant difference in the HPV detection rate between invasive and non-invasive carcinomas. Among invasive carcinomas, HPV DNA was detected in 7 (20%) papillotubular carcinomas, 5 (29%) solid-tubular carcinomas, and 9 (20%) scirrhous carcinomas. Human papillomavirus detection rates were not different among those histological types of invasive carcinomas (data not shown in the table). The presence of HPV was not related to the expression of oestrogen and progesterone receptors. Among the 12 patients with bilateral breast carcinomas, we could obtain breast cancer specimens from the other side from 2 HPV-positive and 2 HPV-negative cases. We also examined the presence of HPV DNA in these specimens by the same PCR methods. However, none of them was HPV-positive.
HER2/neu expression was examined in 23 invasive and 1 non-invasive HPV-positive breast carcinomas. Three (13%) invasive carcinomas had its overexpression (score of 3+) and the non-invasive carcinoma had no HER2/neu overexpression (score=1). On the other hand, in HPV-negative carcinomas, its overexpression was observed in 6 out of 40 (15%) invasive carcinomas, and in 1 out of 2 non-invasive carcinomas. Neither in HPV-positive nor in HPV-negative carcinomas HER2/neu overexpression was associated with any clinicopathological factors, including tumor size, lymph vessel invasion, vascular invasion, and lymph node metastasis (data not shown).
The most prevalent HPV type was HPV-16, which was detected in 24 (92%) out of 26 HPV-positive cases, using the INNO-LiPA HPV genotyping assay and the type-specific approach (Table 2). Among them, three cases (BC-72, BC-78, and BC-112) were identified as HPV-16-positive only by the PCR with HPV-16-specific primers. Other HPV types, identified only by the INNO-LiPA HPV genotyping assay, were HPV-6 in 12 (50%) cases, HPV-18 in 3 (12%) cases, HPV-51 in 2 (8%) cases, and HPV-33 in 1 (4%) case. Multiple infections were found in 12 (46%) HPV-positive cases (Table 2).
All of the HPV-16-positive breast carcinoma specimens were subjected to quantitative real-time PCR analysis to determine the viral load and physical status of HPV-16. The HPV-16 copy numbers of E6 and E2 genes per 104 cells, the ratios of E2 to E6, and the viral physical status are compiled in Table 2. The geometric mean of HPV-16 copies per 104 cells was 5.4 in cancers of the breast and 130 480 in cancers of the uterine cervix. In 19 (95%) breast carcinoma cases, E2 DNA was not detected, and in 1 (5%) case, E2 DNA was detected, but the E2/E6 ratio was less than unity. In cervical carcinoma cases, there were two (33%) cases where E2 DNA was not detected. On the other hand, there were four (67%) cases where the E2 DNA was detected, but the E2/E6 ratio was less than unity.
For 11 HPV-16-positive breast carcinoma specimens, we examined the presence of HPV DNA in 1 specimen of morphologically normal breast tissue adjacent to the carcinoma. Human papillomavirus-16 DNA was detected in seven (64%) of these specimens (Table 3). The geometric mean of viral load in the normal tissue was 92 copies per 104 cells, which was higher than that in breast carcinomas (5.4 copies per 104 cells); however, the difference was not statistically significant (P=0.162 by the Mann–Whitney test). The analysis of the E2/E6 ratio in normal epithelium specimens showed that in one (17%) case, E2 DNA was not detected, and in four (66%) cases, E2 DNA was detected but the E2/E6 ratio was less than unity. The remaining one (17%) case had an E2/E6 ratio of approximately one. We also examined 11 normal breast specimens adjacent to HPV-negative breast tumor tissue, but none of them was HPV-positive (Table 3). The difference in HPV detection rates in surrounding normal mucosa of HPV-positive and HPV-negative breast carcinoma cases was statistically significant (P=0.004 by Fisher's exact test).
Discussion
In this study, we found HPV DNA in 21% (n=26) of breast carcinomas in Japan. Another study conducted in Japan detected HPV DNA in 11.1% of breast carcinomas (Yu et al, 1999). High-risk types, such as HPV-16, -18, and -33, were detected in our study. Despite great variability in the HPV detection rate worldwide, the majority of HPV types that are detected are the oncogenic types, HPV-16 and -18 (Di Lonardo et al, 1992; Hennig et al, 1999; Liu et al, 2001; Damin et al, 2004; Kan et al, 2005). Our results are in agreement with these previous reports. The association of high-risk HPV was reported to be stronger in invasive carcinomas (Yasmeen et al, 2007b). In this study, however, the HPV frequency in invasive carcinomas was higher than that of non-invasive carcinomas although the difference was not statistically significant (P=0.279).
The physical status of HPV-16 was determined by the HPV-16 E2/E6 ratio in this study. When the ratio was equal to or higher than unity, all of the HPV-16 genome was considered to be in the episomal form. Note, however, the E2/E6 ratio of unity or larger does not necessarily deny the possibility of HPV integration because HPV integration does not always cause E2 disruption (Vernon et al, 1997; Eriksson et al, 1999). However, as we found no breast carcinoma with the exclusive presence of episomal HPV-16 (E2/E6 ratio being equal to or higher than unity), this assumption does not affect the interpretation of our observations. On the other hand, the lack of amplified HPV-16 E2 genome was considered to indicate the integration of all of the HPV-16 DNA into the host genome. When the E2/E6 ratio was larger than zero and smaller than unity, this condition was considered as a mixture of episomal and integrated forms (Peitsaro et al, 2002). We found HPV-16 DNA integrated into the host genome in all HPV-16-positive breast carcinoma cases, although one case harboured both integrated and episomal forms of HPV-16. In cervical cancer samples, 67% of the samples had HPV-16 in a mixed form, where HPV existed in both episomal and integrated forms, and 33% of the samples had only the integrated form of HPV. To our knowledge, this is the first study reporting the physical status of HPV-16 in breast cancer tissues.
In this study, the HPV-16 viral load determined by quantitative real-time PCR in breast carcinoma was with a geometric mean of 5.4 per 104 cells, which was much lower than that observed in cervical cancer (geometric mean=130480). It is unlikely, however, that the low viral loads in breast carcinoma specimens were a consequence of formalin fixation and/or heating during paraffin embedding, as a higher viral load was detected in formalin-fixed and paraffin-embedded specimens of cervical cancer obtained from the same institute. Moreover, we performed parallel amplification of a housekeeping gene (β-globin) to obtain an estimate of the amount of amplifiable genomic DNA in each sample, and to help reconcile the inhibitory effects of formalin fixation and paraffin embedding on DNA amplification.
A low copy number of HPV-16 in non-genital carcinomas has also been reported in studies of Chilean lung carcinomas (Aguayo et al, 2007) and Chinese oesophageal cancer (Shuyama et al, 2007) conducted by our laboratory, and in a Finish study on head and neck cancer (Koskinen et al, 2003). It should also be noted that SiHa cells, which are a cervical cancer cell line, contain only 1–2 copies of HPV-16 per cell. Such a low copy number of HPV DNA in SiHa cells suggests that a viral load as low as 1 copy per cell may be sufficient to promote carcinogenesis, especially if the viral DNA is integrated into the host cell genome (Si et al, 2005). In this study, however, the viral load in breast carcinoma was much lower than 1 copy per cell. As breast cancer is considered a monoclonal expansion and the integrated HPV genome is unlikely to disappear from the host genome during cell replication, at least one copy of integrated HPV is expected to be present in all carcinoma cells even if only a copy of integrated HPV is sufficient for its aetiological involvement. Therefore, even though HPV-16 was found integrated in breast cancer cells in this study, its extremely low viral load suggests that HPV-16 DNA is unlikely to be involved in the development of those breast carcinomas.
In this study, HPV-16 was also found in 64% of normal mucosal specimens adjacent to HPV-16-positive tumors but not in the non-malignant epithelia from HPV-16-negative tumors. The presence of HPV-16, not only in breast carcinomas but also in adjacent normal tissue, can also be explained by the infection of HPV in carcinomas after their development because both carcinoma and adjacent normal tissue are likely to be exposed to such an infection.
Hormonal factors (namely, oestrogen, and its derivatives) are known to be involved in breast carcinogenesis (Pike et al, 1993). Oestrogen receptor-positive breast carcinomas are more sensitive to tamoxifen, an antioestrogen. An interesting question is whether oestrogen-related breast cancer is strongly related to HPV. In this regard, Hennig et al (1999) and Damin et al (2004) reported that the presence of oestrogen or progesterone receptor was not related to HPV presence in breast carcinomas. We also did not observe any significant association of HPV presence with oestrogen and progesterone receptor expression.
Approximately 25–30% of all breast cancers have an amplification of the HER2/neu gene or overexpression of its protein product (Slamon et al, 1987). Yasmeen et al (2007a) reported that E6/E7 of HPV-16 cooperates with the HER2/neu receptor to induce breast tumorigensis and metastasis. This study, however, did not show any evidence indicating that HPV presence affects the relationship between HER2/neu overexpression and tumor invasiveness.
We did not find any difference in the average age at diagnosis between HPV-positive and HPV-negative breast cancers. Similar results were described in studies of Norwegian and Brazilian women (Hennig et al, 1999; Damin et al, 2004). In contrast, Kroupis et al (2006) and Lawson et al (2006) demonstrated that the average age of women with HPV-positive breast cancer is significantly younger than women with HPV-negative breast cancer, suggesting that sexual activity is one of the risk factors of HPV-positive breast cancer.
In cervical cancer, the cytopathic effect of HPV infection is well known as koilocytosis. There are several studies reporting similar histological features among non-genital cancers (Miller et al, 1997; Al-Qahtani et al, 2007). Although we reviewed haematoxylin–eosin staining slides of all HPV-positive cases, none of them showed pathological features of HPV infection such as koilocytes (data not shown).
The transmission route of HPV detected in breast carcinoma is yet unclear. Two independent studies suggested possible hematogenic and/or lymphatic transfer of the virus from one organ to another (Hennig et al, 1999; Widschwendter et al, 2004). Interestingly, the study by Hennig et al (1999) detected HPV-16 DNA in 46% of breast cancer occurring among women with a history of high-grade cervical intraepithelial neoplasia (CIN III). Their finding suggests that HPV-associated cervical neoplasia might be the original site of HPV infection from which the virus could be transported to the breast. In our study, there were four breast cancer cases with a history of cervical cancer but only 1 of them was HPV-positive in their breast tumors. de Villiers et al (2005) showed HPV presence in the nipple, suggesting HPV transfer in a retrograde fashion from the nipple via areola, lactiferous ducts, and sinuses.
The reported prevalence of HPV infection in breast cancer shows a great variation worldwide, ranging from 0 to 86% (Hennig et al, 1999; Damin et al, 2004; de Villiers et al, 2005; Kan et al, 2005; Kroupis et al, 2006; Choi et al, 2007; Lindel et al, 2007; Yasmeen et al, 2007b). Demographic features and genetic backgrounds may contribute to the geographical difference of HPV prevalence in breast carcinomas worldwide. In addition, the difference in published reports may be attributed to the numbers of samples tested, methodological differences, and the sensitivity of methods used, such as use of different primer sets. In this study, the use of HPV-16-specific primers detected three additional HPV-16-positive cases, which were HPV-16-negative by SPF10-PCR, although the SPF10 primer set is considered highly sensitive. The discrepancy between the SPF10 consensus primer set PCR and PCR with HPV-16-specific primers stems from the fact that SPF10 primers target the sequence of the L1 gene, which may be lost during the integration of HPV-16 into the host genome (Noffsinger et al, 1995; Karlsen et al, 1996).
In summary, HPV DNA was detected in 26 (21%) breast carcinomas and, in all HPV-16-positive cases, the HPV genome was considered to be integrated into the host genome. However, their extremely low viral loads suggest that it is unlikely that integrated HPV-16 is aetiologically involved in the development of Japanese breast cancer cases examined in this study. As reported by Shuyama et al (2007), the role of HPV in non-genital cancer may vary in different study areas. Therefore, in the case of breast cancer, we cannot deny the possibility that HPV may play a significant role in breast cancer development in other countries. Further studies are warranted to elucidate the aetiological role and pathogenesis of HPV in breast cancer.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Aguayo F, Castillo A, Koriyama C, Higashi M, Itoh T, Capetillo M, Shuyama K, Corvalan A, Eizuru Y, Akiba S (2007) Human papillomavirus-16 is integrated in lung carcinomas: a study in Chile. Br J Cancer 97: 85–91
Al-Qahtani K, Brousseau V, Paczesny D, Domanowski G, Hamid Q, Hier M, Black M, Franco E, Kost K (2007) Koilocytosis in oral squamous cell carcinoma: what does it mean? J Otolaryngol 36: 26–31
Band V, Zajchowski D, Kulesa V, Sager R (1990) Human papillomavirus DNAs immortalize human mammary epithelial cells and reduce their growth factor requirements. Proc Natl Acad Sci USA 87: 463–467
Choi YL, Cho EY, Kim JH, Nam SJ, Oh YL, Song SY, Yang JH, Kim DS (2007) Detection of human papillomavirus DNA by DNA Chip in breast carcinomas of Korean Women. Tumor Biol 28: 327–332
Cuschieri KS, Cubie HA, Whitley MW, Gilkison G, Arends MJ, Graham C, McGoogan E (2005) Persistent highrisk HPV infection associated with development of cervical neoplasia in a prospective population study. J Clin Pathol 58: 946–950
Damin APS, Karam R, Zettler CG, Caleffi M, Alexandre COP (2004) Evidence for an association of human papillomavirus and breast carcinomas. Breast Cancer Res Treat 84: 131–137
de Villiers EM, Sandstrom RE, zur Hausen H, Buck CE (2005) Presence of papillomavirus sequences in condylomatous lesions of the mamillae and in invasive carcinoma of the breast. Breast Cancer Res 7: R1–R11
Di Lonardo A, Venuti A, Marcante ML (1992) Human papillomavirus in breast cancer. Breast Cancer Res Treat 21: 95–100
Eriksson A, Herron JR, Yamada T, Wheeler CM (1999) Human papillomavirus type 16 variant lineages characterized by nucleotide sequence analysis of the E5 coding segment and the E2 hinge region. J Gen Virol 80: 595–600
Gillison ML, Shah KV (2003) Role of mucosal human papillomavirus in nongenital cancers. J Natl Cancer Inst Monogr 31: 57–65
Hennig EM, Suo Z, Thoresen S, Holm R, Kvinnsland S, Nesland JM (1999) Human papillomavirus 16 in breast cancer of women treated for high-grade cervical intraepithelial neoplasia (CIN III). Breast Cancer Res Treat 53: 121–135
Japan Society of Obstetrics and Gynaecology, The Japanese Society of Pathology, and The Japan Radiological Society (1999) General Rules for Clinical and Pathological Study of Uterine Cervical Cancer in Japan. pp 20–66. Kanehara and Co., Ltd: Tokyo, Japan
Jeon S, Allen-Hoffmann BL, Lambert PF (1995) Integration of human papillomavirus type 16 into the human genome correlates with a selective growth advantage of cells. J Virol 69: 2989–2997
Jeon S, Lambert PF (1995) Integration of human papillomavirus type 16 DNA into the human genome leads to increased stability of E6 and E7 mRNAs: implications for cervical carcinogenesis. Proc Natl Acad Sci USA 92: 1654–1658
Kalantari M, Karlsen F, Kristensen G, Holm R, Hagmar B, Johansson B (1998) Disruption of the E1 and E2 reading frames of HPV 16 in cervical carcinoma is associated with poor prognosis. Int J Gynecol Pathol 17: 146–153
Kan CY, Iacopetta BJ, Lawson JS, Whitaker NJ (2005) Identification of human papillomavirus DNA gene sequences in human breast cancer. Br J Cancer 93: 946–948
Karlsen F, Kalantari M, Jenkins A, Pettersen E, Kristensen G, Holm R, Johansson B, Hagmar B (1996) Use of multiple PCR primer sets for optimal detection of human papillomavirus. J Clin Microbiol 34: 2095–2100
Ketler B, van Doorn LJ, Schrauwen L, Molijin A, Sastrowijoto S, ter Schegget J, Lindeman J, ter Harmsel B, Burger M, Quint W (1999) Development and clinical evaluation of a highly sensitive PCR-reverse hybridization line probe assay for detection and identification of anogenital human papillomavirus. J Clin Microbiol 37: 2508–2517
Koskinen W, Chen RW, Leivo I, Makitie A, Back L, Kontio R, Suuronen R, Lindqvist C, Auvinen E, Molijn A, Quint WG, Vaheri A, Aaltonen LM (2003) Prevalence and physical status of human papillomavirus in squamous cell carcinomas of the head and neck. Int J cancer 107: 401–406
Kroupis C, Markou A, Vourlidis N, Dionyssiou-Asteriou A, Lianidou ES (2006) Presence of high-risk human papillomavirus sequences in breast cancer tissues and association with histopathological characteristics. Clin Biochem 39: 727–731
Lawson JS, Kan CY, Iacopetta BJ, Whitaker NJ (2006) Are some breast cancers sexually transmitted? Br J Cancer 95: 1708
Lindel K, Forster A, Altermatt HJ, Greiner R, Gruber G (2007) Breast cancer and human papillomavirus (HPV) infection: no evidence of a viral etiology in a group of Swiss women. Breast 16: 172–177
Liu Y, Klimberg VS, Andrews NR, Hicks CR, Peng H, Chiriva-Internati M, Henry-Tilman R, Hermonat PL (2001) Human papillomavirus DNA is present in a subset of unselected breast cancers. J Hum Virol 4: 329–334
Miller BA, Davidson M, Myerson D, Icenogle J, Lanier AP, Tan J, Beckmann AM (1997) Human papillomavirus type 16 DNA in esophageal carcinomas from Alaska natives. Int J Cancer 71: 218–222
Noffsinger AE, Suzuk L, Hui YZ, Gall AA, Fenoglio-Preiser CM (1995) Differential sensitivities of E6 type-specific and L1 consensus primers in the detection of human papillomavirus in anal carcinoma. Mod Pathol 8: 509–514
Parkin DM, Pisani P, Ferlay J (1999) Global cancer statistics. Ca Cancer J Clin 49: 33–64
Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB (2002) Cancer Incidence in Five Continents, VIII. pp 602–605. IARC: Lyon, France (Scientific publications no. 155)
Peitsaro P, Johansson B, Syrjanen S (2002) Integrated human papillomavirus type 16 is frequently found in cervical cancer precursors as demonstrated by a novel quantitative real-time PCR technique. J Clin Microbiol 40: 886–891
Pike MC, Spicer DV, Dahmoush L, Press MF (1993) Estrogens, progestogens, normal breast cell proliferation, and breast cancer risk. Epidemiol Rev 15: 17–35
Shuyama K, Castillo A, Aguayo F, Sun Q, Khan N, Koriyama C, Akiba S (2007) Human papillomavirus in high- and low-risk areas of oesophageal squamous cell carcinoma in China. Br J Cancer 96: 1554–1559
Si HX, Tsao SW, Poon CS, Wong YC, Cheung AL (2005) Physical status of HPV-16 in esophageal squamous cell carcinoma. J Clin Virol 32: 19–23
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL (1987) Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235: 177–182
Steenbergen RD, de Wilde J, Wilting JSM, Brink AA, Snijders PJ, Meijer CJ (2005) HPV mediated transformation of the anogenital tract. J Clin Virol 32: 25–33
The Japanese Breast Cancer Society (2004) General Rules for Clinical and Pathological Recording of Breast Cancer pp 32–68. Kanehara and Co. Ltd: Tokyo, Japan
Tsai JH, Hsu CS, Tsai CH, Su JM, Liu YT, Cheng MH, Wei JC, chen FL, Yang CC (2007) Relationship between viral factors axillary lymph node status and survival in breast cancer. J Cancer Res Clin Oncol 133: 13–21
Venuti A, Manni V, Morello R, De Marco F, Marzetti F, Marcante ML (2000) Physical state and expression of human papillomavirus in laryngeal carcinoma and surrounding normal mucosa. J Med Virol 60: 396–402
Vernon SD, Unger ER, Miller DL, Lee DR, Reeves WC (1997) Association of human papillomavirus type 16 integration in the E2 gene with poor disease-free survival from cervical cancer. Int J Cancer 74: 50–56
Vousden K (1993) Interactions of human papillomavirus transforming proteins with the products of tumor suppressor genes. FASEB 7: 872–879
Wazer DE, Liu XL, Chu Q, Gao Q, Band V (1995) Immortalization of distinct human mammary epithelial cell types by human papillomavirus 16 E6 or E7. Proc Natl Acad Sci USA 92: 3687–3691
Widschwendter A, Brunhuber T, Wiedemair A, Mueller-Holzner E, Marth C (2004) Detection of human papillomavirus DNA in breast cancer of patients with cervical cancer history. J Clin Virol 31: 292–297
Wrede D, Luqmani YA, Coombes RC, Vousden KH (1992) Absence of HPV 16 and 18 DNA in breast cancer. Br J Cancer 65: 891–894
Yasmeen A, Bismar TA, Dekhil H, Ricciardi R, Kassab A, Gambacorti-Passerini C, Al Moustafa AE (2007a) ErbB-2 receptor cooperates with E6/E7 oncoproteins of HPV type 16 in breast tumorigenesis. Cell Cycle 6: 2939–2943
Yasmeen A, Bismar TA, Kandouz M, Foulkes WD, Desprez PY, Al Moustafa AE (2007b) E6/E7 of HPV type 16 promotes cell invasion and metastasis of human breast cancer cells. Cell Cycle 6: 2038–2042
Yu Y, Morimoto T, Sasa M, Okazaki K, Harada Y, Fujiwara T, Irie Y, Takahashi E, Tanigami A, Izumi K (1999) HPV 33 DNA in premalignant and malignant breast lesions in Chinese and Japanese populations. Anticancer Res 19: 5057–5061
zur Hausen H (1991) Human papillomaviruses in the pathogenesis of anogenital cancer. Virology 184: 9–13
Acknowledgements
This work was financed by Grants-in-Aid for Scientific Research on Priority Areas (17015037) of the Ministry of Education, Culture, Sports, Science and Technology, Japan. We thank Ms Yoshie Minakami for her technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Khan, N., Castillo, A., Koriyama, C. et al. Human papillomavirus detected in female breast carcinomas in Japan. Br J Cancer 99, 408–414 (2008). https://doi.org/10.1038/sj.bjc.6604502
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604502
Keywords
This article is cited by
-
Catching viral breast cancer
Infectious Agents and Cancer (2021)
-
High-risk human papillomaviruses and Epstein–Barr virus in breast cancer in Lebanese women and their association with tumor grade: a molecular and tissue microarray study
Cancer Cell International (2021)
-
The association between HPV gene expression, inflammatory agents and cellular genes involved in EMT in lung cancer tissue
BMC Cancer (2020)
-
Human papilloma virus and breast cancer: the role of inflammation and viral expressed proteins
BMC Cancer (2019)
-
Presence of human papillomavirus DNA in breast cancer: a Spanish case-control study
BMC Cancer (2017)