Key Points
-
Amalgam continues to be preferred for core build-ups.
-
Despite their disadvantages dentine pins are still widely used.
-
Laminate veneers are preferred by younger practitioners for the restoration of anterior teeth.
-
All-ceramic crowns are prescribed occasionally and a significant number of practitioners do not prescribe them.
-
For inlay/onlay type restorations, ceramic is the preferred material and there is considerable uncertainty about which material to use for these restorations.
Abstract
Objectives: To investigate, by questionnaire, the use and selection of materials and techniques for indirect restorations and fixed prosthodontics by dental practitioners in the North West of England and Scotland.
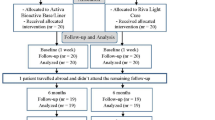
Methods: A questionnaire was sent to 1,000 general dental practitioners selected at random from dentists in Scotland and the North West of England. Non-responders were sent another questionnaire after a period of 4 weeks had elapsed.
Results: A total of 701 usable questionnaires were returned, giving a response rate of 70%. When selecting a material for the core build-up of vital teeth, practitioners used the following materials (%): amalgam (60), dual and light-cured resin composite (54), glass-ionomer cements (47), compomer (29) and resin-modified glass-ionomer cements (24). Where the use of a post was indicated indirect posts of both precious (67) and non-precious (37) alloys were preferred to prefabricated posts by the majority of practitioners for the restoration of root filled teeth. Direct titanium (14) and stainless steel (14) posts were not used extensively. Impression materials used by the practitioners were as follows: addition-cured silicone (70), condensation-cured silicone (20), polyether (9) and polysulphide (2). Traditional glass-ionomer cements (59) were used for the luting of single and multiple porcelain fused to metal units, with zinc phosphate and polycarboxylate cements (33) being the preferred alternatives.
Conclusions: The majority of the practitioners surveyed in this study used: amalgam for core build-ups; indirect posts; addition-cured silicone for impressions; and glass-ionomer cements for luting procedures.
Similar content being viewed by others
Introduction
General dental practitioners provide a significant number of indirect restorations and fixed prostheses.1 This is probably due to three principal factors, namely: patients are demanding fixed as opposed to removable prostheses for the replacement of missing teeth; patients are living longer and retaining more teeth; and increasingly indirect restorations are being used to restore damaged and worn teeth to form and function. The recent adult dental health survey demonstrated that the trend towards increasing numbers of adults retaining more teeth is set to continue and it is therefore logical to assume that more fixed prostheses will be both requested by patients and provided by practitioners.2 Against this backdrop practitioners have the opportunity to apply increased choices in terms of materials and techniques many of which have a dubious evidence base.3
Previous studies have looked at the design and prescription of bridgework, standards of tooth preparation for indirect restorations and impressions, but to date little is known about the materials and techniques that practitioners are using for the provision of indirect restorations and fixed prosthodontics in the UK, let alone the extent to which newer materials and techniques have been adopted.4,5,6,7,8 The aim of this study was to investigate, by questionnaire, the use and selection of materials and techniques for indirect restorations and fixed prosthodontics by two selected groups of practitioners in the UK. A further aim was to investigate any differences between the two groups with respect to materials and techniques used.
Materials and methods
A questionnaire, based on an annual survey of practitioners in the USA by clinical research associates, was designed to seek information about various aspects of current practice in primary dental care.9 The questionnaire, which comprised 18 sections and 79 questions, was piloted by 10 practitioners in the North West and in the light of feedback from these practitioners modified for the purposes of the study.
The questionnaire was sent to 1,000 randomly selected practitioners, 500 in the North West and 500 in Scotland, who were selected, by postcode, from databases of practitioners so that there was an even distribution across the two geographical areas being investigated. The questionnaire was sent with a covering letter and a reply paid envelope. After a period of 4 weeks another questionnaire with a covering letter and reply paid envelope was sent to practitioners who had not responded.
A number of questions were asked that related to materials and techniques used for indirect restorations and fixed prosthodontics, namely:
-
Material selection for core build-up in vital teeth and whether pins were used
-
Type of post and core system used for the restoration of non-vital teeth
-
Impression materials, luting cements, and alloys used
-
Whether crowns or veneers were preferred for the restoration of anterior teeth
-
Use of tooth-coloured inlays and metal free crowns.
The data contained in the returned questionnaires were computerised and analysed using SPSS for Windows version 10.10
A possible relationship between the materials and techniques used for indirect restorations or fixed prosthodontics and the practitioner's age, in terms of years since graduation, gender, practice location and number of practitioners in the practice was explored using appropriate statistical tests. Cross-tabulation and non-parametric tests such as Mann Whitney and Kruskal Wallis were performed. The level of significance was set at 1% because of the number of tests being carried out, and to reduce the chance of getting false positive results.
Results
In all, 701 usable questionnaires were returned — 345 from the North West of England and 356 from Scotland — giving an overall response rate of 70%. The demographics of this group of practitioners have been described previously.11
Core-build up for vital teeth
The majority (n = 418, 60%) of practitioners in this study used amalgam for core build-up of vital teeth with glass ionomer cements (n = 329, 47%) and light-cured resin composite (n = 296, 42%) as preferred alternatives. Using the Mann Whitney U test it was apparent that more recently qualified practitioners tended to use light-cured resin composite than older practitioners (P = 0.006). There is a significant association between material use for vital teeth and the location of practice in the two national regions at the 1% level, with Fisher's exact test P = 0.002. Of those who use light-cured resin composite, 42% were in the North West compared with 58% in Scotland. There is a very strong association between gender of dentists and the use of amalgam as the core build-up material used for vital teeth, with a Fisher's exact test of P < 0.0001. Of those who did not use amalgam for vital teeth, 81% were male dentists compared with 19% female dentists. Compomer (n = 203, 29%) and resin modified glass-ionomer cements (n = 170, 24%) were used regularly with dual (n = 82, 12%) and chemically cured (n = 69, 10%) resin composites infrequently used (Table 1).
Dentine pins
The majority of the practitioners used dentine pins with a small number (n = 64, 9%) electing not to use pins at all. There was a regional variation in the use of any type of dentine pins and this was significant at the 1% level with Fisher's exact test P = 0.01. Of those who did not use stainless steel retentive pins, 46% were in the North West compared with 55% in Scotland. Where dentine pins were used, stainless steel (n = 259, 37%) or titanium alloy (n = 214, 31%) pins were the most widely used with pure titanium (n = 151, 22%) or gold anodised stainless steel (n = 37, 5%) pins being used infrequently (Table 2). The Mann Whitney U test indicates that stainless steel pins were preferred by more recent graduates and this difference was very highly significant (P < 0.0001). In contrast, pure titanium pins were preferred by older practitioners and this difference was again significant (P = 0.004).
Post systems
Indirect cast posts were preferred by a majority of practitioners and these were more commonly produced from a precious (n = 469, 67%) as opposed to a non-precious alloy (n = 262, 37%). Direct posts of stainless steel (n = 95, 14%), titanium alloy (n = 70, 10%) and pure titanium (n = 26, 4%) were prescribed less frequently with very few practitioners not placing posts (n = 6, 1%) (Table 3). The use of titanium alloy posts was affected by the number of years the practitioners had been qualified with older practitioners preferring titanium alloy posts. This difference was significant P = 0.01 using the Mann Whitney U test.
Impression materials
Silicone based impression materials, either addition- (n = 487, 70%) or condensation-cured (n = 143, 20%), were the most preferred impression materials by the practitioners in this study. There was some regional variation and this was significant at the 1% level, Fisher's exact test P = 0.009. Of those who did not use addition cured silicone impression material, 42% were in the North West compared with 58% in Scotland. Polyether (n = 61, 9%) and polysulphide (n = 12, 2%) impression materials were also used but less frequently (Table 4).
Bonding alloys
A precious bonding alloy was used almost routinely by a majority (n = 534, 76%) of practitioners, with non-precious alloys used by a minority (n = 136, 19%).
Luting cements
Luting cements based on traditional glass-ionomer cements were used to cement porcelain fused to metal reconstructions by a majority (n = 414, 59%) of the practitioners in this study. The Mann Whitney U test shows that younger practitioners in contrast to older practitioners preferred to use glass-ionomer luting cements for gold restorations (P = 0.009). These cements were also used to cement resin composite (n = 118, 17%), ceramic (n = 268, 38%) and gold (n = 330, 47%) restorations and cast metal posts and cores (n = 413, 59%). Specifically, younger practitioners seem to see resin composite restorations as an absolute indicator for a resin based luting cement whilst older practitioners did not (P < 0.0001). The same difference was noted for the luting of ceramic restorations (p = 0.006). Polycarboxylate (n = 229, 33%) and zinc phosphate (n = 227, 32%) cements were used by a significant number of practitioners.
Luting cements based on resin composite with (n = 43, 6%) or without (n = 49, 7%) a special affinity for metal were used infrequently. However, generally older practitioners preferred resin-based luting cements to younger practitioners (P = 0.012). When single porcelain fused to metal units and gender were being looked at, this is significant at the 1% level with Fisher's exact test P = 0.012. This points to there being a strong relationship between use of resin based cement for single porcelain fused to metal units and the gender of dentists. Of the male dentists, 95% did not use this type compared with 5% who use this type of cement. Of the female dentists, 90% did not use this compared with 10% who use this type of cement. Of those who did not use this type of cement, 75% were male dentists compared with 25% female dentists. Of those who use this type of cement, 56% were male compared with 44% who were female. These cements were used to cement resin composite (n = 300, 43%), ceramic (n = 343, 49%) and gold (n = 67, 10%) restorations and cast metal posts and cores (n = 113, 16%). Compomer (n = 5, 1%) and resin modified glass-ionomer (n = 83, 12%) based luting cements were not used by many practitioners (Table 5). The practitioners were also asked if they would use a different luting cement if multiple units were to be cemented but this proved not to be the case.
Choice of indirect restoration for anterior teeth
The preferred choice of restoration for anterior teeth was laminate veneers (n = 310, 44%), porcelain fused to metal crowns (n = 161, 23%) and all ceramic crowns (n = 138, 20%). It was apparent that more recently graduated practitioners used more veneers than older practitioners and this difference was significant, P = 0.005 using the Mann Whitney U test.
Use of tooth–coloured inlays/onlays and metal free crowns
Out of 701 questionnaires, tooth coloured inlays/onlays were predominately produced (n = 448, 64%) on a refractory die with little (n = 7, 1%) use of restorations produced with the aid of CAD/CAM equipment. The materials chosen to make tooth coloured inlays were ceramic (n = 292, 42%), resin composite (n = 139, 20%), either material (n = 63, 9%) or practitioners were unsure (n = 137, 20%) which material to use. When the materials used for the production of tooth coloured inlays/onlays and gender were investigated, this was significant at the 1% level with Pearson chi-squared value = 10.89, 3 degree of freedom and P = 0.012. This indicates that there is an association between the material used for production of tooth coloured inlays and onlays in premolar teeth and gender of dentists. Of the male dentists, 47% used ceramic compared with 34% who used resin composite, 9% used either and 19% were not sure. Of the female dentists, 43% used ceramic compared with 16% who used resin composite, 12% used either and 29% were not sure. Of those who used ceramic, 76% were male dentists compared with 24% who were female. Of those who used resin composite, 81% were male dentists compared with 19% who were female. Of those who used either, 70% were male dentists compared with 30% who were female. Of those who were not sure, 65% were male dentists compared with 35% who were female. The Mann Whitney U test points to more recently qualified graduates preferring to use either material with older practitioners preferring to use resin composite. This difference was significant (P = 0.01).
The 701 practitioners were asked if they would use different materials for the restoration of molars and premolars, which proved not to be the case. Metal free crowns were not provided regularly (n = 66, 9%) with occasional prescription common (n = 463, 66%) but some practitioners choose not to provide them (n = 153, 22%).
Discussion
A response rate of 70% is considered adequate for limiting non-response bias for questionnaire based studies. This study can therefore be considered to provide useful information about material use and selection by 701 GDPs from two geographic regions of the UK. The demographics of the sample, as previously described, suggests that the sample is representative of 'typical' practitioners and therefore broadly representative of practitioners in the UK.11
Amalgam was the principal choice of the practitioners in this study for the core build-up of vital teeth, which implies core build-up of posterior rather than anterior teeth was common practice. This is not surprising given that traditional teaching, in UK dental schools, has been that amalgam is the material for choice for core build-up of vital and non-vital posterior teeth. This, coupled with the proven longevity of amalgam in this clinical situation, almost certainly explains its widespread use.12 In contrast, significant numbers of practitioners would appear to use light-cured resin composite and traditional glass-ionomer cement as direct core materials. Whilst it is not unreasonable to use resin composite, the physical properties of traditional glass-ionomer cement limits its value as a durable core material.13 It is anticipated that crowns and bridgework supported by cores of traditional glass-ionomer cements are likely to be prone to early failure in clinical service. Surprisingly, there would appear to be limited use of resin-modified glass-ionomer cements for the core build up of vital teeth despite its use being previously recommended.14 Compomer materials, which are generically similar to resin composite, were used to a similar extent to resin-modified glass-ionomer cements. This group of materials has inferior physical properties to those of resin composites and, as a consequence, their use confers no advantage over the use of resin composite, which a small but important number of practitioners in this study did not appear to have appreciated.15 In contrast, practitioners used dual and chemically cured resin composites infrequently, preferring light-cured resin composites for direct core build up of vital teeth. The use of light-cured resin composite is potentially problematic when cores are placed in deep preparations.16 The difficulties relate to access to the increments of material in the deeper parts of the preparation, often essential for retention if boxes, slots, groves or undercuts in endodontic access cavities are being used to retain the core. It is possible that limited access for light curing could result in inadequate curing of the deeper aspects of the core leading to failure of the core. Whilst chemically cured resin composites are not ideal for core build up of anterior teeth because of poor long-term colour stability, they are very useful for the core build up of posterior teeth as it is likely there will be a higher degree of conversion (cure) in the deepest aspects of the preparation. Further research is needed to establish why male dentists were more unlikely to use amalgam as a core material than their female colleagues.
Dentine pins were widely used by the practitioners in this study for the retention of large restorations and core build up techniques. NHS regulations for general dental service may encourage such extensive use of pins. The respondents in this study used a variety of pin systems. This is somewhat surprising given that the considerable evidence that pins have been shown to weaken teeth, the core and/or restoration and the overall integrity of the restored unit, let alone the potential for perforation into the periodontal membrane or pulp chamber if incorrectly placed.17 Circumferential grooves, boxes and slots or bonding as an alternative have been shown to be preferable for retaining large complex or compound restorations without the disadvantage of weakening the restored unit.18 Given that a dentine pin was to be used, it was interesting that younger and older practitioners preferred different types of materials. Further research is needed to establish why this might be.
Cast precious posts were the most widely used form of post in this study; with non-precious alloys used as an alternative. It would seem that practitioners still use posts widely, possibly in the mistaken belief that they strengthen teeth.24 Again, it is possible that NHS regulations for general dental services may encourage this practice. Further studies of the type reported could attempt to determine differences in the use of materials/techniques between NHS and private practice. It is now understood that posts inherently weaken teeth, especially anterior teeth, and should only be used if there is insufficient dentine to support an extra coronal restoration.19 If a post and core is clinically indicated, direct placement of a prefabricated post and direct core build-up is to be preferred. However, the practitioners in this study infrequently used this technique. This is surprising given that direct posts and cores save the patient a visit and at the same time appear to have a reduced risk of fracture when directly placed prefabricated posts are used with direct resin composite core materials.20 More recently introduced fibre posts show promising results, but the incidence of use was not included in the questionnaire for this study.21 Older practitioners preferred titanium posts possibly because they had realised optimal long-term results with posts made of this material.
It is accepted that addition cured polyvinylsiloxane along with polyether are the most accurate impression materials, giving predictable results in the hands of the majority of practitioners.22 It was reassuring that the majority of the practitioners in this study routinely used an addition cured silicone impression material yet somewhat surprising that relatively few practitioners used polyether materials routinely. Polyether impression materials are very rigid and usually recommended for implant cases. They are somewhat difficult to disinfect, which probably explains the small use recorded in the study.23 Condensation cured polyvinylsiloxane impression materials are not as accurate as addition cured silicones and polyethers, yet 20% of the practitioners used this group of materials on a regular basis. It would appear that the limitations, principally inaccuracy, of this group of impression materials have been appreciated by the majority of practitioners in this study, with reduced use of these materials being recorded. Polysulphide impression materials have very poor accuracy and a very long setting time and have been replaced by more accurate materials, namely, addition cured silicone impression materials, consequently it is surprising that 12 practitioners continued to use them.
Precious bonding alloys are thought to have improved marginal adaptation, which enhances longevity when compared with non-precious alloys. This possibly explains why precious bonding alloys were used by an overwhelming majority of the practitioners in this study.
Luting cements based on traditional glass-ionomer cements are recommended for cementing cast restorations and indirect posts. These cements have a low film thickness and a proven longevity as luting materials, which explains their almost universal use for the cementation of cast restorations, which seems to have been appreciated by the younger practitioners in the survey. It is interesting to note that a large number of practitioners in this study were using these cements to cement resin composite and ceramic restorations, with little evidence of resin composite based luting cements being used. Despite this, older and female practitioners were more likely to use resin based luting cements. Further research is needed to establish why there is so much uncertainty about the absolute indications for resin based luting cements. This thinking is at odds with guidelines for the luting of ceramic, metal and resin composite restorations, which accrue many benefits from being luted into place with a resin composite luting cement. These benefits include specifically increased retention, improved strength and, very importantly, reduced marginal leakage. Increasingly, resin modified glass-ionomer cements are being recommended for luting, but these materials were not widely used by the practitioners in this study. This, coupled with many practitioners having been found to use polycarboxylate and zinc phosphate luting cements suggests that the practitioners in this study were unaware of the benefits of resin based luting systems based on either glass-ionomer or resin composite, let alone the limitations of using zinc phosphate cement for the cementation of all-ceramic restorations. Further research is needed to determine why practitioners are not using resin based luting cements more extensively.
Laminate veneers are minimally interventive and, aside from tooth whitening in suitably selected cases, were the preferred approach for restoring the appearance of sound but discoloured anterior teeth by the practitioners in this study. It is interesting that laminate veneers were preferred by younger practitioners. The reluctance of older practitioners to use laminate veneers is probably explained by poor results being realised with earlier systems, let alone the fact that veneer techniques are now taught in UK dental schools. Despite growth in the use of resin bonded and all ceramic crowns, which have been shown to be both durable and aesthetic restorations, the practitioners in this study had an almost equal preference for porcelain fused to metal and all ceramic crowns as alternative treatments for the restoration of anterior teeth. This suggests that traditional full coverage techniques are still preferred to veneer procedures by some practitioners. Porcelain fused to metal crowns require a deeper preparation, which can have adverse consequences on the pulpal-dentinal complex, leading to a loss of vitality in around 19% of crowned teeth.24 Whilst the preservative potential of less interventive techniques such as resin-bonded crowns is accepted there will be cases where porcelain fused to metal crowns are still required. It is not clear whether the practitioners in this study would have used a porcelain fused to metal crown where an all-ceramic crown could have been used. Further research is needed to investigate trends and influential factors in crown selection.
CAD/CAM systems are expensive and currently in the UK, practitioners seem to prefer to use a laboratory to produce their restorations despite the high success rates being reported.25 The results of this study support this, with only 1% of restorations produced with the aid of CAD/CAM.
A significant proportion of practitioners (19%) in this study, especially female practitioners, were unsure as to when to use ceramic or resin composite for tooth-coloured inlays and onlays, with only 9% of the practitioners having used either ceramic or resin composite as the material of choice for such restorations. This is an area that is poorly understood, which almost certainly explains practitioner uncertainty as to which material is indicated for a given clinical situation. Given the more favourable loading characteristics of single unit, indirect resin composite restorations coupled with the reparability of these restorations, further research is needed to establish clear clinical guidelines for material selection for inlay/onlay procedures. It may well be that older practitioners prefer resin composite having had poor results with ceramic restorations. Further research is needed to establish whether this is the case.
Practice location and number of practitioners in the practice made no difference to the materials and techniques used for indirect restorations or fixed prosthodontics. This is interesting, given that younger practitioners, single-handed practitioners and practitioners more distant from centres for postgraduate education are often considered to have a different practising profile. This proved not to be the case for the practitioners in this study. Equally, practitioners in the North West of England and Scotland showed no difference, with few exceptions, in their preference for materials and techniques. In some areas this study has shown practitioners' thinking to be out of step with current recommendations. It would appear therefore that there is a need for educational initiatives aimed at addressing this shortfall.
Conclusions
Within the limitations of the study, the following conclusions can be drawn:
-
Amalgam was the preferred material for core build-ups in posterior teeth
-
Dentine pins were used routinely
-
Indirect posts were preferred to direct posts
-
Addition-cured silicone was the most widely used impression material
-
Traditional glass-ionomer cements were the most popular luting cements
-
CAD/CAM restorations are not widely prescribed
-
Practitioners in the North West of England and Scotland used and selected similar materials and techniques for indirect restorations and fixed prosthodontics.
References
Annual Digests of Statistics (2000-2002). Eastbourne: Dental Practice Board.
Adult Dental Health Survey (1998). London: Office for National Statistics, HMSO, 2000.
Richards D, Lawrence A, Sackett DL . Bringing an evidence base to dentistry. Comm Dent Hlth 1997; 14: 63– 65.
Brunton PA, Wilson NHF . Preparations for porcelain laminate veneers in general dental practice. Br Dent J 1998; 184: 553– 556.
Winstanley RB, Carrotte PV, Johnson A . The quality of impressions for crowns and bridges received at commercial dental laboratories. Br Dent J 1997; 183: 209– 213.
Carrotte PV, Winstanley RB, Green JR . A study of the quality of impressions for anterior crowns received at a commercial laboratory. Br Dent J 1993; 174: 235– 240.
Johnson A, Winstanley RB, Northeast SE, Van Noort R, White GE . Variations in bridge construction in commercial laboratories. Rest Dent 1991; 65: 74– 77.
Seymour KG, Samarawickrama, DY, Zou L, Lynch E . Assessing the quality of shoulder preparations for metal ceramic crowns. Eur J Prosthodont Rest Dent 1999; 7: 125– 129.
Burke FJT, Wilson NHF, Wastell DG, Cheung SW . Glove use in clinical practice: A survey of 2000 dentists in England and Wales. Br Dent. J 1991; 171: 128– 132.
SPSS. SPSS Inc, 233 S. Wacker Drive, 11th floor, Illinois, Chicago, 60606.
Burke FJT, Wilson NHF, Christensen GJ, Cheung SW, Brunton PA . Contemporary dental practice in the UK: demographic data and practicing arrangements. Br Dent J 2004; 198: 39– 43.
Scurria MS, Shugars DA, Hayden WJ, Felton DA . General dentists' patterns of restoring endodontically treated teeth. J Am Dent Assoc 1995; 126: 775– 779.
Piwowarczyk A, Ottl P, Lauer HC, Buchler A . Laboratory strength of glass ionomer cement, compomers and resin composites. J Prosthodont 2002; 11: 86– 91.
Wilson NHF, Cowan AJ, Crisp RJ, Wilson MA . A short-term clinical evaluation of a tricure glass-ionomer system as a transitional restoration and core buildup material. Quintessence Int 1999; 30: 405– 411.
Brunton PA, Hickel R, Wilson NHF . Direct restorative material use of selected practitioners in the UK. Primary Dent Care 2002; 9: 133– 137.
Hansen EK, Asmussen E . Visible light curing units: correlation between depth of cure and distance between exit window and resin surface. Acta Odontol Scand 1997; 55: 162– 166.
Papa J, Wilson PR, Tyas MJ . Pins for direct restorations. J Dent 1993; 21: 259– 264.
Outhwaite WC, Gorman TA, Pashley DH . Pin vs. slot retention in extensive amalgam restorations. J Prosthet Dent 1979; 41: 396– 400.
Guzy GE, Nicholls JL . In vitro comparison of intact endodontically treated teeth with and without endo-post reinforcement. J Prosthet Dent 1979; 42: 39– 44.
Blignaut JB, Grobler SR . The resistance to deformation forces of endodontic posts manufactured from six different materials. J Dent Assoc S Afr 1995; 50: 363– 366.
Mannocci F, Bertelli E, Sherriff M, Watson TF, Ford TP . Three year clinical comparison of survival of endodontically treated teeth restored with either full cast coverage or with direct composite restoration. J Prosthet Dent 2002; 88: 297– 301.
Chee WW, Donovan TE . Polyvinylsiloxane impression materials: a review of properties and techniques. J Prosthet Dent 1992; 68: 728– 732.
Johnson GH, Drennon DG, Powell GL . Accuracy of elastomeric impressions disinfected by immersion. J Am Dent Assoc 1988; 116: 525– 530.
Saunders WP, Saunders EM . Prevalence of periradicular periodontitis associated with crowned teeth in an adult Scottish subpopulation. Br Dent J 1998; 185: 137– 140.
Martin N, Jedynakiewicz NM . Clinical performance of CEREC ceramic inlays: a systematic review. Dent Mater 1999; 15: 54– 61.
Acknowledgements
The authors would like to acknowledge the support of this research by the NHS R&D Levy and to thank the practitioners for participating.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Brunton, P., Christensen, G., Cheung, S. et al. Contemporary dental practice in the UK: indirect restorations and fixed prosthodontics. Br Dent J 198, 99–103 (2005). https://doi.org/10.1038/sj.bdj.4811980
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4811980
This article is cited by
-
Dental practice in the UK in 2015/2016. Part 2: aspects of direct restorations, bleaching, endodontics and paediatric dentistry
British Dental Journal (2019)
-
Dental practice in the UK in 2015/2016. Part 3: aspects of indirect restorations and fixed prosthodontics
British Dental Journal (2019)
-
Dental practice in the UK in 2015/2016. Part 4: changes since 2002?
British Dental Journal (2019)
-
A survey to compare the use and rationale for selection of intra-radicular posts among dental practitioners
British Dental Journal (2016)
-
Why, when, and how general practitioners restore endodontically treated teeth: a representative survey in Germany
Clinical Oral Investigations (2016)