Key Points
-
Reviews the results of the literature review commissioned by the GDC in 2012 to establish the potential risks and benefits of direct access.
-
Highlights there was no evidence of significant issues of patient safety resulting from direct access.
-
Stresses strong evidence shows direct access improved access to dental care, provided cost benefits to patients and increased patient satisfaction.
Abstract
The decision by the General Dental Council (GDC) in March 2013 to remove the requirement for a patient to first see a dentist before any treatment by a dental care professional, has been seen by some as controversial. The GDC has stated patient safety is the utmost priority and a literature review on direct access in dental and other healthcare fields was commissioned by the GDC in April 2012. The review considered whether any expansion of direct access would involve increased risk to patients, either by treatment or through failure to recognise and refer problems outside DCPs' clinical remit. This paper is an edited version of the results of that literature review.
Similar content being viewed by others
Introduction
On 28 March the General Dental Council (GDC) removed the requirement for a patient to first see a dentist before any treatment by a dental care professional (DCP). The decision was described as 'controversial' in the April 2013 edition of the BDJ, with support coming from The British Society of Dental Hygiene and Therapy, The British Association of Dental Nurses and The Office of Fair Trading, countered by strong reservations from the British Dental Association, which called the GDC's decision 'misguided'.1 The new arrangements came into force on 1 May 2013.
The GDC stressed that the decision was made with patient safety as the utmost priority, and that it followed a detailed review of evidence. An important component of this body of evidence came from a literature review on direct access in dental and other health fields commissioned by the GDC in April 2012. The review was intended to inform the GDC about any expansion of direct access evidence that may involve increased risk to patients, either by treatment or through failure to recognise and refer problems outside DCPs' clinical remit. This paper is an edited version of the results of that literature review, presented to the GDC in July 2012. The full Report may be found at http://www.gdc-uk.org/newsandpublications/research/pages/research.aspx
Background
Direct access has been legal for some years in a number of countries, US states and Canadian provinces, both for dental hygienists and, perhaps more controversially, for dental therapists, who are trained to perform a considerable range of restorative treatment otherwise undertaken by dentists. This summary focuses on three areas examined by the review:
-
1
Evidence about the impact of direct access in jurisdictions where it operates, including risks and benefits to patients/clients and any other impacts for example, on attendance, patient/client attitude or the attitudes of other affected healthcare professionals
-
2
Challenges that the introduction of direct access has presented in those countries and services, how relevant these are to dental services in the UK and any evidence of these challenges being managed and risks mitigated
-
3
Completeness, robustness and credibility of the available evidence.
Methods
The literature review involved searching for studies evaluating or describing direct access arrangements or issues pertinent to such arrangements in both dental and other healthcare fields. Extensive enquiries were made to dental organisations worldwide. However, it should be noted that as the GDC commission was for a rapid evidence review, selection and grading of the relevant literature was not exhaustive. This is particularly true with regard to grey literature and to papers with restricted access. Searches were restricted to post-1993, the year of the Nuffield Report.2
We searched eight online sources of published literature (Medline, CinAHL, PsycINFO, SCI, SSCI, Cochrane Database of Systematic Reviews, Business Source Premier, Google scholar), representing a wide range of disciplines and journal types using a systematic search strategy. The team also made efforts to contact:
-
Educational institutions running dental hygiene/therapy and dental nurse training to identify aspects relevant to any extension of direct access to these practitioners
-
DCP professional associations in the UK and in countries where direct access has been instigated. For example, each US state has different arrangements regarding direct access to dental hygienists
-
Relevant bodies in other professions where direct access has been established, for example regarding nurse practitioners in the UK.
The reference lists of studies included in the review were scrutinised for any pertinent studies. Publications were checked independently by two team members, and a decision made as to their inclusion in the final review using criteria outlined in Table 1.
The initial screening stage resulted in a shortlist of articles including titles and abstracts. In the second stage, eligibility assessment was performed independently by two reviewers, with any disagreements being resolved by consultation with the third reviewer. The third stage involved retrieval of the eligible articles in full text. Final selection of the studies to be included in the review was further assessed and discussed within the team until consensus was reached. One reviewer extracted data from the included studies and a second checked the extracted data. Disagreements were resolved by discussion with the third reviewer.
Methodological quality was measured by reference to checklists developed by the Critical Appraisal Skills Programme (CASP)3 and the Scottish Intercollegiate Guidelines Network (SIGN).4 The use of such tools ensures the extraction of pertinent data to allow an appraisal of the overall methodological quality of individual quantitative studies as very poor, poor, moderate or good. In addition, the level of evidence was noted: ie Level I: systematic review (or meta-analysis) of all relevant randomised controlled trials; Level II: randomised controlled trial; Level III: (1) pseudo-randomised controlled trials (alternate allocation or some other method); (2) comparative but non-randomised studies; cohort studies; case control studies; interrupted time series with a control group; (3) comparative studies with historical control, two or more single-arm studies or interrupted time series without a parallel control group; Level IV: case series, either post-test or pre-test/post-test, non-comparative studies.
Qualitative studies set out to answer different types of questions, and it was therefore not appropriate to grade them alongside quantitative studies. We performed a global assessment of study quality, that is, strong, moderate or weak. Strong studies are likely to include triangulation of data, respondent validation, evidence of data saturation, clear exposition of methods of data collection and analysis, and reflexivity.
Results
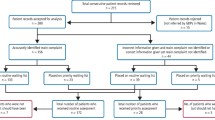
Figure 1 shows the process of evidence identification and appraisal for the dental papers. One hundred and thirty-nine full text papers were retrieved and accessed for relevance. Of those, 35 were judged to have empirical evidence of sufficient relevance and quality for inclusion. These papers were then evaluated for quality using the appropriate CASP/SIGN checklists and the levels of evidence typology. The level of evidence ranged from Level III-2 to Level IV.
Figure 2 shows the results of the second search to identify non-dental health related papers.
Impacts, including risks and benefits
Evidence on the impact of direct patient access to GDPs comes predominantly from papers relating to the role of dental hygienists and dental therapists in the US. Nineteen studies from the US were reviewed, including six dealing with dental health aide therapists (DHATs) in the state of Alaska. Of the non-US papers, four relate to the UK, four to Australia, two to Norway, and one each to New Zealand, Sweden, Spain, Italy and Canada. Of the 35 papers, 23 deal with dental hygienists, 7 with dental therapists, 1 with dental assistants, 1 with denturists, and 3 with both hygienists and therapists. However, some papers did not examine direct access arrangements as such, but rather compared knowledge, clinical decision-making, costs etc pertaining to DCPs and dentists. As such they provide relevant information on the appropriateness of different professional groups assuming greater autonomy in their clinical activity.
Eight factors emerged from the review of dental studies as the potential major impacts, including risks and benefits, of introducing direct access.
Potential negative impacts
Risks to patient safety
In seven studies that examined aspects of patient safety,5,6,7,8,9,10,11 none provided any evidence of increased risk. Quality of evidence: moderate/good in five of seven studies.
However, two of these mentioned evidence of deficiencies in facilities and equipment, one in respect to radiographs,6 and another to sterilisation and equipment.8 Both these studies refer to the Alaska DHATs, who work in remote and under-served tribal localities. Quality of evidence: moderate/good in two of two studies.
Two descriptive Scottish papers do not present data directly pertaining to safety issues and extended duties dental nurses (EDDNs) acting under direct access arrangements.12,13 However, no significant adverse events have been recorded in this programme in over 168,000 fluoride varnish applications (personal communication, Childsmile Central Evaluation and Research Team, Glasgow Dental School, June 2012).
Risks relating to diagnosis and referral decision-making
Eleven studies were found that looked at the quality of DCPs' referral decision-making. Four found evidence of poor specificity (that is, referring a high proportion of problematic cases but also a significant number of non-problematic cases), leading to over-referral and unnecessary consultations.10,14,16 While one study noted good agreement between DCP and dentist regarding DCP referral decisions,17 others reported under-referral18 or problems in getting dentists to accept referrals.19 One US study reported good uptake of referrals by adult patients,20 but another reported a low uptake of referrals from a school dental service.15
Two European studies found knowledge and training deficiencies regarding oral cancer detection among dental hygienists,21,22 while a UK sample survey reported a lack of confidence among hygienists and therapists in their own ability to detect possible oral cancer.23 None of these three studies compared DCPs' knowledge with that of dentists. Quality of evidence: moderate/good in 10 of 11 studies.
Support to patients
Seven studies looked at aspects of DCPs' knowledge or support to patients regarding smoking cessation,21,22,24,25, diabetes26, child abuse27 and domestic violence.28 All but one24 found deficiencies in DCPs' knowledge or support to patients, but there is no evidence from these studies to suggest that dentists were any better in these respects. Quality of evidence: moderate/good in five of seven studies.
Concerns and lack of knowledge of professional and patients regarding direct access.
Both dentists and patients in several studies have shown mixed views about DCPs providing treatment. These findings contradict the conclusions of studies involving patients of DCPs (see 'patient satisfaction' below). Studies conclude that the introduction of direct access will require education and the preparation of information for health professionals, patients and parents.23,29,32 Quality of evidence: moderate in five of five studies.
Potential positive impacts
Increased access to dental care, both preventive and restorative
Ten studies provide evidence that the deployment of dental therapists and dental hygienists (and in one study, dental assistants) in indirect or general supervision or unsupported by a dentist resulted in greater access to and use of dental services by under-served groups and communities.6,8,15,19,20,33,37 Quality of evidence: moderate/good in seven of ten studies.
There is a limited amount of evidence regarding the work of dental nurses or dental assistants. One study examined the impact on access of a new type of dental assistant ('scaling assistants') in Maine, US,37 and concluded that workforce data suggested an increase in access to dental care. In the UK, EDDNs may effectively act under direct access in limited settings of day nursery and primary schools, in that they provide preventive care, including fluoride varnish treatment, with only general supervision from a dentist. Routinely collected monitoring data from the Scottish Childsmile programme12,13 indicate that in addition to any gain in the protection of children's teeth, access to restorative care is likely to have been increased. In over 108,000 appointments for fluoride varnish application completed in 2011, 22% resulted in parents being recommended to take their child for care from a dental practice, usually because untreated caries had been detected by the EDDNs (Personal communication, Childsmile Central Evaluation and Research Team, Glasgow Dental School, June 2012).
Cost savings to patients and the public purse
Three studies10,38,39 suggest variable and at most modest benefits regarding cost savings to the patients and service providers. Quality of evidence: moderate/good in two of three studies. The evidence for savings in dentists' time or other resources is inconclusive.20,37,38 Quality of evidence: moderate in one of three studies.
Patient satisfaction
Six studies gave consistent findings that patient satisfaction was high and/or dental anxiety low among dental hygienist and dental therapist patients.15,33,35,36,40,41 Two report higher satisfaction among patients of independent dental hygienist practices than among dentists' patients.33,41 Quality of evidence: moderate/good in four of six studies.
Higher job satisfaction among dental therapists and hygienists
One US and one UK study found that job satisfaction was higher when DCPs worked to their full remit and training.19,23 Quality of evidence: moderate in two of two studies.
Challenges/mitigation of risk
Potential barriers to direct access identified through the direct access literature search relate to practitioner and patient attitudes towards an extended DCP role. Attitudes among both dentists and patients tended to be more positive with direct experience of working with or being treated by DCPs, and DCPs themselves were confident in their abilities to work more independently.23,30,32,42 Five approaches to the mitigation of risk were identified:
Limitations of clinical remit, patient groups or settings.
Commonly limitations of the DCPs' clinical remit relate to restorative treatments, particularly those classed as 'irreversible.' There are examples of such limitations being widened over time or varying according to levels of experience, training or supervision. In some models patient groups have been limited to children, the elderly, the under-served (defined by the spatial distribution of dentists and their patient base), those on welfare benefit (for example, Medicaid, Medicare). Specified settings are commonly public service clinics or walk-in centres (as opposed to private practice), schools, care homes or other residential settings. There was no found evidence demonstrating the value of restriction by patient group or setting.
Stipulated levels of experience, qualification or training
Some models of direct access have stipulated levels of experience, qualification or training required by DCPs working independently or under general supervision. Again no evaluation material has been found which tests or compares restrictions of this kind.
Formal supervision
Formal supervision by dentists is a common, but not universal, method of regulating DCPs working directly with patients. These arrangements may involve a 'named dentist', as in the Alaska DHAT model. This dentist monitors activity, provides advice by telephone or audio-visual link, and accepts referrals.
Audit and inspection
Audit and inspection arrangements may exist outside supervision by a dentist. For example, the Alaska DHAT model maintains close audit returns of local performance.
Line management
DCPs may have a line management structure such as exists within the Childsmile oral health improvement programme in Scotland with its use of EDDNs working in schools and nursery schools, answerable to a programme coordinator and ultimately the Director of Dental Public Health within each Health Board.
These approaches to regulation and patient safety are by no means mutually exclusive, or limited to arrangements for direct access to dental care. For example, in the early 1990s the following limitations on practice in physical therapy (physiotherapy) direct-access models applied in different US states: diagnosis requirements, eventual referral requirements, physical therapist qualifications, patient consent requirements and practice setting restrictions.43
There is little evidence to evaluate or compare these approaches. However, a 2005 study found no reported disciplinary actions against dental hygienists in respect to the administration of anaesthesia across 13 US states over a ten year period.11
Gaps in the evidence
-
1
Despite the fact that New Zealand is generally recognised as pioneering direct access to dental care provided by DCPs, particularly therapists and nurses, only one paper34 was identified that evaluated in that country. However, a 2012 review of the global literature on dental therapists includes a 58-page account of the development, organisation and performance of the New Zealand dental therapist profession44
-
2
Evaluations of long-term outcomes of dental therapists' restorations were not found6
-
3
Very little research evidence pertaining to dental nurses, dental technicians, and clinical dental technicians was found
-
4
The research literature is dominated by papers from the US, a reflection both of recent developments in Alaska and elsewhere in response to poor access to dental care on the part of many Americans, and the controversy regarding safety and efficacy of independent 'mid-level' practitioners
-
5
Only three research studies made reference to the referral pathway from DCP to dentist.15,19,20 There is a need for more detailed evidence on the extent to which patients and families fail to follow up referral to a dentist once they or their child has received treatment from a DCP, and the extent to which any such failure of referral is associated with treatment need
-
6
There was insufficient relevant and good quality evidence to be able to evaluate different models of direct access with, for example, different levels of supervision. However, anecdotal evidence45 that US dental hygiene malpractice insurance premiums are the same regardless of the level of supervision the hygienist practices under, or the range of clinical services she performs, supports Scofield and colleagues11 in their conclusion that dental hygienists successfully and safely administer local anaesthetics to dental patients under varying supervision arrangements
-
7
No research evidence on the operation of shared record keeping was found, although one study describes arrangements in the Alaska DHAT service.10
Direct access in other areas of regulated healthcare
As Figure 2 shows, the literature search identified seven areas of healthcare where some form of direct access has been reported. Three of these, and 40 of the 66 identified papers, relate to nurses working under direct access arrangements. This often involved primary care settings – probably the most useful comparison for dental services. A Cochrane systematic review46 on the substitution of doctors by nurses in primary care, although not explicitly defined as direct access, is also relevant to this review.
As patient safety was the prime concern of the GDC in commissioning the review, we restricted our summarising of this evidence base to issues of patient safety, including treatment and referral quality, in three areas felt to be most relevant to primary care-based dental services: direct access to nurses in primary care, including telephone triage schemes; physiotherapy; and audiology.
Overall the evidence from the eight nursing studies is favourable, in that six found no evidence that patient safety had been compromised by use of nurses or nurse practitioners.47,48,49,50,51,52 The systematic review by Laurante46 also reports no impact on health outcomes, but cautions about study quality. Moll van Charante et al. found considerable variation among nurses making telephone-based assessments and referral decisions.53
The evidence from physiotherapy studies on patient safety or referral quality is more mixed, with eight studies concluding that direct access does not pose a risk to public safety,54,55,56,57,58,59,60,61 three with equivocal findings,62,63,64 and three with at least partially negative findings.65,66,67 The main recommendation from this latter group was the need for relevant training to improve assessment and referral skills. The findings from the two audiology studies were very positive about patient safety and direct access to such services.68,69
Finally, we note the 2006 systematic review of evidence on extended roles for allied health professionals.70 While 21 studies progressed to full review and data extraction, the authors were unable to evaluate any pooled effects as patient health outcomes were rarely considered. They conclude that health outcomes, how best to introduce such roles, or how best to educate, support and mentor these practitioners, had rarely been evaluated (systematic review, evidence level I; study quality: good).
Conclusions
Over 100 research dental and other health-related papers were identified as relevant for this review of direct access. The quality of the evidence regarding direct access issues in dental care practitioners was varied but of moderately good quality as a whole. The material on direct access in dental services was overwhelmingly related to the work of dental hygienists and dental therapists, and mostly US in origin.
There was no evidence of significant issues of patient safety resulting from the clinical activity of DCPs. In contrast, there was strong evidence that access to dental care improved as a result of direct access arrangements, of cost benefits to patients, and of high levels of patient satisfaction. Of course, if access to dental care is widened, and appropriate referrals of patients with hitherto unmet treatment needs are made by DCPs to dentists, demands on dentists' services may rise. There was some evidence that DCPs may over-refer patients to dentists, which may ensure patient safety but lead to wasteful use of resources and a high level of 'no shows' on referral.
Finally, there is evidence of ongoing training needs to strengthen the assessment and referral skills of DCPs in respect to patients with other health problems or risk factors, but little evidence that dentist are any less in need of such training.
References
GDC announces controversial decision on direct access. Br Dent J 2013; 214: 379.
Smith N J . Education and training of personnel auxiliary to dentistry. A submission to the Nuffield Foundation. Br Dent J 1993; 175: 193–195.
Critical Appraisal Skills Programme (CASP). Find, appraise, act. Online information available at http://www.casp-uk.net/find-appraise-act/ (accessed November 2013).
Scottish Intercollegiate Guidelines Network (SIGN). Methodology checklists. Online checklists available at www.sign.ac.uk/methodology/checklists.html (accessed November 2013).
Battrell A M, Gadbury-Amyot C C, Overman P R . A qualitative study of limited access permit dental hygienists in Oregon. J Dent Educ 2008; 72: 329–343.
Bolin K A . Assessment of treatment provided by dental health aide therapists in Alaska: a pilot study. J Am Dent Assoc 2008; 139: 1530–1535.
Bader J D, Lee J Y, Shugars D A, Burrus B B, Wetterhall S . Clinical technical performance of dental therapists in Alaska. J Am Dent Assoc 2011; 142: 322–326.
Wetterhall S, Bader J D, Burrus B B, Lee J Y, Shugars D A . Evaluation of the dental health aide therapist workforce model in Alaska. RTI Project Number 0211727.000.001. W K Kellogg Foundation, 2010.
Williard M E, Fauteux N . Dentists provide effective supervision of Alaska's dental health aide therapists in a variety of settings. J Public Health Dent 2011; 71 (Suppl 2): S27–33.
Wang N J . Variation in clinical time spent by dentist and dental hygienist in child dental care. Acta Odontol Scand 1994; 52: 280–289.
Scofield J C, Gutmann M E, DeWald J P, Campbell P R . Disciplinary actions associated with the administration of local anaesthetics against dentists and dental hygienists. J Dental Hyg 2005; 79: 8.
Macpherson L M, Ball G E, Brewster L et al. Childsmile: the national child oral health improvement programme in Scotland. Part 1: establishment and development. Br Dent J 2010; 209: 73–78.
Turner S, Brewster L, Kidd J et al. Childsmile: the national child oral health improvement programme in Scotland. Part 2: monitoring and delivery. Br Dent J 2010; 209: 79–83.
Kwan S Y, Prendergast M J . The use of clinical dental auxiliaries as examiners in caries prevalence surveys in the United Kingdom: a feasibility study. Community Dent Oral Epidemiol 1998; 26: 194–200.
Simmer-Beck M, Gadbury-Amyot C C, Ferris H et al. Extending oral health care services to underserved children through a school-based collaboration: part 1: a descriptive overview. J Dent Hyg 2011; 85: 181–192.
Brocklehurst P, Ashley J, Walsh T, Tickle M . Relative performance of different dental professional groups in screening for occlusal caries. Community Dent Oral Epidemiol 2012; 40: 239–246.
Hopcraft M S, Morgan M V, Satur J G, Wright F A . Utilizing dental hygienists to undertake dental examination and referral in residential aged care facilities. Community Dent Oral Epidemiol 2011; 39: 378–384.
Hawley G M, Wainwright-Stringer Y, Craven R, Blinkhorn A S . An investigation into the use of a dental hygienist in school screening. Community Dent Health 1999; 16: 232–235.
Mertz E, Glassman P Alternative practice dental hygiene in California: past, present, and future. J Calif Dent Assoc 2011 January; 39: 37–46.
Perry D A, Freed J R, Kushman J E . Characteristics of patients seeking care from independent dental hygienist practices. J Public Health Dent 1997; 57: 76–81.
López-Jornet P, Camacho-Alonso F, Molina Minano F . Knowledge and attitude towards risk factors in oral cancer held by dental hygienists in the Autonomous Community of Murcia (Spain): a pilot study. Oral Oncol 2007; 43: 602–606.
Nicotera G, Gnisci F, Bianco A, Angelillo I F . Dental hygienists and oral cancer prevention: knowledge, attitudes and behaviours in Italy. Oral Oncol 2004; 40: 638–644.
Turner S, Ross M, Ibbetson R . Dental hygienists and therapists: how much professional autonomy do they have? How much do they want? Results from a UK survey. Br Dent J 2011; 210: E16.
Brothwell D J, Gelskey S C . Tobacco use cessation services provided by dentists and dental hygienists in Manitoba: part 1. Influence of practitioner demographics and psychosocial factors. J Can Dent Assoc 2008; 74: 905.
Chambers A K, Corbin D E . Tobacco control activities of Iowa dental hygienists. J Community Health 1996; 21: 375–387.
Boyd L D, Hartman-Cunningham M L. Survey of diabetes knowledge and practices of dental hygienists. J Dent Hyg 2008; 82: 43.
Chadwick B L, Davies J, Bhatia S K, Rooney C, McCusker N . Child protection: training and experiences of dental therapists. Br Dent J 2009; 207: E6.
Mascarenhas A K, Deshmukh A, Scott T . New England, USA dental professionals' attitudes and behaviours regarding domestic violence. Br Dent J 2009; 206: E5.
Hopcraft M, McNally C, Ng C et al. Attitudes of the Victorian oral health workforce to the employment and scope of practice of dental hygienists. Aust Dent J 2008; 53: 67–73.
Abelsen B, Olsen J A . Task division between dentists and dental hygienists in Norway. Community Dent Oral Epidemiol 2008; 36: 558–566.
Dyer T A, Robinson P G . Exploring the social acceptability of skill-mix in dentistry. Int Dent J 2008; 58: 173–180.
Dyer T A, Robinson P G . Public awareness and social acceptability of dental therapists. Int J Dent Hyg 2009; 7: 108–114.
Freed J R, Perry D A, Kushman J E . Aspects of quality of dental hygiene care in supervised and unsupervised practices. J Public Health Dent 1997; 57: 68–75.
Squillace J . Study of a rural practice dental hygienist in a public health setting: analysis of an administrative dataset. J Health Care Poor and Underserved 2012; 23: 739–751.
Wetterhall S, Burrus B, Shugars D, Bader J . Cultural context in the effort to improve oral health among Alaska Native people: the dental health aide therapist model. Am J Public Health 2011; 101: 1836–1840.
Calache H, Shaw J, Groves V et al. The capacity of dental therapists to provide direct restorative care to adults. Aust N Z J Public Health 2009; 33: 424–429.
Mitchell T V, Peters R, Gadbury-Amyot C C, Overman P R, Stover L . Access to care and the allied oral health care workforce in Kansas: perceptions of Kansas dental hygienists and scaling dental assistants. J Dent Educ 2006; 70: 263–278.
Bailit H, Beazoglou T, Drozdowski M . Financial feasibility of a model school-based dental programme in different states. Public Health Rep 2008; 123: 761–767.
Devlin N J . The effects of denturism: New Zealand dentists' response to competition. Am J Public Health 1994 84: 1675–1677.
Calache H, Hopcraft M S . Provision of oral health care to adult patients by dental therapists without the prescription of a dentist. J Public Health Dent 2011; 72: 19–27.
Hakeberg M, Cunha L . Dental anxiety and pain related to dental hygienist treatment. Acta Odontol Scand 2008; 66: 374–379.
Hopcraft M, McNally C, Ng C et al. Attitudes of the Victorian oral health workforce to the employment and scope of practice of dental hygienists. Aust Dent J 2008; 53: 67–73.
Taylor T K, Domholdt E . Legislative change to permit direct access to physical therapy services: a study of process and content issues. Phys Ther 1991; 71: 362–389.
Nash D A, Friedman J W, Mathu-Muju K R et al. A review of the global literature on dental therapists. W K. Kellogg Foundation, 2012. Online review available at http://www.wkkf.org/knowledge-center/resources/2012/04/nash-dental-therapist-literature-review.aspx (accessed November 2013).
American Dental Hygienist Association (personal communication, June 2012).
Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B . Substitution of doctors by nurses in primary care (review). Cochrane Database of Systematic Reviews. Art No: CD001271. The Cochrane Collaboration, John Wiley & Sons, 2009.
Gardner A, Gardner G . A trial of nurse practitioner scope of practice. J Adv Nurs 2005; 49: 135–145.
Everett C M, Schumacher J R, Wright A, Smith M A . Physician assistants and nurse practitioners as a usual source of care. J Rural health 2009; 25: 407–414.
Coulthard M G, Vernon S J, Lambert H J, Matthews J N . A nurse led education and direct access service for the management of urinary tract infections in children: prospective controlled trial. BMJ 2003; 327: 656.
Myers P C . A nurse practitioner as the first point of contact for urgent medical problems in a general practice setting. Fam Pract 1997; 14: 492–497.
Offredy M . Decision-making in primary care: outcomes from a study using patient scenarios. J Adv Nurs 2002; 40: 532–541.
Lattimer V, George S, Thompson F et al. Safety and effectiveness of nurse telephone consultation in out of hours primary care: randomised controlled trial. The South Wiltshire Out of Hours Project (SWOOP) Group. BMJ 1998; 317: 1054–1059.
Moll van Charante E P, van der Riet G, Drost S, van der Linden L, Klazinga N S, Bindels P J . Nurse telephone triage in out-of-hours GP practice: determinants of independent advice and return consultation. BMC Fam Pract 2006; 7: 74.
Ferguson A, Griffin E, Mulcahy C . Patient self-referral to physiotherapy in general practice – a model for the new NHS? Physiotherapy 1999; 85: 13–20.
MacKay C, Davis A M, Mahomed N, Badley E M . Expanding roles in orthopaedic care: a comparison of physiotherapist and orthopaedic surgeon recommendations for triage. J Eval Clin Pract 2009; 15: 178–183.
Mitchell J M, de Lissovoy G. A comparison of resource use and cost in direct access versus physician referral episodes of physical therapy. Phys Ther 1997; 77: 10–18.
Moore J H, Goss D L, Baxter R E et al. Clinical diagnostic accuracy and magnetic resonance imaging of patients referred by physical therapists, orthopaedic surgeons, and nonorthopaedic providers. J Orthop Sports Phys Ther 2005 35: 67–71.
Moore J H, McMillian D J, Rosenthal M D, Weishaar, M D. Risk determination for patients with direct access to physical therapy in military health care facilities. J Orthop Sports Phys Ther 2005; 35: 674–678.
Shoemaker M J . Direct consumer access to physical therapy in Michigan: challenges to policy adoption. Phys Ther 2012; 92: 236–250.
Daker-White G, Carr A J, Harvey I et al. A randomised controlled trial. Shifting boundaries of doctors and physiotherapists in orthopaedic outpatient departments. J Epidemiol Community Health 1999; 53: 643–650.
Childs J D, Whitman J M, Sizer P S, Puglia M L, Flynn T W, DeLitto A . A description of physical therapists' knowledge in managing musculoskeletal conditions. BMD Musculoskeletal Disorders 2005; 6: 32.
Leemrijse C J, Swinkels I C, Veenhof C . Direct access to physical therapy in the Netherlands: results from the first year in community-based physical therapy. Phys Ther 2008; 88: 936–946.
Foster N E, Williams B, Grove S, Gamlin J, Salisbury C . The evidence for and against 'PhysioDirect' telephone assessment and advice services. Physiotherapy 2011; 97: 78–82.
Hattam P . The effectiveness of orthopaedic triage by extended scope physiotherapists. Clinical Governance: an International Journal 2004; 9: 244–252.
Jette D U, Ardleigh K, Chandler K, McShea L . Decision-making ability of physical therapists: physical therapy intervention or medical referral. Phys Ther 2006; 86: 1619–1629.
Riddle D L, Hillner B E, Wells P S, Johnson R E, Hoffman H J, Zuelzer W A . Diagnosis of lower-extremity deep vein thrombosis in outpatients with musculoskeletal disorders: a national survey study of physical therapists. Phys ther 2004; 84: 717–728.
Schmid A A, Butterbaugh L, Egolf C, Richards V, Williams L . Prevention of secondary stroke in VA: Role of occupational therapists and physical therapists. J Rehabil Res Dev 2008; 45: 1019–1026.
Zapala D A, Stamper G C, Shelfer J S et al. Safety of audiology direct access for medicare patients complaining of impaired hearing. J Am Acad Audiol 2010; 21: 365–379.
Swan I R, Browning G G . A prospective evaluation of direct referral to audiology departments for hearing aids. J Laryngol Otol 1994; 108: 120–124.
McPherson K, Kersten P, George S et al. A systematic review of evidence aboutextended roles for allied health professionals. J Health Serv Res Policy 2006 11: 240–2007.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Turner, S., Tripathee, S. & MacGillivray, S. Direct access to DCPs: what are the potential risks and benefits?. Br Dent J 215, 577–582 (2013). https://doi.org/10.1038/sj.bdj.2013.1145
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2013.1145
This article is cited by
-
The perceptions and attitudes of qualified dental therapists towards a diagnostic role in the provision of paediatric dental care
British Dental Journal (2022)
-
The dental therapist's role in a 'shared care' approach to optimise clinical outcomes
British Dental Journal (2021)
-
The dental therapist's role in a 'shared care' approach to optimise clinical outcomes
BDJ Team (2021)
-
A whole-team approach to optimising general dental practice teamwork: development of the Skills Optimisation Self-Evaluation Toolkit (SOSET)
British Dental Journal (2020)
-
General dental practices with and without a dental therapist: a survey of appointment activities and patient satisfaction with their care
British Dental Journal (2018)