Abstract
Study design:
Prospective, three-way crossover design.
Objective:
Penile vibratory stimulation (PVS) is recommended as the first line of treatment for semen retrieval in anejaculatory men with spinal cord injury (SCI). This study compared ejaculatory success rates and patient preference for three methods of PVS within the same group of men with SCI.
Setting:
Major medical university.
Methods:
Fifteen men with SCI each received three methods of PVS. Method 1 (M1): applying one FertiCare Personal device to the dorsum or frenulum of the glans penis; Method 2 (M2): ‘sandwiching’ the glans penis between two FertiCare devices; Method 3 (M3): sandwiching the glans penis between the two vibrating surfaces of the Viberect-X3 device. The order of M1, M2 and M3 was varied to control for sequencing effects. Following each PVS trial, subjects rated their experience on a questionnaire with scaled responses.
Results:
Ejaculation success rates were high for each method; however, ejaculation latency was significantly longer with M3 compared with M1 or M2. In survey questions about patient preference, there were no significant differences between M1 and M2. In contrast, M3 was rated lower than M1 and M2 in patient preference. Semen collection may be more difficult with the Viberect device.
Conclusions:
On the basis of these findings, we recommend attempting PVS with one FertiCare device. If that fails, use two FertiCare devices. Although the Viberect-X3 was preferred less by patients, it had similar efficacy as the Ferticare vibrator(s) and may be suitable for home use by some patients.
Similar content being viewed by others

Introduction
There are ~282 000 persons living with spinal cord injury (SCI) in the United States. In 2016, there were 17 000 new SCI cases in the United States, with most injuries occurring between the ages of 16 and 30 years, 80% of which were males.1 Consequently, a large proportion of men with newly diagnosed SCI will be at what is considered their prime age of fertility. With no significant decline in long-term mortality in males with SCI, the focus in these men shifts to quality of life.2
After injury, many SCI patients naturally inquire about their attractiveness, relationships and ability to father children.3 Infertility is one of the most disheartening sequelae of SCI, a problem primarily caused by anejaculation and poor semen parameters (for example, low motility and low viability).4, 5, 6 Moreover, only about 9% are able to ejaculate via masturbation.7 The majority of males with SCI who wish to achieve pregnancy, therefore, require medical assistance to obtain sperm for assisted conception procedures.8, 9, 10
Nonsurgical methods to obtain semen include penile vibratory stimulation (PVS), electroejaculation (EEJ) and prostatic massage. Although both PVS and EEJ are highly effective, PVS is recommended as the first-line therapy for anejaculation in men with SCI because of its safety profile, reliability and cost-effectiveness.11, 12 PVS is performed by applying a single vibrator pad to the dorsum or frenulum of the glans penis. During stimulation, care must be taken to prevent adverse reactions such as autonomic dysreflexia and penile skin abrasion. The highest ejaculatory success rates are attained by devices capable of delivering amplitudes of 2.5 mm and 100 Hz in men whose level of injury is T10 and rostral.13 Failures can be salvaged using the ‘sandwich’ method by using two vibrators to simultaneously stimulate the dorsum and frenulum of the penis.14 The Viberect-X3 device was introduced in 2013 for the purpose of inducing ejaculation in anejaculatory men with SCI. This device has two built-in vibrating pads that can simultaneously stimulate the dorsum and frenulum of the glans penis.15
With the availability of these three methods of performing PVS, what algorithm should be recommended? There are no reports directly comparing these methods within the same group of patients. The objective of the present study was to compare ejaculatory success rates, ejaculation latency and patient preference for three methods of PVS (one Ferticare device, two Ferticare devices and the Viberect-X3) within the same group of men with SCI.
Materials and methods
Subjects
The study was approved by the Institutional Review Board, and written consent was obtained from each subject. Subjects were participants in the Male Fertility Research Program of the Miami Project to Cure Paralysis at the University of Miami Miller School of Medicine in Miami, Florida. Eligibility criteria for the current study were men with traumatic SCI of more than 1 year duration, neurological level of injury at T10 or rostral, inability to ejaculate by sexual intercourse or masturbation and no contraindications for PVS. Fifteen subjects were enrolled. Their mean age was 37.3±8.1 years, range 25–56 years. Their levels of injury are shown in Table 3.
Study design
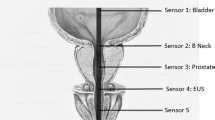
In this prospective study, each subject received the following three methods of PVS, with an interval of 2–4 weeks between each method: Method 1 (M1)—applying one FertiCare Personal (Multicept, Denmark) device to the dorsum or frenulum of the glans penis; Method 2 (M2)—‘sandwiching’ the glans penis between two FertiCare devices; Method 3 (M3)—sandwiching the glans penis between the two vibrating surfaces of the Viberect-X3 (Reflexonic, Frederick, MD, USA) device. These methods are shown in Figure 1.
To control for sequencing effects, five subjects received PVS in the following sequence: M1, M2, M3; five subjects received the sequence M2, M3, M1; and five received the sequence M3, M2, M1. For trials with M1 and M2, FertiCare device(s) were set at 2.5 mm amplitude and 100 Hz. For trials with M3, stimulation parameters of the Viberect-X3 were preset by the manufacturer and were not adjustable.
PVS and Questionnaire
All subjects had their bladder emptied prior to performing PVS. For all methods, PVS was delivered in 2 min increments with inspection of the penile skin between increments. PVS was stopped if ejaculation occurred, or if no ejaculation occurred after 10 min of PVS. Blood pressure was monitored every minute throughout each procedure. Subjects whose level of injury was T6 or rostral were pretreated with 20 mg sublingual nifedipine to manage possible autonomic dysreflexia.16, 17 Following each PVS trial, subjects were asked to rate their experience on a questionnaire with scaled responses. The measured distance from zero of a vertical mark on a 100 mm line indicated a rating between 0 and 100 (Figure 2).
The same operators performed all PVS methods, timing, administering and scoring of the questionnaire.
Statistical analysis
Repeated measures analysis of variance was used to compare differences between groups using GraphPad Prism 5.0 (GraphPad Software, Inc., La Jolla, CA, USA). Statistical significance was considered at P⩽0.05.
Results
All 15 subjects underwent the three methods of PVS. The ejaculation success rates for M1, M2 and M3 were 87, 100 and 87%, respectively (Table 1). The average ejaculation latency was significantly longer with M3 compared to M1 and M2 (56.8 s vs 29.6 and 32.2, respectively, Table 1).
Table 2 shows outcomes for post-stimulation survey Questions 1 through 4. For Question 1 (How much did this method meet your expectations?), PVS with the Viberect-X3 (M3) was rated significantly lower than PVS with one or two FertiCare devices (M1 and M2, respectively). A similar outcome was found for Question 2 (How comfortable did you feel during stimulation?) and Question 4 (Would you recommend this method to other men with spinal cord injury?). For Question 3 (How comfortable do you feel about using this method at home either by yourself or with a partner?), M3 was also rated lowest, but the mean rating for this method (67.5) was not statistically significantly different from the mean ratings for M1 (79.1) or M2 (71.5).
Table 3 shows the results of Question 5 (If you ejaculated with this method, how pleasurable was the ejaculation?) and Question 6 (Did you experience any unpleasant sensations during PVS?). Subject’s ratings on Question 5 varied between 0 and 100 for each method, with a mean±s.e.m. rating of 42.5±10.9, 45.1±8.4 and 48.7±9.5 for M1, M2 and M3, respectively (not statistically different). There was no distinct pattern in ratings of how pleasurable the ejaculation was by method of PVS. For example, four subjects gave the highest rating to M1, four subjects gave the highest rating to M2, four subjects gave the highest rating to M3, two subjects gave the highest rating to two methods, and one subject ejaculated with only one method.
Only four subjects per method reported experiencing unpleasant sensations during PVS (indicated on Table 3). The sensations most often reported were contractions (four subjects during each of methods M1, M2 and M3), tightness in chest (one subject during M2, two subjects during M3), ‘unpleasant feeling in stomach’ (one subject during M1 and M3, and headache (one subject during M3). In general, occurrence of unpleasant sensations did not seem to be related to the subjects’ rating of how pleasurable the ejaculation was, with the possible exceptions of subjects no. 4 and no. 13. For example, subject no. 4 gave ratings of 54 and 48 to M1 and M2, respectively, during which he reported no unpleasant sensations, versus a rating of zero for M3, during which he experienced unpleasant contractions and tightness in the chest. In contrast, subject no. 13 gave a rating of zero for M1 and M2, during which he experienced unpleasant contractions, versus a rating of 53 for M3 during which he experienced no unpleasant sensations.
It should be noted that the unpleasant sensations did not preclude subjects from participating in the study. No subject requested that a procedure be aborted. No subject declined to continue in the study.
Discussion
PVS is considered the method of first choice for semen retrieval in men who are anejaculatory due to spinal cord injury.11 Compared to the alternative semen retrieval method of EEJ,18 PVS results in better semen quality,19 is preferred more by patients20 and can be performed by selected couples wishing to attempt home insemination.8 Consequently, clinicians have sought to optimize the efficiency and success rate of PVS. For example, previous research found that application of two FertiCare devices salvaged 22% of failures to one FertiCare device.14, 21, 22 The introduction of the Viberect-X3 in 2013 provided another tool for inducing ejaculation in this population.15 The purpose of the present study was to compare the efficacy and success rate of the three methods of PVS applied to the same patient. Only men with a neurological level of injury at or rostral to T10 were selected for this study because injuries caudal to T10 may interfere with the ejaculatory reflex arc necessary for the success of PVS.23
The application of 2 FertiCare devices (sandwich method, M2) resulted in the best success rate (100%) compared to the other two methods (87% for both M1 and M3). The Viberect-X3 method (M3) required more time to induce ejaculation than the single FertiCare method (M1) or the sandwich method (M2). Following each PVS trial, patients were asked to answer a survey about their experience. The Viberect-X3 (M3) was the least preferred method, and the single FertiCare method (M1) was the most recommended method by the study subjects. Subjects’ reasons for preferring one method over another were variable. For example, the reasons given by subjects who preferred M1 (application of one FertiCare) included the following: ‘it is effective and you get good results,’ ‘good feeling,’ and ‘it is fast and easy.’ Reasons given by subjects who gave a lower rating for M3 (Viberect-X3) included the following: ‘it did not feel right,’ ‘not as fast and easy to use’ and ‘when my penis is squeezed with the vibrator, it is more difficult to ejaculate.’ Although M3 had the lowest mean rating for patient preference, there were individual subjects who preferred M3 to M1 or M2. For example, subject no. 13 commented that M3 was ‘very comfortable, very fast and convenient.’
Although no clear definition for autonomic dysreflexia (AD) exists, it is described as a conglomeration of symptoms including headache, skin flushing, stuffy nose, diaphoresis, generalized feelings of unwellness and uncontrolled hypertension.24, 25, 26, 27 It is generally accepted that a sudden dangerous rise in blood pressure is the major symptom of autonomic dysreflexia to be avoided. To this end, all subjects at risk for AD received 20 mg of nifedipine sublingually 10–15 min before beginning their procedure. All patients undergoing PVS during the study were monitored by a physician for signs of AD, and protocols were in place to stop the procedure if these symptoms were experienced. Most subjects experienced a rise in blood pressure with all three methods of PVS without other symptoms concerning for AD. No patients were bradycardic and heart rate did not change significantly from baseline during PVS. Those with elevated blood pressures became normotensive shortly after stimulation was stopped. However, three subjects complained of symptoms that tend to be associated with AD; subjects 4 and 15 complained of chest tightness after M3, and subject 11 complained of unpleasant abdominal sensation after M1 and M3. These symptoms were transient and briefly resolved after ejaculation without clinically significant sequelae. Chest tightness was only experienced with M3. Whether this was associated with longer latency to ejaculation remains to be clarified owing to our small sample size. No specific method had a strong correlation to AD. Notwithstanding, the risk for AD during PVS can be minimized through a protocol that includes pre-treatment with oral nifedipine, frequent blood pressure monitoring and close observation. In our experience, performing PVS with any of the three methods, is by and large, safe.
At the time of the performance of this study, the cost of the FertiCare device is ~$800 per unit versus the Viberect-X3, which is ~$300 per unit. The Viberect-X3 thus represents a lower cost option, which may be appropriate for some patients. From the standpoint of clinicians attempting to collect semen for insemination, we found semen collection to be more problematic with M3 versus M1 or M2 because of the configuration of the Viberect-X3 device, which hampered proximity of the specimen cup to the urethral meatus.
Conclusions
Our recommended algorithm is to attempt PVS with one FertiCare device. If that fails, use two FertiCare devices. Although the Viberect-X3 was preferred less by patients, it is a lower cost alternative that may be suitable for home use by some patients.
Data archiving
There were no data to deposit.
References
National SCI Statistical Center. Spinal cord injury (SCI) facts and figures at a glance. J Spinal Cord Med 2016; 39: 370–371.
Strauss DJ, Devivo MJ, Paculdo DR, Shavelle RM . Trends in life expectancy after spinal cord injury. Arch Phys Med Rehabil 2006; 87: 1079–1085.
Medicine CfSC. Sexuality and reproductive health in adults with spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med 2010; 33: 281–336.
Ibrahim E, Lynne CM, Brackett NL . Male fertility following spinal cord injury: an update. Andrology 2016; 4: 13–26.
Brown DJ, Hill ST, Baker HW . Male fertility and sexual function after spinal cord injury. Prog Brain Res 2006; 152: 427–439.
Fode M, Krogh-Jespersen S, Brackett NL, Ohl DA, Lynne CM, Sonksen J . Male sexual dysfunction and infertility associated with neurological disorders. Asian J Androl 2012; 14: 61–68.
Brackett NL, Lynne CM, Ibrahim E, Ohl DA, Sonksen J . Treatment of infertility in men with spinal cord injury. Nat Rev Urol 2010; 7: 162–172.
Kathiresan AS, Ibrahim E, Aballa TC, Attia GR, Lynne CM, Brackett NL . Pregnancy outcomes by intravaginal and intrauterine insemination in 82 couples with male factor infertility due to spinal cord injuries. Fertil Steril 2011; 96: 328–331.
Kathiresan AS, Ibrahim E, Aballa TC, Attia GR, Ory SJ, Hoffman DI et al. Comparison of in vitro fertilization/intracytoplasmic sperm injection outcomes in male factor infertility patients with and without spinal cord injuries. Fertil Steril 2011; 96: 562–566.
Sonksen J, Fode M, Lochner-Ernst D, Ohl DA . Vibratory ejaculation in 140 spinal cord injured men and home insemination of their partners. Spinal Cord 2012; 50: 63–66.
Brackett NL, Ibrahim E, Iremashvili V, Aballa TC, Lynne CM . Treatment for ejaculatory dysfunction in men with spinal cord injury: an 18-year single center experience. J Urol 2010; 183: 2304–2308.
Ibrahim E, Brackett NL, Lynne CM . Advances in the management of infertility in men with spinal cord injury. Asian J Androl 2016; 18: 382–390.
Sonksen J, Biering-Sorensen F, Kristensen JK . Ejaculation induced by penile vibratory stimulation in men with spinal cord injuries. the importance of the vibratory amplitude. Paraplegia 1994; 32: 651–660.
Brackett NL, Kafetsoulis A, Ibrahim E, Aballa TC, Lynne CM . Application of 2 vibrators salvages ejaculatory failures to 1 vibrator during penile vibratory stimulation in men with spinal cord injuries. J Urol 2007; 177: 660–663.
Castle SM, Jenkins LC, Ibrahim E, Aballa TC, Lynne CM, Brackett NL . Safety and efficacy of a new device for inducing ejaculation in men with spinal cord injuries. Spinal Cord 2014; 52 (Suppl 2): S27–S29.
Krassioukov A, Warburton DE, Teasell R, Eng JJ . A systematic review of the management of autonomic dysreflexia after spinal cord injury. Arch Phys Med Rehabil 2009; 90: 682–695.
Partida E, Mironets E, Hou S, Tom VJ . Cardiovascular dysfunction following spinal cord injury. Neural Regen Res 2016; 11: 189–194.
O'Kelly F, Manecksha RP, Cullen IM, McDermott TE, Flynn R, Grainger R . Electroejaculatory stimulation and its implications for male infertility in spinal cord injury: a short history through four decades of sperm retrieval (1975–2010). Urology 2011; 77: 1349–1352.
Brackett NL, Padron OF, Lynne CM . Semen quality of spinal cord injured men is better when obtained by vibratory stimulation versus electroejaculation. J Urol 1997; 157: 151–157.
Ohl DA, Sonksen J, Menge AC, McCabe M, Keller LM . Electroejaculation versus vibratory stimulation in spinal cord injured men: sperm quality and patient preference. J Urol 1997; 157: 2147–2149.
Goetz LL, Stiens SA . Abdominal electric stimulation facilitates penile vibratory stimulation for ejaculation after spinal cord injury: a single-subject trial. Arch Phys Med Rehabil 2005; 86: 1879–1883.
Kafetsoulis A, Ibrahim E, Aballa TC, Goetz LL, Lynne CM, Brackett NL . Abdominal electrical stimulation rescues failures to penile vibratory stimulation in men with spinal cord injury: a report of two cases. Urology 2006; 68: 204–211.
Giuliano F, Clement P . Neuroanatomy and physiology of ejaculation. Annu Rev Sex Res 2005; 16: 190–216.
Karlsson AK . Autonomic dysfunction in spinal cord injury: clinical presentation of symptoms and signs. Prog Brain Res 2006; 152: 1–8.
Rabchevsky AG . Segmental organization of spinal reflexes mediating autonomic dysreflexia after spinal cord injury. Prog Brain Res 2006; 152: 265–274.
Shergill IS, Arya M, Hamid R, Khastgir J, Patel HR, Shah PJ . The importance of autonomic dysreflexia to the urologist. BJU Int 2004; 93: 923–926.
Sweis R, Biller J . Systemic complications of spinal cord injury. Curr Neurol Neurosci Rep 2017; 17: 8.
Acknowledgements
The Miami Project to Cure Paralysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chong, W., Ibrahim, E., Aballa, T. et al. Comparison of three methods of penile vibratory stimulation for semen retrieval in men with spinal cord injury. Spinal Cord 55, 921–925 (2017). https://doi.org/10.1038/sc.2017.60
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2017.60
This article is cited by
-
Evaluation of a re-engineered device for penile vibratory stimulation in men with spinal cord injury
Spinal Cord (2021)
-
Sexual Health in the Neurogenic Patient
Current Bladder Dysfunction Reports (2020)
-
Management of Erectile Dysfunction and Infertility in the Male Spinal Cord Injury Patient
Current Urology Reports (2018)