Key Points
-
Cytotoxic T lymphocytes (CTLs) and natural killer (NK) cells kill virus-infected and transformed cells through both the death-receptor and granule exocytosis pathways. The perforin-dependent granule exocytosis mechanism is crucial for protecting the host against many viral infections, and in mice this pathway is involved in immune surveillance of certain spontaneous cancers, especially B-cell lymphomas.
-
In both humans and rodents, perforin is crucial for the function of the granule exocytosis pathway, as it is required for the trafficking of granzymes to their pro-apoptotic substrates in the target cell. Deficiency in perforin results in severe immune dysregulation. By contrast, deficiencies in single granzymes result in milder immunodeficiency phenotypes.
-
Perforin is encoded by a single gene, and although its primary sequence has some similarity to portions of the complement components that make up the membrane-attack complex, it is otherwise unique. The toxicity of perforin in various expression systems has made it difficult to study its structure and function. However, suitable and informative expression modalities have recently been developed.
-
In humans, congenital perforin deficiency accounts for 30–60% of known cases of the severe immunodeficiency disorder familial haemophagocytic lymphohistiocytosis (FHL). Infants typically present with marked enlargement of the liver and lymphoid organs, anaemia and sometimes neurological deficits, frequently following an otherwise innocuous viral infection.
-
Some of the missense mutations that are associated with FHL have proved invaluable in defining the normal function of certain perforin residues and domains. As a result, we now understand the basis for calcium binding to the C2 domain of perforin, which is necessary for perforin to bind irreversibly to the target-cell plasma membrane.
-
The Ala91Val mutation in perforin is a common isoform in some human populations and had previously been considered an innocent polymorphism. Recent evidence from several groups indicates that the Ala91Val mutation might result in loss of perforin function, raising the issue of why this allele has persisted in the human population.
Abstract
The granule exocytosis pathway of cytotoxic lymphocytes is crucial for immune surveillance and homeostasis. The trafficking of granule components, including the membrane-disruptive protein perforin, to the immunological synapse leads to the delivery of granule proteases (granzymes) into the target cell and its destruction through apoptosis. Several independent molecular abnormalities associated with defects of either granule trafficking or perforin function can cause cytotoxic lymphocyte dysfunction. In humans, inherited perforin mutations result in severe immune dysregulation that manifests as familial haemophagocytic lymphohistiocytosis. This Review describes recent progress in defining the structure, function, biochemistry and cell biology of perforin.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Clark, W. R. Immunology. The hole truth about perforin. Nature 369, 16–17 (1994).
Kagi, D. et al. Cytotoxicity mediated by T cells and natural killer cells is greatly impaired in perforin-deficient mice. Nature 369, 31–37 (1994). The importance of perforin in clearing virus-infected and transformed cells is shown for the first time using perforin-deficient mice.
van den Broek, M. E. et al. Decreased tumor surveillance in perforin-deficient mice. J. Exp. Med. 184, 1781–1790 (1996).
Kagi, D. & Hengartner, H. Different roles for cytotoxic T cells in the control of infections with cytopathic versus noncytopathic viruses. Curr. Opin. Immunol. 8, 472–477 (1996).
Katano, H. & Cohen, J. I. Perforin and lymphohistiocytic proliferative disorders. Br. J. Haematol. 128, 739–750 (2005).
Janka, G. E. Familial hemophagocytic lymphohistiocytosis. Eur. J. Pediatr. 140, 221–230 (1983).
Henter, J. I., Arico, M., Elinder, G., Imashuku, S. & Janka, G. Familial hemophagocytic lymphohistiocytosis. Primary hemophagocytic lymphohistiocytosis. Hematol. Oncol. Clin. North Am. 12, 417–433 (1998).
Menasche, G., Feldmann, J., Fischer, A. & de Saint Basile, G. Primary hemophagocytic syndromes point to a direct link between lymphocyte cytotoxicity and homeostasis. Immunol. Rev. 203, 165–179 (2005).
Trapani, J. A. & Sutton, V. R. Granzyme B: pro-apoptotic, antiviral and antitumor functions. Curr. Opin. Immunol. 15, 533–543 (2003).
Deng, A. et al. Granulysin, a cytolytic molecule, is also a chemoattractant and proinflammatory activator. J. Immunol. 174, 5243–5248 (2005).
Hwang, J. Y., Ohira, T., Hirono, I. & Aoki, T. A pore-forming protein, perforin, from a non-mammalian organism, Japanese flounder, Paralichthys olivaceus. Immunogenetics 56, 360–367 (2004).
Trapani, J. A. & Smyth, M. J. Functional significance of the perforin/granzyme cell death pathway. Nature Rev. Immunol. 2, 735–747 (2002).
Barry, M. & Bleackley, R. C. Cytotoxic T lymphocytes: all roads lead to death. Nature Rev. Immunol. 2, 401–409 (2002).
Heusel, J. W., Wesselschmidt, R. L., Shresta, S., Russell, J. H. & Ley, T. J. Cytotoxic lymphocytes require granzyme B for the rapid induction of DNA fragmentation and apoptosis in allogeneic target cells. Cell 76, 977–987 (1994).
Waterhouse, N. J. et al. A central role for BID in granzyme B-induced apoptosis. J. Biol. Chem. 280, 4476–4482 (2005).
Sutton, V. R., Wowk, M. E., Cancilla, M. & Trapani, J. A. Caspase activation by granzyme B is indirect, and caspase autoprocessing requires the release of proapoptotic mitochondrial factors. Immunity 18, 319–329 (2003).
Heibein, J. A. et al. Granzyme B-mediated cytochrome c release is regulated by the Bcl-2 family members Bid and Bax. J. Exp. Med. 192, 1391–1402 (2000).
Lieberman, J. & Fan, Z. Nuclear war: the granzyme A-bomb. Curr. Opin. Immunol. 15, 553–559 (2003).
Fan, Z., Beresford, P. J., Zhang, D. & Lieberman, J. HMG2 interacts with the nucleosome assembly protein SET and is a target of the cytotoxic T-lymphocyte protease granzyme A. Mol. Cell. Biol. 22, 2810–2820 (2002).
Johnson, H., Scorrano, L., Korsmeyer, S. J. & Ley, T. J. Cell death induced by granzyme C. Blood 101, 3093–3101 (2003).
Kelly, J. M. et al. Granzyme M mediates a novel form of perforin-dependent cell death. J. Biol. Chem. 279, 22236–22242 (2004).
Mullbacher, A. et al. Granzymes are the essential downstream effector molecules for the control of primary virus infections by cytolytic leukocytes. Proc. Natl Acad. Sci. USA 96, 13950–13955 (1999). This study shows that granzymes A and B, when acting synergistically with perforin, are essential for controlling primary virus infections in mice.
Trapani, J. A. Dual mechanisms of apoptosis induction by cytotoxic lymphocytes. Int. Rev. Cytol. 182, 111–192 (1998).
Devadas, S. et al. Granzyme B is critical for T cell receptor-induced cell death of type 2 helper T cells. Immunity 25, 237–247 (2006).
Keefe, D. et al. Perforin triggers a plasma membrane-repair response that facilitates CTL induction of apoptosis. Immunity 23, 249–262 (2005).
McNeil, P. L. & Kirchhausen, T. An emergency response team for membrane repair. Nature Rev. Mol. Cell Biol. 6, 499–505 (2005).
McNeil, P. L. & Terasaki, M. Coping with the inevitable: how cells repair a torn surface membrane. Nature Cell Biol. 3, e124–e129 (2001).
Reddy, A., Caler, E. V. & Andrews, N. W. Plasma membrane repair is mediated by Ca2+-regulated exocytosis of lysosomes. Cell 106, 157–169 (2001).
Henkart, P. A., Millard, P. J., Reynolds, C. W. & Henkart, M. P. Cytolytic activity of purified cytoplasmic granules from cytotoxic rat large granular lymphocyte tumors. J. Exp. Med. 160, 75–93 (1984).
Masson, D. & Tschopp, J. Isolation of a lytic, pore-forming protein (perforin) from cytolytic T-lymphocytes. J. Biol. Chem. 260, 9069–9072 (1985).
Podack, E. R., Young, J. D. & Cohn, Z. A. Isolation and biochemical and functional characterization of perforin 1 from cytolytic T-cell granules. Proc. Natl Acad. Sci. USA 82, 8629–8633 (1985). References 29–31 are the first reports of the isolation and characterization of perforin from cytotoxic lymphocytes.
Liu, C. C., Perussia, B., Cohn, Z. A. & Young, J. D. Identification and characterization of a pore-forming protein of human peripheral blood natural killer cells. J. Exp. Med. 164, 2061–2076 (1986).
Tschopp, J., Masson, D. & Schafer, S. Inhibition of the lytic activity of perforin by lipoproteins. J. Immunol. 137, 1950–1953 (1986).
Young, J. D., Hengartner, H., Podack, E. R. & Cohn, Z. A. Purification and characterization of a cytolytic pore-forming protein from granules of cloned lymphocytes with natural killer activity. Cell 44, 849–859 (1986).
Young, J. D., Liu, C. C., Leong, L. G. & Cohn, Z. A. The pore-forming protein (perforin) of cytolytic T lymphocytes is immunologically related to the components of membrane attack complex of complement through cysteine-rich domains. J. Exp. Med. 164, 2077–2082 (1986).
Young, J. D., Podack, E. R. & Cohn, Z. A. Properties of a purified pore-forming protein (perforin 1) isolated from H-2-restricted cytotoxic T cell granules. J. Exp. Med. 164, 144–155 (1986).
Young, J. D., Damiano, A., DiNome, M. A., Leong, L. G. & Cohn, Z. A. Dissociation of membrane binding and lytic activities of the lymphocyte pore-forming protein (perforin). J. Exp. Med. 165, 1371–1382 (1987).
Lichtenheld, M. G. et al. Structure and function of human perforin. Nature 335, 448–451 (1988).
Persechini, P. M. & Young, J. D. The primary structure of the lymphocyte pore-forming protein perforin: partial amino acid sequencing and determination of isoelectric point. Biochem. Biophys. Res. Commun. 156, 740–745 (1988).
Persechini, P. M., Liu, C. C., Jiang, S. & Young, J. D. The lymphocyte pore-forming protein perforin is associated with granules by a pH-dependent mechanism. Immunol. Lett. 22, 23–27 (1989).
Roozemond, R. C., Urli, D. C., Jansen, J. & Bonavida, B. Liposomes can function as targets for natural killer cytotoxic factor but not for tumor necrosis factor. J. Immunol. 142, 1209–1216 (1989).
Tschopp, J., Schafer, S., Masson, D., Peitsch, M. C. & Heusser, C. Phosphorylcholine acts as a Ca2+-dependent receptor molecule for lymphocyte perforin. Nature 337, 272–274 (1989).
Jiang, S. B., Ojcius, D. M. & Young, J. D. Perforin binding to cells and lipid membranes determined by a simple competition assay. J. Immunol. Methods 126, 29–37 (1990).
Kraut, R. P., Bose, D., Cragoe, E. J. Jr & Greenberg, A. H. The influence of calcium, sodium, and the Na+/Ca2+ antiport on susceptibility to cytolysin/perforin-mediated cytolysis. J. Immunol. 144, 3498–3505 (1990).
Persechini, P. M., Young, J. D. & Almers, W. Membrane channel formation by the lymphocyte pore-forming protein: comparison between susceptible and resistant target cells. J. Cell Biol. 110, 2109–2116 (1990).
Peters, R., Sauer, H., Tschopp, J. & Fritzsch, G. Transients of perforin pore formation observed by fluorescence microscopic single channel recording. EMBO J. 9, 2447–2451 (1990).
Liu, C. C., Walsh, C. M. & Young, J. D. Perforin: structure and function. Immunol. Today 16, 194–201 (1995).
Rochel, N. & Cowan, J. Negative cooperativity exhibited by the lytic amino-terminal domain of human perforin: implications for perforin-mediated cell lysis. Chem. Biol. 3, 31–36 (1996).
Natarajan, K. & Cowan, J. A. Solution structure of a synthetic lytic peptide: the perforin amino terminus. Chem. Biol. 5, 147–154 (1998).
Nalefski, E. A. & Falke, J. J. The C2 domain calcium-binding motif: structural and functional diversity. Protein Sci. 5, 2375–2390 (1996).
Pappa, H., Murray-Rust, J., Dekker, L. V., Parker, P. J. & McDonald, N. Q. Crystal structure of the C2 domain from protein kinase C-δ. Structure 6, 885–894 (1998).
Sutton, R. B., Ernst, J. A. & Brunger, A. T. Crystal structure of the cytosolic C2A-C2B domains of synaptotagmin III. Implications for Ca2+-independent SNARE complex interaction. J. Cell Biol. 147, 589–598 (1999).
Voskoboinik, I. et al. Calcium-dependent plasma membrane binding and cell lysis by perforin are mediated through its C2 domain: a critical role for aspartate residues 429, 435, 483, and 485 but not 491. J. Biol. Chem. 280, 8426–8434 (2005).
Uellner, R. et al. Perforin is activated by a proteolytic cleavage during biosynthesis which reveals a phospholipid-binding C2 domain. EMBO J. 16, 7287–7296 (1997). Post-translational modifications of perforin are shown to be essential for its proteolytic activity.
Balaji, K. N., Schaschke, N., Machleidt, W., Catalfamo, M. & Henkart, P. A. Surface cathepsin B protects cytotoxic lymphocytes from self-destruction after degranulation. J. Exp. Med. 196, 493–503 (2002).
Baran, K. et al. Cytotoxic T lymphocytes from cathepsin B-deficient mice survive normally in vitro and in vivo after encountering and killing target cells. J. Biol. Chem. 281, 30485–30491 (2006).
Henter, J. I., Elinder, G., Soder, O. & Ost, A. Incidence in Sweden and clinical features of familial hemophagocytic lymphohistiocytosis. Acta Paediatr. Scand. 80, 428–435 (1991).
Janka, G. & Zur Stadt, U. Familial and acquired hemophagocytic lymphohistiocytosis. Hematology Am. Soc. Hematol. Educ. Program 82–88 (2005).
Farquhar, J. W. & Claireaux, A. E. Familial haemophagocytic reticulosis. Arch. Dis. Child. 27, 519–525 (1952).
Stepp, S. E. et al. Perforin gene defects in familial hemophagocytic lymphohistiocytosis. Science 286, 1957–1959 (1999). This is the first study that shows the physiological significance of perforin in humans. Perforin mutations in both alleles are linked to the cause of FHL.
Clementi, R. et al. Six novel mutations in the PRF1 gene in children with haemophagocytic lymphohistiocytosis. J. Med. Genet. 38, 643–646 (2001).
Feldmann, J. et al. Functional consequences of perforin gene mutations in 22 patients with familial haemophagocytic lymphohistiocytosis. Br. J. Haematol. 117, 965–972 (2002).
Molleran Lee, S. et al. Characterisation of diverse PRF1 mutations leading to decreased natural killer cell activity in North American families with haemophagocytic lymphohistiocytosis. J. Med. Genet. 41, 137–144 (2004). This is the largest mutational analysis of the perforin gene in patients with FHL2.
Ohadi, M. et al. Localization of a gene for familial hemophagocytic lymphohistiocytosis at chromosome 9q21.3–22 by homozygosity mapping. Am. J. Hum. Genet. 64, 165–171 (1999).
Feldmann, J. et al. Munc13–4 is essential for cytolytic granules fusion and is mutated in a form of familial hemophagocytic lymphohistiocytosis (FHL3). Cell 115, 461–473 (2003). A trafficking defect in cytotoxic lymphocytes that is due to mutations in a Munc-protein-family member is associated with patients with the FHL3 form of disease.
Neeft, M. et al. Munc13–4 is an effector of rab27a and controls secretion of lysosomes in hematopoietic cells. Mol. Biol. Cell 16, 731–741 (2005).
Ishii, E. et al. Review of hemophagocytic lymphohistiocytosis (HLH) in children with focus on Japanese experiences. Crit. Rev. Oncol. Hematol. 53, 209–223 (2005).
Ishii, E. et al. Genetic subtypes of familial hemophagocytic lymphohistiocytosis: correlations with clinical features and cytotoxic T lymphocyte/natural killer cell functions. Blood 105, 3442–3448 (2005).
zur Stadt, U. et al. Linkage of familial hemophagocytic lymphohistiocytosis (FHL) type-4 to chromosome 6q24 and identification of mutations in syntaxin 11. Hum. Mol. Genet. 14, 827–834 (2005). The fourth gene associated with FHL is identified as a member of the SNARE family of proteins, syntaxin 11.
Zur Stadt, U. et al. Mutation spectrum in children with primary hemophagocytic lymphohistiocytosis: molecular and functional analyses of PRF1, UNC13D, STX11, and RAB27A. Hum. Mutat. 27, 62–68 (2006).
Imashuku, S. et al. Occurrence of haemophagocytic lymphohistiocytosis at less than 1 year of age: analysis of 96 patients. Eur. J. Pediatr. 164, 315–319 (2005).
Badovinac, V. P., Hamilton, S. E. & Harty, J. T. Viral infection results in massive CD8+ T cell expansion and mortality in vaccinated perforin-deficient mice. Immunity 18, 463–474 (2003).
Jordan, M. B., Hildeman, D., Kappler, J. & Marrack, P. An animal model of hemophagocytic lymphohistiocytosis (HLH): CD8+ T cells and interferon γ are essential for the disorder. Blood 104, 735–743 (2004).
Lee, S. M. et al. Patients of African ancestry with hemophagocytic lymphohistiocytosis share a common haplotype of PRF1 with a 50delT mutation. J. Pediatr. 149, 134–137 (2006).
Voskoboinik, I., Thia, M. C. & Trapani, J. A. A functional analysis of the putative polymorphisms A91V and N252S and 22 missense perforin mutations associated with familial hemophagocytic lymphohistiocytosis. Blood 105, 4700–4706 (2005).
Shiver, J. W. & Henkart, P. A. A noncytotoxic mast cell tumor line exhibits potent IgE-dependent cytotoxicity after transfection with the cytolysin/perforin gene. Cell 64, 1175–1181 (1991).
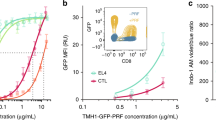
Voskoboinik, I. et al. The functional basis for hemophagocytic lymphohistiocytosis in a patient with co-inherited missense mutations in the perforin (PFN1) gene. J. Exp. Med. 200, 811–816 (2004). This is the introduction of novel methodologies for studying perforin function. It is the first formal demonstration that perforin mutations found in patients with FHL affect perforin function at the presynaptic or postsynaptic levels.
Risma, K. A., Frayer, R. W., Filipovich, A. H. & Sumegi, J. Aberrant maturation of mutant perforin underlies the clinical diversity of hemophagocytic lymphohistiocytosis. J. Clin. Invest. 116, 182–192 (2006).
Trapani, J. A. & Voskoboinik, I. The vexed question of assessing perforin expression, processing and function. J. Clin. Invest., [online] (2006).
Trambas, C. et al. A single amino acid change, A91V, leads to conformational changes that can impair processing to the active form of perforin. Blood 106, 932–937 (2005).
Santoro, A. et al. A single amino acid change A91V in perforin: a novel, frequent predisposing factor to childhood acute lymphoblastic leukemia? Haematologica 90, 697–698 (2005).
Zur Stadt, U. et al. A91V is a polymorphism in the perforin gene not causative of an FHLH phenotype. Blood 104, 1909–1910 (2004).
Busiello, R. et al. Role of A91V mutation in perforin gene in hemophagocytic lymphohistiocytosis. Blood 104, 1910 (2004).
Busiello, R. et al. Atypical features of familial hemophagocytic lymphohistiocytosis. Blood 103, 4610–4612 (2004).
Clementi, R. et al. Adult onset and atypical presentation of hemophagocytic lymphohistiocytosis in siblings carrying PRF1 mutations. Blood 100, 2266–2267 (2002).
Mancebo, E. et al. Familial hemophagocytic lymphohistiocytosis in an adult patient homozygous for A91V in the perforin gene, with tuberculosis infection. Haematologica 91, 1257–1260 (2006).
Clementi, R. et al. Variations of the perforin gene in patients with autoimmunity/lymphoproliferation and defective Fas function. Blood 108, 3079–3084 (2006).
Smyth, M. J., Voskoboinik, I. & Trapani, J. A. Immune surveillance of lymphoma in humans? Blood 105, 4159–4160 (2005).
Clementi, R. et al. A proportion of patients with lymphoma may harbor mutations of the perforin gene. Blood 105, 4424–4428 (2005).
Mehta, P. A. et al. Perforin polymorphism A91V and susceptibility to B-precursor childhood acute lymphoblastic leukemia: a report from the Children's Oncology Group. Leukemia 20, 1539–1541 (2006).
Nakajima, H., Park, H. L. & Henkart, P. A. Synergistic roles of granzymes A and B in mediating target cell death by rat basophilic leukemia mast cell tumors also expressing cytolysin/perforin. J. Exp. Med. 181, 1037–1046 (1995).
Shiver, J. W., Su, L. & Henkart, P. A. Cytotoxicity with target DNA breakdown by rat basophilic leukemia cells expressing both cytolysin and granzyme A. Cell 71, 315–322 (1992). Reconstitution of perforin and granzyme in a cellular system shows their synergistic mode of action.
Binder, D. et al. Aplastic anemia rescued by exhaustion of cytokine-secreting CD8+ T cells in persistent infection with lymphocytic choriomeningitis virus. J. Exp. Med. 187, 1903–1920 (1998).
Matloubian, M. et al. A role for perforin in downregulating T-cell responses during chronic viral infection. J. Virol. 73, 2527–2536 (1999).
Shustov, A. et al. Role of perforin in controlling B-cell hyperactivity and humoral autoimmunity. J. Clin. Invest. 106, R39–R47 (2000).
Spielman, J., Lee, R. K. & Podack, E. R. Perforin/Fas-ligand double deficiency is associated with macrophage expansion and severe pancreatitis. J. Immunol. 161, 7063–7070 (1998).
Kagi, D., Odermatt, B. & Mak, T. W. Homeostatic regulation of CD8+ T cells by perforin. Eur. J. Immunol. 29, 3262–3272 (1999).
Spaner, D., Raju, K., Rabinovich, B. & Miller, R. G. A role for perforin in activation-induced T cell death in vivo: increased expansion of allogeneic perforin-deficient T cells in SCID mice. J. Immunol. 162, 1192–1199 (1999).
Loh, J., Chu, D. T., O'Guin, A. K., Yokoyama, W. M. & Virgin, H. W. T. Natural killer cells utilize both perforin and γ interferon to regulate murine cytomegalovirus infection in the spleen and liver. J. Virol. 79, 661–667 (2005).
Tay, C. H. et al. The role of LY49 NK cell subsets in the regulation of murine cytomegalovirus infections. J. Immunol. 162, 718–726 (1999).
Gupta, M. et al. CD8-mediated protection against Ebola virus infection is perforin dependent. J. Immunol. 174, 4198–4202 (2005).
Muller, U. et al. Concerted action of perforin and granzymes is critical for the elimination of Trypanosoma cruzi from mouse tissues, but prevention of early host death is in addition dependent on the FasL/Fas pathway. Eur. J. Immunol. 33, 70–78 (2003).
Ma, L. L. et al. NK cells use perforin rather than granulysin for anticryptococcal activity. J. Immunol. 173, 3357–3365 (2004).
Mullbacher, A. et al. Granzyme A is critical for recovery of mice from infection with the natural cytopathic viral pathogen, ectromelia. Proc. Natl Acad. Sci. USA 93, 5783–5787 (1996).
Riera, L. et al. Murine cytomegalovirus replication in salivary glands is controlled by both perforin and granzymes during acute infection. Eur. J. Immunol. 30, 1350–1355 (2000).
Harty, J. T. & Badovinac, V. P. Influence of effector molecules on the CD8+ T cell response to infection. Curr. Opin. Immunol. 14, 360–365 (2002).
Smyth, M. J. et al. Perforin-mediated cytotoxicity is critical for surveillance of spontaneous lymphoma. J. Exp. Med. 192, 755–760 (2000). Perforin-regulated lymphocyte cytotoxicity protects against lymphomagenesis and is responsible for the rejection of transplanted primary lymphomas in mice.
Street, S. E., Trapani, J. A., MacGregor, D. & Smyth, M. J. Suppression of lymphoma and epithelial malignancies effected by interferon γ. J. Exp. Med. 196, 129–134 (2002).
Street, S. E. et al. Innate immune surveillance of spontaneous B cell lymphomas by natural killer cells and γδ T cells. J. Exp. Med. 199, 879–884 (2004).
Curcio, C. et al. Nonredundant roles of antibody, cytokines, and perforin in the eradication of established Her-2/neu carcinomas. J. Clin. Invest. 111, 1161–1170 (2003).
Brady, J., Hayakawa, Y., Smyth, M. J. & Nutt, S. L. IL-21 induces the functional maturation of murine NK cells. J. Immunol. 172, 2048–2058 (2004).
Smyth, M. J. et al. Perforin is a major contributor to NK cell control of tumor metastasis. J. Immunol. 162, 6658–6662 (1999).
Street, S. E., Cretney, E. & Smyth, M. J. Perforin and interferon-γ activities independently control tumor initiation, growth, and metastasis. Blood 97, 192–197 (2001).
Bird, C. H. et al. Cationic sites on granzyme B contribute to cytotoxicity by promoting its uptake into target cells. Mol. Cell. Biol. 25, 7854–7867 (2005).
Sutton, V. R. et al. Initiation of apoptosis by granzyme B requires direct cleavage of bid, but not direct granzyme B-mediated caspase activation. J. Exp. Med. 192, 1403–1414 (2000).
Barry, M. et al. Granzyme B short-circuits the need for caspase 8 activity during granule-mediated cytotoxic T-lymphocyte killing by directly cleaving Bid. Mol. Cell. Biol. 20, 3781–94 (2000).
Grossman, W. J. et al. Development of hemophagocytic lymphohistiocytosis in triplets infected with HHV-8. Blood 106, 1203–1206 (2005).
Kogawa, K. et al. Perforin expression in cytotoxic lymphocytes from patients with hemophagocytic lymphohistiocytosis and their family members. Blood 99, 61–66 (2002).
Katano, H. et al. Chronic active Epstein–Barr virus infection associated with mutations in perforin that impair its maturation. Blood 103, 1244–1252 (2004).
Ueda, I. et al. Correlation between phenotypic heterogeneity and gene mutational characteristics in familial hemophagocytic lymphohistiocytosis (FHL). Pediatr. Blood Cancer 46, 482–488 (2006).
Feldmann, J. et al. Severe and progressive encephalitis as a presenting manifestation of a novel missense perforin mutation and impaired cytolytic activity. Blood 105, 2658–2663 (2005).
Nagle, D. L. et al. Identification and mutation analysis of the complete gene for Chediak–Higashi syndrome. Nature Genet. 14, 307–311 (1996).
Barbosa, M. D. et al. Identification of the homologous beige and Chediak–Higashi syndrome genes. Nature 382, 262–265 (1996).
Introne, W., Boissy, R. E. & Gahl, W. A. Clinical, molecular, and cell biological aspects of Chediak–Higashi syndrome. Mol. Genet. Metab. 68, 283–303 (1999).
Clark, R. & Griffiths, G. M. Lytic granules, secretory lysosomes and disease. Curr. Opin. Immunol. 15, 516–521 (2003).
Trambas, C. M. & Griffiths, G. M. Delivering the kiss of death. Nature Immunol. 4, 399–403 (2003).
Griscelli, C. et al. A syndrome associating partial albinism and immunodeficiency. Am. J. Med. 65, 691–702 (1978).
Menasche, G. et al. Mutations in RAB27A cause Griscelli syndrome associated with haemophagocytic syndrome. Nature Genet. 25, 173–176 (2000).
Stinchcombe, J. C. et al. Rab27a is required for regulated secretion in cytotoxic T lymphocytes. J. Cell Biol. 152, 825–834 (2001).
Purtilo, D. T., Cassel, C. K., Yang, J. P. & Harper, R. X-linked recessive progressive combined variable immunodeficiency (Duncan's disease). Lancet 1, 935–940 (1975).
Dupre, L. et al. SAP controls the cytolytic activity of CD8+ T cells against EBV-infected cells. Blood 105, 4383–4389 (2005).
Sumegi, J. et al. Correlation of mutations of the SH2D1A gene and Epstein–Barr virus infection with clinical phenotype and outcome in X-linked lymphoproliferative disease. Blood 96, 3118–3125 (2000).
Coffey, A. J. et al. Host response to EBV infection in X-linked lymphoproliferative disease results from mutations in an SH2-domain encoding gene. Nature Genet. 20, 129–135 (1998).
Arico, M. et al. Hemophagocytic lymphohistiocytosis due to germline mutations in SH2D1A, the X-linked lymphoproliferative disease gene. Blood 97, 1131–1133 (2001).
Latour, S. et al. Binding of SAP SH2 domain to FynT SH3 domain reveals a novel mechanism of receptor signalling in immune regulation. Nature Cell Biol. 5, 149–154 (2003).
Pao, L. I. et al. Functional analysis of granzyme M and its role in immunity to infection. J. Immunol. 175, 3235–3243 (2005).
Takahashi, T. et al. Generalized lymphoproliferative disease in mice, caused by a point mutation in the Fas ligand. Cell 76, 969–976 (1994).
Watanabe, T. et al. A molecular genetic linkage map of mouse chromosome 19, including the lpr, Ly-44, and Tdt genes. Biochem. Genet. 29, 325–335 (1991).
Pham, C. T. & Ley, T. J. Dipeptidyl peptidase I is required for the processing and activation of granzymes A and B in vivo. Proc. Natl Acad. Sci. USA 96, 8627–8632 (1999).
Rieux-Laucat, F., Le Deist, F. & De Saint Basile, G. Autoimmune lymphoproliferative syndrome and perforin. N. Engl. J. Med. 352, 306–307 (2005).
Ericson, K. G. et al. Spectrum of perforin gene mutations in familial hemophagocytic lymphohistiocytosis. Am. J. Hum. Genet. 68, 590–597 (2001).
Acknowledgements
M.J.S. and J.A.T. are supported by senior fellowships and a program grant from the National Health and Medical Research Council of Australia. J.A.T. and I.V. are supported by a program grant from the Juvenile Diabetes Research Foundation. We also thank the many members of the Cancer Immunology Program and our collaborators for contributions over the years to many of the findings referred to in this Review.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
Glossary
- Haemophagocytosis
-
The phagocytosis of erythrocytes that results from excessive activation of macrophages. This is usually a consequence of uncontrolled activation and proliferation of T cells.
- Thrombocytopaenia
-
A reduced number of circulating platelets, owing to either the failure of production from bone-marrow megakaryocytes or increased clearance from the blood, predominantly in the spleen.
- SET complex
-
A 270–420 kDa multiprotein complex that is associated with the endoplasmic reticulum. Pro-apoptotic granzyme A cleaves components of the SET complex, such as the nuclear assembly protein SET, the DNA-bending protein HMG2 and the base-excision repair pathway apurinic endonuclease APE1.
- Ectromelia
-
A natural poxvirus pathogen of mice that is similar to variola virus (smallpox) in humans and vaccinia virus (cowpox) in cows. Cytotoxic T lymphocyes and natural killer cells from mice that are deficient in granzyme A and B or perforin are incapable of controlling primary infection with ectromelia virus.
- Nonsense mutation
-
A mutation that results in the introduction of a stop codon to cause the premature termination of the protein.
- Missense mutation
-
A mutation that results in the substitution of an amino acid in a protein.
- SNARE
-
(Soluble-N-ethylmaleimide-sensitive-factor accessory-protein receptor). A complex formed between the vesicle and the target membrane, with which it is destined to fuse. t-(target membrane) SNAREs on target-membranes, and v-(vesicle-associated) SNAREs on transport vesicles cooperate with other proteins to allow docking and fusion of membranes.
- Heterozygosity
-
The proportion of individuals in a population that carry two different alleles at a locus.
- Hodgkin's lymphoma
-
A B-cell lymphoma that is characterized by the presence of Reed–Sternberg cells; it is observed in the lymph nodes, spleen, liver and bone marrow. It is more commonly diagnosed in younger people (median age 33 years).
- Non-Hodgkin's lymphoma
-
A lymphocytic B- or T-cell lymphoma. This lymphoma is more common among older people (median age 65 years).
- BCR–ABL
-
A tyrosine kinase oncogene. The Abelson leukaemia-virus protein (ABL) is fused with the breakpoint-cluster region (BCR) in the Philadelphia-chromosome translocation found in chronic myeloid leukaemia.
Rights and permissions
About this article
Cite this article
Voskoboinik, I., Smyth, M. & Trapani, J. Perforin-mediated target-cell death and immune homeostasis. Nat Rev Immunol 6, 940–952 (2006). https://doi.org/10.1038/nri1983
Issue Date:
DOI: https://doi.org/10.1038/nri1983
This article is cited by
-
Ultrasound-targeted microbubble destruction remodels tumour microenvironment to improve immunotherapeutic effect
British Journal of Cancer (2023)
-
Preclinical 3D-model supports an invisibility cloak for adenoid cystic carcinoma
Scientific Reports (2023)
-
Osimertinib resistance prognostic gene signature: STRIP2 is associated with immune infiltration and tumor progression in lung adenocarcinoma
Journal of Cancer Research and Clinical Oncology (2023)
-
Infection and inflammation: radiological insights into patterns of pediatric immune-mediated CNS injury
Neuroradiology (2023)
-
Mechanism research and treatment progress of NAD pathway related molecules in tumor immune microenvironment
Cancer Cell International (2022)