Key Points
-
Approximately 10% of cancers in women occur in those <45 years old, and in the USA, the number of new cases of invasive cancer diagnosed in women during 2012 was almost 800,000
-
Chemotherapy, radiotherapy, surgery and bone marrow transplantation have led to a considerable improvement in survival rates, but these treatments can result in premature ovarian failure (POF)
-
The risk of POF depends on the follicular reserve, the age of the patient and the type and dose of drugs used
-
Different options exist to preserve fertility in women at risk of POF, including ovarian transposition, embryo and oocyte cryopreservation, and ovarian tissue cryopreservation
-
In prepubertal girls or patients requiring immediate chemotherapy, ovarian tissue cryopreservation is the only method currently available
-
Medical therapy (with a gonadotropin-releasing hormone agonist) before chemotherapy is still controversial
Abstract
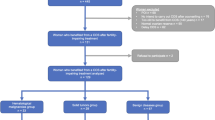
In women, ∼10% of cancers occur in those <45 years old. Chemotherapy, radiotherapy and bone marrow transplantation can cure >90% of girls and young women with diseases that require such treatments. However, these treatments can result in premature ovarian failure, depending on the follicular reserve, the age of the patient and the type and dose of drugs used. This article discusses the different fertility preservation strategies: medical therapy before chemotherapy; ovarian transposition; embryo cryopreservation; oocyte vitrification; and ovarian tissue cryopreservation. The indications, results and risks of these options are discussed. Whether medical therapy should be used to protect the gonads during chemotherapy remains a source of debate. Fertility preservation needs to be completed before chemotherapy and/or irradiation is started and might take 2–3 weeks with established techniques such as embryo or oocyte cryopreservation. Further studies are needed in patients with cancer to confirm the excellent outcomes obtained in patients without cancer or in egg donation programmes. For prepubertal girls or cases where immediate therapy is required, cryopreservation of ovarian tissue is the only available option. Finally, possible future approaches are reviewed, including in vitro maturation of nonantral follicles, the artificial ovary, oogonial stem cells and drugs to prevent follicle loss.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Letourneau, J. M. et al. Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer 118, 1710–1717 (2012).
Siegel, R., Naishadham, D. &. Jemal, A. Cancer statistics, 2012. CA Cancer J. Clin. 62, 10–29 (2012).
Bedoschi, G. & Oktay, K. Current approach to fertility preservation by embryo cryopreservation. Fertil. Steril. 99, 1496–1502 (2013).
Donnez, J. et al. Ovarian tissue cryopreservation and transplantation: a review. Hum. Reprod. Update 12, 519–535 (2006).
Donnez, J. et al. Ovarian tissue cryopreservation and transplantation in cancer patients. Best Pract. Res. Clin. Obstet. Gynaecol. 24, 87–100 (2010).
Wallace, W. H. B., Anderson, R. A. & Irvine, D. S. Fertility preservation for young patients with cancer: who is at risk and what can be offered? Lancet Oncol. 6, 209–219 (2005).
Donnez, J. et al. Restoration of ovarian function after orthotopic (intraovarian and periovarian) transplantation of cryopreserved ovarian tissue in a woman treated by bone marrow transplantation for sickle cell anemia: case report. Hum. Reprod. 21, 183–188 (2006).
Meirow, D. & Nugent, D. The effects of radiotherapy and chemotherapy on female reproduction. Hum. Reprod. Update 7, 535–543 (2001).
Teinturier, C., Hartmann, O., Valteau-Couanet, D., Benhamou, E. & Bougneres, P. F. Ovarian function after autologous bone marrow transplantation in childhood: high-dose busulfan is a major cause of ovarian failure. Bone Marrow Transplant. 22, 989–994 (1998).
Donnez, J. et al. Pregnancy and live birth after autotransplantation of frozen-thawed ovarian tissue in a patient with metastatic disease undergoing chemotherapy and hematopoietic stem cell transplantation. Fertil. Steril. 95, 1787.e1–1787.e4 (2011).
Jadoul, P. & Donnez, J. How does bone marrow transplantation affect ovarian function and fertility? Curr. Opin. Obstet. Gynecol. 24, 164–171 (2012).
Wallace, W. H., Thomson, A. B., Saran, F. & Kelsey, T. W. Predicting age of ovarian failure after radiation to a field that includes the ovaries. Int. J. Radiat. Oncol. Biol. Phys. 62, 738–744 (2005).
Schmidt, K. T. et al. Autotransplantation of cryopreserved ovarian tissue in 12 women with chemotherapy-induced premature ovarian failure: the Danish experience. Fertil. Steril. 95, 695–701 (2011).
Anderson, R. A. & Wallace, H. B. Antimüllerian hormone, the assessment of the ovarian reserve, and the reproductive outcome of the young patient with cancer. Fertil. Steril. 99, 1469–1475 (2013).
Wallace, W. H., Thomson, A. B. & Kelsey, T. W. The radiosensitivity of the human oocyte. Hum. Reprod. 18, 117–121 (2003).
Donnez, J. & Dolmans, M. M. Preservation of fertility in females with haematological malignancy. Br. J. Haematol. 154, 175–184 (2011).
Jadoul, P., Dolmans, M. M. & Donnez, J. Fertility preservation in girls during childhood: is it feasible, efficient and safe and to whom should it be proposed? Hum. Reprod. Update 16, 617–630 (2010).
Wallace, W. H. & Kelsey, T. W. Human ovarian reserve from conception to the menopause. PLoS ONE 27, e8772 (2010).
Rodriguez-Wallberg, K. A. & Oktay, K. Fertility preservation medicine: options for young adults and children with cancer. J. Pediatr. Hematol. Oncol. 32, 390–396 (2010).
Wallace, W. H., Kelsey, T. W. & Anderson, R. A. Ovarian cryopreservation: experimental or established and a cure for the menopause? Reprod. Biomed. Online 25, 93–95 (2012).
Kelsey, T. W. & Wallace, W. H. Ovarian volume correlates strongly with the number of nongrowing follicles in the human ovary. Obstet. Gynecol. Int. 2012, 305025 (2012).
Albamonte, M. I., Albamonte, M. S., Stella, I., Zuccardi, L. & Vitullo, A. D. The infant and pubertal human ovary: Balbiani's body-associated VASA expression, immunohistochemical detection of apoptosis-related BCL2 and BAX proteins, and DNA fragmentation. Hum. Reprod. 28, 698–706 (2013).
Tilly, J. L. Commuting the death sentence: How oocytes strive to survive. Nat. Rev. Mol. Cell Biol. 2, 838–848 (2001).
Tilly, J. L. & Sinclair, D. A. Germline energetics, aging, and female infertility. Cell. Metab. 17, 838–850 (2013).
Liu, L. & Keefe, D. L. Ageing-associated aberration in meiosis of oocytes from senescence-accelerated mice. Hum. Reprod. 17, 267–685 (2002).
Liu, J. P. & Li, H. Telomerase in the ovary. Reproduction 140, 215–222 (2010).
Zou, K. et al. Production of offspring from a germline stem cell line derived from neonatal ovaries. Nat. Cell Biol. 11, 631–636 (2009).
White, Y. A. et al. Oocyte formation by mitotically active germ cells purified from ovaries of reproductive-age women. Nat. Med. 18, 413–421 (2012).
Telfer, E. E. & Zelinski, M. B. Ovarian follicle culture: advances and challenges for human and nonhuman primates. Fertil. Steril. 99, 1523–1533 (2013).
Woods, D. C. & Tilly, J. L. Isolation, characterization and propagation of mitotically active germ cells from adult mouse and human ovaries. Nat. Protoc. 8, 966–988 (2013).
Brougham, M. F. et al. Anti-Müllerian hormone is a marker of gonadotoxicity in pre- and postpubertal girls treated for cancer: a prospective study. J. Clin. Endocrinol. Metab. 97, 2059–2067 (2012).
Anderson, R. A. & Cameron, D. A. Pretreatment serum anti-Müllerian hormone predict long-term ovarian function and bone mass after chemotherapy for early breast cancer. J. Clin. Endocrinol. Metab. 96, 1336–1343 (2011).
Decanter, C. et al. Anti-Müllerian hormone follow-up in young women treated by chemotherapy for lymphoma: preliminary results. Reprod. Biomed. Online 20, 280–285 (2010).
Hagen, C. P. et al. Low concentration of circulating anti-Müllerian hormone is not predictive of reduced fecundability in young healthy women: a prospective cohort study. Fertil. Steril. 98, 1602–1608 (2012).
Hamre, H., Kiserud, C. E., Ruud, E., Thorsby, P. M. & Fossa, S. D. Gonadal function and parenthood 20 years after treatment for childhood lymphoma: a crosssectional study. Pediatr. Blood Cancer 59, 271–277 (2012).
Janse, F. et al. Limited value of ovarian function markers following orthotopic transplantation of ovarian tissue after gonadotoxic treatment. J. Clin. Endocrinol. Metab. 96, 1136–1144 (2011).
Lawrenz, B. et al. Centers of FertiPROTEKT Network. Reduced pretreatment ovarian reserve in premenopausal female patients with Hodgkin lymphoma or non-Hodgkin-lymphoma-evaluation by using antimüllerian hormone and retrieved oocytes. Fertil. Steril. 98, 141–144 (2012).
Ebbel, E., Katz, A., Kao, C. N. & Cedars, M. Reproductive aged women with cancer have a lower antral follicle count than expected. Fertil. Steril. 96, S199–S200 (2011).
Donnez, J. Introduction: Fertility preservation, from cancer to benign disease to social reasons: the challenge of the present decade. Fertil. Steril. 99, 1467–1468 (2013).
Donnez, J. et al. Restoration of ovarian activity and pregnancy after transplantation of cryopreserved ovarian tissue: a review of 60 cases of reimplantation. Fertil. Steril. 99, 1503–1513 (2013).
Andersen, C. Y. et al. Two successful pregnancies following autotransplantation of frozen/thawed ovarian tissue. Hum. Reprod. 23, 2266–2272 (2008).
Silber, S. J. et al. Ovarian transplantation between monozygotic twins discordant for premature ovarian failure. N. Engl. J. Med. 353, 58–63 (2005).
Silber, S. J. Ovary cryopreservation and transplantation for fertility preservation. Mol. Hum. Reprod. 18, 59–67 (2012).
Meirow, D. et al. Pregnancy after transplantation of cryopreserved ovarian tissue in a patient with ovarian failure after chemotherapy. N. Engl. J. Med. 353, 318–321 (2005).
Poirot, C. J. et al. Feasibility of ovarian tissue cryopreservation for prepubertal females with cancer. Pediatr. Blood Cancer 49, 74–78 (2007).
Donnez, J. et al. Livebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet 364, 1405–1410 (2004).
Donnez, J. et al. Children born after autotransplantation of cryopreserved ovarian tissue, a review of 13 live births. Ann. Med. 43, 437–450 (2011).
Glode, L. M., Robinson, J. & Gould, S. F. Protection from cyclophosphamide-induced testicular damage with an analogue of gonadotropin-releasing hormone. Lancet 1, 1132–1134 (1981).
Blumenfeld, Z. & von Wolff, M. GnRH-analogues and oral contraceptives for fertility preservation in women during chemotherapy. Hum. Reprod. Update 14, 543–552 (2008).
Bedaiwy, M. A. et al. Gonadotropin-releasing hormone analog cotreatment for preservation of ovarian function during gonadotoxic chemotherapy: a systematic review and meta-analysis. Fertil. Steril. 95, 906–914 (2011).
Elgindy, E. A. et al. Gonadatrophin suppression to prevent chemotherapy-induced ovarian damage: a randomized controlled trial. Obstet. Gynecol. 121, 78–86 (2013).
Del Mastro, L. et al. Effect of the gonadotropin-releasing hormone analogue triptorelin on the occurrence of chemotherapy-induced early menopause in premenopausal women with breast cancer: a randomized trial. JAMA 306, 269–276 (2011).
Demeestere, I. et al. Gonadotropin-releasing hormone agonist for the prevention of chemotherapy-induced ovarian failure in patients with lymphoma: 1-year follow-up of a prospective randomized trial. J. Clin. Oncol. 31, 903–909 (2013).
Loren, A. W. et al. Fertility preservation for patients with cancer: American society of clinical oncology clinical practice guideline update. J. Clin. Oncol. 31, 2500–2510 (2013).
Morice, P. et al. Fertility results after ovarian transposition for pelvic malignancies treated by external irradiation or brachytherapy. Hum. Reprod. 13, 660–663 (1998).
Morice, P. et al. Ovarian transposition for patients with cervical carcinoma treated by radiosurgical combination. Fertil. Steril. 74, 743–748 (2000).
Al-Asari, S. & Abduljabbar, A. Laparoscopic ovarian transposition before pelvic radiation in rectal cancer patient: safety and feasibility. Ann. Surg. Innov. Res. 6, 9 (2012).
Han, S. S. et al. Underuse of ovarian transposition in reproductive-aged cancer patients treated by primary or adjuvant pelvic irradiation. J. Obstet. Gynaecol. Res. 37, 825–829 (2011).
Bisharah, M. & Tulandi, T. Laparoscopic preservation of ovarian function: an underused procedure. Am. J. Obstet. Gynecol. 188, 367–370 (2003).
Barahmeh, S. et al. Ovarian transposition before pelvic irradiation: Indications and functional outcome. J. Obstet. Gynaecol. Res. http://dx.doi.org/10.1111/jog.12096.
Morice, P., Haie-Meder, C., Pautier, P., Lhomme, C. & Castaigne, D. Ovarian metastasis on transposed ovary in patients treated for squamous cell carcinoma of the uterine cervix: report of two cases and surgical implications. Gynecol. Oncol. 83, 605–607 (2001).
Cakmak, H. & Rosen, M. P. Ovarian stimulation in cancer patients. Fertil. Steril. 99, 1476–1484 (2013).
Devroey, P., Polyzos, N. P. & Blockeel, C. An OHSS-Free Clinic by segmentation of IVF treatment. Hum. Reprod. 26, 2593–2597 (2011).
Roque, M. et al. Fresh embryo transfer versus frozen embryo transfer in in vitro fertilization cycles: a systematic review and meta-analysis. Fertil. Steril. 9, 156–162 (2013).
Von Wolff, M. et al. Ovarian stimulation to cryopreserve fertilized oocytes in cancer patients can be started in the luteal phase. Fertil. Steril. 92, 1360–1365 (2009).
Bedoschi, G. M., De Albuquerque, F. O., Ferriani, R. A. & Navarro, P. A. Ovarian stimulation during the luteal phase for fertility preservation of cancer patients: case reports and review of the literature. J. Assist. Reprod. Genet. 27, 491–494 (2010).
Oktay, K. Further evidence on the safety and success of ovarian stimulation with letrozole and tamoxifen in breast cancer patients undergoing in vitro fertilization to cryopreserve their embryos for fertility preservation. J. Clin. Oncol. 23, 3858–3859 (2005).
Oktay, K., Buyuk, E., Libertella, N., Akar, M. & Rosenwaks, Z. Fertility preservation in breast cancer patients: a prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J. Clin. Oncol. 23, 4347–4353 (2005).
Cobo, A., Garcia-Velasco, J. A., Domingo, J., Remohí, J. & Pellicer, A. Is vitrification of oocytes useful for fertility preservation for age-related fertility decline and in cancer patients? Fertil. Steril. 99, 1485–1495 (2013).
Chung, K., Donnez, J., Ginsburg, E. & Meirow, D. Emergency IVF versus ovarian tissue cryopreservation: decision making in fertility preservation for female cancer patients. Fertil. Steril. 99, 1534–1542 (2013).
Cobo, A. & Diaz, C. Clinical application of oocyte vitrification: a systematic review and meta-analysis of randomized controlled trials. Fertil. Steril. 96, 277–285 (2011).
Cobo, A., Bellver, J., de los Santos, M. J. & Remohí, J. Viral screening of spent culture media and liquid nitrogen samples of oocytes and embryos from hepatitis B, hepatitis C, and human immunodeficiency virus chronically infected women undergoing in vitro fertilization cycles. Fertil. Steril. 97, 74–78 (2012).
Cobo, A. et al. Storage of human oocytes in the vapor phase of nitrogen. Fertil. Steril. 94, 1903–1907 (2010).
Cobo, A., Remohí, J., Chang, C. C. & Nagy, Z. P. Oocyte cryopreservation for donor egg banking. Reprod. Biomed. Online 23, 341–346 (2011).
Cobo, A., Meseguer, M., Remohí, J. & Pellicer, A. Use of cryo-banked oocytes in an ovum donation programme: a prospective, randomized, controlled, clinical trial. Hum. Reprod. 25, 2239–2246 (2010).
Ubaldi, F. et al. Cumulative ongoing pregnancy rate achieved with oocyte vitrification and cleavage stage transfer without embryo selection in a standard infertility program. Hum. Reprod. 25, 1199–1205 (2010).
Rienzi, L. et al. Consistent and predictable delivery rates after oocyte vitrification: an observational longitudinal cohort multicentric study. Hum. Reprod. 27, 1606–1612 (2012).
Rienzi, L. et al. Embryo development of fresh 'versus' vitrified metaphase II oocytes after ICSI: a prospective randomized sibling-oocyte study. Hum. Reprod. 25, 66–73 (2010).
Noyes, N., Porcu, E. & Borini, A. Over 900 oocyte cryopreservation babies born with no apparent increase in congenital anomalies. Reprod. Biomed. Online 18, 769–776 (2009).
Katayama, K. P., Stehlik, J., Kuwayama, M., Kato, O. & Stehlik, E. High survival rate of vitrified human oocytes results in clinical pregnancy. Fertil. Steril. 80, 223–224 (2003).
Nagy, Z. P. et al. The efficacy and safety of human oocyte vitrification. Semin. Reprod. Med. 27, 450–455 (2009).
Edgar, D. H. & Gook, D. A. A critical appraisal of cryopreservation (slow cooling versus vitrification) of human oocytes and embryos. Hum. Reprod. Update 18, 536–554 (2012).
Kuwayama, M., Vajta, G., Kato, O. & Leibo, S. P. Highly efficient vitrification method for cryopreservation of human oocytes. Reprod. Biomed. Online 11, 300–308 (2005).
Lucena, E. et al. Successful ongoing pregnancies after vitrification of oocytes. Fertil. Steril. 85, 108–111 (2006).
Kim, M. K. et al. Live birth with vitrified-warmed oocytes of a chronic myeloid leukemia patient nine years after allogenic bone marrow transplantation. J. Assist. Reprod. Genet. 28, 1167–1170 (2011).
Garcia-Velasco, J. A. et al. Five years' experience using oocyte vitrification to preserve fertility for medical and nonmedical indications. Fertil. Steril. 99, 1994–1999 (2013).
Vajta, G., Rienzi, L., Cobo, A. & Yovich, J. Embryo culture: can we perform better than nature? Reprod. Biomed. Online 20, 453–469 (2010).
Dittrich, R. et al. Oncofertility: combination of ovarian stimulation with subsequent ovarian tissue extraction on the day of oocyte retrieval. Reprod. Biol. Endocrinol. 11, 1–6 (2013).
Sanchez, M., Novella-Maestre, E., Teruel, J., Ortiz, E. & Pellicer, A. The Valencia programme for fertility preservation. Clin. Transl. Oncol. 10, 433–438 (2008).
Ozkaya, E., San Roman, G. & Oktay, K. Luteal phase GnRHa trigger in random start fertility preservation cycles. J. Assist. Reprod. Genet. 29, 503–505 (2012).
McLaren, J. F. & Bates, G. W. Fertility preservation in women of reproductive age with cancer. Am. J. Obstet. Gynecol. 207; 455–462 (2012).
Sönmezer, M., Türkçüoglu, I., Coskun, U. & Oktay, K. Random-start controlled ovarian hyperstimulation for emergency fertility preservation in letrozole cycles. Fertil. Steril. 95, 2125.e9–11 (2011).
Cakmak, H., Zamah, A. M., Katz, A., Cedars, M. & Rosen, M. P. Effective method for emergency fertility preservation: random-start controlled ovarian hyperstimulation. Fertil. Steril. 98, S170 (2012).
Oktay, K. et al. Letrozole reduces estrogen and gonadotropin exposure in women with breast cancer undergoing ovarian stimulation before chemotherapy. J. Clin. Endocrinol. Metab. 91, 3885–3890 (2006).
Oktay, K., Türkçüoglu, I. & Rodriguez-Wallberg, K. A. GnRH agonist trigger for women with breast cancer undergoing fertility preservation by aromatase inhibitor/FSH stimulation. Reprod. Biomed. Online 20, 783–788 (2010).
Azim, A. A., Costantini-Ferrando, M., Lostritto, K. & Oktay, K. Relative potencies of anastrozole and letrozole to suppress estradiol in breast cancer patients undergoing ovarian stimulation before in vitro fertilization. J. Clin. Endocrinol. Metab. 92, 2197–2200 (2007).
Azim, A. A., Costantini-Ferrando, M. & Oktay, K. Safety of fertility preservation by ovarian stimulation with letrozole and gonadotropins in patients with breast cancer: a prospective controlled study. J. Clin. Oncol. 26, 2630–2635 (2008).
Johnson, L. N. et al. Response to ovarian stimulation in patients facing gonadotoxic therapy. Reprod. Biomed. Online 26, 337–344 (2013).
Engmann, L. et al. The use of gonadotropin-releasing hormone (GnRH) agonist to induce oocyte maturation after cotreatment with GnRH antagonist in high-risk patients undergoing in vitro fertilization prevents the risk of ovarian hyperstimulation syndrome: a prospective randomized controlled study. Fertil. Steril. 89, 84–91 (2008).
Pirard, C., Donnez, J. & Loumaye, E. GnRH agonist as luteal phase support in assisted reproduction technique cycles: results of a pilot study. Hum. Reprod. 2, 1894–1900 (2006).
Friedler, S., Koc, O., Gidoni, Y., Raziel, A. & Ron-El, R. Ovarian response to stimulation for fertility preservation in women with malignant disease: a systematic review and meta-analysis. Fertil Steril. 97, 125–133 (2012).
Waimey, K. E. et al. Future directions in oncofertility and fertility preservation: a report from the 2011 Oncofertility Consortium Conference. J. Adolesc. Young Adult. Oncol. 2, 25–30 (2013).
Poirot, C. J. et al. Feasibility of ovarian tissue cryopreservation for prepubertal females with cancer. Pediatr. Blood Cancer 49, 74–78 (2007).
Martin, J. R. & Patrizio, P. Options for fertility preservation in pediatric populations undergoing cancer chemotherapy. Pediatr. Endocrinol. Rev. 6, 306–314 (2009).
Sauvat, F., Binart, N., Poirot, C. & Sarnacki, S. Preserving fertility in prepubertal children. Horm. Res. 71, 82–86 (2009).
Donnez, J. et al. Live birth after transplantation of frozen-thawed ovarian tissue after bilateral oophorectomy for benign disease. Fertil. Steril. 98, 720–725 (2012).
Oktay, K. et al. Endocrine function and oocyte retrieval after autologous transplantation of ovarian cortical strips to the forearm. JAMA 26, 1490–1493 (2001).
Kim, S. S. Assessment of long term endocrine function after transplantation of frozen-thawed human ovarian tissue to the heterotopic site: 10 year longitudinal follow-up study. J. Assist. Reprod. Genet. 29, 489–493 (2012).
Rodriguez-Wallberg, K. A. & Oktay, K. Fertility preservation and pregnancy in women with and without BRCA mutation-positive breast cancer. Oncologist 17, 1409–1417 (2012).
Stern, C. J. et al. First reported clinical pregnancy following heterotopic grafting of cryopreserved ovarian tissue in a woman after a bilateral oophorectomy. 28, 2996–2999 (2013).
Callejo, J. et al. Live birth in a woman without ovaries after autograft of frozen-thawed ovarian tissue combined with growth factors. J. Ovarian Res. 7, 33 (2013).
Meirow, D., Raanani, H., Brengauz, M. & Dor, J. Results of one center indicate that transplantation of thawed ovarian tissue is effective. Repeated IVF reveals good egg quality and high pregnancy rate. Presented at the 28th meeting of the European Society of Human Reproduction and Embryology, Istanbul, Turkey (2012).
Schmidt, K. L. T. et al. Follow up of ovarian function post chemotherapy following ovarian cryopreservation and transplantation. Hum. Reprod. 20, 3539–3546 (2005).
Dolmans, M. M. et al. IVF outcome in patients with orthotopically transplanted ovarian tissue. Hum. Reprod. 24, 2778–8277 (2009).
Nottola, S. A. et al. Cryopreservation and xenotransplantation of human ovarian tissue: an ultrastructural study. Fertil. Steril. 90, 23–32 (2008).
Van Eyck, A. S. et al. Both host and graft vessels contribute to revascularization of xenografted human ovarian tissue in a murine model. Fertil. Steril. 93, 1676–1685 (2010).
Van Eyck, A. S. et al. Electron paramagnetic resonance as a tool to evaluate human ovarian tissue reoxygenation after xenografting. Fertil. Steril. 92, 374–381 (2009).
Dolmans, M. M. et al. Short-term transplantation of isolated human ovarian follicles and cortical tissue into nude mice. Reproduction. 134, 253–262 (2007).
David, A. et al. Effect of cryopreservation and transplantation on the expression of kit ligand and anti-Müllerian hormone in human ovarian tissue. Hum. Reprod. 27, 1088–1095 (2012).
Amorim, C. A., Curaba, M., Van Langendonckt, A., Dolmans, M. M. & Donnez, J. Vitrification as an alternative means of cryopreserving ovarian tissue. Reprod. Biomed. Online 23, 160–186 (2011).
Amorim, C. A., Van Langendonckt, A., David, A., Dolmans, M. M. & Donnez, J. Survival of human pre-antral follicles after cryopreservation of ovarian tissue, follicular isolation and in vitro culture in a calcium alginate matrix. Hum. Reprod. 24, 92–99 (2009).
Keros, V. et al. Vitrification versus controlled-rate freezing in cryopreservation of human ovarian tissue. Hum. Reprod. 24, 1670–1683 (2009).
Ting, A. Y., Yeoman, R. R., Lawson, M. S. & Zelinski, M. B. In vitro development of secondary follicles from cryopreserved rhesus macaque ovarian tissue after slow-rate freeze or vitrification. Hum. Reprod. 26, 2461–2672 (2011).
Ting, A. Y. et al. Morphological and functional preservation of pre-antral follicles after vitrification of macaque ovarian tissue in a closed system. Hum. Reprod. 28, 1267–1279 (2013).
Amorim, C. A. et al. Successful vitrification and autografting of baboon (Papio anubis) ovarian tissue. Hum. Reprod. 28, 2146–2156 (2013).
David, A., Dolmans, M. M., Van Langendonckt, A., Donnez, J. & Amorim, C. A. Immunohistochemical localization of growth factors after cryopreservation and 3 weeks' xenotransplantation of human ovarian tissue. Fertil. Steril. 95, 1241–1246 (2011).
des Rieux, A. et al. 3D systems delivering VEGF to promote angiogenesis for tissue engineering. J. Control Release 30, 272–278 (2011).
Dath, C. et al. Endothelial cells are essential for ovarian stromal tissue restructuring after xenotransplantation of isolated ovarian stromal cells. Hum. Reprod. 26, 1431–1439 (2011).
Dolmans, M. M., Luyckx, V., Donnez, J., Andersen, C. Y. & Greve, T. Risk of transferring malignant cells with transplanted frozen-thawed ovarian tissue. Fertil. Steril. 99, 1514–1522 (2013).
Dolmans, M. M. et al. Reimplantation of cryopreserved ovarian tissue from patients with acute lymphoblastic leukemia is potentially unsafe. Blood 116, 2908–2914 (2010).
Greve, T. et al. No signs of viable malignant cells in frozen-thawed ovarian cortex intended for fertility preservation from patients with leukaemia. Blood 22, 4311–4316 (2012).
Dolmans, M. M. Safety of ovarian autotransplantation. Blood. 22, 4275–4276 (2012).
Vanacker, J. et al. Transplantation of an alginate-matrigel matrix containing isolated ovarian cells: first step in developing a biodegradable scaffold to transplant isolated preantral follicles and ovarian cells. Biomaterials 33, 6079–6085 (2012).
Meirow, D. et al. Searching for evidence of disease and malignant cell contamination in ovarian tissue stored from hematologic cancer patients. Hum. Reprod. 23, 1007–1013 (2008).
Meirow, D. et al. Ovarian tissue banking in patients with Hodgkin's disease: is it safe? Fertil. Steril. 69, 996–998 (1998).
Kim, S. S. et al. Ovarian tissue harvested from lymphoma patients to preserve fertility may be safe for autotransplantation. Hum. Reprod. 16, 2056–2060 (2001).
Seshadri, T. et al. Lack of evidence of disease contamination in ovarian tissue harvested for cryopreservation from patients with Hodgkin lymphoma and analysis of factors predictive of oocyte yield. Br. J. Cancer 94, 1007–1010 (2006).
Bittinger, S. E. et al. Detection of Hodgkin lymphoma within ovarian tissue. Fertil. Steril. 95, 803 (2011).
Kyono, K. et al. Potential indications for ovarian autotransplantation based on the analysis of 5571 autopsy finding of females under the age of 40 in Japan. Fertil. Steril. 1, 2429–2430 (2010).
Radford, J. A. et al. Orthotopic reimplantation of cryopreserved ovarian cortical strips after high-dose chemotherapy for Hodgkin's lymphoma. Lancet 357, 1172–1175 (2001).
Demeestere, I. et al. Ovarian function and spontaneous pregnancy after combined heterotopic and orthotopic cryopreserved ovarian tissue transplantation in a patient previously treated with bone marrow transplantation: case report. Hum. Reprod. 21, 2010–2014 (2006).
Rosendahl, M. et al. Biochemical pregnancy after fertilization of an oocyte aspirated from a heterotopic autotransplant of cryopreserved ovarian tissue: case report. Hum. Reprod. 21, 2006–2009 (2006).
Demeestere, I., Simon, P., Emiliani, S., Delbaere, A. & Englert, Y. Fertility preservation: successful transplantation of cryopreserved ovarian tissue in a young patient previously treated for Hodgkin's disease. Oncologist 12, 1437–1442 (2007).
Meirow, D. et al. Ovarian tissue cryopreservation in hematologic malignancy: ten years' experience. Leuk. Lymphoma 48, 1569–1576 (2007).
Azem, F. et al. Histologic evaluation of fresh human ovarian tissue before cryopreservation. Int. J. Gynecol. Pathol. 29, 19–23 (2010).
American Cancer Society. Breast Cancer Facts & Figures 2011–2012 [online], (2013).
Perrotin, F. et al. Incidence, diagnosis and prognosis of ovarian metastasis in breast cancer. Gynecol. Obstet. Fertil. 29, 308–315 (2001).
Gagnon, Y. & Têtu, B. Ovarian metastases of breast carcinoma. A clinicopathologic study of 59 cases. Cancer 64, 892–898 (1989).
Li, C. I., Anderson, B. O., Daling, J. R. & Moe, R. E. Trends in incidence rates of invasive lobular and ductal breast carcinoma. JAMA 289, 1421–1424 (2003).
Sánchez-Serrano, M. et al. Malignant cells are not found in ovarian cortex from breast cancer patients undergoing ovarian cortex cryopreservation. Hum. Reprod. 24, 2238–2243 (2009).
Rosendahl, M. et al. Cryopreservation of ovarian tissue for fertility preservation: no evidence of malignant cell contamination in ovarian tissue from patients with breast cancer. Fertil. Steril. 95, 2158–2161 (2011).
Luyckx, V. et al. Is transplantation of cryopreserved ovarian tissue from patients with advanced-stage breast cancer safe? A pilot study. J. Assist. Reprod. Genet. http://dx.doi.org/10.1007/s10815-013-0065-0063.
Nakanishi, T. et al. A comparison of ovarian metastasis between squamous cell carcinoma and adenocarcinoma of the uterine cervix. Gynecol. Oncol. 82, 504–509 (2001).
Pan, Z., Wang, X., Zhang, X., Chen, X. & Xie, X. Retrospective analysis on coexisting ovarian cancer in 976 patients with clinical stage I endometrial carcinoma. J. Obstet. Gynaecol. Res. 37, 352–358 (2011).
Dundar, E. et al. The significance of local cellular immune response of women 50 years of age and younger with endometrial carcinoma. Eur. J. Gynaecol. Oncol. 23, 243–246 (2002).
Oktay, K. Ovarian tissue cryopreservation and transplantation: preliminary findings and implications for cancer patients. Hum. Reprod Update 7, 526–534 (2001).
Ernst, E., Bergholdt, S., Jørgensen, J. S. & Andersen, C. Y. The first woman to give birth to two children following transplantation of frozen/thawed ovarian tissue. Hum. Reprod. 25, 1280–1281 (2010).
Telfer, E. E. & McLaughlin, M. Strategies to support human oocyte development in vitro. Int. J. Dev. Biol. 56, 901–907 (2012).
McLaughlin, M. & Telfer, E. E. Oocyte development in bovine primordial follicles is promoted by activin and FSH within a two-step serum-free culture system. Reproduction 139, 971–978 (2010).
Vanacker, J. et al. Should we isolate human preantral follicles before or after cryopreservation of ovarian tissue? Fertil. Steril. 99, 1363–1368e2 (2013).
Amorim, C. A. et al. Vitrification and xenografting of human ovarian tissue. Fertil. Steril. 98, 1291–1298 (2012).
Johnson, J., Canning, J., Kaneko, T., Pru, J. K. & Tilly, J. L. Germline stem cells and follicular renewal in the postnatal mammalian ovary. Nature 428, 145–150 (2004).
Hayashi, K. et al. Offspring from oocytes derived from in vitro primordial germ cell-like cells in mice. Science 338, 971–975 (2012).
Dunlop, C., Telfer, E. & Anderson, A. Ovarian stem cells—potential roles in infertility treatment and fertility preservation. Maturitas http://dx.doi.org/10.1016/j.maturitas.2013.04.017.
Telfer, E. E. & McLaughlin, M. Natural history of the mammalian oocyte. Reprod. Biomed. Online 15, 288–295 (2007).
Anckaert, E., De Rycke, M. & Smitz, J. Culture of oocytes and risk of imprinting defects. Hum. Reprod. Update 19, 52–66 (2013).
Woods, D. C. & Tilly, J. L. Isolation, characterization and propagation of mitotically active germ cells from adult mouse and human ovaries. Nat. Protoc. 8, 966–988 (2013).
Kalich-Philosoph, L. et al. Cyclophosphamide triggers follicle activation and “burnout”; AS101 prevents follicle loss and preserves fertility. Sci. Transl. Med. 15, 185ra62 (2013).
Morita, Y. et al. Oocyte apoptosis is suppressed by disruption of the acid sphingomyelinase gene or by sphingosine-1-phosphate therapy. Nat. Med. 6, 1109–1114 (2000).
Soleimani, R., Heytens, E. & Oktay, K. Enhancement of neoangiogenesis and follicle survival by sphingosine-1-phosphate in human ovarian tissue xenotransplants. PLoS ONE 6, e19475 (2011).
Tsai, Y. C. et al. Antiapoptotic agent sphingosine-1-phosphate protects vitrified murine ovarian grafts. Reprod. Sci. http://dx.doi.org/10.1177/1933719113493515.
Dolmans, M. M. et al. A review of 15 years of ovarian tissue bank activities. J. Assist. Reprod. Genet. 30, 305–314 (2013).
Author information
Authors and Affiliations
Contributions
Both authors contributed equally to all aspects of the manuscript.
Corresponding author
Ethics declarations
Competing interests
J. Donnez is a board member of PregLem SA and has received payment for lectures and scientific presentations at congresses from Ferring, MSD, Organon and Serono. M.-M. Dolmans declares no competing interests.
Rights and permissions
About this article
Cite this article
Donnez, J., Dolmans, MM. Fertility preservation in women. Nat Rev Endocrinol 9, 735–749 (2013). https://doi.org/10.1038/nrendo.2013.205
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrendo.2013.205
This article is cited by
-
Menstrual blood-derived endometrial stem cell, a unique and promising alternative in the stem cell-based therapy for chemotherapy-induced premature ovarian insufficiency
Stem Cell Research & Therapy (2023)
-
Live birth in woman with premature ovarian insufficiency and 46, XY karyotype after chemotherapy and bone marrow transplant: a case report
BMC Pregnancy and Childbirth (2023)
-
UC-MSCs promote frozen-thawed ovaries angiogenesis via activation of the Wnt/β-catenin pathway in vitro ovarian culture system
Stem Cell Research & Therapy (2022)
-
Synergistic Promoting Effects of X-Linked Inhibitor of Apoptosis Protein and Matrix on the In Vitro Follicular Maturation of Marmoset Follicles
Tissue Engineering and Regenerative Medicine (2022)
-
Comparison between two cryopreservation techniques of human ovarian cortex: morphological aspects and the heat shock response (HSR)
Cell Stress and Chaperones (2022)