Abstract
We describe our experience using two real-time polymerase chain reaction (PCR) assays for detecting the t(14;18)(q32;q21) in a large series of non-Hodgkin's lymphomas (NHLs). These assays utilize the 5′ → 3′ exonuclease activity of Taq polymerase, which cleaves a probe labeled with a fluorescent reporter dye at its 5′ end and a quencher dye at its 3′ end during the extension phase of PCR. In a previous study, Luthra and colleagues developed these real-time PCR assays for detecting the t(14;18) involving the major and minor breakpoint cluster regions of the bcl-2 gene and assessed a small number of NHLs. In this larger study, we analyzed 135 NHLs, 6 Hodgkin's disease, 10 reactive biopsy specimens, and 11 peripheral blood specimens. The NHL group included 46 of 70 (65.7%) follicular NHLs, 1 of 2 (50%) diffuse small cleaved cell NHLs, and 13 of 24 (54.2%) diffuse large B-cell NHLs with the t(14;18) detected by conventional PCR methods. There was excellent agreement between the real-time and conventional PCR assays with overall concordance in 160 of 162 (98.8%) specimens. For the NHLs, concordance was found in 134 of 135 (99.3%) specimens. Disagreement was observed in one case of follicular NHL in which the real-time PCR assay detected bcl-2 minor breakpoint cluster region/JH DNA fusion sequences and the conventional method was negative. The overall concordance for 10 benign biopsy specimens and 11 normal peripheral blood samples was 20 of 21 (95.2%). One lymph node biopsy specimen that showed reactive follicular hyperplasia was positive for the bcl-2 minor breakpoint cluster region/JH DNA fusion sequences detected by the real-time PCR assay but was negative by conventional PCR methods. This patient had no clinical evidence of NHL. We conclude that real-time PCR assays for detecting the t(14;18) are sensitive, specific, and more convenient than conventional PCR methods.
Similar content being viewed by others
INTRODUCTION
Follicular lymphoma is the most common type of non-Hodgkin's lymphoma (NHL) in the United States (1). Up to 90% of follicular lymphomas carry a reciprocal balanced chromosomal translocation, the t(14;18)(q32;q21), involving the bcl-2 gene on chromosome 18q21 and the immunoglobulin heavy chain gene in 14q32. The majority of the breakpoints on chromosome 18 are tightly clustered in two regions: the major (MBR) and minor (MCR) breakpoint cluster regions (2, 3, 4, 5, 6). The clustering of these breakpoints makes these regions amenable to PCR analysis and has led to development of highly sensitive PCR assays to detect the t(14;18) (7, 8, 9).
Real-time PCR assays that utilize the 5′ → 3′ exonuclease activity of Taq polymerase haved been developed (10, 11, 12). In these assays, a nonextendable oligonucleotide probe is designed to anneal downstream to one of the PCR primers and is labeled with a fluorescent reporter dye at its 5′ end and a quencher dye at its 3′ end. During the extension phase of PCR, the 5′ → 3′ exonuclease activity of Taq polymerase cleaves the reporter dye from the probe, resulting in an increase of fluorescence. This fluorescence can be conveniently detected and quantified using automated methods (10, 13, 14, 15, 16).
In a preliminary study, Luthra and colleagues (10) developed two novel 5′ → 3′ exonuclease-based real-time PCR assays for detecting the t(14;18) involving the bcl-2 MBR and MCR and assessed 38 NHLs. In this study, we expanded these results by using these real-time PCR assays to assess a large number of NHLs and benign lesions. Our results confirm that these real-time PCR assays for detecting the t(14;18) are equivalent to conventional PCR assays. Furthermore, these real-time PCR assays yield results immediately after amplification, do not require standard post-PCR product detection steps, and therefore are more convenient than conventional PCR assays.
MATERIALS AND METHODS
We analyzed a total of 162 specimens for the presence of the t(14;18)(q32;q21). The specimens were collected from a variety of sites: 104 lymph node, 45 extranodal, 3 bone marrow aspiration, and 11 normal (patients without a history of lymphoma) peripheral blood specimens. High molecular weight DNA was isolated using standard proteinase K digestion and organic extraction procedures.
Conventional PCR
Conventional PCR methods for detecting the t(14;18) involving the bcl-2 MBR and MCR have been described previously (10). The PCR was performed in a model 9600 thermal cycler (PE Applied Biosystems, Foster City, CA). Coamplification of β-globin was performed to prove the presence of amplifiable DNA in the specimens.
The reaction mixture contained 500 ng genomic DNA in 50 μl volume and was subjected to 40 PCR cycles as follows: 94° C for 30 seconds (denaturation), 54° C for 30 seconds (annealing), and 72° C for 1 min (extension). The primers used are shown in Table 1. The amplified products were electrophoresed in 2% agarose gels, transferred by Southern blotting to nylon membranes, and hybridized with 32P-labeled probes specific for either the MBR or the MCR regions of the bcl-2 gene. Positive and negative controls were included in each test run.
Real-Time PCR
The 5′ → 3′ exonuclease-based real-time PCR methods used in this study were described previously (10). The assays were performed in a PRISM 7700 Sequence Detector (PE Applied Biosystems) equipped with a 96-well thermal cycler in the presence of 0.15 μmol/L bcl-2 MBR- or MCR-specific oligonucleotide probes. The probes were labeled with 6-carboxy fluorescein (FAM) at their 5′ end and 6-carboxy-tetramethyl rhodamine (TAMRA) at their 3′ end.
PCR was carried out in a 50 μl volume containing 500 ng genomic DNA, 1 × Taqman buffer, 4.4 mmol/L MgCl2, 400 μmol/L dUTP, 200 μmol/L dATP, 200 μmol/L dCTP, 200 μmol/L dGTP, 0.125 μmol/L of each primer, 0.5 U AmpErase uracil-N-glycosylase, and 1.25 U AmpliTaq Gold. β-actin was coamplified using 0.03 μmol/L of the appropriate primers (Table 1) and 0.12 μmol/L of fluorescently labeled β-actin–specific probe. A fluorescent dye, 6-carboxy-X-rhodamine, was included in the Taqman buffer to serve as an internal reference. The DNA was denatured for 10 min at 95° C and subjected to 40 cycles of a two-step PCR protocol: 95° C for 15 seconds (denaturation) followed by 60° C for 1 min (combined annealing/extension). The fluorescence emission data for each sample was analyzed immediately after PCR was completed. Positive and negative controls were included in each test run (Fig. 1).
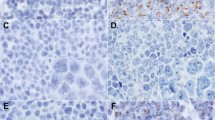
A, follicular lymphoma, Grade 2, in which conventional and real-time polymerase chain reaction (PCR) methods amplified bcl-2 major breakpoint cluster region/JH DNA fusion sequences (hematoxylin-eosin, 2×). B, PCR products (in duplicate) generated using conventional methods are shown on ethidium bromide–stained gel (below). The products are also shown after transfer to a nylon membrane by Southern blotting and hybridization with a specific bcl-2 major breakpoint cluster region internal probe (above). P1, follicular lymphoma shown in A positive for the t(14;18); P2, t(14;18)-negative lymphoma. Positive and negative controls are indicated with plus and minus signs. Molecular size markers in base pairs are listed to the left. C, real-time PCR assay results (in duplicate) as shown by amplification plots of the t(14;18)-positive follicular lymphoma shown in A (green). Positive (red) and negative (blue) controls are also shown. The plots are generated from the fluorescence emission data collected during the extension phase of each PCR cycle.
Collection and Analysis of Fluorescence Emission Data
The increase in fluorescence signal in each of the 96 wells was monitored in real-time during PCR using the PRISM 7700 Sequence Detector equipped with a charged coupled device camera. The online software system analyzes the spectral data collected during the extension phase of each cycle and plots fluorescence intensity versus cycle number. The fluorescence data are expressed as Rn or ΔRn. Rn, the normalized reporter signal, is the fluorescence signal of the reporter dye divided by the fluorescence signal of the passive, internal reference dye. ΔRn is Rn minus the baseline signal established in the first few cycles of PCR. Normalization corrects for fluorescence fluctuations resulting from changes in volume or pipetting errors.
Sensitivity
Two cell lines, LR and DS, derived from different cases of follicular lymphoma known to carry the t(14;18) involving the bcl-2 MBR (gifts from Dr. Richard J. Ford), were amplified in duplicate using the real-time PCR assay described above. 500 ng cell line DNA from approximately 60,000 to 80,000 cells was serially diluted with normal DNA to achieve 10−1- to 10−5-fold dilutions. Thus, the 10−5-fold dilution contained approximately 0.6 to 0.8 genomes. A standard curve showing the threshold cycle (cycle number) at which an increase in the positive fluorescence signal initially occurred was plotted against the amount of target in each dilution.
RESULTS
There was overall concordance between the real-time and conventional PCR assays in 160 of 162 (98.8%) specimens analyzed. The study included 126 B-cell NHLs, 9 T-cell NHLs, and 6 cases of Hodgkin's disease (Table 2). We also assessed 10 biopsy specimens with reactive lymphoid hyperplasia and 11 normal donor peripheral blood specimens.
Non-Hodgkin's Lymphomas and Hodgkin's Disease
For the NHL, concordance was observed in 134 of 135 (99.3%) specimens. Seventy cases of follicular lymphoma were assessed, 34 Grade 1 (predominantly small cleaved), 19 Grade 2 (mixed small cleaved and large), and 17 Grade 3 (predominantly large cell). The overall concordance between the real-time and conventional PCR assays for the follicular lymphomas was 69 of 70 (98.6%) (Fig. 1). The discrepancy occurred in one case of Grade 2 follicular lymphoma in which bcl-2 MCR/JH DNA fusion sequences were detected by the real-time PCR assay but not by the conventional method.
Among the group of follicular lymphomas, the t(14;18) was detected by either conventional or real-time PCR methods in each histologic grade as follows: 25 of 34 (73.5%) Grade 1, 14 of 19 (73.7%) Grade 2, and 8 of 17 (47.1%) Grade 3. The lower detection rate for Grade 3 neoplasms has been reported by others (8).
For the diffuse NHL, there was complete agreement between the real-time and conventional PCR assays. The t(14;18) was detected in 1 of 2 (50%) cases of diffuse small cleaved cell lymphoma, 5 of 7 (71.4%) diffuse large B-cell lymphomas in patients who had a history of follicular lymphoma, and 8 of 17 (47.1%) cases of diffuse large B-cell lymphoma in patients who did not have a known history of follicular lymphoma. All other diffuse NHLs were negative for the t(14;18), including 9 marginal zone B-cell lymphomas (4 mucosa-associated lymphoid tissue type, 2 nodal, and 3 splenic), 14 cases of small lymphocytic lymphoma/chronic lymphocytic leukemia, 6 mantle cell lymphomas, 9 T-cell lymphoma specimens (6 mycosis fungoides, 2 anaplastic large cell lymphoma, 1 lymphoblastic), and 1 hairy cell leukemia.
Six cases of Hodgkin's disease, all nodular sclerosis type, were analyzed. Each case was negative for the t(14;18) using both real-time and conventional PCR methods.
Reactive Lesion and Normal Peripheral Blood Specimens
The concordance for the 10 cases of reactive follicular hyperplasia was 9 of 10 (90%). In one case, bcl-2 MCR/JH DNA fusion sequences that were not detected by the conventional PCR method were detected using the real-time PCR assay. This case was a small occipital lymph node, 0.5 cm. The patient had a history of recent viral infection without clinical evidence of malignant lymphoma, either at time of diagnosis or 6 months later.
All 11 normal peripheral blood samples from patients who did not have a history of malignant lymphoma were negative for the t(14;18) assessed using both real-time and conventional PCR assays.
Cell Line Studies
The real-time bcl-2 MBR/JH PCR assay was performed in duplicate using serially diluted DNA derived from two cell lines carrying the t(14;18) involving the bcl-2 MBR region. Using the LR cell line, bcl-2 MBR/JH DNA fusion sequences were detected in all dilutions including the 10−5 dilution sample, estimated to contain 0.6 to 0.8 genomes (Fig. 2A). However, using the DS cell line, bcl-2 MBR/JH DNA fusion sequences could be detected consistently only in 10−4 dilutions, estimated to contain 6 to 8 genomes.
Detection sensitivity of 5′ → 3′ exonuclease-based real-time polymerase chain reaction (PCR) assay for t(14;18). Genomic DNA (500 ng) was isolated from two cell lines (LR and DS) carrying the t(14;18) involving the bcl-2 major breakpoint cluster region and serially diluted with DNA from non-neoplastic tissue to obtain the final DNA quantity indicated. These dilutions were then analyzed using the real-time PCR method. A, amplification plots showing the fluorescence increase on log scale. The red and blue colors distinguish the amplification cycles of the two cell lines at different dilutions. The threshold cycle is the cycle at which the fluorescence signal increases above the base line. B, standard curve generated from the LR cell line showing a linear correlation between the DNA quantity (x axis) and the threshold cycle (y axis).
The cycle number at which the initial fluorescence signal was detected was inversely proportional to the quantity of target DNA present in the reaction mix. A standard curve generated from the amplification plots of both cell lines is shown in Figure 2B. This curve shows a linear correlation between the threshold cycle and serial dilutions of a t(14;18) bcl-2 MBR-positive cell line. The x axis shows the target DNA quantity of the sample. The y axis shows the threshold cycle at which a logarithmic increase in fluorescence was first detected. Correlation of the x and y axes of this cell line standard curve allows more accurate estimate of the target DNA quantity in test samples with unknown amounts of target DNA.
DISCUSSION
Detection of the t(14;18)(q32;q21) has become an important tool in the diagnosis of follicular lymphomas (2, 3, 4, 5, 6). Several methods to detect the t(14;18) are available, including PCR, restriction fragment analysis, and cytogenetics. Although the last two techniques are sensitive and specific, they are more labor intensive and time consuming. As PCR methods are faster and less labor intensive, they often are used as an initial step for the detection of the t(14;18).
The sensitivity of these 5′ → 3′ exonuclease-based real-time t(14;18) PCR assays was determined in a previous study using a cell line known to carry JH/bcl-2 MCR DNA fusion sequences (10). In this study, the sensitivity of these real-time PCR assays was reevaluated by studying two additional cell lines known to carry the t(14;18) involving the bcl-2 MBR. These cell lines were serially diluted with non-neoplastic DNA to attain 10−1- to 10−5-fold dilutions. As observed in a previous study (10), real-time PCR methods are able to detect bcl-2 MBR/JH DNA fusion sequences in the samples diluted up to 10−5. However, bcl-2 MBR/JH fusion sequences were inconsistently detected in samples with 10−5 dilutions estimated to have 0.6 to 0.8 genomes. This result may be attributed to low DNA copy number, the Poisson effect, or possibly the PCR conditions in our assay, such as the number of cycles. Other reports using real-time PCR methods show similar inconsistent detection of target DNA when analyzing samples with low DNA copy number, ranging from 1 to 5 copies (10, 17). With these real-time PCR assays, we were able to detect bcl-2 MBR/JH or bcl-2 MCR/JH DNA fusion sequences consistently in samples containing at least 6 to 8 copies of target DNA.
More accurate estimates of target DNA quantity in patient samples can be determined by comparison with standard curves generated from serial dilutions of t(14;18)-positive cell lines. As illustrated in the standard curves in Figure 2B, the threshold cycle of each cell line did not vary by more than 0.8 cycles, indicating that the use of cell lines with known target chromosomal translocations can be used as a control for quantitative studies. This mild variation between cell lines may be attributable to variations in pipetting and dilution. The threshold cycles generated with the undiluted samples (500 ng target DNA) showed a minimal difference in threshold cycle number, 0.07. This suggests that one does not need to clone t(14;18) fusion sequences from every patient who has a t(14;18)-positive NHL to determine the quantity of minimal residual disease. Comparison with standard curves generated from a cell line is probably adequate.
The high overall concordance rate in this study between the two assays for analyzing cases of NHL, Hodgkin's disease, and reactive lymphoid hyperplasia indicates that the sensitivity and specificity of real-time PCR assays for detecting the t(14;18) are comparable to conventional PCR methods.
Only two cases (<2%) in this study yielded discordant results. In one case of follicular lymphoma, bcl-2 MCR/JH DNA fusion sequences were detected using the real-time PCR assay but not using the conventional method. Repeat analysis yielded identical results. The amount of DNA was insufficient for restriction fragment analysis. The second discrepancy was a case of follicular hyperplasia involving a 0.5-cm lymph node from a 22-year-old woman who had recurrent viral infections and peripheral lymphadenopathy. Bcl-2 MCR/JH DNA fusion sequences were detected only by the real-time PCR assay. We reviewed the slide of this biopsy specimen and reconfirmed the benign diagnosis. Clinical follow-up of this patient, for 6 months, has shown no clinical evidence of malignant lymphoma. Thus, this case may be an example of reactive follicular hyperplasia with the t(14;18), as has been described by others (18, 19, 20). However, the possibility of incipient malignant lymphoma cannot be excluded.
In summary, we have shown in this study that these real-time PCR assays to detect the t(14;18) involving the bcl-2 MBR or MCR are equivalent to conventional PCR methods. The 5′ → 3′ exonuclease-based real-time PCR assays are advantageous because they eliminate the need for radioactive materials used for product detection, as well as labor-intensive post-PCR detection steps. These real-time PCR assays yield results as soon as PCR is completed (within 2 hours) allowing rapid triage of the patient to different treatment protocols. Rough estimation of target DNA quantity, as demonstrated in our experiments using serial dilutions of cell lines, is also applicable and achieved through analysis of standard curves. If desired, real-time PCR amplified products may be electrophoresed or sequenced.
References
Jones ES, Fuks Z, Bull M, Kadin ME, Dorfman RF, Kaplan HS, et al. Non-Hodgkin's lymphomas: IV. Clinicopathologic correlation in 405 cases. Cancer 1973; 31: 806–23.
Tsujimoto Y, Cossman J, Jaffe E, Croce C . Involvement of the bcl-2 gene in human follicular lymphoma. Science 1985; 228: 1440–3.
Fukuhara S, Rowley JD, Variakojis D, Golomb HM . Chromosome abnormalities in poorly differentiated lymphocytic lymphoma. Cancer Res 1979; 39: 3119–29.
Yunis JJ, Oken MM, Theologides A, Howe RB, Kaplan ME . Recurrent chromosomal defects are found in most patients with non-Hodgkin's lymphoma. Cancer Genet Cytogenet 1984; 13: 17–28.
Ong ST, LeBeau MM . Chromosomal abnormalities and molecular genetics of non-Hodgkin's lymphoma. Semin Oncol 1998; 25: 447–60.
Wang J, Raffeld M, Medeiros LJ, Longo DL, Jaffe ES, Duffey D, et al. Follicular center cell lymphoma with the t(14;18) translocation in which the rearranged bcl-2 gene is silent. Leukemia 1993; 7: 1834–9.
Bakhashi A, Jensen JP, Goldman P, Wright JJ, McBride CW, Epstein AL, et al. Cloning of the chromosomal breakpoint of t(14;18) human lymphoma clustering around the JH on chromosome 14 and near a transcriptional unit on 18. Cell 1985; 41: 899–906.
Klefstrom J, Franssila K, Peltomaki P, Kaatinen M, Solin ML, Kniuultila S . Major and minor breakpoint sites of chromosomal translocation t(14;18) in subtypes of non-Hodgkin's lymphoma. Leuk Res 1994; 18: 245–50.
Lee KA, Goepel JR, Winfield DA, Hancock BW, Goynes MH . Investigation of bcl-2 gene rearrangements in a United Kingdom series of low and high grade non-Hodgkin's lymphoma. Leuk Lymphoma 1993; 11: 91–8.
Luthra R, McBride JA, Cabanillas F, Sarris A . Novel 5′ exonuclease-based PCR assay for the detection of the t(14;18)(q32;q21) in patients with follicular lymphoma. Am J Pathol 1998; 141: 291–9.
Holland PM, Abramson RD, Watson R, Gelfand DH . Detection of specific polymerase chain reaction product by utilizing the 5′-3′ exonuclease activity of the thermus aquaticus DNA polymerase. Proc Natl Acad Sci U S A 1991; 88: 7276–80.
Livak KJ, Flood SJA, Marmaro J, Giusti W, Deetz K . Oligonucleotide with fluorescent dyes at the opposite ends provide a quenched probe system useful for detecting PCR products and nucleic acid hybridization. PCR Methods Appl 1995; 4: 357–62.
Higuchi R, Dollinger G, Walsh P, Griffith R . Simultaneous amplification and detection of specific DNA sequences. Biotechnology 1993; 10: 413–7.
Higuchi R, Fockler C, Watson R . Kinetic PCR: real-time monitoring of DNA amplification reactions. Biotechnology 1993; 11: 1026–30.
Heid CA, Stevens J, Livak KJ, Williams PM . Real-time quantitative PCR. Genome Res 1996; 6: 986–94.
Gibson UEM, Heid CA, Williams PM . A novel method for real-time quantitative RT-PCR. Genome Res 1996; 6: 995–1001.
Dolken L, Schuler F, Dolken G . Quantitative detection of t(14;18)-positive cells by real-time quantitative PCR using fluorogenic probes. Biotechniques 1998; 25: 1058–64.
Limpens J, de Jong D, Van Krieken JHJM, Price CGA, Young DB, Van Ommen GJB, et al. Bcl-2/JH rearrangements in benign lymphoid tissues with follicular hyperplasia. Oncogene 1991; 6: 2271–6.
Ji W, Qu G, Ye P, Zhang X, Halabi S, Erlich M . Frequent detection of bcl-2/JH translocation in human blood and organ samples by a quantitative polymerase chain reaction assay. Cancer Res 1995; 55: 2876–82.
Bruckheimer EM, Cho SH, Sarkiss M, Hermann J, McDonnell TJ . The bcl-2 gene family and apoptosis. Adv Biochem Eng Biotechnol 1998; 62: 75–105.
Acknowledgements
The authors thank Richard J. Ford, M.D., Ph.D., for donating the LR and DS t(14;18)-positive cell lines. We also thank Seema Hai for technical assistance and Danielle Evans and Yolanda Newman for typing the manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Estalilla, O., Medeiros, L., Manning, J. et al. 5′ → 3′ Exonuclease-Based Real-Time PCR Assays for Detecting the t(14;18)(q32;21): A Survey of 162 Malignant Lymphomas and Reactive Specimens. Mod Pathol 13, 661–666 (2000). https://doi.org/10.1038/modpathol.3880116
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3880116
Keywords
This article is cited by
-
Long-term safety and outcome of fludarabine, cyclophosphamide and mitoxantrone (FCM) regimen in previously untreated patients with advanced follicular lymphoma: 12 years follow-up of a phase 2 trial
Annals of Hematology (2017)
-
A nanostructured genosensor for the early diagnosis of systemic arterial hypertension
Biomedical Microdevices (2015)
-
Detection of minimal residual disease in hematologic malignancies by real-time quantitative PCR: principles, approaches, and laboratory aspects
Leukemia (2003)
-
Real-Time t(14;18)(q32;q21) PCR Assay Combined with High-Resolution Capillary Electrophoresis: A Novel and Rapid Approach that Allows Accurate Quantitation and Size Determination of bcl-2/JH Fusion Sequences
Modern Pathology (2002)
-
Detection of bcl-2/IgH Rearrangements by Quantitative-competitive PCR and Capillary Electrophoresis
Molecular Diagnosis (2001)