Abstract
Human papillomavirus (HPV) infection is etiologically associated with low- (LSIL) and high-grade squamous intraepithelial lesions (HSIL) and with cervical cancer. The progression or regression of the lesions may depend, among other factors, on the host heritable immune response. Because human leukocyte antigen (HLA)-G molecules are involved in the modulation of innate and adaptive immune responses, and because no previous studies have evaluated HLA-G polymorphism in patients with SIL, we conducted a study to assess the association between HLA-G polymorphisms and cervical lesions harboring HPV infection. Cervico-vaginal scrapings and blood samples were collected from 125 women with SIL (68 LSIL and 57 HSIL) and from 94 healthy women without HPV infection and cytological abnormalities. HPV type and HLA-G polymorphisms in exons 2, 3 and 8 (14 bp insertion/deletion) were evaluated by PCR methodology, and digested with restriction endonucleases. The Genepop software and the EM and PHASE algorithms were used for statistical analysis. A significant protective association was observed between the presence of the G*0103 allele and SIL and between the G0101/G0104 genotype and HSIL in the group of patients compared to control. The presence of the G0104/+14 bp and G0104/−14 bp haplotypes conferred susceptibility to SIL compared to control. In addition, patients possessing the G0104/+14 bp haplotype and harboring HPV-16 and -18 co-infections were particularly associated with HSIL. These findings suggest that HLA-G polymorphisms may be associated with HPV infection and SIL, consequently representing a profile of predisposition to cervical cancer.
Similar content being viewed by others
Main
Human papillomavirus (HPV) infects the mucosal and cutaneous epithelium causing benign warts and genital lesions. Low-risk HPV types are associated with the development of genital warts, and high-risk types such as HPV-16 and HPV-18 are associated with the development of low- and high-grade squamous intraepithelial lesions (LSIL and HSIL) and cervical cancer.1 Although HPV infection is eliminated in 70–90% of cases, infected cells may develop mechanisms to escape from the immune response,2 leading to persistent HPV infection and oncogenic transformation.3
The human major histocompatibility complex (MHC), known in humans as the human leukocyte antigen (HLA) system, is a highly polymorphic genomic region located on the 6p21.3 chromosome. Several functionally different MHC genes/molecules have been described such as classical HLA class Ia (HLA-A, B, C), nonclassical HLA class Ib (HLA-E, -F, -G), classical HLA class II (HLA-DR, DQ, DP) and class III (complement system components and tumor necrosis factors, among others). The major function of classical HLA class Ia and class II molecules is antigen presentation to T CD8+ and T CD4+ cells, respectively, whereas nonclassical class Ib molecules are involved in the regulation of the immune response through interaction with surface receptors on natural killer (NK), T and antigen-presenting cells.4 Several lines of evidence support the involvement of classical HLA molecules in the development of HPV-related cervical cancer. Some viral proteins, including the E7 protein of HPV-16 and HPV-18, may downregulate the cell-surface expression of classical HLA class I antigens,5 allowing infected cells to escape from T CD8+ cytolytic cell killing. However, the lack of HLA classical class I expression may expose an infected cell to the attack of NK cells. On the other hand, the lytic action of NK may be regulated by the interaction of the specific NK immunoglobulin-like receptor (KIR) with class I HLA-C, -G and -E molecules.6
HLA-G has a restricted distribution on normal tissue cells, being primarily expressed in the thymus, pancreas and intestines. HLA-G is also abundantly expressed in placental tissue, particularly in the extravillous cytotrophoblast,7 being implicated in the inhibition of the cytotoxic function of maternal NK cells.8 The HLA-G gene generates multiple protein isoforms by alternative splicing of a single mRNA, giving rise to four membrane-bound isoforms (HLA-G1mb to -G4mb), and three soluble isoforms (HLA-G5s to -G7s) generated by the presence of a stop codon in intron 4.9 HLA-G transcripts are also expressed at low levels in a variety of normal human adult tissues;10 however, normal cervical cells do not express HLA-G.11 HLA-G expression may be upregulated in inflammatory and neoplastic tissues,12 and in viral infections.13, 14, 15 The membrane-bound variant HLA-G1 suppresses the proliferation of T CD4+ cells, and the soluble variant HLA-G5 may induce apoptosis of activated T CD8+ cells.16, 17 Several polymorphic sites have been described for the HLA-G locus. Nucleotide substitutions mainly in exons 2, 3 and 4 may discriminate 42 confirmed alleles clustered into nine distinct allele groups, and generating only 15 different proteins due to the presence of several synonymous substitutions among HLA-G alleles (Anthony Nolan Research Institute, February 2009).18 HLA-G alleles may influence the plasma levels of soluble HLA-G (sHLA-G).19 In addition, a 14 bp insertion/deletion polymorphism has been reported in the 3′-untranslated region (UTR) of exon 8.20 HLA-G alleles exhibiting the 14 bp insertion (+14 bp) undergo an alternative splicing that removes 92 bases from 3′ UTR,21 influencing the stability of HLA-G mRNA.22 Although removal of the 92 bases produces a more stable mRNA, the presence of +14 bp has been associated with a lower mRNA production.20
Some virus including Epstein–Barr virus, rabies virus and cytomegalovirus may upregulate HLA-G expression;13, 23, 24, 25 however, the function of HPV in HLA-G expression has not been determined. Recently, we reported that cervical lesions may express HLA-G molecules that may differ according to the severity of SIL in HPV-infected women. As the cervical lesion progressed from low to high grade, a decreased expression of HLA-G was observed.11 Whether the expression of HLA-G may depend on HPV type, genetic background of patients or both is a question that has not been elucidated. In the present study we evaluated the polymorphism of the HLA-G locus, including the 14 bp insertion/deletion in exon 8, in patients harboring HPV infection, stratified according to the lesion severity and the presence of the most common oncogenic HPV types, ie, HPV-16 and -18.
Patients and methods
Study Design and Subjects
A total of 219 sexually active women were studied: 125 of them presented a cytological and colposcopic suspicion of HPV infection (patient group), and 94 had no cytological and/or colposcopic abnormalities (control group). Patients and controls were aged 15–71 years (median=31.07±10.9 and 34.05±15.1, respectively), and were from the same geographic area, presumably presenting similar ethnic backgrounds. Although individuals that compose the Brazilian population are highly admixed, both patients (78.2%) and controls (82%) were primarily of European ancestry. Patients underwent routine gynecological examination at the Division of Infectious Diseases of the Department of Gynecology and Obstetrics, University Hospital, School of Medicine of Ribeirão Preto, University of São Paulo, Brazil. The local and the Brazilian Institutional Ethics Committees on human experimentation approved the study (protocols 1635/2002 and 885/2002, respectively). All patients gave written informed consent to participate in the study.
Sample Collection
Patients and controls were submitted to peripheral blood withdrawal and cervical scraping at the time of the medical visit. Because 10–30% of normal women may harbor HPV and do not exhibit SIL, and because this group may exhibit a transient infection, which may evolve to virus elimination or virus persistency (SIL), only those with no previous history of infectious diseases, without colposcopic or cytological abnormalities and exhibiting no DNA HPV detection were selected to form the control group. Patients were also submitted to cervical biopsies whenever indicated. Tissues were sectioned and evaluated histologically after staining with hematoxylin and eosin, and two experienced histopathologists determined the lesion stage in a double-blind protocol.
To obtain DNA for HPV detection and typing, cervico-vaginal scrapings were collected with appropriate brushes and placed in microtubes containing the following buffer: 0.01 M Tris/HCL (pH 7.6), 5 mM MgCl2 and 1% Triton X-100. DNA was extracted from peripheral blood and cervical scrapings as previously described.26
According to the results of cervical cytology, biopsy and DNA HPV detection, patients were stratified into two subgroups: 68 women with LSIL (cervical intraepithelial lesion grade I) and 57 with HSIL (cervical intraepithelial lesion grades II and III).
HPV Detection and Typing
MY09 and MY11 primers,27 which amplify a 450 bp DNA fragment, were used for generic HPV amplification. Because HPV-16 and -18 are the most frequent types associated with SIL and invasive cervical lesions in Brazil,28, 29, 30 attention was focused on them, using previously described specific primers and conditions.31 The absence of amplification by HPV-16 or -18 primers but the presence of amplification by the MY09 and MY11 primers did not exclude the presence of other HPV types, which in this study were designated as HPVX. All reactions were performed using positive controls for HPV-16 (SiHa cell line) and HPV-18 (HeLa cell line) detection and controls for contamination.
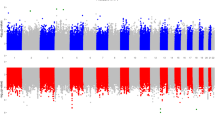
HLA-G Typing
HLA-G polymorphism was defined by nucleotide sequence variations in exons 2 and 3. DNA amplification for HLA-G typing was carried out using previously described specific primers and cycling conditions.32 Amplified DNA products were then digested with the restriction endonucleases HinfI, HaeIII, MspI, Bsp1286I, BsrBI for exon 2, and BseGI, HgaI, Cfr13I for exon 3 (Fermentas Life Science, Burlington, Canada) according to the manufacturer's instructions. The cleavage products were submitted to 7% polyacrylamide gel electrophoresis and stained with silver nitrate.33 The restriction fragment length polymorphism band pattern was used to define allele groups or specific alleles. Because most of the HLA-G alleles currently identified have synonymous substitutions, generating only nine different proteins when considering amino-acid sequences, and several of these groups are rare in the Brazilian population,34 we primarily used allele groups, as described in Table 1, to correlate with SIL severity.
HLA-G 14 bp Polymorphism in Exon 8 (3′ UTR)
The HLA-G 14 bp polymorphism was typed as previously described.35 The amplified products were visualized by electrophoresis on 4% Nusieve GTG agarose gel (Sigma, Saint Louis, MO, USA) stained with ethidium bromide (Sigma).
Statistical Analysis
The Genepop 3.4 software 36 was used to compare the frequencies of HLA-G allele groups. The associations between HLA-G polymorphisms among patients and controls, and among patients stratified according to lesion severity, HPV type or both, were evaluated by the two-sided Fisher's exact test and the odds ratio (OR), using the GraphPad InStat 3 software.37 P-values were considered to be significant when ≤0.05.
The EM and PHASE algorithms 38, 39 were used to determine HLA-G allele groups/14 bp polymorphism haplotypes. The Hardy–Weinberg equilibrium expectations were evaluated using the Genepop 3.4 software.36
Results
HPV Detection
All samples obtained from the patient group presenting a cytological and colposcopic suspicion of HPV infection were positive for HPV DNA by generic HPV amplification, and the samples obtained from the control group presented negative results for HPV DNA. The frequency (%) of HPV types in patients with LSIL and HSIL is described in Table 2.
HLA-G Alleles and the 14 bp Insertion/Deletion in Exon 8
The HLA-G genotypes did not fit the expected Hardy–Weinberg proportions in either the patient or control group (P=0.0040±0.0003 and 0.0000±0.0000, respectively), exhibiting heterozygote deficiency. The individuals included in the two groups were from different localities in São Paulo state, thus not representing a sample of a Mendelian population, a fact that may inflate the genetic diversity (expected heterozygosity) and lead to heterozygosis deficiency. However, the 14 bp genotypes fit the Hardy–Weinberg expectations (P=0.1223±0.0015 and 0.1667±0.0012, respectively).
Four (G0101, G0103, G0104 and G0105N) of the five allelic groups evaluated in this study were observed. The G*0102 allele, known to be absent in the Brazilian population,34 was not identified in this series of Brazilian subjects, Tables 3 and 4 show the frequency of the HLA-G allele groups and HPV genotypes observed in patients and controls. Table 5 illustrates the frequencies of HLA-G/14 bp haplotypes in patients and controls.
HLA-G in Patients and Controls
Considering the patient group irrespective of lesion severity and HPV type, the G*0103 allele was absent, being observed only in the control group (4.3%; Table 3). When patients and controls were compared, the G*0103 allele was found to be associated with protection against the occurrence of HPV lesions (P=0.0010). The same protective effect was observed when we compared the presence of the G*0103/G*0103 genotype (Table 4). However, this was probably a ‘hitch-hiking’ effect of the above association, as all G*0103 individuals were homozygous for the allele (as confirmed by sequencing analysis). In addition, the G*0103/+14 bp haplotype was also shown to be protective (Table 5), although this is also the same effect of the G*0103 allele because this allele is known to be always associated with the presence of the 14 bp sequence in the Brazilian population.34
No significant results were observed when patients and controls were compared solely in terms of the presence or absence of the 14 bp polymorphism.
HLA-G in Patients Stratified according to Lesion Severity
The G0101/G0104 genotype was shown to be protective in patients presenting high-grade lesions when compared to LSIL patients, although with a borderline probability (OR=0.2593, 95% CI=0.06929–0.9701; P=0.0510). When the HSIL group was compared to control, the same influence was found (OR=0.2135, 95% CI=0.06008–0.7584; P=0.0094), indicating that the G0101/G0104 genotype may influence the susceptibility to high-grade lesions (Table 4).
HLA-G in Patients Stratified according to Lesion Severity and HPV Type
Compared with controls, the G0104/−14 bp haplotype was associated with low-grade lesions in women harboring HPVX (OR=3.601, 95% CI=1.080–12.012; P=0.0445); however, no association was found when the XHSIL and XLSIL groups and the G0104 allele group itself were compared. The rare haplotype G0104/+14 bp34 was only present in women with high-grade lesions harboring both HPV-16/18 infections (OR=34.697, 95% CI=1.594–755.46; P=0.0177) (Table 5); however, no association was found when LSIL 16/18 and HSIL 16/18 were compared.
Discussion
Several reports have evaluated HLA-G expression in fully developed cancer cells;40 however, few studies have evaluated the expression of HLA-G in SIL or cervical cancer.41, 42, 43 Polakova and Russ43 studied different tumor cell types and observed no HLA-G expression on cervical cancer cells. Yoon et al41 reported that high HLA-G mRNA expression was associated with early stage cervical cancer. In a previous study evaluating HLA-G and HLA-E expression in SIL biopsies, HLA-G expression was increased during the first stage of the lesions (LSIL), decreasing with increasing lesion grade (HSIL). In contrast, HLA-E expression exhibited an opposite behavior according to SIL severity.11 The balance between constitutive HLA-G and virus-modulated expression may determine the outcome of the infection, facilitating or not virus persistence. This study was designed to evaluate the potential involvement of polymorphic sites of the HLA-G gene in the development of SIL in women harboring HPV infection.
Several HLA-G polymorphisms have been reported to be associated with differential expression of the HLA-G molecule.19 In this study, the HLA-G*0103 was associated with protection against HPV lesions when patients considered as a whole were compared to controls. In addition, all the individuals presenting the G*0103 allele in this study were homozygous for this allele (confirmed by sequencing analysis), indicating that the associations with the G*0103 allele or G*0103/G*0103 genotype were not independent observations. The same protective effect was observed for the G*0103/+14 bp haplotype; however, this allele is known to always be associated with the insertion of the 14 bp fragment in the Brazilian population.34
Considering that the G*0103 allele ranks third in frequency (8.74%) in the normal Brazilian population,34 and that in the present series it was absent in patients, these data indicate that this allele may protect against SIL even in the presence of the more oncogenic HPV types. Certain HLA-G alleles have been associated with the magnitude of HLA-G molecule production; however, no association between the G*0103 allele and levels of HLA-G production, HLA-G expression or both, has been reported.
On the other hand, the HLA-G*010401 allele has been associated with high plasma levels of sHLA-G.19 Considering that the G*010401 and G*010404 alleles are the most frequent in the G0104 allele group, with a frequency of 8.25 and 3.88% in the normal Brazilian population, respectively,34 and given that both alleles (1) have the same coding and non-coding sequences (except for a single nucleotide exchange in exon 4), (2) are related to the deletion of the 14 bp fragment,34 (3) are probably associated with the same promoter activity and (4) probably have similar HLA-G production ability, the G0104 allele group, as well as the G*010401 allele, may be associated with high sHLA-G production.19 In spite of a possible harmful influence of a high-producer allele group and SIL, in the present series the G0101/0104 genotype seemed to confer protection against the occurrence of HSIL.
In the present study, the G0104 group consisted of five different HLA-G alleles (Table 1), two of which have been previously associated with the deletion of the 14 bp fragment, and the others were rare in the Brazilian population and have no recognized 14 bp association.34 However, the G*010401/+14 bp haplotype has already been reported, probably due to the occurrence of crossing-over inside the HLA-G gene or these may simply be haplotypes of African or Amerindian origin.34 In the present series, the G0104/−14 bp haplotype seemed to be associated with low-grade lesions in women infected with HPVX compared to controls, but no association was found when low- and high-grade patients were compared. Similarly, the G0104/+14 bp haplotype was associated with high-grade lesions in women infected with both HPV-16/18 compared to controls, but no association was found when low- and high-grade patients were compared. Considering that the G0104 allele group is probably associated with a higher production of sHLA-G19 and that the 14 bp insertion produces a more stable mRNA,22 these findings indicate that women possessing the G0104/+14 bp haplotype may produce more HLA-G and, therefore, may evade the attack of NK cells. Although the strength of this association (OR) is high (P=0.0177; OR=34.697; 95% CI=1.594–755.46), it should be noted that no association was found comparing LSIL and HSIL groups (only with controls), no individual association was found with the G0104 allele group (only when stratified into haplotypes), and the association between G0104/−14 and HSIL (16/18+) was based only on two positive cases (a rare haplotype in our population).
In this study, we reported that women presenting the HLA-G*0103 allele may be protected against SIL. In addition, women who harbor co-infection with HPV-16 and -18 and who possess the high-production HLA-G0104 allele group together with the presence of other mRNA stability factors, such as +14 bp, were at higher risk for the occurrence of HSIL compared with women without HPV infection and with women infected with other HPV types.
In conclusion, the G*0103 allele and G0101/G0104 genotype may be associated with protection against SIL. The G0104/+14 bp and G0104/−14 bp haplotypes conferred susceptibility to SIL compared to controls; however, patients possessing the G0104/+14 bp haplotype who presented HPV-16 and -18 co-infection were particularly associated with HSIL. Whether the amount of sHLA-G production and magnitude of HLA-G membrane expression or the balance between HLA molecules on the cervical cell surface that produce inhibitory or stimulatory signals for NK cells is necessary to modulate the outcome of the infection are questions that need to be further explored. Although other HLA class I and class II classical genes have been associated with SIL,44, 45, 46, 47 the results of the present study indicate that HLA-G polymorphisms as well as the HPV type are associated with SIL. To clarify the function of HLA-G alleles in SIL susceptibility, it would be interesting to conduct a longitudinal study on normal women exhibiting HPV infection with no SIL to determine whether these alleles are associated with elimination or persistence of HPV infection.
References
Munoz N, Bosch FX, de Sanjose S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med 2003;348:518–527.
O'Brien PM, Saveria Campo M . Evasion of host immunity directed by papillomavirus-encoded proteins. Virus Res 2002;88:103–117.
Koutsky LA, Holmes KK, Critchlow CW, et al. A cohort study of the risk of cervical intraepithelial neoplasia grade 2 or 3 in relation to papillomavirus infection. N Engl J Med 1992;327:1272–1278.
Carosella ED, Favier B, Rouas-Freiss N, et al. Beyond the increasing complexity of the immunomodulatory HLA-G molecule. Blood 2008;111:4862–4870.
Georgopoulos NT, Proffitt JL, Blair GE . Transcriptional regulation of the major histocompatibility complex (MHC) class I heavy chain, TAP1 and LMP2 genes by the human papillomavirus (HPV) type 6b, 16 and 18 E7 oncoproteins. Oncogene 2000;19:4930–4935.
Borrego F, Kabat J, Kim DK, et al. Structure and function of major histocompatibility complex (MHC) class I specific receptors expressed on human natural killer (NK) cells. Mol Immunol 2002;38:637–660.
Carosella ED, Moreau P, Le Maoult J, et al. HLA-G molecules: from maternal–fetal tolerance to tissue acceptance. Adv Immunol 2003;81:199–252.
Rouas-Freiss N, Goncalves RM, Menier C, Dausset J, Carosella ED . Direct evidence to support the role of HLA-G in protecting the fetus from maternal uterine natural killer cytolysis. Proc Natl Acad Sci USA 1997;94:11520–11525.
Fujii T, Ishitani A, Geraghty DE . A soluble form of the HLA-G antigen is encoded by a messenger ribonucleic acid containing intron 4. J Immunol 1994;153:5516–5524.
Crisa L, McMaster MT, Ishii JK, et al. Identification of a thymic epithelial cell subset sharing expression of the class Ib HLA-G molecule with fetal trophoblasts. J Exp Med 1997;186:289–298.
Goncalves MA, Le Discorde M, Simoes RT, et al. Classical and non-classical HLA molecules and p16(INK4a) expression in precursors lesions and invasive cervical cancer. Eur J Obstet Gynecol Reprod Biol 2008;141:70–74.
Rouas-Freiss N, Moreau P, Ferrone S, et al. HLA-G proteins in cancer: do they provide tumor cells with an escape mechanism? Cancer Res 2005;65:10139–10144.
Lafon M, Prehaud C, Megret F, et al. Modulation of HLA-G expression in human neural cells after neurotropic viral infections. J Virol 2005;79:15226–15237.
Lozano JM, Gonzalez R, Kindelan JM, et al. Monocytes and T lymphocytes in HIV-1-positive patients express HLA-G molecule. AIDS 2002;16:347–351.
Onno M, Pangault C, Le Friec G, et al. Modulation of HLA-G antigens expression by human cytomegalovirus: specific induction in activated macrophages harboring human cytomegalovirus infection. J Immunol 2000;164:6426–6434.
LeMaoult J, Krawice-Radanne I, Dausset J, et al. HLA-G1-expressing antigen-presenting cells induce immunosuppressive CD4+ T cells. Proc Natl Acad Sci USA 2004;101:7064–7069.
Fournel S, Aguerre-Girr M, Huc X, et al. Cutting edge: soluble HLA-G1 triggers CD95/CD95 ligand-mediated apoptosis in activated CD8+ cells by interacting with CD8. J Immunol 2000;164:6100–6104.
Anthony Nan Research Institute. Full List of HLA Class I alleles. http://hla.alleles.org/class1.html 2009, Accessed: 7 March 2007.
Rebmann V, van der Ven K, Passler M, et al. Association of soluble HLA-G plasma levels with HLA-G alleles. Tissue Antigens 2001;57:15–21.
Hviid TV, Hylenius S, Rorbye C, et al. HLA-G allelic variants are associated with differences in the HLA-G mRNA isoform profile and HLA-G mRNA levels. Immunogenetics 2003;55:63–79.
Hiby SE, King A, Sharkey A, et al. Molecular studies of trophoblast HLA-G: polymorphism, isoforms, imprinting and expression in preimplantation embryo. Tissue Antigens 1999;53:1–13.
Rousseau P, Le Discorde M, Mouillot G, et al. The 14 bp deletion-insertion polymorphism in the 3′ UT region of the HLA-G gene influences HLA-G mRNA stability. Hum Immunol 2003;64:1005–1010.
Gazit E, Sherf M, Balbin E, et al. HLA-G expression is induced in Epstein–Barr virus-transformed B-cell lines by culture conditions. Hum Immunol 2007;68:463–468.
Megret F, Prehaud C, Lafage M, et al. Modulation of HLA-G and HLA-E expression in human neuronal cells after rabies virus or herpes virus simplex type 1 infections. Hum Immunol 2007;68:294–302.
Pangault C, Le Tulzo Y, Minjolle S, et al. HLA-G expression in Guillain–Barre syndrome is associated with primary infection with cytomegalovirus. Viral immunology 2004;17:123–125.
Higuchi R . Simple and rapid preparation of samples for PCR In: Erlich HA (ed). PCR Technology: Principles and Applications for DNA Amplification. Stockton Press: New York, 1989, pp 31–38.
Manos MM, Ting Y, Wright DK, et al. The use of polymerase chain reaction amplification for the detection of genital human papillomaviruses In: Furth M, Greaves M (eds). Molecular Diagnostics of Human Cancer: Cancer Cells Vol. 7, Cold Spring Harbor Laboratory: New York, 1989, pp 209–214.
Freitas TP, Carmo BB, Paula FD, et al. Molecular detection of HPV 16 and 18 in cervical samples of patients from Belo Horizonte, Minas Gerais, Brazil. Revista do Instituto de Medicina Tropical de Sao Paulo 2007;49:297–301.
Pereira CR, Rosa ML, Vasconcelos GA, et al. Human papillomavirus prevalence and predictors for cervical cancer among high-risk women from Rio de Janeiro, Brazil. Int J Gynecol Cancer 2007;17:651–660.
Zereu M, Zettler CG, Cambruzzi E, Zelmanowicz A . Herpes simplex virus type 2 and Chlamydia trachomatis in adenocarcinoma of the uterine cervix. Gynecol Oncol 2007;105:172–175.
Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide (see comments). J Pathol 1999;189:12–19.
Morales P, Corell A, Martinez-Laso J, et al. Three new HLA-G alleles and their linkage disequilibria with HLA-A. Immunogenetics 1993;38:323–331.
Sanguinetti CJ, Dias Neto E, Simpson AJ . Rapid silver staining and recovery of PCR products separated on polyacrylamide gels. Biotechniques 1994;17:914–921.
Castelli EC, Mendes-Junior CT, Donadi EA . HLA-G alleles and HLA-G 14 bp polymorphisms in a Brazilian population. Tissue Antigens 2007;70:62–68.
Bermingham J, Jenkins D, McCarthy T, et al. Genetic analysis of insulin-like growth factor II and HLA-G in pre-eclampsia. Biochem Soc Trans 2000;28:215–219.
Raymond M, Rousset F . GENEPOP on the Web (Version 3.4). http://wbiomed.curtin.edu.au/genepop/2.0 edn, Vol. 83, J Heredity 2004, pp 248–249.
GraphPad. GraphPad InStat Version 3.00 for Windows 95 3.01 edn GraphPad Software Inc.: San Diego, CA, USA, 1998.
Excoffier L, Slatkin M . Maximum-likelihood estimation of molecular haplotype frequencies in a diploid population. Mol Biol Evol 1995;12:921–927.
Stephens M, Smith NJ, Donnelly P . A new statistical method for haplotype reconstruction from population data. Am J Hum Genet 2001;68:978–989.
Carosella ED, Moreau P, Lemaoult J, et al. HLA-G: from biology to clinical benefits. Trends Immunol 2008;29:125–132.
Yoon BS, Kim YT, Kim JW, et al. Expression of human leukocyte antigen-G and its correlation with interleukin-10 expression in cervical carcinoma. Int J Gynaecol Obstet 2007;98:48–53.
Zhou JH, Ye F, Chen HZ, et al. Altered expression of cellular membrane molecules of HLA-DR, HLA-G and CD99 in cervical intraepithelial neoplasias and invasive squamous cell carcinoma. Life Sci 2006;78:2643–2649.
Polakova K, Russ G . Expression of the non-classical HLA-G antigen in tumor cell lines is extremely restricted. Neoplasma 2000;47:342–348.
Ades S, Koushik A, Duarte-Franco E, et al. Selected class I and class II HLA alleles and haplotypes and risk of high-grade cervical intraepithelial neoplasia. Int J Cancer 2008;122:2820–2826.
Chan DP, Cheung TH, Tam AO, et al. Risk association between human leukocyte antigen-A allele and high-risk human papillomavirus infection for cervical neoplasia in Chinese women. J Infect Dis 2005;192:1749–1756.
de Araujo Souza PS, Maciag PC, Ribeiro KB, et al. Interaction between polymorphisms of the human leukocyte antigen and HPV-16 variants on the risk of invasive cervical cancer. BMC Cancer 2008;8:246.
Eiguchi K, Tatti S, Alonio LV, et al. Association of DRB1 and DQB1 HLA class II polymorphisms in high-grade and neoplastic cervical lesions of women from Argentina. J Low Genit Tract Dis 2008;12:262–268.
Acknowledgements
We thank Sandra Rodrigues and Ana Maria Rocha for excellent technical assistance and Dr Luisa Lina Villa for providing the HPV-16 and HPV-18 DNA-positive standard samples.
Financial Support: This work was supported by grants from CAPES (DS 103/00) to Simões, and from FAPESP (01/02908-2) and CAPES (0313/04-1) to Gonçalves (Brazilian and São Paulo State governments, respectively).
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure/conflict of interest
This paper was reviewed and approved by all authors. There is no conflict of interests regarding this article.
Rights and permissions
About this article
Cite this article
Simões, R., Gonçalves, M., Castelli, E. et al. HLA-G polymorphisms in women with squamous intraepithelial lesions harboring human papillomavirus. Mod Pathol 22, 1075–1082 (2009). https://doi.org/10.1038/modpathol.2009.67
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2009.67
Keywords
This article is cited by
-
The association of HLA-G polymorphism with oral and genital HPV infection in men
European Journal of Clinical Microbiology & Infectious Diseases (2022)
-
HLA-G polymorphism impacts the outcome of oral HPV infections in women
BMC Infectious Diseases (2021)
-
Physiopathology and effectiveness of therapeutic vaccines against human papillomavirus
Environmental Science and Pollution Research (2021)
-
Association of HLA-G 3′ UTR polymorphism and expression with the progression of cervical lesions in human papillomavirus 18 infections
Infectious Agents and Cancer (2018)
-
Cervix smear abnormalities: linking pathology data in female twins, their mothers and sisters
European Journal of Human Genetics (2011)