Abstract
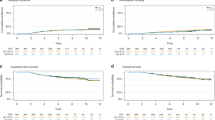
We report outcomes after single (s) and double (d) umbilical cord blood transplantation (UCBT) after myeloablative conditioning (MAC) regimen for 239 patients transplanted for acute leukemia in first complete remission (CR1). All sUCBT patients received a total nucleated cell dose >2.5 × 107/kg. Conditioning regimen for sUCBT was total body irradiation (TBI)12 Gy- or busulfan (BU)-based±fludarabine (Flu) (n=68, group 1), thiotepa+BU+Flu (TBF) (n=88, group 2), and for dUCBT it was TBI12 Gy+cyclophosphamide±Flu (n=83, group 3). dUCBT recipients were younger, received higher cell dose and less frequently antithymocyte globulin. In multivariate analysis, we found similar neutrophil recovery among the three groups; however, acute graft-versus-host disease II–IV was higher in dUCBT compared with others. Non-relapse mortality and relapse incidence were not statistically different among the three groups. Leukemia-free survival was 30% for sUCBT using TBI- or BU-based MAC compared with 48% for sUCBT TBF and 48% for dUCBT (P=0.02 and P=0.03, respectively), and it was not statistically different between sUCBT with TBF and dUCBT. In conclusion, use of sUCBT with adequate cell dose (>2.5 × 107/kg) and a specific conditioning regimen in the MAC setting results in similar outcomes as dUCBT. The choice of TBF conditioning regimen for sUCBT may improve results, and whether this regimen may be effective in dUCBT should be further analyzed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Rowe JM . Prognostic factors in adult acute lymphoblastic leukaemia. Br J Haematol 2010; 150: 389–405.
Dohner H, Estey EH, Amadori S, Appelbaum FR, Buchner T, Burnett AK et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood 2010; 115: 453–474.
Lee S, Chung NG, Cho BS, Eom KS, Kim YJ, Kim HJ et al. Donor-specific differences in long-term outcomes of myeloablative transplantation in adults with Philadelphia-negative acute lymphoblastic leukemia. Leukemia 2010; 24: 2110–2119.
Walter RB, Pagel JM, Gooley TA, Petersdorf EW, Sorror ML, Woolfrey AE et al. Comparison of matched unrelated and matched related donor myeloablative hematopoietic cell transplantation for adults with acute myeloid leukemia in first remission. Leukemia 2010; 24: 1276–1282.
Arcese W, Rocha V, Labopin M, Sanz G, Iori AP . Unrelated cord blood transplants in adults with hematologic malignancies. Haematologica 2006; 91: 223–230.
Rocha V, Labopin M, Sanz G, Arcese W, Schwerdtfeger R, Bosi A et al. Transplants of umbilical-cord blood or bone marrow from unrelated donors in adults with acute leukemia. N Engl J Med 2004; 351: 2276–2285.
Laughlin MJ, Eapen M, Rubinstein P, Wagner JE, Zhang MJ, Champlin RE et al. Outcomes after transplantation of cord blood or bone marrow from unrelated donors in adults with leukemia. N Engl J Med 2004; 351: 2265–2275.
Eapen M, Rocha V, Sanz G, Scaradavou A, Zhang MJ, Arcese W et al. Effect of graft source on unrelated donor haemopoietic stem-cell transplantation in adults with acute leukaemia: a retrospective analysis. Lancet Oncol 2010; 11: 653–660.
Kanda J, Ichinohe T, Kato S, Uchida N, Terakura S, Fukuda T et al. Unrelated cord blood transplantation vs related transplantation with HLA 1-antigen mismatch in the graft-versus-host direction. Leukemia 2013; 27: 286–294.
Gluckman E, Ruggeri A, Volt F, Cunha R, Boudjedir K, Rocha V . Milestones in umbilical cord blood transplantation. Br J Haematol 2011; 154: 441–447.
Barker JN, Weisdorf DJ, DeFor TE, Blazar BR, McGlave PB, Miller JS et al. Transplantation of 2 partially HLA-matched umbilical cord blood units to enhance engraftment in adults with hematologic malignancy. Blood 2005; 105: 1343–1347.
Rocha V, Broxmeyer HE . New approaches for improving engraftment after cord blood transplantation. Biol Blood Marrow Transplant 2010; 16 (1 Suppl): S126–S132.
Barker JN, Weisdorf DJ, Wagner JE . Creation of a double chimera after the transplantation of umbilical-cord blood from two partially matched unrelated donors. N Engl J Med 2001; 344: 1870–1871.
MacMillan ML, Weisdorf DJ, Brunstein CG, Cao Q, DeFor TE, Verneris MR et al. Acute graft-versus-host disease after unrelated donor umbilical cord blood transplantation: analysis of risk factors. Blood 2009; 113: 2410–2415.
Verneris MR, Brunstein CG, Barker J, MacMillan ML, DeFor T, McKenna DH et al. Relapse risk after umbilical cord blood transplantation: enhanced graft-versus-leukemia effect in recipients of 2 units. Blood 2009; 114: 4293–4299.
Brunstein CG, Gutman JA, Weisdorf DJ, Woolfrey AE, Defor TE, Gooley TA et al. Allogeneic hematopoietic cell transplantation for hematologic malignancy: relative risks and benefits of double umbilical cord blood. Blood 2010; 116: 4693–4699.
Scaradavou A, Brunstein CG, Eapen M, Le-Rademacher J, Barker JN, Chao N et al. Double unit grafts successfully extend the application of umbilical cord blood transplantation in adults with acute leukemia. Blood 2013; 121: 752–758.
Tutschka PJ, Copelan EA, Klein JP . Bone marrow transplantation for leukemia following a new busulfan and cyclophosphamide regimen. Blood 1987; 70: 1382–1388.
Saito AM, Cutler C, Zahrieh D, Soiffer RJ, Ho VT, Alyea EP et al. Costs of allogeneic hematopoietic cell transplantation with high-dose regimens. Biol Blood Marrow Transplant 2008; 14: 197–207.
Sanz J, Boluda JC, Martin C, Gonzalez M, Ferra C, Serrano D et al. Single-unit umbilical cord blood transplantation from unrelated donors in patients with hematological malignancy using busulfan, thiotepa, fludarabine and ATG as myeloablative conditioning regimen. Bone Marrow Transplant 2012; 47: 1287–1293.
Szydlo R, Goldman JM, Klein JP, Gale RP, Ash RC, Bach FH et al. Results of allogeneic bone marrow transplants for leukemia using donors other than HLA-identical siblings. J Clin Oncol 1997; 15: 1767–1777.
Majhail NS, Brunstein CG, Wagner JE . Double umbilical cord blood transplantation. Curr Opin Immunol 2006; 18: 571–575.
Avery S, Shi W, Lubin M, Gonzales AM, Heller G, Castro-Malaspina H et al. Influence of infused cell dose and HLA match on engraftment after double-unit cord blood allografts. Blood 2011; 117: 3277–3285, quiz 3478.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation 1974; 18: 295–304.
Terwey TH, Vega-Ruiz A, Hemmati PG, Martus P, Dietz E, le Coutre P et al. NIH-defined graft-versus-host disease after reduced intensity or myeloablative conditioning in patients with acute myeloid leukemia. Leukemia 2012; 26: 536–542.
Kaplan EL, Meier P . Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Cox DR . Regression models and life tables. J R Stat Soc 1972; 34: 187–220.
Fine JPGJ . A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496–509.
Brunstein CG, Eapen M, Ahn KW, Appelbaum FR, Ballen KK, Champlin RE et al. Reduced-intensity conditioning transplantation in acute leukemia: the effect of source of unrelated donor stem cells on outcomes. Blood 2012; 119: 5591–5598.
Costa V, McGregor M, Laneuville P, Brophy JM . The cost-effectiveness of stem cell transplantations from unrelated donors in adult patients with acute leukemia. Value hHealth 2007; 10: 247–255.
Lee JH, Joo YD, Kim H, Ryoo HM, Kim MK, Lee GW et al. Randomized trial of myeloablative conditioning regimens: busulfan plus cyclophosphamide versus busulfan plus fludarabine. J Clin Oncol 2013; 31: 701–709.
Mohty M, Labopin M, Balere ML, Socie G, Milpied N, Tabrizi R et al. Antithymocyte globulins and chronic graft-vs-host disease after myeloablative allogeneic stem cell transplantation from HLA-matched unrelated donors: a report from the Societe Francaise de Greffe de Moelle et de Therapie Cellulaire. Leukemia 2010; 24: 1867–1874.
Brunstein CG, Fuchs EJ, Carter SL, Karanes C, Costa LJ, Wu J et al. Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood 2011; 118: 282–288.
Oran B, Wagner JE, DeFor TE, Weisdorf DJ, Brunstein CG . Effect of conditioning regimen intensity on acute myeloid leukemia outcomes after umbilical cord blood transplantation. Biol Blood Marrow Transplant 2011; 17: 1327–1334.
Robin M, Sanz GF, Ionescu I, Rio B, Sirvent A, Renaud M et al. Unrelated cord blood transplantation in adults with myelodysplasia or secondary acute myeloblastic leukemia: a survey on behalf of Eurocord and CLWP of EBMT. Leukemia 2011; 25: 75–81.
Gluckman E, Rocha V, Arcese W, Michel G, Sanz G, Chan KW et al. Factors associated with outcomes of unrelated cord blood transplant: guidelines for donor choice. Exp Hematol 2004; 32: 397–407.
Rubinstein P, Carrier C, Scaradavou A, Kurtzberg J, Adamson J, Migliaccio AR et al. Outcomes among 562 recipients of placental-blood transplants from unrelated donors. N Engl J Med 1998; 339: 1565–1577.
Barker JN, Byam C, Scaradavou A . How I treat: the selection and acquisition of unrelated cord blood grafts. Blood 2011; 117: 2332–2339.
Wagner JE, Barker JN, DeFor TE, Baker KS, Blazar BR, Eide C et al. Transplantation of unrelated donor umbilical cord blood in 102 patients with malignant and nonmalignant diseases: influence of CD34 cell dose and HLA disparity on treatment-related mortality and survival. Blood 2002; 100: 1611–1618.
Sanz GF, Saavedra S, Planelles D, Senent L, Cervera J, Barragan E et al. Standardized, unrelated donor cord blood transplantation in adults with hematologic malignancies. Blood 2001; 98: 2332–2338.
Acknowledgements
This study was funded in part by the Inserm grant TGIR0805. VR is funded by the National Institute for Health Research (NIHR)-Biomedical Research Centre (BRC) funding scheme. We thank ‘DU formation à la conduit de projet de recherché Clinique’ Université Paris-Diderot-France. We also thank Chantal Kenzey for help with data collection and the following participating centers for contributing to the cases: Australia, Perth, WA—RP Group Royal Perth Hospital; Austria, Graz—Medical University Graz; Austria, Vienna—Medizinische Universitaet Wien; Belgium, Brussels—Universitair Ziekenhuis Brussel; Belgium, Liege—University of Liege; Finland, Helsinki—Helsinki University Central Hospital; France, Angers—CHR Angers; France, Besançon—Saint Jacques; France, Bordeaux—Haut-Lévêque; France, Brest—Augustin Morvan; France, Caen—CHU de Caen; France, Clermont—Ferrand-Hôtel Dieu CHU/Jean Perrin; France, Grenoble—Tronche CHU/Albert Michallon; France, Lille—Claude Huriez; France, Lyon—Edouard Herriot (adulte); France, Marseille—Paoli Calmettes (adulte); France, Montpellier—Lapeyronie (adulte); France, Nancy—Brabois; France, Nantes—Hôtel Dieu; France, Nice—Archet; France, Paris—La Pitié; France, Paris—Saint-Louis; France, Rennes—Pontchaillou; France, Saint-Etienne—Hôpital Nord/Institut de Cancérologie de la Loire; Germany, Düsseldorf—Heinrich Heine Universität; Germany, Düsseldorf—Universitaetsklinikum; Germany, Idar-Oberstein—Klinik Hamatologie/Onkologie; Germany, Munich—Klinikum Grosshadern; Germany, Regensburg—University Regensburg; Greece, Athens—Evangelismos Hospital; Greece, Patras—University Medical School; Hungary, Budapest—St István and St Laszlo Hospital of Budapest; Ireland, Dublin—St James’s Hospital; Israel, Jerusalem—Hadassah University Hospital; Israel, Tel-Hashomer—Chaim Sheba Medical Center; Italy, Bergamo—Ospedali Riuniti di Bergamo; Italy, Bologna—Bologna University, S Orsola-Malpighi Hospital; Italy, Brescia—TMO Adulti Brescia; Italy, Cuneo—Azienda Ospedaliera S Croce e Carle; Italy, Firenze—Azienda Ospedaliero Universitaria Meyer-Ospedale di Careggi; Italy, Monza—Ospedale San Gerardo; Italy, Palermo—Ospedale V Cervello; Italy, Rome—Ospedale S Camillo; Italy, Rome—Rome Transplant Network; Italy, Rome—Universita Cattolica S Cuore; Italy, Siena—Azienda Ospedaliera Universitaria Senese Policlinico S Maria alle Scotte; Italy, Torino—Ospedale Universitaria San Giovanni Battista; Italy, Tricase (Lecce)—Hospital C Panico; Jordan, Amman—King Hussein Cancer Centre; Poland, Warsaw—The Medical University of Warsaw; Portugal, Porto—Inst. Portugues de Oncologia do Porto; Saudi Arabia, Riyadh—King Faisal Specialist Hospital and Research Centre; Spain, Barcelona—Hospital Clinic; Spain, Barcelona—Hospital Santa Creu i Sant Pau; Spain, Barcelona—ICO-Hospital Universitari Germans Trias i Pujol. Jose Carreras Research Institute, Badalona, Spain-ICO-Hospital Duran i Reynals; Spain, Córdoba—Hosp. Reina Sofia; Spain, Granada—Hospital Univ. Virgen de las Nieves; Spain, Madrid—Hospital Gregorio Marañón; Spain, Málaga—Hospital Carlos Haya; Spain, Murcia—Hospital Morales Meseguer; Spain, Oviedo—University Hospital of Asturias; Spain, Salamanca—Hospital Clínico; Spain, Sevilla—Hospital Universitario Virgen del Rocío; Spain, Valencia—Hospital Clínico Universitario; Spain, Valencia—Hospital Universitario La Fe; Sweden, Goeteborg—Sahlgrenska University Hospital; Sweden, Stockholm—Karolinska University Hospital Children’s Hospital; Switzerland, Geneva—Hopitaux Universitaires de Geneve; Switzerland, Zürich—University Hospital; The Netherlands, Leiden—University Hospital; The Netherlands, Rotterdam—Erasmus MC-Daniel den Hoed Cancer Centre; Turkey, Ankara—University Faculty of Medicine; United Kingdom, Birmingham—Birmingham Heartlands Hospital; United Kingdom, Birmingham—Queen Elizabeth Hospital; United Kingdom, Bristol—Royal Hospital for Children; United Kingdom, Glasgow—Gartnaval General Hospital; United Kingdom, Leicester—Leicester Royal Infirmary; United Kingdom, London—Imperial College Hammersmith Hospital; United Kingdom, London—King’s Denmark Hill Campus School of Medicine; United Kingdom, London—Royal Free and University College Medical School; United Kingdom, London—Surrey Royal Marsden Hospital; United Kingdom, Oxford—Churchill Hospital.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author contributions
AR, HB and VR designed the study; AR, HB and SN prepared and analyzed data; AR, FV, EG and VR wrote the paper; GS, AR2, IYA, JR, LM, JS, MM, CS and WA provided cases for the study; and ML helped to analyze the data. All authors edited and approved the manuscript.
Rights and permissions
About this article
Cite this article
Ruggeri, A., Sanz, G., Bittencourt, H. et al. Comparison of outcomes after single or double cord blood transplantation in adults with acute leukemia using different types of myeloablative conditioning regimen, a retrospective study on behalf of Eurocord and the Acute Leukemia Working Party of EBMT. Leukemia 28, 779–786 (2014). https://doi.org/10.1038/leu.2013.259
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2013.259
Keywords
This article is cited by
-
Outcome of human umbilical cord blood stem cell transplantation (CBT) for acute myeloid leukemia in patients achieving first complete remission after one versus two induction courses: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation (EBMT)
Bone Marrow Transplantation (2022)
-
Umbilical cord blood transplants facilitated by the French cord blood banks network. On behalf of the Agency of Biomedicine, Eurocord and the French society of bone marrow transplant and cell therapy (SFGM-TC)
Bone Marrow Transplantation (2021)
-
Allogeneic hematopoietic stem cell transplantation with fludarabine, busulfan, and thiotepa conditioning is associated with favorable outcomes in myelofibrosis
Bone Marrow Transplantation (2020)
-
Reduced dose of MTX for GVHD prophylaxis promotes engraftment and decreases non-relapse mortality in umbilical cord blood transplantation
Annals of Hematology (2020)
-
Umbilical cord blood versus unrelated donor transplantation in adults with primary refractory or relapsed acute myeloid leukemia: a report from Eurocord, the Acute Leukemia Working Party and the Cord Blood Committee of the Cellular Therapy and Immunobiology Working Party of the EBMT
Blood Cancer Journal (2019)