Abstract
Resistance to rifampicin (RIF) is a broad subject covering not just the mechanism of clinical resistance, nearly always due to a genetic change in the β subunit of bacterial RNA polymerase (RNAP), but also how studies of resistant polymerases have helped us understand the structure of the enzyme, the intricacies of the transcription process and its role in complex physiological pathways. This review can only scratch the surface of these phenomena. The identification, in strains of Escherichia coli, of the positions within β of the mutations determining resistance is discussed in some detail, as are mutations in organisms that are therapeutic targets of RIF, in particular Mycobacterium tuberculosis. Interestingly, changes in the same three codons of the consensus sequence occur repeatedly in unrelated RIF-resistant (RIFr) clinical isolates of several different bacterial species, and a single mutation predominates in mycobacteria. The utilization of our knowledge of these mutations to develop rapid screening tests for detecting resistance is briefly discussed. Cross-resistance among rifamycins has been a topic of controversy; current thinking is that there is no difference in the susceptibility of RNAP mutants to RIF, rifapentine and rifabutin. Also summarized are intrinsic RIF resistance and other resistance mechanisms.
Similar content being viewed by others
Introduction
In celebrating the life of Professor Piero Sensi and his discovery of rifampicin (RIF), also known as rifampin, we have recognized the importance of this drug in treating infectious disease, in particular tuberculosis. In thinking about resistance, we should keep in mind that it is not just an inconvenient clinical phenomenon. The study of RIF and of resistant mutants in different bacterial species has had a key role in the elucidation of the structure and function of bacterial DNA-dependent RNA polymerase (RNAP) and its involvement in the modulation of complex physiological pathways.
Early in the study of the rifamycins, the occurrence, in cultures of susceptible organisms, of spontaneous one-step mutations to high-level resistance became apparent, initially as a ‘skipped tube’ phenomenon in MIC determinations. The literature dealing with resistance to RIF is extensive and some of the early publications are not readily available. Areas of study include: resistance mechanisms (primarily acquired resistance because of mutation in the rpoB gene, which encodes the β subunit of RNAP); identification of the amino-acid changes in β associated with resistance in laboratory strains and clinical isolates; the practice of combined antimicrobial therapy to limit the emergence of resistance; cross-resistance of RIF with other RNAP inhibitors; pleiotropic effects of RIF-resistant (RIFr) enzymes on gene expression; and development of rapid tests for the detection of resistance in Mycobacterium tuberculosis. Some of these aspects will be touched upon only briefly.
Primary mechanism of resistance to RIF: mutations affecting RNAP subunit β
Clinical and laboratory studies of RIF initially targeted a broad spectrum of susceptible bacteria, and resistance was reported in laboratory studies and emerging in patients who received monotherapy with RIF. Resistance rates to rifamycins, determined in the laboratory, have ranged from 10−10 to 10−7, depending on the organism and the methodology used.1, 2, 3, 4 RIF resistance was reported in different Gram-negative urinary tract pathogens, in vitro and in treated patients;5 in gonococci and meningococci in the laboratory and the clinic;2, 6, 7 and in tuberculosis patients who failed therapy when RIF was the only active drug administered.8 When treating tuberculosis and other diseases, RIF is almost always combined with other active antimicrobials to prevent the emergence of resistance.
Shortly after RIF was shown to inhibit transcription, cell-free assays demonstrated that resistance, at least in laboratory strains, was related to a change in the properties of the polymerase: RNAP from resistant bacteria was itself resistant in these assays, and it did not bind RIF.9, 10, 11, 12 That the target within the enzyme was the β subunit, one of its two largest polypeptides, was first suggested by the observation that in a RIFr Escherichia coli strain the migration of this subunit in polyacrylamide gel electrophoresis was altered.13 Subsequently, separation and mixed reconstitution of enzymatically active core enzyme, using subunits from susceptible and RIFr strains of E. coli14 and Bacillus subtilis,15 provided a more direct demonstration that resistance was determined by a change in the β subunit.
The spectrum and localization within rpoB of RIFr mutations, in both clinical isolates and strains selected in the laboratory, has been studied in a number of species, including E. coli, M. tuberculosis and Staphylococcus aureus. Although E. coli is generally not a therapeutic target for RIF, it is a model species for genetic and physiological studies, and there were detailed investigations of transcription initiation and termination in this organism. Nearly complete saturation of the RIFr mutational spectrum in E. coli and mapping and sequencing of the mutations in rpoB was achieved in the 1980s, largely by the efforts of Jin and Gross.16 The mapping of RIFr mutations in other organisms has most often been reported with alignment to the consensus numbering scheme of E. coli RNAP, facilitating comparison across species. As RNAP is highly conserved among eubacteria, it is not surprising that the sites of RIFr mutations are also conserved. Mutations affecting residues 516, 526 and 531 of the β consensus sequence predominate in resistant clinical isolates of a number of bacterial species. In the discussion that follows, only strains with a single mutation in rpoB that determines an amino-acid change and a RIFr phenotype are considered; for this reason, conclusions about mutation sites are not always identical to those of the authors.
RIF resistance in E. coli
Complete sequencing of rpoB posed a challenge as, with 1342 amino acids in E. coli, β is the second largest polypeptide in the bacterial cell. In the 1970s, refinements in the cloning and sequencing of overlapping DNA restriction fragments enabled the complete determination and alignment of the nucleotide sequence of rpoB with the amino-acid sequence of the β subunit from a RIFr strain of E. coli.17 Ovchinnikov et al.18 then utilized a susceptible strain to sequence the region of rpoB to which the RIFr mutation had been localized genetically, and identified it as an aspartic acid to valine change at residue 516 of the polypeptide, corresponding to an A:T to T:A transversion in the corresponding codon.
Jin and Gross16 constructed an isogenic set of mutants in E. coli K-12 derived from 42 RIFr strains from their own laboratory (both spontaneous and UV induced) and other sources. As the goal of generating and studying RIFr mutations in this organism was to understand the structure of the β subunit and its functional interaction within RNAP, a broad array of RIFr mutations were included. Thus, although they would likely have no relationship to those emerging in the clinic, the E. coli RIFr mutations included some that determined temperature-dependent and dominant phenotypes, as well as defects in transcription. Mapping was achieved by transformation with plasmids from a susceptible strain having various length deletions of rpoB; the region to which each mutation mapped was sequenced, identifying 17 unique alleles (excluding mutants with more than one change), a few of which had also been described by others, as had two additional unique mutations. Most were point mutations, although there were also three deletions of one to five codons and one insertion of two codons. Mutations specifying two different amino-acid changes were found in each of three codons. A number of the unique alleles were isolated several times, both by Jin and Gross and others. In cell-free RNAP assays, RIF 50% inhibition concentrations (IC50s) for the mutant enzymes ranged from 10 to >10 000 times the IC50 for the enzyme from the isogenic susceptible strain. These values roughly paralleled the concentrations that inhibited the growth of the mutant strains. In a later study, the extent of binding of RIF to the RNAPs from 12 of the mutants was also shown to correlate with the IC50s and with growth inhibition.19 The mutations mapped in the center of the rpoB gene, in three clusters: cluster I (covering amino acids 507–533) included 13 of the 17 RIFr alleles from this study, as well as a deletion mutant mapped by others; three of the mutations were in cluster II (amino acids 563–572); and one was at amino-acid 687 (cluster III). The segment of rpoB encompassing these clusters was initially called the ‘RIF region’, but is also known as the RIF resistance-determining region (RRDR). Another point mutation identified by others mapped outside of the RRDR at amino-acid 146. A few other unique RIFr mutations have since been described in E. coli. Landick et al.20 utilized bisulfite-induced cytosine deamination to mutagenize selected regions of rpoB and screened for termination-altering mutations. A number of the selected mutants were RIFr, and one had a single-amino-acid change within the RRDR that had not been previously reported. Another RIFr mutation within this region is cited by Severinov et al.21
As discussed by Jin and Gross,16 it appeared likely that the different regions of the β subunit in which RIFr mutations occur cooperate, within the core enzyme, to form the RIF-binding site. Approaches to the topology of the active center of the E. coli enzyme and its interaction with the RIF-binding site have been largely indirect; for example, utilizing the binding of different rifamycin derivatives, or of antibodies raised to rifamycin–albumin adducts, or of RIF–nucleotide adducts,22, 23 as well as molecular modeling based on the amino-acid sequence. By cross-linking the polymerase–promoter complex to β, followed by limited proteolysis and chemical degradation, it was demonstrated that cluster I of the RRDR forms part of the active center of the enzyme.24 E. coli RNAP has been crystallized only very recently.25 Although the enzyme is naturally partially resistant to RIF and has limitations in the co-structure of its binding site, studies with crystallized RNAP from Thermus aquaticus showed that the RIF-binding pocket is in the fork domain, part of the active center, and established that most RIFr mutations map to this region.26
RIF resistance in M. tuberculosis and other mycobacteria
Mapping the mutations found in clinical isolates has been critical to the development of rapid methods to detect resistance in patients. Standard susceptibility testing of slow-growing species generally requires 4 weeks of culture (M. tuberculosis) and as long as 1 year in an animal infection model (Mycobacterium leprae). An important finding was the predominance of a single mutation, Ser531Leu, in different studies. Only a selection of the many publications describing RIFr mutations in mycobacteria will be discussed.
Using cell-free RNAP assays, Yamada et al.27 had demonstrated that the RIFr phenotype of two clinical isolates of M. tuberculosis was determined by resistance of their enzymes. Telenti et al.28 determined the amino-acid changes in a collection of 66 RIFr clinical isolates from different geographical areas. They identified 15 distinct mutations in 8 codons within a segment of rpoB that aligned with the RRDR region of E. coli. In a set of 128 isolates from the United States, Kapur et al.29 identified a number of additional RIFr mutations in this region; interestingly, some of the mutations were identified in both studies but at different frequencies, suggesting geographic variation. Data from these and other studies, for a total of 307 RIFr isolates, were compiled by Musser.30 Twenty-eight unique amino-acid changes corresponded to point mutations in 12 different codons, 2 insertions of 1–2 codons and 7 deletions of 1–3 codons; all of them mapped to the region corresponding to cluster I of the E. coli RRDR. In later studies, four additional amino-acid changes and a three-codon deletion, all but one mapping to codons previously identified, were sequenced in clinical isolates from Japan and China.31, 32, 33 Another study of Japanese isolates identified two mutations affecting the N-terminal region of β (one of them corresponding to residue 146, previously identified in E. coli) and two mutations specifying low-level RIF resistance (MIC=12.5 μg ml–1) in RRDR cluster III;34 one of the latter corresponded to the previously identified E. coli mutation in this cluster. Among 63 rpoB clinical isolates from Germany, Heep et al.35 described an additional amino-acid change at residue 526.
Among the point mutations reviewed by Musser,30 there were three major hotspots, each with multiple amino-acid changes: residue 516 (four different amino acids in 25 clinical isolates); residue 526 (eight amino acids in 111 strains); and residue 531 (four amino acids in 132 strains). At each of these loci, a single-amino-acid change predominated, with Ser531Leu (TCG to TTG) alone occurring in 128 isolates. Although all but two of the RIFr mutations identified in M. tuberculosis clinical isolates mapped to codons that aligned with E. coli mutations, Ser531Leu, the single most frequently identified amino-acid change in mycobacteria, was not, although other amino-acid changes occurred at the same residue. This is not of biological significance, however, as this amino-acid replacement in E. coli would require two nucleotide changes (TCT to TTG or TTA) as compared with the single TCG to TTG transition in the M. tuberculosis codon.
In a laboratory study, using the Luria-Delbrück fluctuation test, Morlock et al.36 generated 64 spontaneous, independent RIFr mutations in M. tuberculosis H37Rv and identified eight different point mutations, one insertion and one deletion. All of them mapped to codons identified by mutations in clinical isolates, 20 of them in consensus residue 526 and 41 in residue 531 (39 of them Ser to Leu, TCG to TTG). In a selection experiment in which a few cultures were grown in the presence of RIF, all (non-independent) mutations occurred at residues 526 and 531, with Ser531Leu again predominating.37
In other mycobacterial species smaller numbers of RIFr isolates have been available for sequencing. Honore and Cole38 mapped eight of nine RIFr mutations in clinical isolates of Mycobacterium leprae to the residue corresponding to 531; six of them were Ser531Leu. Williams et al.39 also identified the Ser531Leu mutation in four strains of M. leprae analyzed, and in one Mycobacterium africanum strain and one Mycobacterium avium. Another M. avium isolate had a Ser531Trp mutation. In Mycobacterium kansasii, five RIFr clinical isolates and one laboratory mutant had mutations in codons 513, 526 or 531.40
Knowing the prevalence of different RIFr mutations in M. tuberculosis made it possible to design rapid nucleic acid amplification based molecular tests to detect the organism in patients with suspected infection and to identify resistance in patient isolates. A large number of methods were explored and tested for correlation of the results with those of standard susceptibility tests. In 2013, the Food and Drug Administration approved a commercial PCR-based test to detect the DNA of M. tuberculosis, as well as RIFr mutations, in sputum.41
RIF resistance in S. aureus
Most reports of rpoB mutations in this organism have used S. aureus numbering, in some cases with the consensus codon numbers provided; however, the present discussion will be based only on the E. coli numbering system. In 1979, Morrow and Harmon42 demonstrated that laboratory-generated rifamycin-resistant mutations in S. aureus were chromosomal and affected the ability of the antibiotics to inhibit RNAP activity in cell-free transcription assays. RIFr mutations in paired clinical isolates (susceptible and resistant strains from the same patients) and in laboratory strains of S. aureus were mapped by Aubry-Damon et al.43 A MIC histogram divided these strains into three categories: susceptible, low-level resistant and high-level resistant (MICs of ⩽0.5, 1–4 and ⩾8 μg ml–1, respectively). All 17 RIFr strains sequenced had single mutations, which included 8 distinct changes at 7 sites; 6 of the sites were within the consensus cluster I of the RRDR and corresponded to mutant codons identified in E. coli. Several additional sites of single mutations, two of them in cluster II and the others in cluster I, were reported by Wichelhaus et al.44; all of them corresponded to mutational sites in E. coli and one was the Ser531Leu mutation that predominates in M. tuberculosis. Ser531Leu was also identified by others in S. aureus RIFr clinical and laboratory strains, as was His526Asn; a few additional amino-acid changes have been described, most of them in the same codons identified previously in both E. coli and S. aureus.45, 46, 47, 48
RIF resistance in other species
There is extensive literature on RIF resistance in a number of bacterial species. Mutational changes in the β subunit of RNAP will be briefly discussed only in organisms for which RIF is commonly prescribed. Resistance in these species is frequently associated with mutations in rpoB codons 516, 526 or 531 of the consensus sequence.
RIF has been utilized clinically for prophylaxis in individuals exposed to Neisseria meningitidis, for prophylaxis and treatment of invasive Haemophilus influenzae, and for treatment of β-lactam-resistant Streptococcus pneumoniae infections. Fourteen RIFr strains of N. meningitidis from Italy and the United Kingdom had rpoB mutations in cluster I of the RRDR corresponding to Asp516Val, His526Tyr or His526Asp.49, 50 In clinical isolates of H. influenzae, RIFr single mutations mapped to cluster I of the RRDR, with changes at Asp516 predominating; a strain with intermediate susceptibility had a mutation in cluster II.51 Single-site mutations in invasive isolates of S. pneumoniae from Taiwan were aligned as Asp516Val and His526Tyr.52 Different amino-acid changes at the same two residues, Asp516Glu and His526Asn, were found in RIFr pneumococcal isolates from South Africa.53
Rhodococcus equi, an intracellular organism that causes life-threatening infections in young foals and opportunistic infections in immunocompromised humans, is often treated with RIF combination therapy. RIFr mutations in this species have included Ser531Leu/Trp and several different amino-acids substitutions at consensus codon 526.54, 55
Intrinsic and polymerase-independent resistance to RIF
Low-level RIF resistance in various organisms, including mycobacteria, has been suggested to involve permeability or efflux/influx56 and a plasmid-mediated efflux mechanism has been reported in a strain of Pseudomonas fluorescens.57 These will not be reviewed as their clinical implications are not evident. Relatively high RIF MICs in Enterobacteriaceae and other non-fastidious Gram-negative bacteria, determined by long or abundant outer membrane lipopolysaccharide chains, will also not be discussed.
A few species of bacteria are intrinsically non-susceptible to RIF because of a refractory RNAP. Treponema spp. and other spirochetes, including members of the genera Borrelia and Leptospira, are in this category, as are many strains of soil actinomycetes; resistance in these organisms correlates with the amino-acid naturally present at consensus codon 531 in rpoB: Asn substituting for the Ser of susceptible bacteria.58, 59 Another group of bacteria that are intrinsically non-susceptible to RIF are the mollicutes, which include Mycoplasma, Ureaplasma and Spiroplasma species. Sequencing of the rpoB gene of Spiroplasma citri indicated that the presence of Asp at the consensus residue 526, instead of the His present in susceptible species, is the determinant of resistance; Asp is also present at this residue in various Mycoplasma species.60 Among Rickettsia there is a cluster of naturally RIFr spotted fever group species; the relationship between the rpoB mutation identified and the consensus sequence is not evident.61 A variation on this theme has been reported in the opportunistic pathogen, Nocardia farcinica: the presence of a second gene, homologous to rpoB, termed rpoB2 or rpoBR, which encodes a RIF-refractory β subunit.62 An rpoB2 paralog reportedly occurs in a number of actinomycetes, and in a Nonomuraea sp. the two paralogs are expressed under different physiological conditions; in the latter organism the expression of rpoB2, in stationary phase, is associated with secondary metabolism.63
There are a few examples of inactivation of RIF, mainly in bacterial species that are not its therapeutic targets and associated with low-level resistance These include glucosylation, ribosylation, phosphorylation and decolorization, the latter because of a monooxygenase.64, 65 A monooxygenase has been identified as a secondary resistance mechanism in N. farcinica, revealed when its rpoB2 was deleted.66 The gene for an enzyme (termed ARR-2) capable of ADP-ribosylating RIF has been identified on an integron in a Pseudomonas aeruginosa strain.67
Cross-resistance among RNAP inhibitors
Rifamycins
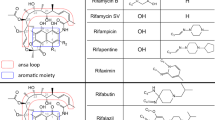
There are currently five rifamycins marketed in various countries: rifamycin SV (with limited availability); RIF, rifapentine and rifabutin (all three mainly utilized for the systemic treatment of mycobacterial infections) and rifaximin (indicated for travelers’ diarrhea). Rifalazil, a sixth rifamycin has been in development for a number of years for various indications. Although there is clinical evidence that the relapse and acquired resistance rates in tuberculosis patients treated with RIF or rifabutin are similar,68 there have been a number of reports suggesting incomplete cross-resistance between rifabutin, RIF and rifapentine. For example, M. tuberculosis RIFr clinical isolates with the rpoB mutations Asp516Val, Asp516Tyr and Leu533Pro69 and Ser522Leu70 were reported to be susceptible to rifabutin. However, in E. coli, mutant RNAPs with Asp516Val (as well as Asp516Asn), Leu533Pro and a different mutation at residue 522 (Ser to Phe) were resistant to all three rifamycins.19 The Asp516Asn RNAP from E. coli was also resistant to all three compounds in a cell-free transcription assay.19 Complete cross-resistance among RIF, rifapentine and rifabutin was also reported in sequenced rpoB mutants of S. aureus.44 It should be noted that the MICs of rifabutin for the M. tuberculosis isolates in question are at the upper end (0.5 μg ml–1) of what has been considered its susceptibility limit. Current thinking is that this breakpoint is too high and that, in the absence of clinical evidence to the contrary, the isolates in question should be considered resistant to rifabutin.71, 72
Other inhibitors of RNAP
Fidaxomicin (lipiarmycin), a macrocyclic antibiotic, is the only marketed non-rifamycin that inhibits bacterial RNAP; it is not cross-resistant with RIF. It acts at the initiation step of transcription but, unlike RIF, it requires core enzyme plus σ factor for optimal inhibitory activity in cell-free transcription assays.73, 74 Kurabachew et al.75 sequenced rpoB and rpoC from a set of lipiarmycin-resistant strains of M. tuberculosis. They identified two codons in rpoB distal to the RRDR that specified various amino-acid changes in the β subunit and two mutations in rpoC specifying changes in β′.
Sorangicin A, a macrolide polyether, also inhibits the initiation step of transcription. In E. coli, it is partially cross-resistant with RIF.19, 76, 77 Two studies19, 76 examined the effects of known amino-acid changes in the β subunit on the extent to which bacterial growth was inhibited by RIF and sorangicin. There is some difference between the two studies regarding the effect of certain mutations on cross-resistance; however, the two sets of mutants were not identical. The study by Xu, et al.19 also compared the extent of inhibition of transcription by both antibiotics in a cell-free assay; inhibition of the mutant RNAPs correlated with growth inhibition of the mutants.
Streptolydigin, a tetramic acid antibiotic that inhibits elongation of transcripts, is not cross-resistant with RIF.19, 21 Although most mutations to streptolydigin resistance map in rpoB, they are found mainly in the spacer region between clusters I and II of the RRDR.21, 78 Mutations in rpoC, encoding the β′ subunit, have also been identified.79, 80
Pleiotropic effects of RIFr mutations
Transcription is a complex, intricately regulated process in which initiation at specific promoters, pausing and termination involve the transient interaction of RNAP core enzyme with other subunits such as σ factors, small molecules, DNA sequences and the transcript RNA itself. RIF has been an important tool in probing bacterial physiology because RIFr mutations affect a number of phenotypes. As summarized by Jin and Gross,81 some of the mutations in E. coli determine temperature-dependent growth; affect the stability of plasmids, the growth of bacteriophages and susceptibility to other inhibitors; and affect phenotypes associated with mutations in other subunits or enzymes. One important effect of some RIFr mutations is on the expression of termination/anti-termination including: the bacteriophage λ N anti-termination function involved in the transcription of late genes; and the cell’s stringent response that regulates transcription of stable RNAs and other stringently controlled genes and is normally controlled by the ρ termination factor and ppGpp.82, 83, 84
Other examples of effects associated with RIFr mutations are: control of sporulation, germination, cell shape and metabolism in B. subtilis;85, 86, 87 abnormal termination at the tryptophan operon attenuator in E. coli;88 alteration of nutritional requirements in Lactobacillus casei;89 activation of silent genes and upregulation of antibiotic production in some actinomycetes.90 There have also been numerous studies in various organisms of the fitness and virulence of RIFr mutants and of adaptation by means of secondary mutations.
Conclusions
RIF is a valuable antibiotic for the treatment of mycobacterial and other diseases; the emergence of resistance during therapy can generally be avoided with the use of adequate combination therapy. The clinically significant resistance mechanism is mutation within a defined region of the rpoB gene, which encodes the target of RIF, the β subunit of bacterial RNAP. The portion of this sequence defined as cluster I is particularly important for high-level resistance. As a result of the high degree of conservation of RNAP, including this region of β, the mutations that determine resistance are also conserved across species. In RIFr clinical isolates of various organisms, mutations are most often found in three specific codons of the consensus sequence, and the Ser531Leu substitution in β predominates in mycobacteria and some other species. Cross-resistance appears to be complete among the rifamycins currently used to treat mycobacterial diseases. For these reasons, it has been possible to develop PCR-based tests to rapidly identify resistant M. tuberculosis. Intrinsic resistance in a few bacterial genera is also determined by the amino acids naturally present at residues 531 or 526 of the consensus sequence. Partial cross-resistance has been reported to another class of RNAP inhibitor, sorangicin A. RIFr mutations can have profound effects on transcription rate, initiation, pausing and termination. As a result of the central role played by RNAP in the bacterial cell, RIFr mutations often affect a number of physiological processes. RIF itself and RIFr mutations have been of great importance in elucidating the structure and function of RNAP and its complex role in the regulation of gene expression.
References
David, H. L. Probability distribution of drug-resistant mutants in unselected populations of Mycobacterium tuberculosis. Appl. Microbiol. 20, 810–814 (1970).
Schneider, H., Dobek, A. S. & Artenstein, M. S. Mutation of gonococci and meningococci in vitro to rifampin (rifampicin) resistance. Br. J. vener. Dis. 48, 500–503 (1972).
O’Neill, A. J., Cove, J. H. & Chopra, I. Mutation frequencies for resistance to fusidic acid and rifampicin in Staphylococcus aureus. J. Antimicrob. Chemother. 47, 647–650 (2001).
Farrell, D. J. et al. In vitro activity and single-step mutational analysis of rifamycin SV tested against enteropathogens associated with traveler’s diarrhea and Clostridium difficile. Antimicrob. Agents Chemother. 55, 992–996 (2011).
Atlas, E. & Turck, M. Laboratory and clinical evaluation of rifampicin. Am. J. Med. Sci. 256, 47–54 (1968).
Malmborg, A. S., Molin, L. & Nyström, B. Rifampicin compared with penicillin in the treatment of gonorrhea. Chemotherapy 61, 319–325 (1971).
Beam, Jr. W. J., Newberg, N. R., Devine, L. F., Pierce, W. E. & Davies, J. A. The effect of rifampin on the nasopharyngeal carriage of Neisseria meningitidis in a military population. J. Infect. Dis. 124, 39–46 (1971).
Vall-Spinosa, A., Lester, W., Moulding, T., Davidson, P. T. & McClatchy, J. K. Rifampin in the treatment of drug-resistant Mycobacterium tuberculosis. New Engl. J. Med. 283, 616–621 (1970).
White, R. J., Lancini, G. C. & Silvestri, L. G. Mechanism of action of rifampicin on Mycobacterium smegmatis. J. Bacteriol. 108, 737–741 (1971).
Nitta, K., Mizuno, S., Yamazaki, H. & Umezawa, H. Streptovaricin- and rifamycin-resistance of RNA polymerase in a resistant clone of Escherichia coli B. J. Antibiot. 21, 521–522 (1968).
Wehrli, W., Knüsel, F., Schmid, K. & Staehelin, M. Interaction of rifamycin with bacterial RNA polymerase. Proc. Natl Acad. Sci. USA 61, 667–673 (1968).
Doi, R. H., Brown, L. R., Rodgers, G. & Hsu, Y. Bacillus subtilis mutant altered in spore morphology and in RNA polymerase activity. Proc. Natl Acad. Sci. USA 66, 404–410 (1970).
Rabussay, D. & Zillig, W. A rifampicin resistant RNA-polymerase from E. coli altered in the β-subunit. FEBS Lett. 5, 104–106 (1969).
Heil, A. & Zillig, W. Reconstitution of bacterial DNA-dependent RNA-polymerase from isolated subunits as a tool for the elucidation of the role of the subunits in transcription. FEBS Lett. 11, 165–168 (1970).
Halling, S. M., Burtis, K. C. & Doi, H. Reconstitution studies show that rifampicin resistance is determined by the largest polypeptide of Bacillus subtilis RNA polymerase. J. Biol. Chem. 25, 9024–9031 (1977).
Jin, D. J. & Gross, C. A. Mapping and sequencing of mutations in the Escherichia coli rpoB gene that lead to rifampicin resistance. J. Mol. Biol. 202, 45–58 (1988).
Ovchinnikov, Y. A. et al. The primary structure of Escherichia coli RNA polymerase. Nucleotide sequence of the rpoB gene and amino-acid sequence of the β-subunit. Eur. J. Biochem. 116, 621–629 (1981).
Ovchinnikov, Y. A. et al. Primary structure of Escherichia coli RNA polymerase. Nucleotide substitution in the β subunit gene of the rifampicin resistant rpoB255 mutant. Mol. Gen. Genet. 184, 536–538 (1981).
Xu, M., Zhou, Y. N., Goldstein, B. P. & Jin., D. J. Cross-resistance of Escherichia coli RNA polymerases conferring rifampin resistance to different antibiotics. Antimicrob. Agents Chemother. 187, 2783–2792 (2005).
Landick, R., Stewart, J. & Lee, D. N. Amino acid changes in conserved regions of the β-subunit of Escherichia coli RNA polymerase alter transcription pausing and termination. Genes Dev. 4, 1623–1636 (1990).
Severinov, K., Soushko, M., Goldfarb, A. & Nikiforov, V. Rifampicin region revisited. New rifampicin-resistant and streptolydigin-resistant mutants in the β subunit of Escherichia coli RNA polymerase. J. Biol. Chem. 28, 14820–14825 (1993).
Stender, W. & Scheit., K. H. Studies of the topography of the binding site of DNA-dependent RNA polymerase from Escherichia coli for the antibiotic rifamycin SV. Eur. J. Biochem. 76, 591–600 (1977).
Mustaev, A. et al. Topology of the RNA polymerase active center probed by chimeric rifampicin-nucleotide compounds. Proc. Natl Acad. Sci. USA 91, 12036–12040 (1994).
Severinov, K. et al. The β subunit Rif-cluster I is only angstroms away from the active center of Escherichia coli RNA polymerase. J. Biol. Chem. 270, 29428–29432 (1995).
Rothman-Denes, L. B. Structure of Escherichia coli RNA polymerase holoenzyme at last. Proc. Natl Acad. Sci. USA 110, 19662–19663 (2013).
Trinh, V., Langelier, M., Archambault, J. & Coulombe, B. Structural perspective on mutations affecting the function of multisubunit RNA polymerases. Microbiol. Mol. Biol. Rev. 70, 12–36 (2006).
Yamada, T., Nagata, A., Ono, Y., Suzuki, Y. & Yamanouchi, T. Alteration of ribosomes and RNA polymerase in drug-resistant clinical isolates of Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 27, 921–924 (1985).
Telenti, A. et al. Detection of rifampicin-resistance mutations in Mycobacterium tuberculosis. Lancet 341, 647–650 (1993).
Kapur, V. et al. Characterization by automated DNA sequencing of mutations in the gene (rpoB) encoding the RNA polymerase β subunit in rifampin-resistant Mycobacterium tuberculosis strains from New York City and Texas. J. Clin. Microbiol. 32, 1095–1098 (1994).
Musser, J. M. Antimicrobial agent resistance in mycobacteria: molecular genetic insights. Clin. Microbiol. Rev. 4, 496–514 (1995).
Ohno, H., Koga, H., Kohno, S., Takayoshi, T. & Hara, K. Relationship between rifampin MICs for and rpoB mutations of Mycobacterium tuberculosis strains isolated in Japan. Antimicrob. Agents Chemother. 40, 1053–1056 (1996).
Yang, B. et al. Relationship between antimycobacterial activities of rifampicin, rifabutin and KRM-1648 and rpoB mutations of Mycobacterium tuberculosis. J. Antimicrob. Chemother. 42, 621–628 (1998).
Pang, Y. et al. Study of the rifampin monoresistance mechanism in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 57, 893–900 (2013).
Taniguchi, H. et al. Rifampicin resistance and mutation of the rpoB gene in Mycobacterium tuberculosis. FEMS Microbiol. Lett. 144, 103–108 (1996).
Heep, M. et al. Frequency of rpoB mutations inside and outside the cluster I region in rifampin-resistant clinical Mycobacterium tuberculosis isolates. J. Clin. Microbiol. 39, 107–110 (2001).
Morlock, G. P., Plikaytis, B. B. & Crawford, K. T. Characterization of spontaneous, in vitro-selected rifampin-resistant mutants of Mycobacterium tuberculosis strain H37Rv. Antimicrob. Agents Chemother. 44, 3298–3301 (2000).
Billington, O. J., McHugh, T. D. & Gillespie, S. H. Physiological cost of rifampin resistance induced in vitro in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 43, 1866–1869 (1999).
Honore, N. & Cole, S. T. Molecular basis of rifampin resistance in Mycobacterium leprae. Antimicrob. Agents Chemother. 37, 414–418 (1993).
Williams, D. L. et al. Characterization of rifampin-resistance in pathogenic mycobacteria. Antimicrob. Agents Chemother. 38, 2380–2386 (1994).
Klein, J. L., Brown, T. J. & French, G. L. Rifampin resistance in Mycobacterium kansasii is associated with rpoB mutations. Antimicrob. Agents Chemother. 45, 3056–3058 (2001).
CDC. Availability of an assay for detecting Mycobacterium tuberculosis, including rifampin-resistant strains and considerations for use—United States, 2013. MMWR 62, 821–824 (2013).
Morrow, T. O. & Harmon, S. A. Genetic analysis of Staphylococcus aureus RNA polymerase mutants. J. Bacteriol. 137, 374–383 (1977).
Aubry-Damon, H., Soussy, C.-J. & Courvalin, P. Characterization of mutations in the rpoB gene that confer rifampin resistance in Staphylococcus aureus. Antimicrob. Agents Chemother. 42, 2590–2594 (1998).
Wichelhaus, T. A., Schäfer, V., Brade, V. & Böddinghaus, B. Molecular characterization of rpoB mutations conferring cross-resistance to rifamycins on methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 43, 2813–2816 (1999).
Wichelhaus, T. A. et al. Biological cost of rifampin resistance from the perspective of Staphylococcus aureus. Antimicrob. Agents Chemother. 46, 3381–3385 (2002).
O’Neill, A. J., Huovinen, T., Fishwick, C. W. G. & Chopra, I. Molecular genetic and structural modeling studies of Staphylococcus aureus RNA polymerase and the fitness of rifampin resistance genotypes in relation to clinical prevalence. Antimicrob. Agents Chemother. 50, 298–309 (2006).
Watanabe, Y., Cui, L., Katayama, Y., Kozue, K. & Hiramatsu, K. Impact of rpoB mutations on reduced vancomycin susceptibility in Staphylococcus aureus. J. Clin. Microbiol. 49, 2680–2684 (2013).
Villar, M. et al. Epidemiological and molecular aspects of rifampicin-resistant Staphylococcus aureus isolated from wounds, blood and respiratory samples. J. Antimicrob. Chemother. 66, 997–1000 (2011).
Stefanelli, P. et al. Rifampicin-resistant meningococci causing invasive disease: detection of point mutations in the rpoB gene and molecular characterization of the strains. J. Antimicrob. Chemother. 47, 219–222 (2001).
Carter, P. E., Abadi, F. J., Yakubu, D. E. & Pennington, T. H. Molecular characterization of rifampin-resistant Neisseria meningitidis. Antimicrob. Agents Chemother. 38, 1256–1261 (1994).
Cruchaga, S., Perez-Vázquez, M., Román, F. & Campos, J. Molecular basis of rifampicin resistance in Haemophilus influenzae. J. Antimicrob. Chemother. 52, 1011–1014 (2003).
Chen, J.-Y. et al. Mutations of the rpoB gene in rifampicin-resistant Streptococcus pneumoniae in Taiwan. N. Antimicrob. Chemother 53, 375–378 (2004).
Padayachee, T. & Klugman, K. P. Molecular basis of rifampin resistance in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 43, 2361–2365 (1999).
Fines, M., Pronost, S., Maillard, K., Taouji, S. & Leclercq, R. Characterization of mutations in the rpoB gene associated with rifampicin resistance in Rhodococcus equi isolated from foals. J. Clin. Microbiol. 39, 2784–2787 (2001).
Asoh, N. et al. Emergence of rifampin-resistant Rhodococcus equi with several types of mutations in the rpoB gene among AIDS patients in northern Thailand. J. Clin. Microbiol. 41, 2337–2340 (2003).
Louw, G. E. et al. A balancing act: efflux/influx in mycobacterial drug resistance. Antimicrob. Agents Chemother. 53, 3181–3189 (2009).
Chandrasekaran, S. & Lalithakumari, D. Plasmid-mediated rifampicin resistance in Pseudomonas fluorescens. J. Med. Microbiol. 47, 197–200 (1998).
Stamm, L. V., Bergen, H. L. & Shangraw, K. A. Natural rifampin resistance in Treponema spp. correlates with presence of N531 in RpoB cluster I. Antimicrob. Agents Chemother. 45, 2973–2974 (2001).
Kim, H. et al. Mechanism of natural rifampicin resistance of Streptomyces spp. Syst. Appl. Microbiol. 28, 398–404 (2005).
Garivaud, P., Laigret, F. & Bove., J. M. Insusceptibility of members of the class Mollicutes to rifampin: Studies of the Spiroplasma citri RNA polymerase β-subunit gene. Antimicrob. Agents Chemother. 40, 858–862 (1996).
Drancourt, M. & Raoult, D. Characterization of mutations in the rpoB gene in naturally rifampin-resistant Rickettsia species. Antimicrob. Agents Chemother. 43, 2400–2403 (1999).
Ishikawa, J., Chiba, K., Kurita, H. & Satoh, H. Contribution of rpoB2 RNA polymerase β subunit gene to rifampin resistance in Nocardia species. Antimicrob. Agents Chemother. 50, 1342–1346 (2006).
Talà, A. et al. Activation of dormant bacterial genes by Nonomuraea sp. strain ATCC 39727 mutant-type RNA polymerase. J. Bacteriol. 191, 805–814 (2009).
Tupin, A. et al. Resistance to rifampicin: at the crossroads between ecological, genomic and medical concerns. Int. J. Antimicrob. Agents 35, 519–523 (2010).
Anderson, S. J., Quan, S., Gowan, B. & Dabbs, E. R. Monooxygenase-like sequence of a Rhodococcus equi gene conferring increased resistance to rifampin by inactivating this antibiotic. Antimicrob. Agents Chemother. 41, 218–221 (1997).
Hoshino, Y. et al. Monooxygenation of rifampicin catalyzed by the rox gene product of Nocardia farcinica: structure elucidation, gene identification and role in drug resistance. J. Antibiot. 63, 23–28 (2010).
Tribuddharat, C. & Fennewald, M. Integron-mediated rifampin resistance in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 43, 960–962 (1999).
Li, J., Munsiff, S. S., Driver, C. R. & Sackoff, J. Relapse and acquired rifampin resistance in HIV-infected patients with tuberculosis treated with rifampin- or rifabutin-based regimens in New York City, 1997-2000. Clin. Infect. Dis. 41, 83–91 (2005).
Casavoglu, C., Karaca-Derici, Y. & Bilgic, A. In-vitro activity of rifabutin against rifampicin-resistant Mycobacterium tuberculosis isolates with known rpoB mutations. Clin. Microbiol. Infect. 10, 662–665 (2004).
Jamieson, F. B. et al. Profiling of rpoB mutations and MICs to rifampicin and rifabutin in Mycobacterium tuberculosis. J. Clin. Microbiol. 52, 2157–2162.
Ängeby, K., Juréen, P., Kahlmeter, G., Hoffner, S. E. & Schön, T. Challenging a dogma: antimicrobial susceptibility testing breakpoints for Mycobacterium tuberculosis. Bull. World Health Organ. 90, 693–698 (2012).
Schön, T. et al. Rifampicin-resistant and rifabutin-susceptible Mycobacterium tuberculosis strains: a breakpoint artefact? J. Antimicrob. Chemother. 68, 2074–2077 (2013).
Somma, S., Pirali, G., White., R. & Parenti, F. Lipiarmycin, a new antibiotic from Actinoplanes. III. Mechanism of action. J. Antibiot. 28, 247–252 (1975).
Sonenshein, A. L. & Alexander, H. B. Initiation of transcription in vitro is inhibited by lipiarmycin. J. Mol. Biol. 127, 55–72 (1979).
Kurabachew, M. et al. Lipiarmycin targets RNA polymerase and has good activity against multidrug-resistant strains of Mycobacterium tuberculosis. J. Antimicrob. Chemother. 62, 713–719 (2008).
Römmele, G. et al. Resistance of Escherichia coli to rifampicin and sorangicin A. J. Antibiot. 43, 88–91 (1990).
Campbell, E. A. et al. Structural, functional and genetic analysis of sorangicin inhibition of bacterial RNA polymerase. EMBO J. 24, 674–682 (2005).
Heisler, L. M., Suzuki, H., Landick, R. & Gross, C. A. Contiguous amino acids define the target for streptolydigin resistance in the β subunit of Escherichia coli RNA polymerase. J. Biol. Chem. 268, 26369–26375 (1993).
Severinov, K. et al. Streptolydigin-resistant mutants in an evolutionarily conserved region of the β’ subunit of Escherichia coli RNA polymerase. J. Biol. Chem. 270, 23926–23929 (1995).
Yang, X. & Price, C. W. Streptolydigin resistance can be conferred by alterations to either the β or β’ subunits of Bacillus subtilis RNA polymerase. J. Biol. Chem. 270, 23930–23933 (1995).
Jin, D. J. & Gross, C. A. Characterization of the pleiotropic phenotypes of rifampin-resistant rpoB mutants of Escherichia coli. J. Bacteriol. 171, 5229–5231 (1999).
Jin, D. J. et al. Effects of rifampicin resistant rpoB mutations on antitermination and interaction with nusA in Escherichia coli. J. Mol. Biol. 204, 247–261 (1988).
Little, R., Ryals, J. & Bremer, H. rpoB mutation in Escherichia coli alters control of ribosome synthesis by guanosine tetraphosphate. J. Bacteriol 154, 787–792 (1983).
Zhou, Y. N. & Jin, D. J. The rpoB mutants destabilizing initiation complexes at stringently controlled promoters behave like ‘stringent’ RNA polymerases in Escherichia coli. Proc. Natl Acad. Sci. USA 95, 2908–2913 (1998).
Sonenshein, A. L., Cami, B., Brevel, J. & Cole, R. Isolation and characterization of rifampin-resistant and streptolydigin-resistant mutants of Bacillus subtilis with altered sporulation properties. J. Bacteriol. 120, 253–265 (1974).
Doi, R. H., Brown, L. R., Rodgers, G. & Hsu, Y. Bacillus subtilis mutant altered in spore morphology and in RNA polymerase activity. Proc. Natl Acad. Sci. USA 66, 404–410 (1970).
Perkins, A. E. & Nicholson, W. L. Uncovering new metabolic capabilities of Bacillus subtilis using phenotypic profiling of rifampin-resistant rpoB mutants. J. Bacteriol. 190, 807–814 (2007).
Yanofsky, C. & Horn, V. Rifampin resistance mutations that alter the efficiency of transcription termination at the tryptophan attenuator. J. Bacteriol. 145, 1334–1341 (1981).
Morishita, T. & Yura, T. Altered nutritional requirements associated with mutations affecting the structures of ribonucleic acid polymerase in Lactobacillus casei. J. Bacteriol. 125, 416–422 (1976).
Tanaka, Y. et al. Activation and products of the cryptic secondary metabolite biosynthetic gene clusters by rifampin resistance (rpoB) mutations in actinomycetes. J. Bacteriol. 195, 2959–2970 (2013).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goldstein, B. Resistance to rifampicin: a review. J Antibiot 67, 625–630 (2014). https://doi.org/10.1038/ja.2014.107
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2014.107
This article is cited by
-
Profile and resistance levels of 136 integron resistance genes
npj Antimicrobials and Resistance (2023)
-
High-resolution landscape of an antibiotic binding site
Nature (2023)
-
Amino acid substitutions in the region between RpoB clusters II and III on rifampin susceptibility in Haemophilus influenzae
European Journal of Clinical Microbiology & Infectious Diseases (2023)
-
Statistical analysis of 914 Mycobacterium tuberculosis genomes reveals single nucleotide polymorphisms in the ponA1 gene associated with rifampicin resistance
The Nucleus (2023)
-
Accelerating the menaquinone-7 production in Bacillus amyloliquefaciens by optimization of the biosynthetic pathway and medium components
Systems Microbiology and Biomanufacturing (2023)