Abstract
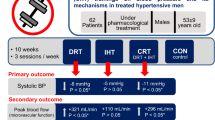
Isolated systolic hypertension (ISH) is the most common form of hypertension in older people. It is characterized by increased resting systolic blood pressure (sBP) and increased sBP in response to exercise. It has previously been shown that slow breathing training reduces resting sBP, and the objective of the present study was to determine whether it also reduced the blood pressure response to static handgrip exercise. ISH patients aged between 60 and 74 years were randomly divided into a control group (10 subjects, 4 of which were male) that breathed normally and a trained group (10 subjects, 4 of which were male) that trained daily for 8 weeks by slow breathing against an inspiratory resistance of 18 cmH2O. Before and immediately after training, subjects underwent a 2-min handgrip test (30% max) followed by 2 min of post-exercise circulatory occlusion (PECO) to assess metaboreflex activity. Training reduced sBP by 10.6 mm Hg (95% confidence interval (CI), −16 to −5 mm Hg, P=0.004), but changes were not observed in the control group. The peak exercise sBP was reduced by 23 mm Hg (95% CI, −16 to −31 mm Hg, P<0.001), while the increase in the sBP above resting was reduced by 12.6 mm Hg (95% CI, −6.9 to −18.2 mm Hg, P=0.002). The sBP during PECO was reduced by 8.9 mm Hg (95% CI, −4 to −14 mm Hg, P=0.008), which is indicative of reduced metaboreflex activity; no such change was observed in the control group. The results demonstrate that conventional treatment of older patients with ISH may be improved in two ways by slow breathing training: resting sBP may be reduced by 10 mm Hg, more than can be achieved by conventional pharmacological therapies, while the response to static exercise may be reduced by approximately twice this value.
Similar content being viewed by others
Introduction
Isolated systolic hypertension (ISH) presents with a high systolic blood pressure (sBP) but a relatively low diastolic blood pressure (dBP), thus giving rise to a high pulse pressure.1 ISH is particularly prevalent among older people, affecting more than 50% of individuals over the age of 60 years,2, 3 and it is a major cause of stroke as well as cardiovascular and kidney disease.4, 5 Despite the high level of risk, more than 60% of patients with ISH have poorly controlled blood pressure and fail to meet the target of 140/90 mm Hg6, 7 or a pulse pressure of 50 mm Hg. In addition, patients with ISH, even those with a well-controlled resting blood pressure, have abnormally high sBP responses to both moderate dynamic exercise and static handgrip contractions8 that could exacerbate the problems associated with a high resting sBP.
There have been a number of studies on slow breathing training in patients with essential hypertension that have reported reductions in resting blood pressure that are comparable to those achieved by exercise training.9, 10, 11, 12, 13, 14 It has also been shown that slow breathing training in patients with essential hypertension reduces the blood pressure response to static handgrip exercise.15
Although the underlying causes of essential hypertension and ISH are probably different, we recently published a study on the effects of slow breathing training on resting blood pressure in well-managed ISH patients that showed significant decreases in resting blood pressure, which was measured at home, over a 8-week training period.16 The effects were greater when breathing with an inspiratory load than without a load, and sBP remained significantly lower than pretraining levels for up to 6 weeks after the end of training. In a study of slow breathing training in patients with essential hypertension,15 we found that the pressor response to hand grip exercise was reduced. Although ISH and essential hypertension are thought to be different conditions, the fact that slow breathing training reduced resting blood pressure in both patient populations raises the interesting question of whether slow breathing training could also reduce the blood pressure response to exercise in patients with ISH.
The primary objective of this study was, therefore, to determine whether any reductions in resting blood pressure were accompanied by reductions in the blood pressure response to static handgrip exercise. The secondary objective was to determine to what extent the reduction in the blood pressure response to exercise might be due to a reduction in metaboreflex activity by measuring the pressure sustained during post-exercise circulatory occlusion (PECO).
The study presented here involved home-based blood pressure measurements in which the participants were randomized into three groups: those undergoing slow breathing training with an added inspiratory load, those undergoing slow breathing training without an added load and a control group; those data have been reported elsewhere.16 Both training groups showed significant reductions in sBP relative to a pretraining run-in period and relative to the control group. The loaded breathing training resulted in the greatest reductions in sBP, and importantly, the effects were sustained for several weeks after the training. Therefore, slow-loaded breathing training appears to be the most promising non-pharmacological approach for the management of age-related ISH. This paper reports data concerning the pressor response to handgrip exercise from patients in the loaded breathing training group and in the control group.
Methods
Participants
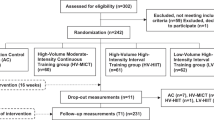
Patients being managed for ISH were recruited from the hypertension clinics in Srinagarind Hospital and three community hospitals in Khon Kaen Province, Thailand. The inclusion criteria were a diagnosis of mild-to-moderate ISH, which was defined as an average sBP>140 mm Hg and an average dBP<90 mm Hg1 at the time of recruitment; a patient age of over 60 years; and constant medication for at least 1 month prior to the study. Patients were excluded if they regularly exercised or had active cardiovascular disease, stroke, chronic renal failure or chronic respiratory disease. Thirty-five patients were screened and 5 were excluded; the remaining 30 were divided into three groups, and the results of two of the groups are reported here: the loaded breathing training group and the control group (these are the same subjects studied by Sangthong et al.16).
The study was approved by the Research Ethics Committee of Khon Kaen University, and all patients gave their informed consent in writing. The study was registered as a clinical trial (NCT 02200926).
Study design and interventions
The study was a prospective randomized trial with a 2-week run-in followed by 8 weeks of breathing training. Compliance with the breathing training was evaluated from the number of recorded training sessions on the patient’s checklist and the time and date information that was downloaded from the blood pressure monitor used for blood pressure and heart rate measurements.
Patients in the training group inspired against a load of 18 cmH2O with an inspiratory time of ~4 s and a total breath cycle of ~10 s. The training program was performed at home for 30 min a day every day for 8 weeks. No breathing instructions were given to the control group.
Patients reported to the laboratory for assessment before and immediately after the 8-week training period. Assessments consisted of resting blood pressure and heart rate measurement, followed by a static handgrip exercise test.
Static exercise pressor response
Subjects reclined in a comfortable chair with a hand dynamometer (Baseline; Irvington, NY, USA) in their right hand, with the elbow flexed and with the forearm supported on an arm rest. The maximum voluntary contraction force was measured as the best of three attempts. After 2 min of rest, subjects performed an isometric hand grip contraction at 30% maximum voluntary contraction for 2 min, based on protocols that have been used in a number of previous studies.15, 17, 18 The force produced during the 2-min contraction was closely monitored, and the subjects were encouraged to maintain a constant force throughout. Just before the end of the contraction, the patients’ circulation was occluded by a pressure cuff that was inflated around the upper arm to 250 mm Hg and maintained for 2 min for PECO. Then, the cuff was deflated, and the subject remained seated for another 2 min for recovery. Heart rate and blood pressure were measured from the left arm every minute during rest, isometric handgrip, PECO and recovery. Subjects were instructed to breathe normally during the test, avoiding any Valsalva maneuver, and breathing frequency was monitored by a plethysmography transducer (BiopacTM SS5 LB, Goleta, CA, USA) that was attached around the chest at the level of the xiphoid process. For data analyses, the two resting values were averaged, as were the two PECO and the two recovery measurements. The exercise value was the measurement taken after the second minute just before the end of exercise.
Outcome measures
Blood pressure
Blood pressure was measured using an automated oscillometric device (BSM-6701 bedside monitor, Nihon Kohden, Tokyo, Japan). An inflatable cuff was placed around each subject’s arm 1 inch above the elbow over the brachial artery. Because it takes 20–30 s to inflate the cuff and register a pressure, the procedure was started 30 s before the measurement was due to be made, and for the measurement at the end of the exercise the exercise was continued until a pressure was recorded. When measuring blood pressure, the arm was always supported on a cushion to reduce extraneous movement and vibration.
Heart rate
ECG electrodes (BiopacTM SS11LA, BIOPAC System) were attached in the lead II configuration and connected to the BIOPAC system. The heart rate was determined from the R-R interval.
Data analysis and statistics
Data were analyzed with a two-factor analysis of variance with replication, and when significant (P<0.05) group-by-time interactions were observed, post hoc Student’s t-tests with Bonferroni adjustments were used to identify differences. Data are reported as the mean±s.d. or s.e.m., or with a 95% confidence interval (CI), as appropriate.
Results
Patient characteristics
Details regarding the patients who completed the study and their medications are presented in Table 1. Although the patients’ blood pressures were well managed at the time of recruitment, the average resting systolic pressure was 171 mm Hg with a dBP of 80 mm Hg when they were first diagnosed, which is consistent with ISH. The compliance with breathing training was very good (92%). One subject was withdrawn from the home-based study16 because of missing blood pressure measurements, possibly as a result of his problems with alcohol, but as he was in the control group, not in the training group, and attended all of the laboratory sessions, he was included in this report. There were no differences in any of the cardiovascular measurements between the two groups during the pretraining visit to the laboratory (Table 2).
The effects of breathing training on resting blood pressure
The resting sBP values measured at the first visit to the laboratory (pretraining) and at the second visit at the end of the 8-week training period are reported in Table 2. For the subjects in the training group, there was an average decrease in resting sBP of 10.6 mm Hg (95% CI, −16 to −5 mm Hg; P=0.001); significant changes were not observed in the control group.
Resting diastolic pressure measurements from the pretraining and post-training visits are shown in Table 2. There was no difference in dBP between the two laboratory visits for either the breathing training group or the controls.
The decrease in pulse pressure after 8 weeks of training (10.3 mm Hg, 95% CI, −6 to −15; P=0.002) observed in the training group mirrored the decrease in sBP (Table 2); a significant change was not observed for the control group.
The resting heart rates of the patients in both groups were unchanged over the 8-week training interval (Table 2).
Exercise blood pressure responses
The maximum handgrip strength was 248±62 and 249±60 N for the control group and training groups before training and 244±59 and 249±57 N after the 8-week training period, respectively; therefore, the subjects were exerting not only the same relative forces but also the same absolute forces before and after the training period. All the subjects were able to maintain a constant force throughout the 2-min contraction. sBP increased throughout the 2-min isometric handgrip exercise; it decreased during PECO but remained above the resting value while the muscle was ischemic, and it then returned to baseline during the subsequent 2 min of recovery (Figures 1a and b). For the trained group, the systolic BP values were significantly lower (P⩽0.05) after training than pretraining at all time points, whereas significant differences were not observed in the control group. The mean value at rest, the peak value at the end of exercise and the mean value during PECO are shown in Figure 2a. Peak sBP (mean ±s.e.m.) at the end of exercise was 183±5.4 mm Hg pretraining and 160±2.9 mm Hg at the end of the 8-week training period. Comparable values were observed for the control group: 180±3.1 mm Hg pretraining and 182±2.6 mm Hg post training.
Blood pressure responses to a static handgrip test. (a) Systolic blood pressure of the trained group; (b) Systolic blood pressure of the control group. (c) Diastolic blood pressure of the trained group; (d) Diastolic blood pressure of the control group. Open circles indicate pretraining values; filled circles indicate post-training values; and open squares and dashed lines indicate values at the 8-week follow-up. Subjects contracted at 30% maximum voluntary contraction force for 2 min (Contract), followed by 2 min of post-exercise circulatory occlusion (PECO). Data are presented as the mean±s.e.m. *Significantly different compared to pretraining, P⩽0.05.
Systolic blood pressure (sBP) responses to handgrip exercise. (a) Data from Figures 1a, b showing the mean resting sBP (Rest), peak pressure at the end of exercise (End Ex) and the mean sBP during post-exercise circulatory occlusion (PECO). (b) sBP at End Ex and during PECO after subtracting the resting sBP values. Control group: pretraining, dark bars; and post training, open bars. Trained group: pretraining, cross-hatched bars; and post training, stippled bars. Data are presented as the mean±s.e.m. Significant differences between pretraining and post training are indicated by a; and significant differences between the trained and control groups are indicated by b.
The reduction in sBP at the end of exercise (23 mm Hg, 95% CI, −16 to−31, P<0.001) was only partly due to the decrease in resting sBP (10.6 mm Hg, 95% CI, −5 to −16). Figure 2b shows the sBP increase above the resting level at the end of exercise and during PECO. After training, the sBP at the end of exercise was reduced by 12.6 mm Hg (95% CI, −6.9 to −18.2, P=0.002). The sBP during PECO at the first visit was slightly higher in the training group than that in the control group, and there was no group-by-time interaction for the PECO measurement. However, within the trained group, there was a very clear reduction in the increase of sBP above resting levels both at the end of exercise and during PECO (P⩽0.001), and changes were not observed in the control group (Figure 3).
Changes in systolic blood pressure (sBP) response during exercise and post-exercise circulatory occlusion (PECO). Changes in the increase in sBP above resting as measured at the end of exercise and during PECO pretraining and post training. Control subjects are indicated by cross hatched bars; trained subjects are indicated by stippled bars. Data are presented as the mean±s.e.m. *Significantly different compared to pretraining and controls.
The increase of sBP above resting during PECO was positively correlated with the increase at the end of exercise (Figure 4). The trend line was forced through the zero intercept on the basis that if there was no rise in sBP above resting, then there cannot be a metaboreflex, and hence, no rise in sBP during PECO. It is notable that the coefficient of the correlation was essentially the same pretraining and post training (0.61 and 0.55, respectively; Figure 4a). For the control group (Figure 4b), the coefficients were, likewise, very similar for the pretraining and post-training period measurements (0.57 and 0.54, respectively).
Relationship between the increase in systolic blood pressure (sBP) above resting during post-exercise circulatory occlusion (PECO) and the rise at the end of exercise. (a) Trained subjects. (b) Control subjects. Filled symbols indicate measurements taken before the training period; and open symbols indicate measurements taken after training.
The dBP response to handgrip exercise is shown in Figures 1c and d. There were changes in resting dBP in both groups, but there was a tendency for the end exercise dBP to be lower in the trained group (96±6 mm Hg pretraining and 88±3 mm Hg post training; P=0.060); however, there was no change in the end-of-exercise dBP in the control group. The dBP maintained during PECO was reduced (by 7±3 mm Hg) as a result of training, but there was also a reduction in the dBP sustained during PECO in the control group without significant group-by-time interactions at any time point.
The patients’ heart rate increased by ~20 bpm at the end of exercise and fell rapidly after the end of exercise to values that were very close to resting. There were no significant group-by-time interactions for heart rate, and significant differences were not observed between the groups.
Discussion
ISH is the main form of hypertension in older people2, 3 and is often poorly controlled by conventional medication. Recently, we have shown that slow breathing is effective at reducing sBP in patients with ISH, according to home-based measurements,16 and the data reported here confirm these findings with laboratory-based measurements. However, while the reduction of resting blood pressure is important, it would also be very desirable to have a treatment that normalizes the excessive blood pressure response to exercise observed in patients with ISH, even in those whose blood pressures are well controlled with medication.8 The present study has shown that slow-loaded breathing training reduced not only resting blood pressure but also the blood pressure response to handgrip exercise.
The reduction in resting sBP of 10 mm Hg (Table 2) is a little less than that reported for the home-based measurements (15 mm Hg; Sangthong et al.16), but is still substantial compared with the reductions of 6–10 mm Hg that have been reported for inspiratory training in patients with essential hypertension,9, 10, 11, 12, 13, 14 reductions of ~4 mm Hg after various forms of aerobic exercise training19 and reductions of 5–7 mm Hg after isometric training.20, 21 The 10 mm Hg reduction in pulse pressure (Table 2) is clinically important, since large fluctuations in blood pressure may be as harmful as high absolute levels.22
These findings indicate that conventional pharmaceutical treatments that would normally be considered effective at managing patients with ISH are not, in fact, reducing resting systolic and pulse pressures as far as possible.
We have previously demonstrated that even well-managed patients with ISH have higher sBP responses to exercise, including moderate dynamic exercise and static handgrip contraction, than do age-matched normotensive subjects.8 This is an additional risk factor since raised blood pressures at rest, during exercise and during recovery are all prognostic for stroke,23 and raised blood pressure during exercise can exacerbate problems with cardiac function since left ventricular hypertrophy is a common complication of ISH.22, 24
The present results show that sBP during exercise was reduced following slow-loaded breathing training. The reduction was due, in part, to a lower initial resting blood pressure, but the increment above resting was also significantly and substantially reduced (Figure 3). This increment is thought to have at least two components. One component decreases rapidly at the end of exercise, but the other is sustained as long as the blood flow to the muscle remains occluded. It has long been argued that the blood pressure increase above resting seen during PECO is the consequence of a metaboreflex,25, 26 arising from the extracellular accumulation of metabolites and from potassium that is trapped in the ischemic muscle. The muscle metaboreflex has been shown to be overactive in hypertensive subjects17, 18 and is thought to reflect changes in autonomic blood pressure control. It is, therefore, a little surprising that it should be so evident in patients with ISH since the main problem with this age-related disorder is considered to be a stiffening of the conduit arteries.27
The coefficients of correlation shown in Figure 4 indicate that in the pretraining state, the sBP during PECO, which is presumed to reflect the metaboreflex, contributes to 55–60% of the sBP rise at the end of exercise, with almost identical results for the trained and control groups. After the training period, sBP decreased both at the end of exercise and during PECO (Figure 3), but the relationship between the two remained the same as that during the pretraining state (Figure 4a). Three of the subjects in the trained group had particularly high metaboreflex values during the pretraining phase, but the reduction in mean metaboreflex shown in Figures 2 and 3 was not solely due to these three individuals since all but one of the subjects in the trained group showed reductions in metaboreflex values after training. Thus, the training reduced both the metaboreflex and non-metaboreflex components of the sBP rise at the end of exercise to the same extent. These results do not indicate the nature of the non-metaboreflex portion of the sBP response during exercise, but two possibilities include a mechano-reflex response to the pressure within the contracted muscle28, 29 and increased stiffness of the conduit arteries,27 which could lead to increased sBP as cardiac output increases.30
How slow-loaded breathing leads to reductions in resting blood pressure is not known. It may be that the enhanced blood pressure fluctuations that occur during slow breathing31 increase the activity of baroreceptors, which if constantly repeated over the course of 8 weeks of training, might lead to some central modification of the autonomic control of blood pressure. Although baroreceptors have generally been thought of as being concerned with only the short-term regulation of blood pressure, it is now clear that they form an important part of an integrated system of control that involves the renin-angiotensin system and Na excretion in the kidney.32, 33, 34 In this respect, there has been interest in exercise-associated changes in renin levels,35 but how these might relate to reductions in blood pressure or whether slow breathing training might have similar effects remains to be determined. There is also an association between inflammatory changes and stiff arteries,36 but it seems unlikely that slow breathing can modify inflammatory processes.
The decrease in metaboreflex activity as a result of training could be a result of either alterations in peripheral receptor sensitivity or the central responses of the autonomic nervous system. In the case of breathing training for essential hypertension, we have argued15 that a decreased exercise pressor response represents a central adaptation, since slow breathing training is unlikely to alter the peripheral receptors in the arm, the musculature of which is not involved in the breathing training. The same arguments apply to the present results; the reduction in the sBP response to exercise after slow-loaded breathing training must reflect a change in the central autonomic control of blood pressure during exercise. Exaggerated blood pressure responses to exercise have been associated with increased levels of inflammatory markers and decreased nitric oxide bioavailability;37 however, as mentioned above regarding resting blood pressure, it is difficult to see how slow-loaded breathing might affect these factors.
The implication of our results is that the patients studied here, and probably older patients with ISH in general, have multiple pathologies that affect resting blood pressure and the blood pressure response to exercise. Conventional pharmacological management is effective at reducing resting systolic and pulse pressure by 20–30 mm Hg, but we show here that it can be reduced by a further 10 mm Hg via slow-loaded breathing training. Slow-loaded breathing training also has the potential to reduce the exaggerated sBP response to exercise that is observed in patients with ISH, even those whose blood pressures are considered to be well controlled by conventional pharmacological treatments.
Limitations
One methodological limitation of this study is that we used an oscillometric device to measure blood pressure. These devices provide estimates of systolic and diastolic pressure rather than direct measurements such as those obtained from an arterial line. The other problem is that there is a degree of uncertainty as to the precise timing of the measurement, as the cuff first inflates and then slowly deflates. This may be a factor contributing to the variation in the measurement of blood pressure at the end of exercise when the pressure is increasing, but it is unlikely to be a major problem during PECO when blood pressure is relatively constant. Nevertheless, these reservations to not appear to be too serious, since the values we obtained for normotensive subjects at the end of exercise in a related study8 were very similar to those reported in the original study of Alam and Smirk25 as well as those reported in more recent work17, 18 in which beat-by-beat measurements were taken from a finger cuff or an arterial line.38
In summary, the laboratory study results presented here for patients with ISH confirm the findings of the home-based blood pressure measurement study, which showed that slow-loaded breathing training reduces resting systolic blood to a clinically significant extent. Furthermore, it has been shown that breathing training reduces the blood pressure responses to static exercise and that this is, in large part, owing to a decrease in metaboreflex activity. Whether breathing training also reduces arterial stiffness and the blood pressure response to dynamic exercise remains to be seen. The results from this relatively small study do not prove that slow-loaded breathing training is an effective treatment for ISH, but they provide a proof-of-principle and suggest that larger trials might be warranted.
References
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ,, National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Cohen DL, Townsend RR . Update on pathophysiology and treatment of hypertension in the elderly. Curr Hypertens Rep 2011; 13: 330–337.
Franklin SS, Jacobs MJ, Wong ND, L’Italien GJ, Lapuerta P . Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives: analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension 2001; 37: 869–874.
Lee H-Y, Oh B-H . Aging and arterial stiffness. Circ J 2010; 74: 2257–2262.
Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, Flack JM, Carter BL, Materson BJ, Ram CVS, Cohen DL, Cadet J-C, Jean-Charles RR, Taler S, Kountz D, Townsend R, Chalmers J, Ramirez AJ, Bakris GL, Wang J, Schutte AE, Bisognano JD, Touyz RM, Sica D, Harrap SB . Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens 2014; 32: 3–15.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ,, Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute, National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206–1252.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F,, Task Force for the Management of Arterial Hypertension of the European Society of Hypertension and the European Society of Cardiology. 2013 ESH/ESC Practice Guidelines for the Management of Arterial Hypertension. Blood Press 2014; 23: 3–16.
Ubolsakka-Jones C, Sangthong B, Aueyingsak S, Jones DA . Older women with controlled isolated systolic hypertension: exercise and blood pressure. Med Sci Sports Exerc 2016; 48: 983–989.
Anderson DE, McNeely JD, Windham BG . Regular slow-breathing exercise effects on blood pressure and breathing patterns at rest. J Hum Hypertens 2010; 24: 807–813.
Grossman E, Grossman A, Schein MH, Zimlichman R, Gavish B . Breathing-control lowers blood pressure. J Hum Hypertens 2001; 15: 263–269.
Jones CU, Sangthong B, Pachirat O . An inspiratory load enhances the antihypertensive effects of home-based training with slow deep breathing: a randomised trial. J Physiother 2010; 56: 179–186.
Logtenberg SJ, Kleefstra N, Houweling ST, Groenier KH, Bilo HJ . Effect of device-guided breathing exercises on blood pressure in hypertensive patients with type 2 diabetes mellitus: a randomized controlled trial. J Hypertens 2007; 25: 241–246.
Mahtani KR, Nunan D, Heneghan CJ . Device-guided breathing exercises in the control of human blood pressure: systematic review and meta-analysis. J Hypertens 2012; 30: 852–860.
Meles E, Giannattasio C, Failla M, Gentile G, Capra A, Mancia G . Nonpharmacologic treatment of hypertension by respiratory exercise in the home setting. Am J Hypertens 2004; 17: 370–374.
Jones CU, Sangthong B, Pachirat O, Jones DA . Slow breathing training reduces resting blood pressure and the pressure responses to exercise. Physiol Res 2015; 64: 673–682.
Sangthong B, Ubolsakka-Jones C, Pachirat O, Jones DA . Breathing training for older patients with controlled isolated systolic hypertension. Med Sci Sports Exerc 2016; 48: 1641–1647.
Delaney EP, Greaney JL, Edwards DG, Rose WC, Fadel PJ, Farquhar WB . Exaggerated sympathetic and pressor responses to handgrip exercise in older hypertensive humans: role of the muscle metaboreflex. Am J Physiol Heart Circ Physiol 2010; 299: H1318–H1327.
Greaney JL, Matthews EL, Boggs ME, Edwards DG, Duncan RL, Farquhar WB . Exaggerated exercise pressor reflex in adults with moderately elevated systolic blood pressure: role of purinergic receptors. Am J Physiol Heart Circ Physiol 2014; 306: H132–H141.
Whelton SP, Chin A, Xin X, He J . Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med 2002; 136: 493–503.
Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA . Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc 2014; 89: 327–334.
Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA . Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res 2016; 39: 88–94.
Pini R, Cavallini MC, Bencini F, Silvestrini G, Tonon E, De Alfieri W, Marchionni N, Di Bari M, Devereux RB, Masotti G, Roman MJ . Cardiovascular remodeling is greater in isolated systolic hypertension than in diastolic hypertension in older adults: the Insufficienza Cardiaca negli Anziani Residenti (ICARE) a Dicomano Study. J Am Coll Cardiol 2002; 40: 1283–1289.
Kurl S, Laukkanen JA, Rauramaa R, Lakka TA, Sivenius J, Salonen JT . Systolic blood pressure response to exercise stress test and risk of stroke. Stroke J Cereb Circ 2001; 32: 2036–2041.
Heesen WF, Beltman FW, May JF, Smit AJ, de Graeff PA, Havinga TK, Schuurman FH, van der Veur E, Hamer JP, Meyboom-de Jong B, Lie KI . High prevalence of concentric remodeling in elderly individuals with isolated systolic hypertension from a population survey. Hypertension 1997; 29: 539–543.
Alam M, Smirk FH . Observations in man upon a blood pressure raising reflex arising from the voluntary muscles. J Physiol 1937; 89: 372–383.
Fisher JP, White MJ . Muscle afferent contributions to the cardiovascular response to isometric exercise. Exp Physiol 2004; 89: 639–646.
Greenwald SE . Ageing of the conduit arteries. J Pathol 2007; 211: 157–172.
Carrington CA, Ubolsakka C, White MJ . Interaction between muscle metaboreflex and mechanoreflex modulation of arterial baroreflex sensitivity in exercise. J Appl Physiol (1985) 2003; 95: 43–48.
Fisher JP, Bell MPD, White MJ . Cardiovascular responses to human calf muscle stretch during varying levels of muscle metaboreflex activation. Exp Physiol 2005; 90: 773–781.
Shoemaker JK, Mattar L, Kerbeci P, Trotter S, Arbeille P, Hughson RL . WISE 2005: stroke volume changes contribute to the pressor response during ischemic handgrip exercise in women. J Appl Physiol (1985) 2007; 103: 228–233.
Davies LC, Colhoun H, Coats AJS, Piepoli M, Francis DP . A noninvasive measure of baroreflex sensitivity without blood pressure measurement. Am Heart J 2002; 143: 441–447.
DiBona GF . Neural control of the kidney: past, present, and future. Hypertension 2003; 41: 621–624.
Sleight P . A historical perspective on peripheral reflex cardiovascular control from animals to man. Exp Physiol 2014; 99: 1017–1026.
Thrasher TN . Baroreceptors, baroreceptor unloading, and the long-term control of blood pressure. Am J Physiol Regul Integr Comp Physiol 2005; 288: R819–R827.
Goessler K, Polito M, Cornelissen VA . Effect of exercise training on the renin-angiotensin-aldosterone system in healthy individuals: a systematic review and meta-analysis. Hypertens Res 2016; 39: 119–126.
Mattace-Raso FUS, Verwoert GC, Hofman A, Witteman JCM . Inflammation and incident-isolated systolic hypertension in older adults: the Rotterdam study. J Hypertens 2010; 28: 892–895.
Michishita R, Ohta M, Ikeda M, Jiang Y, Yamato H . An exaggerated blood pressure response to exercise is associated with nitric oxide bioavailability and inflammatory markers in normotensive females. Hypertens Res 2016; 39: 792–798.
Fisher JP, Seifert T, Hartwich D, Young CN, Secher NH, Fadel PJ . Autonomic control of heart rate by metabolically sensitive skeletal muscle afferents in humans. J Physiol 2010; 588: 1117–1127.
Acknowledgements
The study was supported by The National Research Council of Thailand, the Graduate School and Faculty of Associated Medical Sciences at Khon Kaen University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ubolsakka-Jones, C., Sangthong, B., Khrisanapant, W. et al. The effect of slow-loaded breathing training on the blood pressure response to handgrip exercise in patients with isolated systolic hypertension. Hypertens Res 40, 885–891 (2017). https://doi.org/10.1038/hr.2017.54
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.54
Keywords
This article is cited by
-
Effectiveness of Paced Breathing Guided by Biofeedback on Clinical and Functional Outcomes Patients with Chronic Obstructive Pulmonary Disease: An Uncontrolled Pilot Study
Applied Psychophysiology and Biofeedback (2023)