Abstract
In addition to high blood pressure (BP), BP variability has recently also been shown to increase cardiovascular events. The purpose of this study was to compare the effect of a fixed-dose combinations (FDCs) of valsartan/amlodipine and a valsartan- and amlodipine-free drug combination on 24-h BPV. A total of 85 patients aged 18 or older and with no exclusion criteria were enrolled; of the 85 patients, 43 used the FDCs valsartan/amlodipine (160/10 mg) and 42 used a free drug combination of valsartan 160 mg and amlodipine 10 mg. Twenty-four hour ambulatory BP monitoring (ABPM) was performed after office BP measurements. Mean hourly BP, all-day BP reduction, trough/peak (T/P) ratio and Smoothness Index (SI) were calculated from the 24-h ABPM data. These were calculated separately for all-day, daytime, nighttime and early morning periods. The hourly mean diastolic BP (DBP) at 0800 hours in the FDCs group was significantly higher compared with the free drug combination group in the 24-h BP chronogram (P=0.041). Decreases in the all-day, daytime, nighttime and early morning systolic BP (SBP) and DBP in patients using a free drug combination were significantly greater compared with the FDC group. The SI and T/P ratio of the all-day, daytime and nighttime systolic and diastolic were also significantly higher compared with the FDC group. In addition, nighttime DBP reduction and the SI of DBP were lower in the diabetic patients. A free drug combination of amlodipine and valsartan provides more effective and smooth SBP and DSP control compared with FDCs.
Similar content being viewed by others
Introduction
Hypertension (HT) is the most significant risk factor for preventable deaths worldwide. Blood pressure (BP) control is, therefore, of the greatest importance.1 However, while many patients in numerous countries are aware of their elevated BP and receive antihypertensive treatment, they fail to achieve target values. In addition, BP control is established with two or more antihypertensives in the majority of patients.2, 3 As the number of drugs needed to achieve target BP, compliance and adherence declines. Therefore, the concept of a combination of more than one antihypertensive in a single pill and its use in HT treatment became a reality. The use of a single pill fixed-dose combination (FDCs) can provide more effective BP control by increasing compliance and adherence.4, 5 A meta-analysis in 2010 established that FDCs increased compliance and adherence, but although there was an effective reduction in BP, it was not significant. That same meta-analysis also stated that randomized control studies regarding the long-term cardiovascular protective effectiveness of FDCs were inadequate. Clinical studies have generally compared FDCs with monotherapy or another FDCs. There have been relatively few studies of FDCs compared with the drugs in it given separately at different times (free drug combination).3 The few existing comparisons of FDCs and free drug combinations were performed with β blocker/diuretic, angiotensin-converting enzyme inhibitor (ACE)/diuretic or angiotensin II receptor blockers (ARBs)/diuretic, and the great majority were retrospective.3 No studies have compared the effectiveness of ARBs/calcium channel blocker (CCB) FDCs with a free drug combination. Yet the National Institute for Health and Clinical Excellence HT guideline, newly published in light of recent studies,2 recommends a CCB in combination with an ACE inhibitor or an ARBs.1
Valsartan is an orally active, specific and selective ARBs. Its effect begins 2 h after a single oral dose, with the peak effect appearing in 4–6 h and effectiveness lasting for 24 h.6 Amlodipine is an orally active dihydropyridine CCB. Effectiveness varies with age, but the maximum effect is observed in 4 h, and the antihypertensive effect lasts >24 h.7, 8
Recent studies have shown that high BP variability (BPV) is a cardiovascular risk factor. Valsartan and amlodipine in an FDCs is an antihypertensive drug that has recently been introduced. The Exforge Target Achievement study showed that the valsartan/amlodipine FDCs established good BP control in both the moderate and intensive treatment groups, is well tolerated and has a low side-effect profile.9 In its analysis of the ambulatory BP monitoring (ABPM) results, that study showed that the intensive group achieved better BP targets.10 Previous studies have compared valsartan/amlodipine FDCs with monotherapy,11 although none have compared it with a free drug combination. Target organ injury increases in patients with elevated BPV. In particular, nighttime BPV is a more important risk factor than daytime BPV.12, 13, 14, 15 In addition, a nocturnal reduction and sudden rise during waking is observed in the natural course of BP. This is known as the ‘morning surge.’ A rise in BP in the early morning hours in hypertensive patients leads to an increased occurrence of stroke, myocardial infarction and sudden cardiac death.16, 17 For that reason, in addition to keeping the BP within target range, there has also been a recent emphasis on establishing smooth BP control throughout the day.
In light of the data obtained from the ABPM records, various techniques have been evaluated to determine whether antihypertensive medications establish durable and smooth BP control. One technique is the trough/peak (T/P) ratio, which is calculated from the BP reduction recorded at the trough (just before the following dose) divided by the BP reduction recorded at the time of the peak effect, usually 2–8 h after the dose.18 However, because only a small part of the following 24-h period is considered in the T/P ratio, it is not sufficient for evaluating change over the day. Therefore, researchers developed the Smoothness Index (SI). The SI is obtained by dividing the average BP reduction for each hour over a 24-h period in a patient under the effect of antihypertensive medication (ΔH) by the s.d. of this average.19
We hypothesized that giving single-pill combinations of two antihypertensive agents, commonly called FDCs, would lead to different variations in 24-h ABPM compared with giving these two different antihypertensive agents separately (free drug combination) in the morning and evening. To confirm this, we planned to compare the effects on 24-h BP of an FDCs of valsartan/amlodipine and a valsartan- and amlodipine-free drug combination. We planned to evaluate the differences between average all-day, nighttime, daytime and early morning BP changes and reductions, T/P ratio and all-day, day and nighttime SI on the basis of data obtained from the 24-h ABPM records of the two groups. This made it possible to analyze the differences in BPV between a CCB and an ARBs in a fixed dose and the same drugs in the same doses administered separately.
Methods
Patients who were 18 years of age or older with no exclusion criteria and using FDCs valsartan/amlodipine (160/10 mg) or separate valsartan 160 mg and amlodipine 10 mg with routine monitoring at our HT clinic were included. A total of 85 patients were enrolled, 43 of whom were receiving the FDCs at 0900 hours and 42 of whom were taking valsartan 160 mg at 0900 hours and amlodipine 10 mg at 2100 hours. Patients were excluded from the study because of any of the following: secondary HT, cardiovascular complications, such as congestive heart failure, myocardial infarction, stroke or angina pectoris, cigarette and alcohol use, creatinine levels above 1.5 mg dl−1, pregnancy and breastfeeding, arrhythmia, incompatible ABPM cuff due to the circumference of the subject’s arm, psychiatric disease or drug use that might cause changes in BP (tri- and tetracyclic antidepressants, monoamine oxidase inhibitors, nonsteroidal anti-inflammatory drugs or corticosteroids).
Patients were selected following confirmation by the Karadeniz Technical University Ethical Committee that the study protocol conformed to the Second Helsinki Declaration. Patients were briefed regarding the study protocol and were enrolled after the informed consent forms had been completed.
Ambulatory BP monitoring and office BP measurement
Office BP was measured by a physician using a conventional mercury sphygmomanometer. Measurements were performed according to the JNC VII guidelines.20 Two measurements at 2-min intervals were carried out in a sitting position after 10 min of rest. Systolic BP (SBP) was measured as the point at which the first of two or more Korotkoff sounds were heard (onset of phase 1), and the disappearance of the Korotkoff sound (onset of phase 5) was used to define diastolic BP (DBP). The mean of the two measurements in a sitting position was taken into account in the efficacy analysis. These measurements were taken before the administration of the drug, ∼24±2 h after the last dose, and if possible, at the same hour during each visit.
Ambulatory BP was obtained by a Welch Allyn 6100 device (Medical Device Depot, Ellicott City, MD, USA). The monitor was applied at 09:00 hours±1 h. The cuff was fixed to the non-dominant arm, and the device was set to obtain automatic BP readings at 15-min intervals during the day (from 0600 to 2200 hours) and at 20-min intervals during the night (from 2200 to 0600 hours). The patient was then sent home with instructions to continue usual activities, to hold the relevant arm immobile at the time of measurement, to note in a diary any unusual events or a poor night of sleep and to return to the clinic 24 h later. BP monitoring was always performed over a working day. Before each monitoring, a few automatic BP readings were taken simultaneously with measurements provided by a mercury sphygmomanometer to ensure that the averages of the two sets of values did not differ by >±5 mm Hg.
Data analysis
Hourly average BP measurements over 24-h (at 15-min intervals by day and 20 min at night) and the s.d. were recorded for each patient. Hourly reductions in BP values were calculated as the difference between average BP values at each hour and average BP values at 0900 hours. In addition, daytime, nighttime and early morning reductions were calculated separately. Nighttime measurements were taken from 2200 to 0600 hours, daytime from 0600 to 2200 hours and early morning from 0600 to 2100 hours.
Peak changes were calculated by considering the interval between the second and sixth hours after drug intake. Trough changes were calculated by on-treatment BP values over the last 2 h of the monitoring period. Individual T/P ratio were obtained separately for each patient by dividing the BP change at the trough by the change at the peak. The T/P ratio was calculated based on 0900 hours in the FDCs group, whereas a separate T/P ratio was calculated for valsartan and amlodipine in the group in which these were administered separately. Two T/P ratio were calculated and averages taken based on the time of valsartan administration at 0900 hours and time of amlodipine administration at 2100 hours.
The average reduction in hourly BP over 24-h (ΔH) and the s.d. of that average were determined, and the SI was calculated by using the formula ΔH/s.d. This was calculated separately for all-day, nighttime and daytime intervals for all patients.
Statistical analysis
All statistical analyses were carried out using SPSS (Statistical Package for the Social Sciences) for Windows, version 13.0 (SPSS, Chicago, IL, USA). The compatibility with normal distribution was evaluated using the Kolmogorov–Smirnov test. Comparisons in groups with parametric conditions were performed using the Student’s t-test, while the Mann–Whitney U-test was used for groups with non-parametric conditions. Correlations were tested using the Spearman correlation analysis. Demographic and baseline characteristics were analyzed using the χ2 test. Repeated measurements were evaluated using analysis of variance. Data are expressed as the mean values (±s.d.) or percentages. Statistical significance was set at P<0.05.
Results
A total of 85 patients were included in the study, with 43 patients who used a fixed dose valsartan/amlodipine combination (27 female/16 male, mean age 59.28±11.91) and 42 patients who used valsartan and amlodipine separately (30 female/12 male, mean age 55.81±12.53). There was no difference between the groups in terms of baseline demographic characteristics and biochemical parameters (Table 1). Females represented 62.8% of patients in the FDCs group and 71.4% of patients in the free drug combination group. Diabetes mellitus was present in 11 (25.6%) of the FDCs group patients and 9 (22%) of the patients in the free drug combination group. The average office SBP and DBP were 148.14±23.35 and 87.79±16.66 mm Hg, respectively, in the FDCs group and 150.71±16.58 and 89.17±12.96 mm Hg in the free drug combination group. The duration of HT was 10.42±6.83 and 8.69±7.40 years, respectively, in the FDCs and free drug combination groups.
ABPM analysis
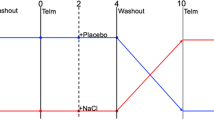
Average 24-h SBP and DBP were 121.19±14.2 and 68.83±9.30 mm Hg, respectively, in the FDCs group and 119.18±14.60 and 67.70±7.73 mm Hg, respectively, in the free drug combination group. Average daytime, nighttime and early morning SBP and DBP were 123.05±14.62 and 70.65±9.46, 117.47±16.00 and 65.18±9.93, and 127.02±13.74 and 74.84±9.78 mm Hg, respectively, in the FDCs group and 121.71±14.32 and 69.98±7.98, 114.3±16.77 and 63.14±8.47 and 125.15±13.52 and 72.54±7.77 mm Hg, respectively, in the free drug combination group, and there was no significant difference between the groups. The chronogram of the hourly average BP values >24 h is shown in Figure 1. There was no difference between the groups in terms of hourly average BP values throughout the day, but average DBP between 0 400 and 2100 hours was higher in the FDCs group, and there was a particularly statistically significant difference at 0800 hours (P=0.041). There was no significant difference between the two groups with regard to all-day, nighttime and daytime pulse pressure and heart rate.
Twenty-four-hour SBP and DBP average chronogram of the FDC and free drug combination groups. Average DBP between 0400 and 2100 hours was higher in the FDC group, and there was a statistically significant difference at 0800 hours. *Average DBP at 0800 hours of FDC vs. free drug combination P=0.041. A full color version of this figure is available at the Hypertension Research journal online.
BP reduction
The 24-h chronograms for the hourly reductions in SBP and DBP for the two groups are shown in Figure 2. As the figures show, hourly reductions (especially at night and early morning) were significantly greater in the free drug combination group. All-day SBP reductions in the FDCs and free drug combination groups were −2.58±9.29 and −8.51±9.07 mm Hg (P=0.004), respectively, and −4.25±5.13 and −7.29±4.07 mm Hg (P=0.003), respectively, for DBP (Figure 3). The daytime, nighttime and early morning reductions in SBP were significantly greater in the free drug combination group compared with subjects on an FDCs, with P-values of 0.01, 0.005 and 0.000, respectively. Daytime, nighttime and early morning DBP was significantly lower in the free drug combination group compared with the fixed dose group (P-values 0.08, 0.01 and 0.000, respectively).
T/P ratio
The T/P ratio for SBP was −0.54±2.50 in the FDCs group and 0.30±1.27 in the free drug combination group, and the difference was not significant. For DBP, the T/P ratio was −1.06±3.21 in the FDCs group and 0.40±0.60 (P=0.00) in the free drug combination group.
Smoothness index
The SI for decreases in SBP and DBP in both groups was calculated separately for all-day, nighttime and daytime. In the free drug combination group, the SI was significantly high for all-day, nighttime and daytime for both SBP and DBP (Figure 4). The all-day, daytime and nighttime SI of SBP in the FDCs group were 0.27±0.91, 0.08±0.98 and 0.83±1.45, respectively, whereas the daytime and nighttime SI of SBP were 0.95±1.07, 0.78±1.09 and 1.89±1.88, respectively, in the free drug combination group. The all-day, daytime and nighttime SI for DBP was 0.56±0.66, 0.37±0.74 and 1.11±1.20 for the FDCs group and 1.02±0.56, 0.87±0.68 and 2.07±1.25 for the free drug combination, all, respectively.
Decreases in BP and SI were correlated with age and duration of HT. There was a negative correlation between age and all-day, nighttime and early morning reduction in SBP (r=−0.234, P=0.031; r=−0.413, P=0.000; and r=−0.276, P=0.011, respectively). There was a negative correlation between the SI of all-day and nighttime SBP and age (r=−0.226, P=0.037 and r=−0.443, P=0.000, respectively). There was no correlation between the T/P ratio and age. There was no correlation between body mass index and decreases in SBP, the T/P ratio and the SI. The nighttime decrease in SBP and the SI of nighttime SBP were lower in patients with a greater duration of HT (r=−0.289, P=0.007; r=−0.257, P=0.018, respectively). The nighttime decrease in SBP and the SI of nighttime SBP were also lower in diabetic patients compared with non-diabetics (P=0.017 and P=0.008, respectively).
There was a negative correlation between all-day decreases in DBP, nighttime decreases in DBP, the SI of nighttime DBP and age (r=−0.236, P=0.030; r=−0.400, P=0.000; r=−0.365, P=0.001, respectively). There was no correlation with body mass index. There was a negative correlation between nighttime decreases in DBP and the SI of nighttime DBP in patients with a greater duration of HT, with P-values of 0.012 (r=−0.272) and 0.042 (r=−0.221), respectively. The nighttime decrease in the DBP and the SI of nighttime DBP were lower in diabetic patients compared with non-diabetics (P=0.023, 0.045).
Discussion
This study showed that a free drug combination of amlodipine (10 mg) and valsartan (160 mg) provided better all-day, daytime, nighttime and early morning reductions in SBP and DBP compared with the fixed dose valsartan/amlodipine (160/10 mg) group. In addition, the all-day, daytime and nighttime SI calculated for patients using the free drug combination was significantly higher. In addition, the T/P ratio for DBP was significantly higher in the free drug combination group. The SI for nighttime SBP and DBP and the decrease in BP in diabetic patients was significantly lower compared with non-diabetics. Our study shows for the first time that a free drug combination of amlodipine (10 mg) and valsartan (160 mg) provides smooth 24-h BP control and reduces early morning BP surges compared with fixed dose valsartan/amlodipine (160/10 mg).
The control of BP with antihypertensive medications reduces cardiovascular morbidity and mortality,1 but very few hypertensive patients achieve BP targets, despite receiving treatment. Many studies have shown that ⩾2 antihypertensive medications are needed to achieve target BP values.2, 3 As in other chronic diseases, patient compliance is very important in HT treatment. However, it is also a fact that as the number of medications increases, patient compliance decreases. The FDCs was produced with the aim of increasing patient compliance, and many studies have shown that FDCs use increases patient compliance compared with monotherapy. However, there are also studies showing that although the use of an FDCs increases patient compliance, the positive effects on BP control are less than expected.4, 5 FDCs exist for many antihypertensive drugs today. In light of HT guideline recommendations, diuretic combination treatments are used in the absence of contraindications in hypertensive patients requiring combination treatment.20 However, that advice has changed in recent years, particularly in the National Institute for Health and Clinical Excellence HT guideline published after the Avoiding Cardiovascular events through COMbination therapy in Patients LIving with Systolic Hypertension (ACCOMPLISH) study. ACCOMPLISH included 11 506 hypertensive patient with high cardiac risk, and despite determining a similar decrease in ambulatory and office BP, there was an increase of ⩾20% in the cardiovascular events that occurred in the group receiving benazepril+HCTZ compared with those receiving benazepril+amlodipine.21 The National Institute for Health and Clinical Excellence HT guideline recommended a combination of ACE or ARBs and a CCB in combination therapy. Valsartan and amlodipine in the form of a single pill FDCs are antihypertensive drugs that have entered use in recent years. The BP-lowering effect of this medication has been proved in several clinical studies.9, 11, 22 Although several studies have compared valsartan/amlodipine FDCs with monotherapy, none have compared it with a free drug combination. We analyzed fixed dose valsartan/amlodipine (160/10 mg) and an amlodipine (10 mg) valsartan (160 mg) free drug combination to determine the difference in effects on BP and 24-h BPV. Although we determined no distinct change in the hourly average SBP and DBP values, apart from at 0800 hours, we determined hourly decreases in all-day, nighttime and early morning BP in favor of the free drug combination.
The significance of the differences in BP measurement techniques (office, home and ABPM) in HT diagnosis has been intensively questioned, and in recent years, the diagnostic importance of ABPM in HT diagnosis and the evaluation of day-long variability has been emphasized.1, 13 In the first years when ABPM was used, decisions were made regarding antihypertensive medication efficacy on the basis of average all-day and nighttime BP and the T/P ratio. In recent years, however, because these parameters do not exactly reflect 24-h BPV, the need has arisen for new parameters to determine BPV. The SI entered into use on the basis of that idea.19 We also produced a SI and a T/P ratio to determine the 24-h BPV of the two drugs and established that both the SI and the T/P ratio were significantly high for both SBP and DBP in the free drug combination group.
In addition to high BP, BPV is correlated with distal organ injury and cardiovascular mortality.12, 13, 14, 15 Pierdomenico et al.12 showed an increase in cardiovascular event frequency in patients with high BPV compared with those with low variability. Another study in which a population of 8938 hypertensive patients (consisting of 2142 residents from Copenhagen, Denmark; 1124 subjects from Noorderkempen, Belgium; 1097 older men from Uppsala, Sweden; 244 subjects from Novosibirsk, the Russian Federation; 1312 inhabitants from Ohasama, Japan; 349 villagers from JingNing County, China; 1372 subjects from Montevideo, Uruguay; 165 subjects from Pilsen, the Czech Republic; 934 subjects from Dublin, Ireland; 310 subjects from Padova, Italy; and 308 subjects from Krakow, Poland) was evaluated with ABPM showed that variability was correlated with stroke, cardiovascular events and mortality.13 Eguchi et al.14 reported that higher BPV was correlated with cardiovascular events in diabetic patients. Therefore, antihypertensive medications that have a BPV-lowering effect may reduce distal organ injury and mortality in hypertensive patients. In our study, we observed that elevated BPV as determined by the calculation of SI and T/P ratio declined with the use of a free drug combination, and that smooth BP control was established in both the daytime and nighttime. Few studies have compared FDCs and a free drug combination.3 The great majority of such studies have compared a B blocker, an ACE inhibitor, ARBs with a diuretic or an ACE inhibitor with CCB FDCs and a free drug combination; studies have usually compared a free drug with combinations from the same group but not generally the same active substance. In addition, the majority were retrospective studies evaluating the BP-lowering effects of two groups.3 These studies showed that FDCs increased patient compliance and adherence by a level of 8%–19.6% compared with a free drug combination.3, 5 However, BP control was not analyzed in some studies that investigated FDCs compliance and adherence in HT treatment. In addition, in some of the studies in which this was evaluated, the expected BP control was not achieved, despite an increase in compliance and adherence.3 In addition to the number of drugs used, various factors, such as patient education and intellectual state, also affect compliance and adherence5 As the analysis of compliance and adherence was not the purpose of our study, it would not be appropriate to make a conclusion on the subject. However, further studies investigating how greater BPV in 24-h BP may influence patient compliance, and thus, the effect of BPV on compliance and adherence might be conducted.
In addition to all-day and nighttime BPV, early morning BP increase is also important in terms of correlation with mortality and morbidity.12, 13, 14, 15 In a meta-analysis by Cohen et al.,17 a strong correlation was reported between excessive early morning BP and sudden cardiac death and myocardial infarction. In our study, early morning BP values in the FDCs group were higher compared with the free drug combination group. We suggest that although antihypertensive effectiveness decreased in the FDCs (valsartan+amlodipine) group in the early morning hours, this efficacy persisted in the early morning hours in the free drug combination group. Therefore, a free drug combination provides smooth day-long BP control.
Many clinical studies have shown higher average SBP and DBP in type 1 diabetic patients compared with non-diabetics in 24-h ABPM and higher average nighttime DBP, especially in patients with microalbuminuria and left ventricular hypertrophy. Likewise, higher 24-h BP averages, both daytime and nighttime, and higher pulse, BP and pressure loads were described alongside the progression to more advanced degrees of diabetic nephropathy (microalbuminuria and macroalbuminuria) in type 2 diabetic patients.23 We also determined a smooth SBP and DBP course in non-diabetic patients compared with diabetics.
There are various limitations to this study in which we evaluate the effects on BPV of fixed dose valsartan/amlodipine (160/10 mg) and an amlodipine-(10 mg)-valsartan-(160 mg) free drug combination. The first is that ours is a sectional study. Second, the cardiovascular outcome of the decrease in BPV with a free drug combination could have been evaluated with long-term follow-up. Third, the pharmacodynamics of antihypertensive drugs can vary according to the time of administration. Therefore, it would have been important to also evaluate the effects of fixed dose valsartan/amlodipine administration at night and the bedtime administration of valsartan. However, bearing in mind the limited number of studies on the effect of FDCs compared with the free drug combination on BPV, our study can still shed light on the gap in the literature and pave the way for future long-term, prospective studies.
It is a fact that the use of FDCs in HT, a chronic disease, increases patient compliance and provides BP control. However, this study has also revealed the differing aspects of FDCs and free drug combination use. FDCs has the advantage, as shown in previous studies, of increasing patient compliance and adherence. However, BP control is smooth with a free drug combination. Therefore, the question of how to combine the advantages of FDCs and free drug combination use is an important one, and it is drug technology that will answer it. Hopefully, a future technology will be able to initiate the release of one drug contained in FDCs immediately and the second drug 12 h later, thus reducing the problems with the use of FDCs.
References
Krause T, Lovibond K, Caulfield M, McCormack T, Williams B . Guideline Development Group Management of hypertension: summary of NICE guidance. BMJ 2011; 343: d4891.
Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, Velazquez EJ, Staikos-Byrne L, Kelly RY, Shi V, Chiang YT, Weber MA . ACCOMPLISH Trial investigators Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet 2010; 375: 1173–1181.
Gupta AK, Arshad S, Poulter NR . Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension 2010; 55: 399–407.
Gerbino PP, Shoheiber O . Adherence patterns among patients treated with fixed-dose combination versus separate antihypertensive agents. Am J Health Syst Pharm 2007; 64: 1279–1283.
Schroeder K, Fahey T, Ebrahim S . How can we improve adherence to blood pressure-lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med 2004; 164: 722–732.
Markham A, Goa KL . Valsartan. A review of its pharmacology and therapeutic use in essential hypertension. Drugs 1997; 54: 299–311.
Leenen FH, Coletta E . Pharmacokinetic and antihypertensive profile of amlodipine and felodipine-ER in younger versus older patients with hypertension. J Cardiovasc Pharmacol 2010; 56: 669–675.
Radauceanu A, Boivin JM, Bernaud C, Fay R, Zannad FCIC General Practitioners Investigators’ Group Differential time effect profiles of amlodipine, compared to valsartan, revealed by ambulatory blood pressure monitoring, self blood pressure measurements and dose omission protocol. Fundam Clin Pharmacol 2004; 18: 483–491.
Oparil S, Giles T, Ofili EO, Pitt B, Seifu Y, Samuel R, Samuel R, Sowers JR . Moderate versus intensive treatment of hypertension with amlodipine/valsartan for patients uncontrolled on angiotensin receptor blocker monotherapy. J Hypertens 2011; 29: 161–170.
Giles TD, Oparil S, Ofili EO, Pitt B, Purkayastha D, Hilkert R, Samuel R, Sowers JR . The role of ambulatory blood pressure monitoring compared with clinic and home blood pressure measures in evaluating moderate versus intensive treatment of hypertension with amlodipine/valsartan for patients uncontrolled on angiotensin receptor blocker monotherapy. Blood Press Monit 2011; 16: 87–95.
Philipp T, Smith TR, Glazer R, Wernsing M, Yen J, Jin J, Schneider H, Pospiech R . Two multicenter, 8-week, randomized, double-blind, placebo-controlled, parallel-group studies evaluating the efficacy and tolerability of amlodipine and valsartan in combination and as monotherapy in adult patients with mild to moderate essential hypertension. Clin Ther 2007; 29: 563–580.
Pierdomenico SD, Lapenna D, Bucci A, Manente BM, Mancini M, Cuccurullo F, Mezzetti A . Blood pressure variability and prognosis in uncomplicated mild hypertension. Am Heart J 2005; 149: 934–938.
Hansen TW, Thijs L, Li Y, Boggia J, Kikuya M, Björklund-Bodegård K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O'Brien E, Staessen JA . International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators. Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension 2010; 55: 1049–1057.
Eguchi K, Ishikawa J, Hoshide S, Pickering TG, Schwartz JE, Shimada K, Kario K . Night time blood pressure variability is a strong predictor for cardiovascular events in patients with type 2 diabetes. Am J Hypertens 2009; 22: 46–51.
Zhang Y, Agnoletti D, Safar ME, Blacher J . Effect of antihypertensive agents on blood pressure variability: the Natrilix SR versus candesartan and amlodipine in the reduction of systolic blood pressure in hypertensive patients (X-CELLENT) study. Hypertension 2011; 58: 155–160.
Ohkubo T, Hozawa A, Nagai K, Kikuya M, Tsuji I, Ito S, Satoh H, Hisamichi S, Imai Y . Prediction of stroke by ambulatory blood pressure monitoring versus screening blood pressure measurements in a general population: the Ohasama study. J Hypertens 2000; 18: 847–854.
Cohen MC, Rohtla KM, Lavery CE, Muller JE, Mittleman MA . Meta-analysis of the morning excess of acute myocardial infarction and sudden cardiac death. Am J Cardiol 1997; 79: 1512–1516.
Omboni S, Parati G, Zanchetti A, Mancia G . Calculation of trough-to-peak ratio of antihypertensive treatment from ambulatory blood pressure: methodological aspects. J Hypertens 1995; 13: 1105–1112.
Parati G, Omboni S, Rizzoni D, Agabiti-Rosei E, Mancia G . The smoothness index: a new, reproducible and clinically relevant measure of the homogeneity of the blood pressure reduction with treatment for hypertension. J Hypertens 1998; 16: 1685–9121.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ . The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Jamerson K, Weber MA, Bakris GL, Dahlof B, Pitt B, Shi V, Hester A, Gupte J, Gatlin M, Velazquez EJ . Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 2008; 359: 2417–2428.
Allemann Y, Fraile B, Lambert M, Barbier M, Ferber P, Izzo JL . Efficacy of the combination of amlodipine and valsartan in patients with hypertension uncontrolled with previous monotherapy: the Exforge in Failure after Single Therapy (EX-FAST) study. J Clin Hypertens 2008; 10: 185–194.
Leitão CB, Canani LH, Silveiro SP, Gross JL . Ambulatory blood pressure monitoring and type 2 diabetes mellitus. Arq Bras Cardiol 2007; 89: 315–321.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ulusoy, S., Ozkan, G., Konca, C. et al. A comparison of the effects of fixed dose vs. single-agent combinations on 24-h blood pressure variability. Hypertens Res 35, 1111–1117 (2012). https://doi.org/10.1038/hr.2012.95
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2012.95