Abstract
The stiffness of large arteries has an important role in cardiovascular hemodynamics. Aortic stiffness (AoStiff) can be assessed non-invasively with regional and local methods. In this paper, we compared these two techniques for evaluating AoStiff. Our subjects comprised of 118 consecutive patients (85 men, mean age: 49±14 years). We evaluated regional AoStiff with carotid-femoral pulse wave velocity (PWV) measured with a tonometric technique and by bioelectrical impedance (BI) wave velocity (IWV). The local AoStiff was calculated from BI signals recorded at the chest. We used glyceryl trinitrate (GTN) to test the effect of peripheral vasodilatation on both methods in a subgroup of 52 patients (37 men, mean age: 52±11 years). We found a significant correlation between IWV and PWV measurements (r=0.88, P<0.0001) as well as between AoStiff and PWV measurements (r=0.75, P<0.0001). GTN administration decreased mean arterial blood pressure by 4% (95% confidence interval: 2–8%, P=0.002) without significant changes in AoStiff and regional IWV. Local AoStiff is correlated with regional measurements and is not influenced by changes in arterial pressure because of systemic peripheral vasodilatation.
Similar content being viewed by others
Introduction
The viscoelastic properties of large arteries have an important role in cardiovascular hemodynamics. Aortic stiffness (AoStiff) (that is, the loss of aortic viscoelastic properties) is a well-recognized independent predictor of cardiovascular mortality and morbidity1, 2, 3 and a surrogate marker of cardiovascular events in hypertension and end-stage renal failure.4
Current techniques measure AoStiff non-invasively by regional measurement of the pulse wave velocity (PWV) using tonometric techniques.4, 5 The pulse wave travels along the arterial wall at a speed related to the stiffness of the aorta6 and is influenced by the elastic modulus of its arterial wall (E), its radius (r) and its thickness (h).7 In practice, aortic PWV is determined between the carotid and the femoral artery, that is, where the pulse is palpable at the skin surface.8 The elastic and geometric properties of arteries (that is, E, r and h) are, however, heterogeneous along this segment.9, 10 As regional carotid-femoral PWV measurement integrates the stiffness of different arterial segments (that is, carotid, aorta, iliac and femoral), it should be regarded as a rough estimate of the local AoStiff.
The accuracy of regional methods could most likely be improved by local determination using dedicated techniques.11 Variables such as local PWV, arterial distensibility and Young's elastic modulus assess the local intrinsic properties of the arterial wall itself and are more closely related to the biomechanical characteristics of the artery.12, 13 However, because these local variables require cumbersome and/or specialized imaging technologies such as ultrasound imaging systems (that is, echo-wall-tracking) for the peripheral arteries and MRI for the aorta, their use is limited to research laboratories.5
We recently proposed a simple method for the evaluation of both local and regional AoStiff.14 It is based on the analysis of non-invasive changes in a bioelectrical impedance (BI) signal generated by the variation of blood volume conductivity in the arterial segment.15, 16 The regional AoStiff is determined by measuring the transit time of the impedance wave velocity (IWV in m s−1) between the chest and the thigh. The local AoStiff index can also be assessed from recordings performed at the level of chest.17, 18 We performed the present study to compare the local AoStiff estimated by the BI technique with the regional methods, PWV and IWV.
Methods
Population
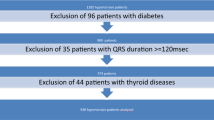
A total of 118 consecutive patients (85 men) between 18 and 88 years of age (mean age: 49±14 years) participated in the study. The effect of decreased arterial pressure induced by peripheral vasodilation on regional and local AoStiff measurements was tested in a subgroup of these patients (n=52 patients, 37 men, mean age: 52±11 years) by measuring stiffness before and after sublingual administration of glycerin trinitrate (GTN). The biometric and hemodynamic characteristics of the participants are summarized in Table 1. All patients were informed of the purposes of the study and gave informed consent. The local institutional ethics committee approved the study (CPP OUEST II—approval no. 2006/10).
Regional AoStiff measurements
Tonometric recordings
A high-resolution tonometer was used to record the transcutaneous carotid-femoral, PWV in the right common carotid and femoral arteries consecutively. The ECG signal was used as a chronometric guide (Pulsepen, DiaTecne, Milan, Italy).19 The distance (in meters) between the two recording sites was measured with a ruler and calculated as the sternal-femoral minus the sternal-carotid distance (see Figure 1).19
Bioelectric impedance recordings
The regional method, like the tonometric technique, is based on the transit time of the BI wave (see Figure 2). BI signals are recorded first in the chest and then in the thigh with two pairs of surface ECG electrodes attached to a four-electrode impedance device (PhysioFlow PF-05 Lab1, Manatec Laboratories, Paris, France).20, 21 For example, a very low electrical current at high frequency (3.8 mA, 75 kHz) was administered through the first pair of electrodes at the chest wall (electrodes 1 and 4), and the differential electrical potential was recorded by the second pair (electrodes 2 and 3) (see refs. 22,23,24,25). The two pairs of electrodes were separated by a distance of 20 cm. An ECG was simultaneously recorded as a time base for the BI signal analysis (see Figure 2). The variations of the BI signal were related to the propagation of the blood volume into the ascending and descending aorta.
To analyze the propagation of the blood volume into the femoral artery, the electrode configuration was shifted from the chest to the thigh while maintaining a constant distance between the two pairs of electrodes. The electrodes were positioned along the main axis of the femoral artery to increase the signal-to-noise ratio17 (see Figure 2). After appropriate signal filtering, IWV (in m s−1) between the ascending aorta and the femoral artery was derived from the following formula:

The term dAB represents the distance between the two electrodes labeled ‘1’ of each site, which correspond to the recording sites (carotid and femoral) for the tonometric technique (see Figure 2). Finally, τAB represents the transit time, or delay, of the peak of the derivative impedance wave between the two sites (see Figure 2).
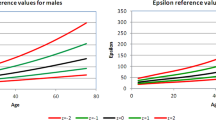
Local AoStiff measurements derived from bioelectrical impedance
The local method was applied at chest level. The local AoStiff index can be assessed using a new algorithm developed by our laboratory. However, we determined the AoStiff index without using the pulse wave to estimate arterial stiffness. The AoStiff index was computed from the determination of two other indices, AoRes and AoDist, which were calculated from the measurement of the energy injected and distributed into the aortic system per volume unit. The left ventricle pumps blood through the aorta with each heartbeat and thus contributes mechanical energy to the vascular system. The biomechanical and hemodynamic properties of the vascular system determine the relative distribution of this energy between kinetic (that is, related to the aortic flow) and elastic (that is, related to the aortic wall displacement) energies. These two energies can be extracted from a specific BI waveform analysis developed by our laboratory and are expressed per pressure unit. The AoRes and AoDist indices are derived from the measurement of these energies, respectively, and are also expressed per pressure unit.14 Then, when divided by the arterial pressure, AoStiff, AoRes and AoDist become dimensionless indices.18
This new approach assumes that AoStiff is a broad concept reflecting two main components of the aortic system:
-
1)
The local resistance exerted by the vessel itself against the aortic blood flow (and defined by the AoRes index). It represents the intensity of the forces that oppose the relative motion of the fluid into the aorta. This local resistance corresponds to the addition of the turbulences due to the presence of whirlpools generated by the geometry of the aorta and the mean shear stress generated by the force applied by the blood flow to the arterial wall. Thus, it mainly depends on the blood velocity and the aortic diameter.
-
2)
The local elastic properties of the arterial wall related to its distensibility during the systolic phase (and defined by the AoDist index). For example, an increase in AoStiff can result from increased apparent resistance of the aorta to blood flow (that is, the AoRes index), impaired aortic elasticity (that is, the AoDist index) or a combination of these two effects.
The detailed calculation of these indices has been described in a previous publication.14
Effect of peripheral vasodilatation on the local and regional stiffness indices
The effect of changes in arterial blood pressure induced by peripheral arterial resistance downstream to the measurement point (that is, the aorta) on the local and regional stiffness indices were studied before and after administration of a peripheral systemic vasodilator (GTN). The vasodilator effect of GTN administration on the peripheral vasculature was also monitored at the brachial artery with a high-resolution echo tracking ultrasound system (Alpha 10, Aloka, Tokyo, Japan). The changes in local diastolic diameter were recorded by two wall-tracking calipers that automatically followed the displacements of the near and distant brachial walls. Ten cardiac cycles were recorded and were averaged to determine the local distensibility (DS in mm Hg−1) of the artery using the following relation:

where ΔP is the pulse pressure (in mm Hg−1), Ddiastole represents the diastolic diameter and ΔD represents the systolic-diastolic changes in diameter.
Protocol
All measurements were performed at rest in a quiet room with dimmed light and controlled ambient temperature (25 °C). The patients lay supine for at least 15 min before recording began. Before each measurement, systolic and diastolic brachial arterial blood pressures were measured by an automatic sphygmomanometer (Welch-Allyn, Vital Signs Monitor 300 Series, New York, NY, USA) with an appropriately sized cuff.
In all patients, carotid-femoral PWV was determined with two successive tonometric measurements by a trained operator (Georges Leftheriotis). BI signals were then recorded twice for 1 min at the chest and then at the thigh. The left brachial arterial blood pressure was obtained at the same time.
Sublingual GTN (Natispray, 2 × 0.15 mg, P&G France, Asnières-sur-Seine, France) was administered after 2 min of recordings at rest. Arterial blood pressure, chest and thigh BI signals as well as local brachial artery properties were recorded 3 min after administration when the effect of GTN had reached its maximum as indicated by brachial diameter monitoring.
Statistical analysis
All statistical analyses were performed with the R software (version 2.9.0, R Foundation, Murray Hill, NJ, USA). Quantitative variables are expressed as mean±s.d. The relationship between variables was evaluated by linear regression, Pearson correlation coefficients and Bland–Altman plots. Comparison between and within groups at rest and after GTN administration was performed using a Mann–Whitney test. Repeatability was determined by calculating a within-subject coefficient of variation for repeated measurements. For all statistics, a P value of <0.05 was considered statistically significant.
Results
The signal-to-noise ratio of carotid-femoral PWV and IWV measurements was good in 86 and 87% of the recordings, respectively. AoStiff, AoRes and AoDist indices were validated in 95% of the recordings (that is, a detection of the characteristic points of BI signal was possible).
Regional and local AoStiff measurements at rest
For all patients, the within-subject repeatability between two successive carotid-femoral PWV and AoStiff measurements in the same session showed a coefficient of variation of 6.05 and 5.05%, respectively, without significant differences. No significant difference was observed for the repeatability of two successive IWV measurements (coefficient of variation, 5.32%).
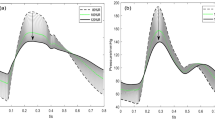
There was no significant difference between the mean carotid-femoral PWV (8.58±2.84 m s−1) measured tonometrically and the mean IWV (8.10±3.50 m s−1) measured with the BI technique. A significant linear relationship was found between both methods, with a correlation coefficient of r=0.88 (95% confidence interval (CI): 0.78–0.90; P<0.0001; IWV=1.12 × PWV−1.26) (see Figure 3). The Bland–Altman plot comparing PWV and IWV showed a systematic offset of −0.28 m s−1 with a limit of agreement from −2.87 to 2.81 m s−1 (see Figure 4).
We found a significant linear relationship between the carotid-femoral PWV and AoStiff (see Figure 5) with a correlation coefficient of r=0.75 (95% CI: 0.65–0.83; P<0.0001; AoStiff=0.05 × PWV+0.27). Likewise, we observed a significant linear relationship between IWV and AoStiff values with a correlation coefficient of r=0.66 (95% CI: 0.54–0.76; P<0.0001; AoStiff=0.03 × IWV+0.39).
Regional and local AoStiff measurements after GTN administration
Hemodynamic changes before and after GTN are summarized in Table 1. Administration of GTN induced a significant 4% (95% CI: −5.71 to −3.53%; P=0.002) drop of mean brachial arterial blood pressure with a 16% (95% CI: 13.45–19.75%; P<0.001) increase in heart rate. Likewise, the brachial diastolic diameter increased by 19% (95% CI: 16.61–20.07%; P<0.001). These changes were associated with a 38% (95% CI: −35.41 to −13.83%; P<0.001) decrease in brachial arterial distensibility.
There was no significant difference in regional (IWV) and local (AoStiff) aortic indices before and after administration of GTN (P=0.71 and 0.74, respectively). However, we observed a 17% (95% CI: 5.13–30.31%; P<0.05) increase in the AoRes index after GTN administration and a 15% (95% CI: 5.93–24.16%; P<0.001) increase in the AoDist index.
Discussion
Over the last decade, the growing interest in the study of biomechanical properties of peripheral vessels has been linked to the development of non-invasive, reliable and convenient techniques for the determination of arterial stiffness.26, 27 Currently, the most popular method for evaluating arterial stiffness is obtained by estimating the pulse transit time between the carotid and femoral arteries using the tonometric technique.8, 19 This technique gives a reliable index of the regional AoStiff,28, 29 but represents only an estimate of the local AoStiff because it is a summation of the individual biomechanical properties of different arterial walls (that is, carotid, aorta, iliac and femoral arteries) located between the two recording sites.30, 31 Our data showed that IWV measurements are highly correlated with the carotid-femoral PWV, indicating that IWV also provides a reliable estimate of the regional AoStiff (see Figures 3 and 4).
Assessment of local AoStiff with the BI technique (AoStiff index) revealed a linear relationship between the AoStiff index and PWV (see Figure 5), suggesting that the AoStiff can be evaluated reliably by local or regional non-invasive methods. However, in contrast to the regional methods that measure at two points, the local method relies on a measurement performed only at one point (that is, the chest). Thus, measurement of the distance between the two recording sites is no longer required. This simplifies the measurement while maintaining reliability even in overweight patients.5 The local method also provides the AoRes and AoDist indices that permit analysis of the underlying mechanisms that contribute to the AoStiff.
However, our results show that the correlation coefficient between the AoStiff index and IWV was lower than that between the AoStiff index and PWV. This observation may be explained by the dependence of the regional method on the length of the arterial segment. At the thigh level, we noted that the arterial segment studied with the regional IWV method is significantly longer than that studied with the PWV method. At this site, the tonometric pulse pressure is measured at the root of the femoral artery, but the BI signal is recorded from a large segment of the thigh (see Figures 1 and 2). The poor correlation observed between the AoStiff index and IWV could reflect this difference. Moreover, our data also show that the correlation coefficient between the carotid-femoral PWV and AoStiff index was weaker than that between the regional IWV and carotid-femoral PWV measurements. This result suggests that these methods do not provide strictly equivalent estimates of AoStiff. These discrepancies are probably explained by the variation of the local and regional elastic properties along the arterial tree. Some studies have shown that the elastin/collagen ratio, which determines the viscoelastic properties of the arteries, can vary continuously along the arterial tree.9, 10, 32 For example, the elastin/collagen ratio of the aorta is of 1.5, whereas that of the femoral artery is 0.5 (see ref. 33). This ratio is also altered during arterial aging and by the atherosclerotic process, and fragmentation of the elastic fiber network leads to premature recruitment of the most rigid collagen fibers.34 Thus, this non-linear variation of the arterial wall elasticity could contribute to the differences observed between the regional and local measurements.
We also investigated the effect of a change in systemic arterial blood pressure induced by peripheral arterial resistance on the regional and local AoStiff indices. In this study, the effect of GTN on the peripheral artery was controlled by the expanded diameter of the brachial artery evaluated by ultrasound. It is often assumed that a decrease in peripheral resistance would reduce AoStiff by reducing the arterial and thus the distending pressure. However, despite a significant drop in mean arterial blood pressure, we found no significant changes in IWV measurements 3 min after GTN administration, the time of maximal effect. Consistent with these results, other studies also showed no significant change in the carotid-femoral PWV measurements after administration of GTN.35, 36 Likewise, the AoStiff index did not change significantly 3 min after GTN administration. Why AoStiff does not change after GTN administration, despite the combined effects of decreased arterial pressure and direct GTN-mediated relaxation of arterial tone, is not known. Both effects would contribute to reducing the propagative properties of arterial wave velocities in the aorta.37, 38
In our model, the AoStiff index is a variable integrating two components: the local resistance of the aorta to the flow (that is, the turbulences and the mean shear stress) and the distensibility of the aortic wall, which could vary independently. With GTN administration, both components may counterbalance each other, leading to an apparently unchanged AoStiff. This was confirmed by the rise in both the AoRes (17%; 95% CI: 5.13–30.31%; leading to increase in AoStiff index) and AoDist indices (15%; 95% CI: 5.93–24.16%; leading to decrease in AoStiff index) after GTN administration. The increased AoRes index could result from increased aortic turbulence and shear stress generated by exaggerated flow following peripheral vasodilation.39 However, the increased AoDist index remains difficult to explain. The relaxing effect of GTN is mediated through NO pathways and should affect muscular (such as the brachial artery) rather than elastic arteries (such as the aorta).35 Whatever the mechanism, the increased AoDist index could help maintain the overall AoStiff, a mechanism that suggests a self-regulating response to decreased peripheral (that is, brachial) distensibility.
Study limitations
This study lacks a direct measurement of local AoStiff such as that provided by MRI or ultrasound analyses of local aortic hemodynamic and geometric properties. However, our objective was to determine whether the local stiffness measurement could be correlated with the regional stiffness measurement and to assess the relative advantages of measurements obtained at one or two points.
This study was also limited by the absence of measurement of the carotid-femoral PWV at 3 min after GTN administration. Because of the necessary positioning of the neck electrodes over the course of carotids for the BI measurements, it was not possible to perform simultaneous measurement of the carotid-femoral PWV and IWV. However, previous studies have demonstrated the invariance of PWV measurements after GTN administration.35, 36
Finally, in the present study, the total cholesterol for the subgroup of 52 patients was significantly lower than for the whole population, suggesting a possible bias in favor of GTN.
Conclusion
Although PWV and the AoStiff index are not strictly identical because of the inhomogeneous elastic properties of the arterial tree, both local and regional methods are well correlated, even in the presence of changes in arterial pressure due to systemic peripheral vasodilatation. In contrast to the regional methods, the local method assessed with the BI technique allows a differential analysis of the components of AoStiff (that is, resistance and distensibility). This technique could represent a useful tool for a more discriminating analysis of the effect of vasoactive drugs on the vasculature.
References
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A . Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001; 37: 1236–1241.
O’Rourke MF, Mancia G . Arterial stiffness. J Hypertens 1999; 17: 1–4.
Iannuzzi A, Licenziati MR, Acampora C, Renis M, Agrusta M, Romano L, Valerio G, Pancio S, Trevisan M . Carotid artery stiffness in obese children with the metabolic syndrome. Am J Cardiol 2006; 97: 528–531.
Liu XN, Gao HG, Li BY, Cheng M, Ma YB, Zhang ZM, Gao XM, Liu YP, Wang M . Pulse wave velocity as a marker of arteriosclerosis and its comorbidities in Chinese patients. Hypertens Res 2007; 30: 237–242.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Panier B, Vlachopoulos C, Wilkinson I, Boudier HS . Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27: 2588–2605.
Nigam A, Mitchell GF, Lambert J, Tardif JC . Relation between conduit vessel stiffness (assessed by tonometry) and endothelial function (assessed by flow-mediated dilatation) in patients with and without coronary heart disease. Am J Cardiol 2003; 92: 395–399.
Willum-Hansen T, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, Jeppesen J . Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation 2006; 113: 664–670.
Millasseau SC, Stewart AD, Patel SJ, Redwood SR, Chowienczyk PJ . Evaluation of carotid-femoral pulse wave velocity: influence of timing algorithm and heart rate. Hypertension 2005; 42: 222–226.
Bergel DH . The static elastic properties of the arterial wall. J Physiol 1961; 156: 445–457.
Bergel DH . The dynamic elastic properties of the arterial wall. J Physiol 1961; 156: 458–469.
Laurent S, Cockroft J . Central aortic Blood Pressure. Les laboratoires Servier, Elsevier: 22 rue Garnier, 95578 Neuilly-sur-seine, France, 2008.
Gamble G, Zorn J, Sanders G, MacMahon S, Sharpe N . Estimation of arterial stiffness, compliance, and distensibility from M-mode ultrasound measurements of the common carotid artery. Stroke 1994; 25: 11–16.
Gatehouse PD, Keegan J, Crowe LA, Masood S, Mohiaddin RH, Kreitner KF, Firmin DN . Applications of phase-contrast flow and velocity imaging in cardiovascular MRI. Eur Radiol 2005; 15: 2172–2184.
Collette M, Leftheriotis G, Humeau A . Modeling and interpretation of the bioelectrical impedance signal for the determination of the local arterial stiffness. Med Phys 2009; 36: 4340–4348.
Kubicek WG, Karnegis JN, Patterson RP, Witsoe DA, Mattson RH . Development and evaluation of an impedance cardiac output system. Aerospace Med 1966; 37: 1208–1212.
Kubicek WG . Minnesota Impedance Cardiograph Model 303. Instruction Manual. University of Minnesota Press: Minneapolis, 1968.
Collette M, Humeau A, Abraham P . Time and spatial invariance of impedance signals in limbs of healthy subjects by time-frequency analysis. Ann Biomed Eng 2008; 36: 444–451.
Collette M, Leftheriotis G, Humeau A . Procédé de mesure d’un indice de la rigidité locale de la paroi d’une artère de conduction et installation correspondante. Patent application No. 08/0764 (pending), 2008.
Salvi P, Lio G, Labat C, Ricci E, Pannier B, Benetos A . Validation of a new non-invasive portable tonometer for determining arterial pressure wave and pulse wave velocity: the PulsePen device. J Hypertens 2004; 22: 2285–2293.
Kubicek WG, Patterson RP, Witsoe DA . The impedance cardiograph as a noninvasive means to monitor cardiac functions. J Assoc Adv Med Instrum 1970; 4: 79–84.
Kubicek WG, Patterson RP, Witsoe DA . Impedance cardiography as a non-invasive method for monitoring cardiac function and other parameters of the cardiovascular system. Ann NY AcadSci 1970; 170: 724–732.
Charloux A, Lonsdorfer-Wolf E, Richard R, Lampert E, Oswald-Mammosser M, Mettauer B, Geny B, Lonsdorfer J . A new impedance cardiograph device for the non-invasive evaluation of cardiac output at rest and during exercise: comparison with the ‘direct’ fick method. Eur J Appl Physiol 2000; 82: 313–320.
Moore R, Sansores R, Guimond V, Abboud R . Evaluation of cardiac output by thoracic electrical bioimpedance during exercise in normal subjects. Chest 1992; 102: 448–455.
VonkNoordegraaf A, Faes TJC, Janse A, Marcus JT, Bronzwaer JGF, Postmus PE, de Vries PM . Noninvasive assessment of right ventricular diastolic function by electrical impedance tomography. Chest 1997; 111: 1222–1228.
Moreau X, Rousseau JM, Thiranos JC, Dubé L, Corbeau JJ, Granry JC, Beydon L . Cardiac output measurements: comparison between a new transthoracic electrical bioimpedance method (PhysioFlow) and the Swan-Ganz method (continuous Cardiac Output or Bolus Technique). Eur J Appl Physiol 2000; 82: 313–320.
Domanski M, Norman J, Wolz M, Mitchell G, Pfeffer M . Cardiovascular risk assessment using pulse pressure in the first national health and nutrition examination survey. Hypertension 2001; 38: 793–797.
Millasseau SC, Guigui FG, Kelly RP, Prasad K, Cockcroft JR, Ritter JM, Chowienczyk PJ . Noninvasive assessment of the digital volume pulse. Comparison with the peripheral pressure pulse. Hypertension 2000; 36: 952–956.
Doonan RJ, Hausvater A, Scallan C, Mikhailidis DP, Pilote L, Daskalopoulou SS . The effect of smoking on arterial stiffness. Hypertens Res 2010; 33: 398–410.
Rerkpattanapipat P . Correlation of aortic stiffness and restenosis after coronary angioplasty. Am J Cardiol 2002; 89: 652.
Stevanov M, Baruthio J, Eclancher B . Fabrication of elastomer arterial models with specified compliance. J ApplPhysiol 2000; 88: 1291–1294.
Van der Heijden-Spek JJ, Staessen JA, Fagard RH, Hoeks AP, Boudier HA, Van Bortel LM . Effect of age on brachial artery wall properties differs from the aorta and is gender dependent: a population study. Hypertension 2000; 121: 1460–1470.
Nichols W, O’Rourke M . McDonald's Blood Flow in Arteries. 5th edn. Arnold: London, 2005.
Hosoda Y, Kawano K, Yamasawa F, Ishii T, Shibata T, Inayama S . Age-dependent changes of collagen and elastin content in human aorta and pulmonary artery. Angiology 1984; 35: 615–621.
Mercier N, Osborne-Pellegrin M, El Hadri K, Kakou A, Labat C, Loufrani L, Henrion D, Challande P, Jalkanen S, Feve B, Lacolley P . Carotid arterial stiffness, elastic fibre network and vasoreactivity in semicarbazide-sensitive amine-oxidase null mouse. Cardiovasc Res 2006; 72: 349–357.
Sorkin EM, Brogden RN, Romankiewicz JA . Intravenous glyceryltrinitrate (nitroglycerin). A review of its pharmacological properties and therapeutic efficacy. Drugs 1984; 27: 45–80.
Kelly RP, Millasseau SC, Ritter JM, Chowienczyk PJ . Vasoactive drugs influence aortic augmentation index independently of pulse wave velocity in healthy men. Hypertension 2001; 37: 1429–1433.
Stewart AD, Jiang B, Millasseau SC, Ritter JM, Chowienczyk PJ . Acute reduction of blood pressure by nitroglycerin does not normalize large artery stiffness in essential hypertension. Hypertension 2006; 48: 404–410.
Yaginuma T, Avolio A, O’Rourke M, Nichols W, Morgan JJ, Roy P, Baron D, Branson J, Feneley M . Effects of glyceryltrinitrate on peripheral arteries alters left ventricular hydroulic load in man. CircRes 1986; 20: 153–160.
Latson TW, Hunter WC, Katoh N, Sagawa K . Effect of nitroglycerin on aortic impedance, diameter, and pulse-wave velocity. Circ Res 1988; 62: 884–890.
Acknowledgements
This project was funded by research program PHRC no. 2006/10. M. Collette was supported by a grant from the University of Angers, France. The authors wish to thank the Clinical Research Center of Angers for assistance with monitoring and data management.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Collette, M., Humeau, A., Chevalier, C. et al. Assessment of aortic stiffness by local and regional methods. Hypertens Res 34, 578–583 (2011). https://doi.org/10.1038/hr.2010.280
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2010.280