Abstract
Purpose:
Molecular karyotyping has rapidly become the test of choice in patients with neurocognitive phenotypes, but studies of its clinical utility have largely been limited to outbred populations. In consanguineous populations, single-gene recessive causes of neurocognitive phenotypes are expected to account for a relatively high percentage of cases, thus diminishing the yield of molecular karyotyping. The aim of this study was to test the clinical yield of molecular karyotyping in the highly consanguineous population of Saudi Arabia.
Methods:
We have reviewed the data of 584 patients with neurocognitive phenotypes (mainly referred from pediatric neurology clinics), all evaluated by a single clinical geneticist.
Results:
At least 21% of tested cases had chromosomal aberrations that are likely disease-causing. These changes include both known and novel deletion syndromes. The higher yield of molecular karyotyping in this study as compared with the commonly cited 11% can be explained by our ability to efficiently identify single-gene disorders, thus enriching the samples that underwent molecular karyotyping for de novo chromosomal aberrations. We show that we were able to identify a causal mutation in 37% of cases on a clinical basis with the help of autozygome analysis, thus bypassing the need for molecular karyotyping.
Conclusion:
Our study confirms the clinical utility of molecular karyotyping even in highly consanguineous populations.
Genet Med 17 9, 719–725.
Similar content being viewed by others
Introduction
Developmental delay/intellectual disability (DD/ID) is a common condition affecting 1–3% of children.1 The method of approaching such cases has evolved over the years. Some of these children present with a combination of clinical features that allows the clinician to recognize a single-gene or a structural or numerical chromosomal disorder. In such cases, mutation analysis of specific candidate genes, fragile X syndrome (FRAXA) testing, or conventional karyotyping is usually pursued first. Unfortunately, the majority of patients lack a specific presentation, which poses a diagnostic challenge. For these cases, a large number of nonspecific diagnostic assays are ordered, albeit with very low diagnostic yield. For instance, the yield of conventional karyotyping is estimated at 3% (excluding Down syndrome and other recognizable chromosomal syndromes).2 Clearly, a diagnostic assay with a wide range of indications and a higher clinical sensitivity is required. Molecular karyotyping has quickly been embraced as such an assay: it has revolutionized the diagnosis of unexplained neurocognitive phenotypes and has become the recommended first-tier clinical diagnostic test for these individuals.3 It has been called an indispensable genetic analysis in the diagnosis of idiopathic (DD/ID)4 and is likely to remain so until supplanted by the increasingly popular whole-exome/whole-genome sequencing. Unlike a regular karyotype that relies on the microscopic inspection of chromosomes, molecular karyotyping constructs virtual chromosomes based on the copy-number analysis of DNA, which improves its resolution by 100-fold.5 Like any other test, there are limitations: microarray platforms cannot identify truly balanced chromosomal rearrangements or point mutations, and low-level mosaicism for unbalanced rearrangements and aneuploidy may not be detected.3 Furthermore, with the increasing recognition of the pervasiveness of copy-number polymorphisms, as well as the recent realization that reduced penetrance of some pathogenic copy-number variants (CNVs) can influence the clinical phenotype, assigning pathogenicity to CNVs that are uncovered at an increasingly high resolution by molecular karyotyping can be very challenging.
Miller and colleagues2 conducted a literature review of 33 studies including 21,698 patients tested by chromosomal microarray. They found an average diagnostic yield of 11% (range, 5.1–20.0%).2 This wide range is attributable to the fact that studies used different platforms with different resolutions and different inclusion criteria. Curiously, it is noted that all these studies were performed using outbred populations. Consanguineous populations have historically been investigated for recessive single-gene disorders, but there are no data regarding the contribution of CNVs to DD/ID disease burden in these populations. One may predict that the yield will be diminished because single-gene recessive causes of neurocognitive phenotypes account for a relatively high percentage of cases.
In the present study, we attempted to address this gap in knowledge by investigating a cohort of DD/ID patients in Saudi Arabia, a country with a consanguinity rate of 56%. We present data from our cohort of patients with a neurocognitive phenotype, and we demonstrate that the yield of molecular karyotyping is in fact paradoxically high at 21%, probably due to the successful identification of single-gene disorders in patients who were deemed ineligible for molecular karyotyping. In addition to established microdeletion syndromes, our study identifies novel ones and challenges previous reports that assigned pathogenicity to a CNV that we show to be likely benign.
Materials and Methods
Human subjects
Our study is a retrospective chart review of all patients (n = 584) with a neurocognitive phenotype (mainly referred from pediatric neurology clinics) who were seen by a single clinical geneticist in his clinic from September 2007 to June 2013. All families were enrolled under a King Faisal Specialist Hospital and Research Center institutional review board–approved protocol after signing written informed consent. Those whose clinical photographs are shown have specifically signed a patient photograph release form. Our inclusion criteria comprised the presence of a neurocognitive phenotype (i.e., syndromic and nonsyndromic cases of DD, autism, ID, and epilepsy) with a normal regular karyotype, and the evaluation by a single clinical geneticist (F.S.A.) in his clinic. Patients who were not candidates for having a molecular karyotype were excluded. This included patients who had an abnormal regular karyotype result (mainly Down syndrome), patients with suspected Prader–Willi/Angelman syndrome, patients with positive family history consistent with autosomal recessive inheritance, patients with an environmental cause of their neurocognitive phenotype, and those cases suggestive of a specific syndromic diagnosis for which the causative gene is known. A subset of patients was excluded due to logistic (e.g., parents declined testing) or technical reasons (e.g., molecular karyotyping had been performed but failed due to poor-quality DNA and could not be repeated because the patient could not be recalled or had died).
Molecular karyotyping
Initially we used the Affymetrix SNP 6.0 array, which was replaced by the Cyto-V2 and later the CytoScan HD (Affymetrix, Riyadh, Saudi Arabia) arrays. The latter was used for the majority of our patients. Whole-genome chromosome single-nucleotide polymorphism (SNP) microarray analysis was performed to assess for imbalances (i.e., gains or losses) in the genomic DNA using the genome-wide SNP CytoScan HD array. This array platform contains 2.6 million markers for CNV detection (Affymetrix), of which 750,000 are genotype SNPs and 1.9 million are nonpolymorphic probes, for the whole genome coverage. The analysis was performed using the Chromosome Analysis Suite version Cyto 2.0.0.195(r5758). Oligonucleotide probe information is based on build 37 of the UCSC Genome Browser (http://genome.ucsc.edu/cgi-bin/hgGateway, GRCh37/hg19).
Briefly, 250 ng of genomic DNA was digested with the restriction enzyme NspI and then ligated to an adapter, followed by polymerase chain reaction (PCR) amplification using a single pair of primers that recognized the adapter sequence. The PCR products were run on a 2% tris-borate-EDTA gel to confirm that the majority of products were between 150 and 2,000 bp in length. To obtain a sufficient quantity of PCR product for further analysis, all products from each sample were combined and purified using magnetic beads (Agencourt AMPure, Beckman Coulter, Beverly, MA). The purified PCR products were fragmented using DNase I and visualized on a 4% tris-borate-EDTA agarose gel to confirm that the fragment sizes ranged from 25 to 125 bp. The fragmented PCR products were subsequently end-labeled with biotin and hybridized to the array. Arrays were then washed and stained using a GeneChip Fluidics Station 450 and scanned using an Affymetrix GeneChip Scanner 3000 7G. Scanned data files were generated using Affymetrix GeneChip Command Console Software (version 1.2) and analyzed with the Chromosome Analysis Suite.
The hidden Markov model available within the Chromosome Analysis Suite software package was used to determine the copy-number states and their breakpoints. Thresholds of log2 ratio ≥0.58 and ≤ −1 were used to categorize altered regions as CNV gains (amplification) and copy-number losses (deletions), respectively.
To minimize the detection of false-positive CNVs arising due to inherent microarray “noise,” only alterations that involved at least 50 consecutive probes and that were at least 500 kb in size were used to categorize altered regions as CNV gains (amplification), whereas those at least 200 kb in size were used to categorize copy-number losses (deletions) in our study.
We then proceeded to evaluate the CNVs detected in our patients based on the American College of Medical Genetics and Genomics standards and guidelines.3 The genic content in the CNV interval of all the patients who had a molecular karyotype performed was taken into consideration by seeking recent publications to compare breakpoints, phenotypes, and different sizes of CNVs that overlapped. To exclude aberrations representing common benign CNVs, all the identified CNVs were compared with those reported in the Database of Genomic Variants (http://projects.tcag.ca/variation/) and those reported in our own database for individuals who have been classified as normal.
CNVs were divided into the three recommended categories: pathogenic, benign/likely benign, and of uncertain clinical significance. Under pathogenic, we had (i) de novo CNVs that met the size cutoff of 200 kb for deletions and 500 kb for duplications (based on the laboratory’s consideration of the performance characteristics of the assay used) and were not found in either parent and (ii) the CNVs that were inherited from a clinically affected parent. These included novel CNVs as well as those that were previously published as either representing a well-established syndrome or being linked to a neurocognitive phenotype. The benign/likely benign CNVs were previously reported as a benign variant or were present in one of the unaffected parents, respectively. However, this does not eliminate the possibility that pathogenic CNVs exhibiting incomplete penetrance or variable expressivity can be present in an unaffected parent. CNVs that were found in patients whose parents were not tested were classified as being of uncertain clinical significance.
Results
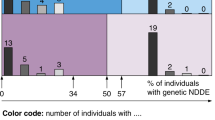
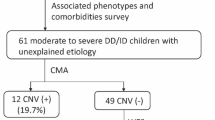
Of all the charts reviewed from September 2007 to June 2013, 584 patients with various neurocognitive phenotypes met the inclusion criteria. We then excluded (i) 76 patients with an abnormal regular karyotype (72 cases of Down syndrome, 1 case of trisomy 18, 1 case of inverted duplications of chromosome 15 syndrome, 1 case referred with Chr6q14q21 deletion, and 1 case referred with an unbalanced chromosome 7 translocation); (ii) 6 patients with Prader–Willi syndrome; (iii) 54 with positive family history consistent with autosomal recessive inheritance, because they are more likely to have a single-gene disorder than a deletion/duplication; (iv) 1 case with an environmental cause for the neurocognitive phenotype (kernicterus); (v) 217 with molecularly confirmed single-gene disorders; (vi) 1 case of mitochondrial DNA depletion; and (vii) 46 due to logistic and technical reasons (see above). This is presented in Supplementary Figure S1 online.
Seventy-five discrete disorders were identified at the single-gene level. Mutations in more than 80 single genes were found in these patients. No single gene accounted for more than 2% of the cases, with the exception of ADAT3 (6.5%), which was recently reported to be a cause of ID with strabismus.6
Valid molecular karyotyping data were obtained for 183 patients. Based on the American College of Medical Genetics and Genomics standards and guidelines for interpretation and reporting of postnatal constitutional CNVs,3 38 (21%) patients (a father/two sons trio with the same pathogenic CNV were counted once) were found to have pathogenic CNVs. Thirty-four CNVs were de novo (two patients were each found to have two de novo pathogenic CNVs). Three CNVs representing known microdeletion syndromes (Chr22q11.21 deletion, Chr17p11.2 deletion, and Chr16p11.2 deletion) were of unknown inheritance because one of the healthy parents was not available for testing. Three CNVs were inherited from an affected parent. In addition, 141 patients (77.5%) had benign/likely benign CNVs or a normal molecular karyotype, and 3 patients (1.5%) showed variants of uncertain clinical significance.
Of the 40 pathogenic CNVs, 30 were previously reported (24 represent well-established syndromes and 6 were reported as being associated with a neurocognitive phenotype). These cases are summarized in Supplementary Table S1 online; the genic content of the CNVs of these patients can be found in Supplementary Table S2 online, and the facial features for some are shown in Figure 1 .
Facial features of some of those with previously reported pathogenic copy-number variants. (a) Patient 08DG00312 with Chr1p21.3-1p13.3 deletion. (b) Patient 09DG00247 with Chr1p36.33-1p36.32 deletion. (c) Patient 11DG0743 with Chr7q11.23 deletion. (d) Patient 08DG00076 with Chr9p24.3-9q21.11 duplication. (e) Patient 08DG00254 with Chr13q12.3 deletion. (f) Patient 12DG1161 with Chr15q11.2-15q13.1 deletion. (g) Patient 13DG1086 with Chr15q11.2-15q13.3 triplication. (h) Patient 11DG2239 with Chr16p11.2 deletion. (i) Patient 13DG0756 with Chr16p11.2 deletion. (j) Patient 14DG0263 with Chr17p11.2 deletion. (k) Patient 11DG0257 with Chr17p13.3 deletion. (l) Patient 11DG2019 with Chr17q21.31 deletion. (m) Patient 08DG00155 with Chr22q11.21 deletion. (n) Patient 10DG0083 with Chr22q11.21 deletion. (o) Patient 11DG0448 with Chr22q11.1-22q11.21 deletion. (p) Patient 11DG2451 with Chr22q13.33 deletion.
The well-established syndromes found in 23 of our patients included the following: an interesting case of Williams syndrome with intact ELN; Bannayan–Riley–Ruvalcaba syndrome with autism and severe ID; a CHARGE-like case with trisomy 12p; 14q32.3 deletion syndrome with Dubowitz-like features; and triplication of 15q11–15q13. Of the remaining six pathogenic CNVs, patient 13DG0291 shared maternally inherited Bannayan–Riley–Ruvalcaba syndrome (Chr10q23.31 deletion involving PTEN) with his two sisters, but only he has autism and severe ID. Patient 08DG00254 with ID, epilepsy, and attention deficit hyperactivity disorder (ADHD) had a paternally inherited Chr13q12.3 deletion. His father has learning difficulties and psychological problems.
The remaining 10 pathogenic CNVs were novel (one CNV was found in a father/two brothers trio representing a novel ID syndrome and was counted once, and two CNVs were found in a single patient). These cases are summarized in Supplementary Table S3 online; the genic content of the CNVs of these patients can be found in Supplementary Table S4 online, and the facial features for most are shown in Figures 2 – 4 .
Facial features of the family with a novel intellectual disability/dysmorphology syndrome represented by an identical Chr1p36.22–1p36.23 deletion. (a) Patient 13DG0955 with Chr1p36.22-1p36.23 deletion. (b) Mouth of patient 13DG0955 showing fissured corners. (c) Patient 13DG0956 with Chr1p36.22-1p36.23 deletion. (d) Mouth of patient 13DG0956 showing fissured corners. (e) Patient 13DG0957 with Chr1p36.22-1p36.23 deletion (father of patients 13DG0955 and 13DG0956). (f) Mouth of patient 13DG0957 showing fissured corners.
Features of patient 10DG1455 with Chr5q11.2-q13.2 deletion and Chr9p13.1-9q13 duplication. (a) Face showing dysmorphic features including frontonasal dysplasia, widow’s peak, severe hypertelorism, and prominent broad nasal bridge. (b) Back of head showing flat occiput and low posterior hairline. (c) Hands showing syndactyly and broad thumbs.
Three of our patients showed variants of uncertain clinical significance because either one or both parents could not be tested. These are summarized in Supplementary Table S5 online; the genic content of the CNVs of these patients can be found in Supplementary Table S6 online, and the facial features are shown in Figure 5 .
Facial features of those with likely pathogenic copy-number variants of undetermined de novo status. (a) Patient 11DG0134 with Chr2p14 deletion and Chr19p12 deletion. (b) Patient 08DG00087 with Chr3q22.1 deletion and ChrXp22.33 duplication. (c) Patient 08DG00521 with Chr9p12 duplication. (d) Right eye of patient 08DG00521 showing coloboma.
Discussion
In our study, we demonstrate the relatively high yield of molecular karyotyping (21%) for neurocognitive phenotypes in a consanguineous population by revealing 40 pathogenic CNVs. This is unlikely to be due to an overcalling of pathogenic CNVs because 75% were previously reported. Rather, the paradox is explained by the fact that more than one-third of our cohort (37%) was found to have a single-gene disorder confirmed molecularly, thus obviating the need for molecular karyotyping. These accounted for 75 discrete disorders identified mainly by autozygosity mapping, almost all of which were recessive. This essentially enriched the denominator for nonautosomal recessive causes of neurocognitive phenotypes, that is, de novo dominant causes, whether CNVs or point mutations. Furthermore, had we not excluded these cases from the denominator, our yield would have decreased to 9.5%, which is comparable with many cited yields. In line with this is the observation that the enrichment was significantly higher among patients with consanguineous parents (2.8-fold) as compared with those with nonconsanguineous parents (1.5-fold).
Several other observations in our study are worth highlighting. For example, in several cases with previously reported CNVs, we expanded the associated described phenotype. Patient 11DG0743 is an interesting case of Williams syndrome as he was found to have an atypical de novo deletion of the Williams–Beuren syndrome critical region in 7q11.23 retaining the ELN gene, which is in keeping with his normal cardiac evaluation.7 The genes CLIP2, GTF2IRD1, and GTF2I have been proposed to be linked to abnormal cognition in the Williams–Beuren syndrome critical region.7,8 However, we note that the deletion in our patient, who has the classic cognitive and behavioral phenotype of the Williams–Beuren syndrome critical region, preserves these genes.
The index case (13DG0291) in a family with classic Bannayan–Riley–Ruvalcaba syndrome is worth highlighting. He presented with autism, severe ID, and ADHD. His examination revealed macrocephaly and multiple macules on his penis (Supplementary Figure S2 online). Family history was negative, but examination revealed an affected mother—13DG0296 (with papillomatous papules over the nose and eyelids)—and indeterminate status of two affected sisters—13DG0292 and 13DG0295—all of whom completely lacked any neurocognitive involvement. All four were found to have the same hemizygous 10q23.1 deletion involving the gene PTEN (Supplementary Figure S3 online). Autistic behavior is an uncommon feature of Bannayan–Riley–Ruvalcaba syndrome; it has been described in only three cases.9,10,11 It is interesting that PTEN mutations have been associated with autism spectrum disorder with or without classic features of Bannayan–Riley–Ruvalcaba syndrome, and that even though all four members of our family have the same deletion breakpoints, only 13DG0291 has a neurocognitive phenotype.
Three of our patients (09DG00498, 11DG2239, 13DG0756) were found to have Chr16p11.2 microdeletion syndrome with very similar breakpoints (Supplementary Figure S4 online) involving almost the same genes, yet they have very different phenotypes. Patient 13DG0756 presented classically with ID and morbid truncal obesity.12 However, patient 09DG00498 presented with DD, significant failure to thrive, and right radial ray defect with an abnormally placed right pedunculated thumb, which has never been reported in this syndrome (Supplementary Figure S6 online). It is tempting to speculate that this radial ray defect may be related to the de novo 16p deletion in compound heterozygosity with a second hit from the other allele, akin to thrombocytopenia/absent radius syndrome. However, we cannot exclude the possibility of two independent disorders. Finally, patient 11DG2239 presented with significant speech delay despite apparently normal cognition and hearing. He also had poor weight gain, postaxial polydactyly of the left hand, and poor dentition. Childhood apraxia of speech was confirmed by his Chr16p11.2 deletion with breakpoints similar to those previously reported.13 Interestingly, neither of these reported patients was obese. The literature clearly demonstrates that the 16p11.2 deletion is associated with obesity, but the reciprocal duplication is associated with failure to thrive.14 Despite this, patients 09DG00498 and 11DG2239 presented with failure to thrive. It should also be noted that the 23 genes with an impact on pathways central to the development of obesity were included in all three deletions: SPN, QPRT, C16orf54, MAZ, PRRT2, MVP, CDIPT, SEZ6L2, ASPHD1, KCTD13, TMEM219, TAOK2, HIRIP3, INO80E, DOC2A, C16orf92, FAM57B, ALDOA, PPP4C, TBX6, YPEL3, GDPD3, and MAPK3.12 The deletion found in patient 11DG2239 did not involve SPN. SEZ6L2 and DOC2A, genes included in all three deletions, have been implicated in autism disorder,15 but our patients did not present with autistic features. Curiously, all three patients presented with hand anomalies, and it is particularly interesting that 09DG00498 presented with right radial ray defect, whereas 11DG2239 presented with its reciprocal, postaxial polydactyly of the left hand.
Patient 13DG0955 is a child with syndromic ID that he inherited from his father (patient 13DG0957); his brother, patient 13DG0956, is similarly affected. All three were found to have an identical Chr1p36.22-1p36.23 deletion (Supplementary Figure S5 online), representing a novel syndrome presenting with a peculiar facial appearance of short palpebral fissures, wrinkled lower eyelids, prominent columella, and fissured corners of the mouth ( Figure 2 ). They also presented with short stature. Patient 13DG0955 was found to have mitral valve prolapse and mitral regurgitation, whereas his brother’s (patient 13DG0956) echocardiogram was normal (the father was not tested). Vitiligo of both hands and a large rough nevus was also evident in patient 13DG0955, but not in his brother. Patient 13DG0956 demonstrated low insulin-like growth factor 1 and delayed bone age. His brother (13DG0955) also had delayed bone age, but insulin-like growth factor 1 was normal.
Patient 11DG1823 was found to have a de novo Chr2p21 deletion encompassing only two genes: SIX2 and SIX3. This patient presented with ID, DD, and epilepsy. On examination, she was found to have generalized hypotonia with normal reflexes but no dysmorphic features. A patient with normal neurocognitive development with hemizygous deletion of the SIX2 gene with frontonasal dysplasia and craniosynostosis was previously reported, suggesting a role for SIX2 in craniofacial disorders.16 Our patient suggests that a role for SIX2 in craniofacial dysmorphism is, at best, subject to reduced penetrance. Similarly, lack of holoprosencephaly on brain magnetic resonance imaging in our patient despite haploinsufficiency for SIX3, one of the four major holoprosencephaly genes,17 suggests that this may be an example of incomplete penetrance of the holoprosencephaly phenotype in association with SIX3 deletion.
We were also able to identify aberrations that were previously reported as potentially pathogenic but that we found to be compatible with normal phenotype. These CNVs are listed in Supplementary Table S7 online. For instance, a mother with normal cognition—patient 13DG1188—was found to have a Chr10q11.22 duplication, which we found among several patients and parents with both normal and abnormal cognition, which may explain the controversy surrounding the pathogenicity of this CNV in the literature.18 Another interesting finding was a 7q31.1 deletion that encompasses IMMP2L, a gene that has been reported in association with ADHD,19 autism,20 and Tourette syndrome.21 This deletion was maternally inherited in a patient with cognitive impairment (08DG00266) from an unaffected mother (08DG00268). Furthermore, one of our patients with DD (10DG0415) was found to have a hemizygous 20p12.1 deletion that encompasses MACROD2. Although haploinsufficiency (microdeletion of exon 5) for this gene has been reported to cause Kabuki syndrome, we note that the phenotypically normal father (10DG0416) has the same deletion.22 Finally, the normal father (13DG1373) of one of our patients (08DG00076) was found to have an Xp21.2 deletion involving IL1RAPL1, which was reported as an X-linked mental retardation gene.23,24 These findings suggest that care should be exercised in assigning pathogenicity to CNVs without rigorous calculation of their comparative burden in large cohorts of patients and controls.25
In conclusion, this study provides the first empirical data regarding the clinical utility of molecular karyotyping in a consanguineous population. In addition to confirming the high diagnostic yield of this clinical test, our study revealed novel CNV-related syndromes that we hope will be replicated by others in future studies. The apparent discrepancies in the phenotypic consequences of certain deletions as compared with previous reports requires further clarification in additional patients to determine whether these represent reduced penetrance or true lack of replication of the initial reports.
Disclosure
The authors declare no conflict of interest.
References
Roeleveld N, Zielhuis GA, Gabreëls F . The prevalence of mental retardation: a critical review of recent literature. Dev Med Child Neurol 1997;39:125–132.
Miller DT, Adam MP, Aradhya S, et al. Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am J Hum Genet 2010;86:749–764.
South ST, Lee C, Lamb AN, Higgins AW, Kearney HM ; Working Group for the American College of Medical Genetics and Genomics Laboratory Quality Assurance Committee. ACMG Standards and Guidelines for constitutional cytogenomic microarray analysis, including postnatal and prenatal applications: revision 2013. Genet Med 2013;15:901–909.
Rodríguez-Revenga L, Vallespín E, Madrigal I, et al. A parallel study of different array-CGH platforms in a set of Spanish patients with developmental delay and intellectual disability. Gene 2013;521:82–86.
Shoukier M, Klein N, Auber B, et al. Array CGH in patients with developmental delay or intellectual disability: are there phenotypic clues to pathogenic copy number variants? Clin Genet 2013;83:53–65.
Alazami AM, Hijazi H, Al-Dosari MS, et al. Mutation in ADAT3, encoding adenosine deaminase acting on transfer RNA, causes intellectual disability and strabismus. J Med Genet 2013;50:425–430.
Antonell A, Del Campo M, Magano LF, et al. Partial 7q11.23 deletions further implicate GTF2I and GTF2IRD1 as the main genes responsible for the Williams-Beuren syndrome neurocognitive profile. J Med Genet 2010;47:312–320.
Vandeweyer G, Van der Aa N, Reyniers E, Kooy RF . The contribution of CLIP2 haploinsufficiency to the clinical manifestations of the Williams-Beuren syndrome. Am J Hum Genet 2012;90:1071–1078.
Boccone L, Dessì V, Zappu A, et al. Bannayan-Riley-Ruvalcaba syndrome with reactive nodular lymphoid hyperplasia and autism and a PTEN mutation. Am J Med Genet A 2006;140:1965–1969.
Zori RT, Marsh DJ, Graham GE, Marliss EB, Eng C . Germline PTEN mutation in a family with Cowden syndrome and Bannayan-Riley-Ruvalcaba syndrome. Am J Med Genet 1998;80:399–402.
Parisi MA, Dinulos MB, Leppig KA, Sybert VP, Eng C, Hudgins L . The spectrum and evolution of phenotypic findings in PTEN mutation positive cases of Bannayan-Riley-Ruvalcaba syndrome. J Med Genet 2001;38:52–58.
Walters RG, Jacquemont S, Valsesia A, et al. A new highly penetrant form of obesity due to deletions on chromosome 16p11.2. Nature 2010;463:671–675.
Raca G, Baas BS, Kirmani S, et al. Childhood Apraxia of Speech (CAS) in two patients with 16p11.2 microdeletion syndrome. Eur J Hum Genet 2013;21:455–459.
Jacquemont S, Reymond A, Zufferey F, et al. Mirror extreme BMI phenotypes associated with gene dosage at the chromosome 16p11.2 locus. Nature 2011;478:97–102.
Kumar RA, KaraMohamed S, Sudi J, et al. Recurrent 16p11.2 microdeletions in autism. Hum Mol Genet 2008;17:628–638.
Saal HM, Hufnagel R, Bender PL, Zimmerman S . Putting the cart before the mouse: a new frontonasal dysplasia syndrome caused by deletion of the SIX2 gene. 2011 David W. Smith Workshop on Malformations and Morphogenesis, Lake Arrowhead, CA, 9–14 September 2011.
Rosenfeld JA, Ballif BC, Martin DM, et al. Clinical characterization of individuals with deletions of genes in holoprosencephaly pathways by aCGH refines the phenotypic spectrum of HPE. Hum Genet 2010;127:421–440.
Liehr T, Stumm M, Wegner RD, et al. 10p11.2 to 10q11.2 is a yet unreported region leading to unbalanced chromosomal abnormalities without phenotypic consequences. Cytogenet Genome Res 2009;124:102–105.
Elia J, Gai X, Xie HM, et al. Rare structural variants found in attention-deficit hyperactivity disorder are preferentially associated with neurodevelopmental genes. Mol Psychiatry 2010;15:637–646.
Maestrini E, Pagnamenta AT, Lamb JA, et al.; IMGSAC. High-density SNP association study and copy number variation analysis of the AUTS1 and AUTS5 loci implicate the IMMP2L-DOCK4 gene region in autism susceptibility. Mol Psychiatry 2010;15:954–968.
Petek E, Windpassinger C, Vincent JB, et al. Disruption of a novel gene (IMMP2L) by a breakpoint in 7q31 associated with Tourette syndrome. Am J Hum Genet 2001;68:848–858.
Maas NM, Van de Putte T, Melotte C, et al. The C20orf133 gene is disrupted in a patient with Kabuki syndrome. J Med Genet 2007;44:562–569.
Kozák L, Chiurazzi P, Genuardi M, Pomponi MG, Zollino M, Neri G . Mapping of a gene for non-specific X linked mental retardation: evidence for linkage to chromosomal region Xp21.1-Xp22.3. J Med Genet 1993;30:866–869.
Franek KJ, Butler J, Johnson J, et al. Deletion of the immunoglobulin domain of IL1RAPL1 results in nonsyndromic X-linked intellectual disability associated with behavioral problems and mild dysmorphism. Am J Med Genet A 2011;155A:1109–1114.
Girirajan S, Brkanac Z, Coe BP, et al. Relative burden of large CNVs on a range of neurodevelopmental phenotypes. PLoS Genet 2011;7:e1002334.
Willemsen MH, Vallès A, Kirkels LA, et al. Chromosome 1p21.3 microdeletions comprising DPYD and MIR137 are associated with intellectual disability. J Med Genet 2011;48:810–818.
Bonaglia MC, Giorda R, Tenconi R, et al. A 2.3 Mb duplication of chromosome 8q24.3 associated with severe mental retardation and epilepsy detected by standard karyotype. Eur J Hum Genet 2005;13:586–591.
Youngs EL, McCord T, Hellings JA, Spinner NB, Schneider A, Butler MG . An 18-year follow-up report on an infant with a duplication of 9q34. Am J Med Genet A 2010;152A:230–233.
Lesca G, Rudolf G, Labalme A, et al. Epileptic encephalopathies of the Landau-Kleffner and continuous spike and waves during slow-wave sleep types: genomic dissection makes the link with autism. Epilepsia 2012;53:1526–1538.
Gijsbers AC, Bosch CA, Dauwerse JG, et al. Additional cryptic CNVs in mentally retarded patients with apparently balanced karyotypes. Eur J Med Genet 2010;53:227–233.
Acknowledgements
We thank the affected individuals and their families for their enthusiastic participation. Thanks are also due to Khalid Alshalan from King Khalid University Hospital Cytogenetic Laboratory for his technical help with regular karyotypes.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Figure S1
(PDF 746 kb)
Supplementary Figure S2
(PNG 164 kb)
Supplementary Figure S3
(PDF 58 kb)
Supplementary Figure S4
(PDF 58 kb)
Supplementary Figure S5
(PDF 58 kb)
Supplementary Figure S6
(PNG 185 kb)
Supplementary Table S1
(DOC 121 kb)
Supplementary Table S2
(DOC 119 kb)
Supplementary Table S3
(DOC 79 kb)
Supplementary Table S4
(DOC 65 kb)
Supplementary Table S5
(DOC 49 kb)
Supplementary Table S6
(DOC 43 kb)
Supplementary Table S7
(DOC 43 kb)
Rights and permissions
About this article
Cite this article
Al-Qattan, S., Wakil, S., Anazi, S. et al. The clinical utility of molecular karyotyping for neurocognitive phenotypes in a consanguineous population. Genet Med 17, 719–725 (2015). https://doi.org/10.1038/gim.2014.184
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2014.184
Keywords
This article is cited by
-
Long contiguous stretches of homozygosity detected by chromosomal microarrays (CMA) in patients with neurodevelopmental disorders in the South of Brazil
BMC Medical Genomics (2019)
-
Clinical genomics expands the morbid genome of intellectual disability and offers a high diagnostic yield
Molecular Psychiatry (2017)
-
A null mutation in TNIK defines a novel locus for intellectual disability
Human Genetics (2016)