Abstract
Purpose
The lateral compartment of the orbit can readily be accessed through a horizontal lateral canthotomy without the need to swing the lid or remove bone. In this paper the technique, accessible orbital territory, and duration of surgery are presented.
Patients and methods
Retrospective, non-interventional descriptive case series for patients who underwent a lateral canthotomy to access pathology within the lateral orbit.
Results
A series of 18 patients are included, all presenting with pathology lateral to, or within, the optic nerve. Pathologies included amyloidosis (1), lymphoma (4), metastatic adenocarcinoma within the optic nerve (1), idiopathic lateral rectus muscle mysositis (4), meningothelial meningioma of the optic nerve (1), intraconal orbital meningioma (1), reactive lymphoid hyperplasia (1), optic nerve glioma (3), optic nerve meningioma (1), and cavernous haemangioma (1). The median surgical time was 36 min (range 23–75 min). No patient required detachment of the lower lid, the technique leaving both upper and lower ‘arms’ of the lateral canthal tendon attached to Whitnall’s tubercle.
Conclusions
The lateral canthotomy approach orbitotomy is a rapid, safe, and minimally disruptive approach for accessing pathology in the lateral orbit and optic nerve. The lateral canthal tendon is split along the horizontal raphe without detachment of either limb from Whitnall’s tubercle, no bone is removed, and the post-operative recovery is rapid with minimal associated inflammation or chemosis. This approach is also flexible, permitting the clinician to increase exposure to the orbit peroperatively by swinging the lower lid if required.
Similar content being viewed by others
Introduction
There are six main approaches to orbitotomy, all through incisions concealed within periorbital rhytids or conjunctiva, and they allow wide access to most parts of the orbit.
Kronlein’s early description of the lateral orbitotomy was a major advance in the management of orbital disease,1 but the long, crescent-shaped incision resulted in unsightly scarring, and many other approaches have since been proposed.2, 3, 4, 5
The lateral parts of the orbit can, however, be readily reached through a horizontal lateral canthotomy without the need to mobilize bone or divide the crura of the lateral canthal tendons. This canthotomy approach gives access lateral to the optic nerve, both the intra- and extra-conal space, and allows tissue sampling from several diverse tissues where there is diffuse intraorbital pathology.
This technique, and the location of pathology which can be accessed, is illustrated with a series of patients undergoing such surgery at Moorfields Eye Hospital.
Materials and methods
Retrospective, non-interventional descriptive case series of patients who underwent lateral canthotomy orbitotomy, with review of the medical records, pathology, surgical timing, and recovery period. All surgeries were performed by two experienced orbital surgeons (DHV, GER).
Surgical technique
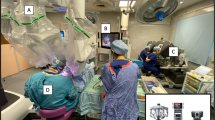
Scissors are used to divide the outer canthus 1–1.5 cm horizontally (to the bone) and 2/0 silk traction sutures placed through the upper and lower canthal tissues, thereby creating a rhomboid entry site (Figure 1a); neither the upper nor lower canthi are detached from the orbital rim (Figure 1b). Using two paddle retractors, and with diathermy and blunt dissection through the fat, pathology within the lateral extra-conal and intraconal spaces may be accessed. Canthotomy closure is quickly achieved by lid margin alignment, apposition of the upper and lower limbs of the tendon, and skin closure—all using a single 6-0 soluble suture (Figure 1c).
The technique gives an access for biopsy or debulking of pathology within the lateral two-thirds of the orbit; where greater access is required, the lower canthal tendon can be divided to convert it to a ‘low’ lower lid swinging flap (Figure 2).6
Results
Medical records and imaging were available for 18 patients having orbitotomy through a lateral canthotomy.
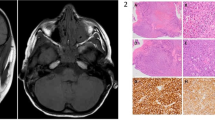
Nine patients had lesions in the intraconal space, 5 in the lateral rectus, 4 had complete excision of optic nerve glioma/meningioma, and 5 had pathology biopsied from several tissues (Table 1; Figure 3). Most lesions were neoplastic (five malignant, eight benign), four had inflammation and one had localized amyloid infiltration.
Surgical time
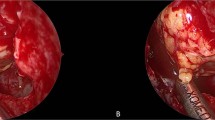
The intraoperative time ranged from 23 to 75 min for biopsies (mean 42; median 36 min) and 66 min average for excision of the orbital optic nerve. There were no permanent complications attributable to the surgical approach, but with excision of the optic nerve or orbital apex surgery, it was usual to see a global reduction in eye movements for a few weeks after surgery. None of the cases were complicated by hemorrhage, or by unexpected visual loss, mydriasis, diplopia, or abduction deficit. There were no cases of canthal dystopia and in all cases the incision healed rapidly in the lateral rhytid (Figure 4).
Discussion
Historically, bone-swinging lateral orbitotomy was the favored access to the lateral intraconal space and the Kronlein incision (from 1888) was crescent-shaped, with the anterior convexity at the lateral orbital rim, and extending over the temporal fossa toward the ear.1 The Kronlein incision leaves a long and visible scar (Figure 5a), and the approach has been modified over the years.2, 3, 4, 5, 6, 7, 8 The Kocher approach placed the incision below the brow and turning to the midpoint of the zygomatic arch7 (Figure 5b), and the S-shaped Stallard–Wright incision was partially hidden within the brow (Figure 5c).3, 8 A modified Kronlein approach for bone-swinging lateral orbitotomy has been described using either a horizontal incision through lateral canthus,2, 4, 5 an incision placed laterally in the upper lid skin crease,9, 10, 11 or a lateral canthal skin incision requiring dedicated micro-instrumentation and an operating microscope.12
All the above techniques tend to cause long and visible scars, with various authors subsequently advocating different approaches to minimize scarring, which includes approaches through the upper lid skin crease approach,10, 11 an incision within the hairline anterior to the ear,13 and a coronal scalp flap approach.14 Although the coronal approach avoids a visible incision, it carries a risk of injury to the upper divisions of the facial nerve (with entrance to the fat pad superficial to the temporalis muscle in Yasargil’s plane), is time-consuming, and generally unnecessary given the alternatives.15 Of interest, Nemet et al have proposed the ‘lateral triangle flap approach’ lateral orbitotomy, this being a combination of a lateral upper lid skin crease incision and a horizontal skin incision lateral to the lateral canthus; such an approach allows access to the lateral and superolateral orbital compartments, with the option of proceeding to a bone-swinging orbitotomy if required.16
In contrast, for biopsy or debulking of pathology in the lateral canthal compartment where a biopsy or debulk is required, or for excision of a relatively small lesion, the lateral canthotomy orbitotomy as described here is rapid, safe, and minimally disruptive, giving wide access to the lateral orbit including the retrobulbar space and optic nerve. It is a viable method for optic nerve fenestration, given the relatively posterior entry point to the orbit, compared to the upper lid skin crease and retrocaruncular approaches, the optic nerve is visualized with a greater ‘conoid of view’ where the access path being shorter. There are many indications for this approach (Table 2), and it has several advantages (Table 3); Chief among its advantages is that—by dividing the tendon along the lateral horizontal raphe without detaching of either limb from Whitnall’s tubercle—the surgical time is typically short and post-operative recovery rapid, with minimal post-operative inflammation or chemosis, and no chance of canthal dystopia. Finally, should increased exposure be required, this is readily achieved by detaching the lower limb of the tendon and opening the inferior fornix, thereby converting it to a lower lid swinging flap.

References
Kronlein RU . Zur pathologie und operative behandlung der dermoidcysten der orbita. Bruns Beitr Klin Chir 1888; 4: 149–163.
Berke RN . Modified Kronlein operation. AMA Arch Ophthalmol 1954; 51: 609–632.
Stallard HB . Surgery of the orbit. Ann R Coll Surg Engl 1968; 43: 125–140.
Reese AB . Orbital tumors and their surgical treatment. Am J Ophthalmol 1941; 24: 386–394497-502.
Smith JL . Anterolateral approach to the orbit. Trans Am Acad Ophthalmol Otolaryngol 1971; 75: 1059–1064.
Verity DH, Rose GE. Surgical approaches to the orbit. In: Perry JD, Singh AD (eds). Clinical Ophthalmic Pathology. Springer: Heidelberg, 2014..
Rootman J, Stewart B, Golbert RA (eds). Orbital Surgery—a Conceptual Approach. Lippincott: Philadelphia, 1995..
Wright JE. Surgical exploration of the orbit. In: Stewart WB (ed). Ophthalmic Plastic and Reconstructive Surgery. American Academy of Ophthalmology: San Francisco, 1984, pp 309–315..
Henderson JW Orbital Tumors. Raven Press: New York, 1994, pp 425–434..
Harris GJ, Logani SC . Eyelid crease incision for lateral orbitotomy. Ophthalmic Plast Reconstr Surg 1999; 15: 9–18.
Unal M, Ileri F, Konuk O, Hasanreisogglu B . Balanced orbital decompression in Graves’ orbitopathy: upper eyelid crease incision for extended lateral wall decompression. Orbit 2000; 19: 109–117.
Maroom JC, Kennerdell JS . Lateral microsurgical approach to intraorbital tumors. J Neurosurg 1976; 44: 556–561.
Guyton JS . Decompression of the orbit. Surgery 1946; 19: 790–809.
Stewart WB, Levin PS, Toth BA . Orbital surgery. The technique of coronal scalp flap approach to the lateral orbitotomy. Arch Ophthalmol 1988; 106: 1724–1726.
Rootman J, Stewart B, Goldberg RA. Regional approach to the anterior, mid and apical orbit. In: Rootman J, Stewart B, Goldberg RA (eds). Orbital Surgery. Lippincott-Raven Publishers: Philadelphia, 1995, pp 228..
Nemet A, Martin P . The lateral triangle flap—a new approach for lateral orbitotomy. Orbit 2007; 26: 89–95.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hamed-Azzam, S., Verity, D. & Rose, G. Lateral canthotomy orbitotomy: a rapid approach to the orbit. Eye 32, 333–337 (2018). https://doi.org/10.1038/eye.2017.173
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.173
This article is cited by
-
Stereotactic radiosurgery for orbital cavernous venous malformation: a single center’s experience for 15 years
Acta Neurochirurgica (2021)
-
Möglichkeiten des chirurgischen Zugangs zur Orbita
HNO (2018)