Abstract
Three anti-vascular endothelial growth factor (VEGF) therapies are currently used for the treatment of patients with wet age-related macular degeneration (AMD): pegaptanib, ranibizumab, and bevacizumab. Ranibizumab is an antibody fragment approved for the treatment of wet AMD. Bevacizumab is a full-length antibody registered for use in oncology but unlicensed for wet AMD. However, it is used off-label worldwide not only for wet AMD but also for various other ocular diseases associated with macular edema and abnormal vessel growth. We consider aspects of ranibizumab and bevacizumab in relation to their molecular characteristics, in vitro and in vivo properties, and preclinical safety data. Before 2009, most studies described the short-term toxicity of bevacizumab in multiple cell types of the eye. Since 2009, an increasing number of studies have compared the properties of ranibizumab and bevacizumab and investigated their impact on retinal cell functioning. Compared with bevacizumab, ranibizumab neutralizes VEGF better at low concentrations, maintains efficacy for longer, and has a higher retinal penetration and potency. Studies in animals demonstrate ranibizumab to be better localized to the injected eye, whereas bevacizumab appears to have a greater effect in the fellow eye. In humans, a localized and systemic effect has been reported for both molecules. In conclusion, overlapping yet distinct pharmacological properties of ranibizumab and bevacizumab indicate that safety or efficacy data from one cannot be extrapolated to the other.
Similar content being viewed by others
Introduction
Three anti-vascular endothelial growth factor (VEGF) therapies are currently used for the treatment of patients with wet age-related macular degeneration (AMD): pegaptanib (Macugen, Pfizer, Sandwich, UK), ranibizumab (Lucentis, Novartis, Horsham, UK), and bevacizumab (Avastin, Roche, Welwyn Garden City, UK).1, 2 Pegaptanib is an oligonucleotide aptamer and was the first VEGF antagonist to be approved by the US Food and Drug Administration for use in wet AMD.1, 3 However, wet AMD patients treated with pegaptanib still experience visual decline.1, 4 Ranibizumab is an anti-VEGF antibody fragment specifically designed for ophthalmic use. Ranibizumab represents a major advance in ophthalmology because it can stabilize, and even improve visual acuity (VA) in the majority of patients with wet AMD.5, 6, 7, 8, 9 Ranibizumab is approved in the United States, Europe, and Japan for the treatment of patients with neovascular AMD.
Ranibizumab was developed for intraocular administration. This was born from the possibility that adverse effects might occur in an elderly population, such as those with AMD, and from hints of serious toxicity in clinical trials with systemic administration of bevacizumab.10 Antigen-binding fragments (Fabs) have a shorter half-life than full-length antibodies and do not possess the fragment crystallizable (Fc) domain, which can initiate immune system activation. Consequently, it was reasoned that a Fab would prevent Fc-dependent complement activation or immune cell destruction and limit systemic antibody exposure.10 Following its development, a number of recent studies have supported the rationale behind ranibizumab development. Choroidal neovascular membranes from patients with wet AMD treated with bevacizumab are characterized by significantly higher inflammatory and proliferative activity.11 Preliminary results have also demonstrated the Fc domain of bevacizumab to bind effectively to human retinal pigment epithelial (RPE) and human umbilical vascular endothelial cell (HUVEC) membranes via Fc receptors or membrane-bound VEGF, activating the complement cascade and leading to cell death. In contrast, ranibizumab does not have a Fc domain and does not activate the complement cascade.12, 13, 14, 15
Bevacizumab is a full-length anti-VEGF antibody that has been developed and registered for use in oncology but has not been licensed for the treatment of wet AMD or any other ocular conditions. However, it is used off-label worldwide not only for wet AMD but also for other ocular disease entities associated with macular edema and abnormal vessel growth. Bevacizumab vials (100 and 400 mg) are stable at 2–8°C (36–46°F) and should be protected from light, not frozen, and not shaken. Diluted bevacizumab solutions may be stored at 2–8°C (36–46°F) for up to 8 h and are recommended for storage in the original carton until time of use.16 Consequently, there are concerns regarding the compounding of bevacizumab into smaller doses for use in intraocular indications. Significant differences in IgG concentration measured from repackaged bevacizumab syringes have been reported, with a trend for an increased micron-sized protein aggregates in some samples raising the concern for obstruction of aqueous outflow and elevation in intraocular pressure. Bevacizumab repackaged into plastic syringes may be contaminated by silicone oil microdroplets, and mishandling can further increase levels of particle contaminants.17 In 2009, the freezing and thawing of bevacizumab was shown to affect its biological activity,18 stressing the importance of implementing optimum protocols when compounding pharmacies prepare bevacizumab for intravitreal use in wet AMD. Prolonged storage of bevacizumab in plastic syringes over a period of 3 months can reduce its effectiveness by 9%. However, these findings may serve to influence vigilance during repeated bevacizumab injections and increase the potential for observed inflammation.19
This review intends to consider aspects of ranibizumab and bevacizumab for the treatment of wet AMD in relation to their molecular characteristics, in vitro and in vivo properties and preclinical safety data.
Materials and methods
This review was based on a literature search performed in http://PubMed.gov using two separate searches. The first search used the terms ‘ranibizumab’ and ‘age-related macular degeneration’. The second search used the terms ‘bevacizumab’ and ‘age-related macular degeneration’. The review focussed upon, but was not limited to, pre-clinical studies in English language retrieved using these criteria. Additional studies, which were deemed relevant to the topic of this review, were also considered for inclusion.
Ranibizumab and bevacizumab generation and characteristics
Ranibizumab is a Fab of an antibody that was developed as part of an anti-VEGF program in AMD.10 Bevacizumab is a full-length antibody that was developed as a potential therapeutic agent for use in oncology.20 Both ranibizumab and bevacizumab were constructed from the mouse anti-human VEGF monoclonal antibody (mAb) A.4.6.1, which was produced using hybridoma generated from mice immunized with the predominant VEGF165 isoform conjugated to keyhole limpet hemocyanin. This murine mAb has been shown to recognize all VEGF-A isoforms and inhibit the growth of human tumor cell lines in vivo.21, 22 Intraocular administration of mAb A.4.6.1 was found to inhibit iris neovascularization secondary to retinal ischemia in primates.23
In 1997, the humanization of mAb A.4.6.1 into what is now known as bevacizumab was reported. The approach of the researchers who carried out the humanization was to transfer six regions that determine antibody binding to VEGF (known as complimentarity determining regions, CDRs) from mAb A.4.6.1 to a human antibody framework, which had been used for previous humanizations.24 Transferring the CDRs from mAb A.4.6.1 to the human framework resulted in a Fab with binding to VEGF that was reduced over 1000-fold. Consequently, to achieve VEGF binding equivalent to mAb A.4.6.1, seven framework residues in the humanized antibody variable heavy domain and one framework residue in the humanized antibody variable light domain were changed from human to murine.24 The full-length bevacizumab antibody was constructed from 1 of the 12 constructed Fab variants: Fab-12.24
Bevacizumab is produced in Chinese hamster ovary (CHO) cells from the expression plasmid pSVID5.ID.LLnspeV.xvegf36HC.LC. The resulting bevacizumab antibody is produced from the G7 clone as a 149 kDa full-length IgG1 antibody composed of two 214-residue light chains and two 453-residue heavy chains. Each light chain is covalently linked to a heavy chain and the two heavy chains are covalently linked. The resulting bevacizumab antibody contains 93% human amino acid sequence.10, 22
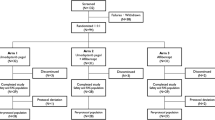
Ranibizumab was developed in an effort to obtain higher affinity variants of Fab-12 with improved potency and efficacy.25 Although bevacizumab was derived from Fab-12, ranibizumab was derived via an in vitro CDR mutation and affinity selection from a different humanized anti-VEGF Fab variant, known as MB1.6.26, 27 Ranibizumab is produced as a 48 kDa Fab in Escherichia coli from the expression plasmid pY0317. The heavy and light chains fold into their native confirmation following secretion into the bacteria periplasmic space and are covalently linked. The resulting Fab-Y0317 is now known as ranibizumab.10, 25, 28 A schematic diagram of ranibizumab and bevacizumab generation is depicted in Figure 1.
In vitro studies of ranibizumab and bevacizumab
Ranibizumab and bevacizumab are both able to bind to all human VEGF-A isoforms.10, 20 Following its generation from Fab-12, bevacizumab was found to inhibit VEGF-induced proliferation of endothelial cells in vitro and tumor growth in vivo with potency and efficacy similar to those of the parent murine antibody A.4.6.1.24 Ranibizumab (Fab-Y0317) demonstrated a 22-fold improvement in binding affinity over Fab-12 in VEGF competition assays and had 120- to 140-fold improved affinity over Fab-12 in kinetic experiments.10, 25 Furthermore, ranibizumab had a 30- to 100-fold increased potency in bioassays measuring VEGF-induced endothelial cell mitogenesis. On a molar basis, ranibizumab was determined to be 5- to 20-fold more potent than full-length bevacizumab at binding VEGF-A.10, 25 The characteristic properties of ranibizumab and bevacizumab are summarized in Table 1 .
The majority of studies investigating the in vitro efficacy of ranibizumab and bevacizumab were performed in 2006 or later. Before 2009, most of the studies were related to the short-term toxicity of bevacizumab in multiple cell types of the eye. In 2006, the Bevacizumab Study Group demonstrated no significant short-term effects of bevacizumab on retinal function of isolated bovine retina, but concluded that long-term effects could not be excluded.29 In vitro, bevacizumab was shown to be non-toxic or not to alter cell viability of rat neurosensory retinal (R28),30 retinal ganglion,31 and medulla-derived PC12 cells32 or human RPE,30, 33 microvascular endothelial (HMVECad),30 corneal keratinocyte,34 corneal fibroblast,34 and corneal endothelial cells.34, 35 In addition, bevacizumab was demonstrated to reduce VEGF-induced permeability and proliferation of cultured porcine choroidal endothelial cells,18 inhibit VEGF-stimulated proliferation of monkey choroidal endothelial cells,33 and inhibit VEGF-induced migration of HUVEC.36 In contrast to these studies, bevacizumab was shown to have a stimulatory effect on cell proliferation in the rat retinal ganglion cell line RGC-5, which was suggested to be due to a nonspecific effect via increasing the protein contents of the cell growth environment.37
Since 2009, there have been increasing number of studies that have compared the properties of ranibizumab and bevacizumab and investigated their impact on physiological retinal cell functioning. In vitro studies in human microvascular endothelial cells demonstrated ranibizumab and bevacizumab to be non-cytotoxic, increase apoptosis, decrease cellular proliferation, migration, vascular assembly and VEGF secretion, and also to decrease VEGF receptor expression and activity.38 Ranibizumab can reverse VEGF-induced proliferation and migration, and delocalization of tight junction proteins in immortalized bovine retinal cells.39 It has been demonstrated that at clinical doses, bevacizumab and ranibizumab are equally potent at neutralizing VEGF, and that to neutralize VEGF completely in porcine RPE, a fraction of the clinical dose is needed.37 Both ranibizumab and bevacizumab were able to reduce VEGF protein levels. Interestingly, at lower antibody concentrations, ranibizumab was found to be more efficient than bevacizumab at neutralizing VEGF.37 It has more recently been shown that high concentrations of bevacizumab may be harmful to human trabecular meshwork cells in primary culture, whereas no such effect was observed with ranibizumab.40 In that study, 4 mg/ml bevacizumab reduced cellular metabolism to 34.4±12.4% compared with human IgG controls (P<0.0001) and reduced cellular proliferation to 62.7±9.2% of controls (P<0.0001). No significant decrease was seen with 2 mg/ml bevacizumab, or with molar equivalents of ranibizumab.40
In a study investigating the influence of VEGF antagonists on the barrier function of RPE cells and the underlying mechanisms, bevacizumab and ranibizumab were found to decrease porcine RPE cell barrier function, with bevacizumab exhibiting a prolonged and more profound effect.41 Several studies have investigated whether the uptake of ranibizumab and bevacizumab impairs RPE cell proliferative, healing, and phagocytotic abilities.42, 43 In these studies, neither ranibizumab nor bevacizumab induced significant cell death following 7 days of treatment and no inhibition of VEGF secretion was observed after 3 days of culture. However, bevacizumab, but not ranibizumab, internalized into porcine RPE cells in vitro and accumulated in the cells. Because the RPE has important functions in maintaining retinal homeostasis it was concluded that storage of bevacizumab might compromise the cells’ physiological function.42 In a following study, bevacizumab, and to a lesser extent ranibizumab, were found to impair the proliferation of porcine RPE cells and to have no effect on wound healing.43 Bevacizumab, but not ranibizumab, was found to reduce the phagocytotic function of RPE cells, indicating possible long-term effects of repeated bevacizumab treatment.43 The selective uptake of bevacizumab, but not ranibizumab, may be owed to the presence of an Fc domain and sugar moieties on bevacizumab. The uptake of bevacizumab may be mediated by Fc-receptor mediated phagocytosis or via RPE cell mannose receptors and galectins.42
In vivo preclinical efficacy in animal models
The majority of specific in vivo data relating to bevacizumab and ranibizumab in wet AMD are derived from studies in monkeys and rabbits that were published between 2005 and 2007.44, 45, 46, 47
Early studies in rabbits and monkeys demonstrated that smaller antibody moieties such as single-chain variable fragments and Fabs have better tissue penetration than full-length antibodies. In monkeys, a humanized antibody with a framework similar to that of bevacizumab (trastuzumab) was compared with Fab-12, as bevacizumab was not available at a level of purity suitable for intraocular administration. In rabbits, the full-length ranibizumab and bevacizumab precursor (mAb A.4.6.1) was compared with a mouse/human chimeric Fab. These studies showed that, under the conditions tested, the Fabs were more diffusible than the full-length antibodies.10 Studies in monkeys have demonstrated that after a single intravitreal administration, ranibizumab can distribute rapidly to the retina (6–24 h).47 Studies in rabbits have demonstrated that ranibizumab can rapidly penetrate through the retina to reach the choroid, just 1 h after intravitreal administration.46
In primates, after a single intravitreal administration, biologically effective retinal concentrations of ranibizumab were shown to be maintained for approximately 1 month, with a terminal half-life of 3 days.47 Vitreous ranibizumab concentrations were 169 mg/ml at 6 h or 612 mg/ml at 24 h after intravitreal injection.47 Ranibizumab was found to be cleared from the vitreous with a terminal half-life of approximately 2.9 days in a study characterizing the pharmacokinetic profile and intraocular distribution of intravitreal ranibizumab injection in rabbits.46 In that study, at 1 h after intravitreal administration of 625 μg/eye, ranibizumab produced a mean peak vitreous concentration of 1280 μg/ml.46
In a study comparing the pharmacokinetics of 0.5 mg of intravitreal ranibizumab with 1.25 mg of intravitreal bevacizumab in the rabbit, the vitreous half-life of ranibizumab was found to be 2.88 days, shorter than the bevacizumab half-life of 4.32 days.44 Peak concentrations in the aqueous humor of the treated eye at 3 days following treatment have been demonstrated to be 37.7 μg/ml for bevacizumab45 and 17.9 μg/ml for ranibizumab.44 In primates, serum ranibizumab levels were found to be greater than 1000-fold lower than in the vitreous humor following a single intravitreal injection.47 In the rabbit, systemic ranibizumab levels were found to be <0.01% of the vitreous exposure.46
In a recent comparative study, intravitreal injection of ranibizumab or bevacizumab was not found to be toxic in vivo to rat eyes with healthy retinal ganglion cells or with N-methyl-D-aspartate-induced damage.48
Localized vs systemic antibody effects in animal models
There are a number of studies that demonstrate ranibizumab to be localized to the injected eye. Following intravitreal ranibizumab injection, studies in rabbits have not detected any ranibizumab in the fellow eye.44
In contrast, studies in mice have demonstrated intravitreally administered full-length IgG to be eliminated across the blood–retinal barrier into the blood system, raising concerns for a systemic effect with intravitreal bevacizumab injection.49 Indeed, intravitreally injected IgGs have been demonstrated to be eliminated into the blood system more rapidly in laser-photocoagulated eyes when compared with normal control eyes because of neonatal Fc receptor upregulation in the laser-photocoagulated retina.49 This raises the possibility of Fc-mediated systemic transfer of bevacizumab from the eye and into the circulation.
Although studies in rabbits have not revealed any long-term tolerability concerns following intravitreal bevacizumab injection,50 other studies in rabbits have detected bevacizumab in the untreated fellow eye,45 and have demonstrated bevacizumab in the subretinal space following intravitreous injection as a possible result of diffusion through the retina.51 Nomoto et al52 also investigated the pharmacokinetics of intravitreal bevacizumab (1.25 mg/0.05 ml) in rabbits. After intravitreal injection in the treated eye, the mean maximum concentrations (Cmax) of bevacizumab in the iris/ciliary body and retina/choroid were 109 192.6 and 93 990.0 ng/g, respectively. Both intravitreal injections of bevacizumab resulted in high plasma concentration and distributed into the intraocular tissues in fellow eyes via the systemic circulation. In the fellow eyes, the Cmax was 753.6 ng/g in the iris/ciliary body and 224.2 ng/g in the retina/choroid.52
In a study comparing the pharmacokinetics of 0.5 mg of intravitreal ranibizumab with 1.25 mg of intravitreal bevacizumab in the rabbit, ranibizumab was not detected in the serum or the fellow uninjected eye; whereas small amounts of intravitreal bevacizumab were detected at both sites (untreated eye 29.4 ng/ml at 1 week, serum 3.33 μg/ml at 8 days following injection).44, 45 Although it has been suggested that there may be limitations in the detection of serum ranibizumab in the method of assay used in the above study,53 these results are consistent with other studies and are suggestive of a systemic effect with bevacizumab.53
The first comparison of the efficacy of intraocular ranibizumab and bevacizumab in animal models of subretinal neovascularization has recently been published.54 In that study, Rho/VEGF mice were used, which have sustained expression of human VEGF in photoreceptors and develop progressive subretinal neovascularization similar to that seen in patients with wet AMD. When mice were treated with either antibody, higher doses or repeated injections of bevacizumab, but not ranibizumab, resulted in a systemic effect.54
Pharmacokinetics and pharmacodynamics in humans
Ranibizumab was specifically developed for AMD and consequently, the most robust efficacy data for ranibizumab are derived from large phase III trials in patients with wet AMD. This is not the focus of the current review, but in summary, improvements in VA have been seen for ranibizumab monotherapy and ranibizumab in combination with standard care in studies with up to 2 years of follow-up.5, 6, 7, 55, 56, 57, 58 As a result of such data and approval of ranibizumab in wet AMD, there are limited in vivo data available outside of a clinical trial setting regarding the anti-angiogenic efficacy profile of ranibizumab in AMD.
A recent prospective study in patients with AMD has demonstrated a significant decrease of VEGF from 85.57 pg/ml to values below the physiological levels of VEGF in controls following intravitreal injection of ranibizumab (P=0.001).59 Another recent study assessing aqueous humor samples from 16 eyes with choroidal neovascularization (CNV) secondary to AMD, demonstrated VEGF concentrations (range 47.2–307.4 pg/ml, mean 125.9 pg/ml) to decrease to <31 pg/ml, the lower limit of detection, 4 weeks after ranibizumab injection.60
In humans, much of the pharmacodynamic and pharmacokinetic data relating to bevacizumab are derived from cancer patients systemically treated with this antibody and preclinical studies using bevacizumab off-label for various ocular indications. The pharmacokinetic properties of bevacizumab are consistent with a typical humanized mAb, with a terminal half-life in humans of 17–21 days.16, 20, 61 In 2006, two patients were described from whom samples of vitreous humor were obtained 4 weeks or 48 h after a bevacizumab injection.62 Consistent with the animal studies, a single dose of intravitreal bevacizumab was suggested to provide complete intravitreal VEGF blockade for a minimum of 4 weeks, with an intravitreal half-life of 3 days.62 The unbound VEGF concentration was below detectable levels (<41 pg/ml).62 During therapy with bevacizumab, VEGF levels have been reported to decrease below detection levels in the first 2 months of treatment in patients with retinal vein occlusion.63 In 34 eyes with CNV secondary to AMD treated with 3 monthly intravitreal bevacizumab injections, the mean aqueous VEGF level decreased from 102.6±90.6 pg/ml at baseline to 18.3±22.5 pg/ml at 2 months.64
The Tübingen Bevacizumab Study Group investigated the vitreous levels of bevacizumab and VEGF following intravitreal injection in patients with CNV.65 They found the pharmacokinetics of intravitreal bevacizumab to follow a two-compartment model with initial and terminal half-lives of 0.5 and 6.7 days, respectively. The peak concentration (range 2.63 ng/ml to 165 μg/ml) was observed on the second day after intravitreal bevacizumab injection; vitreous free VEGF-A levels (range 0.2–33.9 pg/ml) showed a negative correlation with bevacizumab concentration and a positive correlation with time.65 A separate study in human non-vitrectomized eyes administered a single intravitreal injection of 1.5 mg bevacizumab reported the concentration of bevacizumab in aqueous humor to peak on the first day after injection with a mean concentration of 33.3 μg/ml (range, 16.6–42.5 μg/ml) and an aqueous half-life of 9.82 days.66
Implication of pharmacological differences on clinical outcomes
A number of clinical studies have investigated the influence of single- and double-dosed intravitreal injections and determined no significant clinical difference in short- or long-term effects on functional or anatomical parameters.67, 68, 69 Meyer et al68 compared single- (1.5 mg) or double-dosed (3.0 mg) intravitreal bevacizumab injections and determined a higher peak concentration of unbound bevacizumab and an extruded duration above therapeutic levels by one half-life in the double-dosed group.68 Although there is no difference in the half-time between 1.25 or 2.5 mg intravitreal bevacizumab, double dosing increases the peak antibody concentration in the anterior chamber of the eye. Although 500 ng/ml of bevacizumab is the minimum concentration required to completely block VEGF-A-induced endothelial cell proliferation, double dosing of bevacizumab had only a moderate effect on biological activity.69 Double dosing of intravitreal bevacizumab has a significant effect on the duration of its efficacy; it extends the duration by one half-time or approximately 8–10 days and seems to have no significant clinical impact on functional and anatomical outcomes.68
On the basis of mathematical modeling, 27–38 days after a single bevacizumab (1.25 mg) injection, the intravitreal VEGF-binding activity would be comparable with that of ranibizumab at 30 days.70 Bevacizumab injections would need to be performed every 3 days for 1 month to equal the peak activity after a ranibizumab injection. More frequent bevacizumab injections increase the average binding activity, but not to the degree achieved with a single ranibizumab injection.70 On the basis of macular volume measurements in patients with wet AMD, it has been reported that the mean duration of action was 101.8 days for bevacizumab and 74.0 days for ranibizumab, although both drugs had equal effects on decreasing central foveal point thickness or macular volume.71
In a subset of patients with wet AMD that were switched from bevacizumab to ranibizumab, there were no apparent differences in VA outcomes or injection rates.72 However, another study demonstrated that 53% of patients treated with ranibizumab, but only 35% of patients treated with bevacizumab had short-term effectiveness as assessed by incremental improvement on optical coherence tomography (OCT) parameters, suggesting differences in the biological activities between the two antibodies.73
Recently, a statistically significant benefit of ranibizumab over bevacizumab on OCT was demonstrated in the reduction of central foveal thickness—a key marker of disease progression—with patients receiving ranibizumab requiring fewer injections.74, 75 In a separate study, patients switching from bevacizumab (≥three-injection subgroup) to ranibizumab demonstrated a statistically significant improvement in both VA and retinal thickness.76 These small studies suggest ranibizumab may provide greater benefits on VA than bevacizumab, but larger studies are required to reveal significant efficacy differences in the overall wet AMD population.
A recent prospective, randomized clinical trial that enrolled 131 patients with wet AMD (the Avastin (bevacizumab) for choroidal neovascular age-related macular degeneration (ABC) trial) demonstrated 1.25 mg intravitreous bevacizumab injections given as part of a six weekly variable retreatment regimen to be superior to previous standard care (pegaptanib sodium, verteporfin, sham), with low rates of serious ocular adverse events among the 65 patients treated with bevacizumab.77 In this study, patients treated with bevacizumab on average maintained the VA gain over the study period of 12 months with outcomes similar to studies administering monthly ranibizumab.
A retrospective examination of charts of 215 eyes undergoing intravitreal injection with anti-VEGF agents for wet AMD has provided a comparison of bevacizumab and ranibizumab.78 The study demonstrated 9.9% (10/101) of eyes receiving only bevacizumab had sustained elevated intraocular pressure, whereas 3.1% (3/96) of eyes receiving only ranibizumab experienced increases (P=0.049).78
Localized vs systemic antibody effects in humans
Studies in cancer had demonstrated that the systemic half-life of a Fab is a few hours, whereas that of a full-length IgG is up to 3 weeks, implying that any systemic exposure to an anti-VEGF agent would be minimized by using a Fab and prompting the generation of ranibizumab for AMD.10
There are some studies that have demonstrated bevacizumab to have no effect in the untreated fellow eye following intravitreal injection.79, 80 In one study, the concentration of unbound bevacizumab was below the detectable limit of the ELISA (5 ng/ml in all samples) in the untreated fellow eye of human patients following contralateral intravitreal bevacizumab injection.79 No or minimal effect of intravitreal bevacizumab injection on the uninjected fellow eye has also been reported in studies with macaques and patients with proliferative diabetic retinopathy.80, 81 Velez-Montoya et al82 investigated the systemic effects of unilateral intravitreal bevacizumab administration and reported no differences between baseline and follow-up measurements in untreated fellow eyes.82 In total, 23 consecutive patients with bilateral diffuse diabetic macular edema (DME) and a central retinal thickness (CRT) greater than 275 μm on OCT were treated with 2.5 mg bevacizumab intravitreally in the worst eye and performed examinations in both eyes every 2 weeks for 4 weeks. There were no statistically significant differences between baseline and follow-up measurements in untreated fellow eyes. Visual acuity on Early Treatment Diabetic Retinopathy Study (ETDRS) letters was 34.46±17.29 at baseline, 38.31±14.64 at 2 weeks, and 37.38±14.59 at 4 weeks. The CRT was 324.77±76.51 μm at baseline, 319±75.7 μm at 2 weeks, and 315.54±78.2 μm at 4 weeks. The macular volume was 8.99±1.2 mm3 at baseline, 9.16±1.26 mm3 at 2 weeks, and 8.99±1.09 mm3 at 4 weeks. The authors concluded that the systemic effect in untreated fellow eyes after contralateral intravitreal injection of 2.5 mg bevacizumab seemed to be unlikely due to the lack of significant changes in any parameter.82
The results of a double-blind, randomized, prospective pilot-study (BEAT-AMD) has demonstrated bevacizumab to have an effect on visual outcomes in subjects with vision-threatening ophthalmic diseases associated with AMD following systemic administration.83 A 2008 case report of an 83-year-old man, with macular edema from branch retinal vein occlusion in the right eye, who developed neovascular AMD in the left eye demonstrated both intravitreal ranibizumab and bevacizumab to improve symptoms in the contralateral eye.84
In the first demonstration of blood growth factor levels following intravitreal bevacizumab injection in a human case series, samples of blood were collected from 11 patients with type II diabetes and a control group of 30 non-diabetic patients just before injection with 1.25 mg bevacizumab and after 1 day, 7 days, and 1 month.85 Decreased levels of blood VEGF after an intravitreal injection of bevacizumab (eg from 114.0 to 9.7 pg/ml after 1 day) indicate that bevacizumab enters the general circulation.85 This raises concern over the potential systemic complications with bevacizumab and emphasizes safety concerns in the absence of clinical studies of high level of evidence with bevacizumab use in patients with AMD. Indeed, a recent Letter to the Editor reported two cases of women who suffered an early loss of pregnancy (at 7 and 10 days) following intravitreal bevacizumab injection.86 Paradoxically, rapid progression of subclinical AMD in the untreated fellow eye after intravitreal bevacizumab injection has also been reported.87, 88 In addition, inhibition of VEGF in the kidney and consequent glomerular disease characteristic of thrombotic microangiopathy has been show to develop in six patients with different cancer diagnoses following treatment with bevacizumab.89
In humans, serum ranibizumab concentrations are predicted to be approximately 90 000-fold lower than vitreal concentrations.90 Indeed, studies in humans could not demonstrate a therapeutic effect of ranibizumab in the untreated fellow eye,91 and retrospective analyses of the ANCHOR6, 7 and MARINA5 clinical trials do not support the hypothesis that monthly ranibizumab injections reduce the rate of CNV development in untreated fellow eyes.92 However, ranibizumab has also demonstrated positive effects on the VA of the fellow untreated eye,93 that is, a systemic effect of ranibizumab cannot be ruled out. A meta-analysis of available 1- and 2-year data from the FOCUS,55, 56 MARINA,5 ANCHOR,6, 7 PIER,57 and SAILOR58 studies has been performed to assess the safety of ranibizumab in terms of stroke, myocardial infarction, and other adverse events.94 In the final analysis of SAILOR, although there were more cases of stroke in the 0.5 mg treatment arm, the risk was not statistically significant.58 Evidence of bevacizumab systemic safety from multiple clinical trials in patients with wet AMD does not yet exist.
Discussion
On review of the available evidence, ranibizumab and bevacizumab have overlapping yet some distinct pharmacological properties. Their differences are not surprising but indicate that safety or efficacy data from one cannot be extrapolated to the other. Although both ranibizumab and bevacizumab were constructed from the mouse anti-human VEGF mAb A.4.6.1, bevacizumab is a full-length antibody that was developed as a potential therapeutic agent for use in oncology,20 whereas ranibizumab is a Fab that was developed as part of an anti-VEGF program in AMD.10
In terms of in vitro efficacy and safety, both ranibizumab and bevacizumab can bind all VEGF-A isoforms and can similarly downregulate a number of VEGF signaling components. However, from the very beginning of development, ranibizumab was shown to be superior to bevacizumab in its affinity and ability to bind VEGF-A. Perhaps most importantly, the Fc domain and sugar residues present on bevacizumab mean that the antibody can interfere with the physiological metabolism or functioning of retinal cells and result in complement-mediated cell death. On the basis of these data, we would conclude ranibizumab to be superior to bevacizumab in terms of efficacy and safety.
In terms of in vivo preclinical efficacy and safety in animal models, both ranibizumab and bevacizumab appear similar in their half-lives and direct cellular toxicity. However, differences emerge when investigating the potential for a systemic effect following intravitreal administration of these molecules. Studies in animals, including two direct comparative studies, demonstrate ranibizumab to be better localized to the injected eye, whereas bevacizumab has a greater effect in the fellow eye. Combined with other data demonstrating that intravitreally administered full-length IgGs can cross the blood–retinal barrier, which can be mediated by an antibody Fc domain, these data suggest an increased risk for systemic complications with bevacizumab compared with ranibizumab.
In humans, there seemed to be more pharmacodynamic and pharmacokinetic data available for bevacizumab, but both ranibizumab and bevacizumab were seen to decrease VEGF levels to below detection limits of the assays used. Although the large ABC trial demonstrated the average VA gain maintained over 12 months with bevacizumab to be equivalent to similar studies with ranibizumab, other studies have demonstrated ranibizumab to be more effective than bevacizumab at decreasing markers of disease progression and improving VA. Although these studies appear to suggest improvements in efficacy in humans treated with ranibizumab compared with bevacizumab, larger studies—which are already ongoing—will be needed to reveal significant differences in efficacy on the overall wet AMD population.
In terms of systemic safety with the two molecules in humans, there are studies for both ranibizumab and bevacizumab that support a localized and a systemic effect. The strongest evidence exists for ranibizumab and is derived from analyses of the large, randomized, double-blind, phase III ANCHOR6, 7 and MARINA5 trials. Although one study demonstrated that ranibizumab might induce some therapeutic effect in selected cases of end-stage CNV scarring, the second study demonstrated that monthly ranibizumab injections do not reduce the rate of CNV development in untreated fellow eyes. Before a full conclusion can be made regarding the localized vs systemic effect of ranibizumab and bevacizumab, the levels of VEGF levels in the fellow eye of patients with wet AMD treated with these molecules need to be evaluated. However, a meta-analysis of five large clinical trials of ranibizumab in wet AMD5, 6, 7, 55, 56, 57, 58 provide evidence that ranibizumab is not associated with significant increases in the rates of stroke, myocardial infarction, and other adverse events.94
Although ranibizumab was designed specifically for intraocular use in patients with wet AMD, the possibility of a systemic effect of ranibizumab cannot be excluded. However, unlike bevacizumab, ranibizumab has demonstrated robust and consistent efficacy in a clinical trial program that has included a number of studies of Level I and II evidence that have monitored the safety of thousands of patients with wet AMD.5, 6, 7, 55, 56 Bevacizumab is unlicensed for ocular conditions, intraocular administration, or compounding into smaller doses. Pharmacovigilance measures have been installed for ranibizumab but not, or not to a similar degree, for bevacizumab. In contrast, ranibizumab has been approved for the treatment of wet AMD since 2006 and meets the US Pharmacopoeia specifications for injections in to the eye.95, 96
Ranibizumab was designed for use in ophthalmology and designed with potential for systemic complications in mind. Ongoing head-to-head studies in various countries are currently comparing ranibizumab with bevacizumab in terms of efficacy and safety. Results of Comparison of Age-related Macular Degeneration Treatments Trials (CATT; NCT00593450) in the USA are expected in 2011. However, these trials may be underpowered to detect potential differences in safety profiles between the two agents and thus, may not provide conclusive evidence.
References
Emerson MV, Lauer AK . Current and emerging therapies for the treatment of age-related macular degeneration. Clin Ophthalmol 2008; 2: 377–388.
Kroll P, Meyer CH . Which treatment is best for which AMD patient? Br J Ophthalmol 2006; 90: 128–130.
Jager RD, Mieler WF, Miller JW . Age-related macular degeneration. N Engl J Med 2008; 358: 2606–2617.
Gragoudas ES, Adamis AP, Cunningham Jr ET, Feinsod M, Guyer DR . Pegaptanib for neovascular age-related macular degeneration. N Engl J Med 2004; 351: 2805–2816.
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 2006; 355: 1419–1431.
Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med 2006; 355: 1432–1444.
Brown DM, Michels M, Kaiser PK, Heier JS, Sy JP, Ianchulev T . Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ANCHOR study. Ophthalmology 2009; 116: 57–65 e55.
Mitchell P, Korobelnik JF, Lanzetta P, Holz FG, Prunte C, Schmidt-Erfurth U et al. Ranibizumab (Lucentis) in neovascular age-related macular degeneration: evidence from clinical trials. Br J Ophthalmol 2010; 94: 2–13.
Holz FG, Korobelnik JF, Lanzetta P, Mitchell P, Schmidt-Erfurth U, Wolf S et al. The effects of a flexible visual acuity-driven ranibizumab treatment regimen in age-related macular degeneration: outcomes of a drug and disease model. Invest Ophthalmol Vis Sci 2010; 51: 405–412.
Ferrara N, Damico L, Shams N, Lowman H, Kim R . Development of ranibizumab, an anti-vascular endothelial growth factor antigen binding fragment, as therapy for neovascular age-related macular degeneration. Retina 2006; 26: 859–870.
Tatar O, Yoeruek E, Szurman P, Bartz-Schmidt KU, Adam A, Shinoda K et al. Effect of bevacizumab on inflammation and proliferation in human choroidal neovascularization. Arch Ophthalmol 2008; 126: 782–790.
Tezel TH, Zeng Q, Schaal S, Kaplan HJ . Bevacizumab (Avastin®) differs from ranibizumab (Lucentis®) in its binding affinity to retinal pigment epithelium (RPE) and vascular endothelium cell membranes. Invest Ophthalmol Vis Sci 2010; 51: E-Abstract 4955.
Zeng Q, Schaal S, Kaplan HJ, Tezel TH . Ability to bind Fc-receptors on retinal pigment epithelium (RPE) can explain the higher occurrence of RPE tears with bevacizumab (Avastin®) compared with ranibizumab (Lucentis®). Invest Ophthalmol Vis Sci 2010; 51: E-Abstract 4954.
Chan CK, Meyer CH, Gross JG, Abraham P, Nuthi AS, Kokame GT et al. Retinal pigment epithelial tears after intravitreal bevacizumab injection for neovascular age-related macular degeneration. Retina 2007; 27: 541–551.
Kook D, Wolf A, Neubauer AS, Haritoglou C, Priglinger SG, Kampik A et al. Retinal pigment epithelial tears after intravitreal injection of bevacizumab for AMD. Frequency and progress. Ophthalmologe 2008; 105: 158–164.
Avastin. Avastin prescribing information. Available at http://www.avastin.com/avastin/hcp/overview/index.html. Accessed 27 June 2010.
Liu L, Ammar DA, Ross L, Mandava N, Kahook M, Carpenter J . Silicone oil microdroplets and protein aggregates in repackaged bevacizumab and ranibizumab: effects of long-term storage and product mishandling. Invest Ophthalmol Vis Sci 2011; 52 (2): 1023–1034.
Peters S, Julien S, Heiduschka P, Grisanti S, Ziemssen F, Adler M et al. Antipermeability and antiproliferative effects of standard and frozen bevacizumab on choroidal endothelial cells. Br J Ophthalmol 2007; 91: 827–831.
Grisanti S, Tura A . Qualitätsunterschiede zwischen ranibizumab original & fertigspritzen. Ophthalmologe 2010; 107: 1123–1132.
Ferrara N, Hillan KJ, Gerber HP, Novotny W . Discovery and development of bevacizumab, an anti-VEGF antibody for treating cancer. Nat Rev Drug Discov 2004; 3: 391–400.
Kim KJ, Li B, Houck K, Winer J, Ferrara N . The vascular endothelial growth factor proteins: identification of biologically relevant regions by neutralizing monoclonal antibodies. Growth Factors 1992; 7: 53–64.
European Medicines Agency. Avastin assessment history, initial marketing authorization documents: Avastin EPAR scientific discussion. Available at http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000582/human_med_000663.jsp&murl=menus/medicines/medicines.jsp&mid=WC0b01ac058001d125. Accessed July 2010.
Adamis AP, Shima DT, Tolentino MJ, Gragoudas ES, Ferrara N, Folkman J et al. Inhibition of vascular endothelial growth factor prevents retinal ischemia-associated iris neovascularization in a nonhuman primate. Arch Ophthalmol 1996; 114: 66–71.
Presta LG, Chen H, O’Connor SJ, Chisholm V, Meng YG, Krummen L et al. Humanization of an anti-vascular endothelial growth factor monoclonal antibody for the therapy of solid tumors and other disorders. Cancer Res 1997; 57: 4593–4599.
Chen Y, Wiesmann C, Fuh G, Li B, Christinger HW, McKay P et al. Selection and analysis of an optimized anti-VEGF antibody: crystal structure of an affinity-matured Fab in complex with antigen. J Mol Biol 1999; 293: 865–881.
Muller YA, Chen Y, Christinger HW, Li B, Cunningham BC, Lowman HB et al. VEGF and the Fab fragment of a humanized neutralizing antibody: crystal structure of the complex at 2.4 A resolution and mutational analysis of the interface. Structure 1998; 6: 1153–1167.
Baca M, Presta LG, O’Connor SJ, Wells JA . Antibody humanization using monovalent phage display. J Biol Chem 1997; 272: 10678–10684.
European Medicines Agency. Lucentis assessment history, initial marketing authorization documents: Lucentis EPAR scientific discussion. Available at http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000715/human_med_000890.jsp&murl=menus/medicines/medicines.jsp&mid=WC0b01ac058001d125. Accessed July 2010.
Luke M, Warga M, Ziemssen F, Gelisken F, Grisanti S, Schneider T et al. Effects of bevacizumab on retinal function in isolated vertebrate retina. Br J Ophthalmol 2006; 90: 1178–1182.
Luthra S, Narayanan R, Marques LE, Chwa M, Kim DW, Dong J et al. Evaluation of in vitro effects of bevacizumab (Avastin) on retinal pigment epithelial, neurosensory retinal, and microvascular endothelial cells. Retina 2006; 26: 512–518.
Iriyama A, Chen YN, Tamaki Y, Yanagi Y . Effect of anti-VEGF antibody on retinal ganglion cells in rats. Br J Ophthalmol 2007; 91: 1230–1233.
Cheng CK, Peng PH, Tien LT, Cai YJ, Chen CF, Lee YJ . Bevacizumab is not toxic to retinal ganglion cells after repeated intravitreal injection. Retina 2009; 29: 306–312.
Brar VS, Sharma RK, Murthy RK, Chalam KV . Evaluation of differential toxicity of varying doses of bevacizumab on retinal ganglion cells, retinal pigment epithelial cells, and vascular endothelial growth factor-enriched choroidal endothelial cells. J Ocul Pharmacol Ther 2009; 25: 507–511.
Yoeruek E, Spitzer MS, Tatar O, Aisenbrey S, Bartz-Schmidt KU, Szurman P . Safety profile of bevacizumab on cultured human corneal cells. Cornea 2007; 26: 977–982.
Yoeruek E, Tatar O, Spitzer MS, Saygili O, Biedermann T, Bartz-Schmidt KU et al. Effects of bevacizumab on apoptosis, Na+ -K+ -adenosine triphosphatase and zonula occludens 1 expression on cultured corneal endothelial cells. Ophthalmic Res 2010; 44: 43–49.
Han YS, Lee JE, Jung JW, Lee JS . Inhibitory effects of bevacizumab on angiogenesis and corneal neovascularization. Graefes Arch Clin Exp Ophthalmol 2009; 247: 541–548.
Sharma RK, Chalam KV . In vitro evaluation of bevacizumab toxicity on a retinal ganglion cell line. Acta Ophthalmol 2009; 87: 618–622.
Costa R, Carneiro A, Rocha A, Pirraco A, Falcao M, Vasques L et al. Bevacizumab and ranibizumab on microvascular endothelial cells: a comparative study. J Cell Biochem 2009; 108: 1410–1417.
Deissler H, Deissler H, Lang S, Lang GE . VEGF-induced effects on proliferation, migration and tight junctions are restored by ranibizumab (Lucentis) in microvascular retinal endothelial cells. Br J Ophthalmol 2008; 92: 839–843.
Kahook MY, Ammar DA . In vitro effects of antivascular endothelial growth factors on cultured human trabecular meshwork cells. J Glaucoma 2010; 19: 437–441.
Miura Y, Klettner A, Roider J . VEGF-antagonists decrease barrier function of retinal pigment epithelium in vitro -possible participation of intracellular glutathione. Invest Ophthalmol Vis Sci 2010; 51: 4848–4855.
Klettner AK, Kruse ML, Meyer T, Wesch D, Kabelitz D, Roider J . Different properties of VEGF-antagonists: bevacizumab but not ranibizumab accumulates in RPE cells. Graefes Arch Clin Exp Ophthalmol 2009; 247: 1601–1608.
Klettner A, Mohle F, Roider J . Intracellular bevacizumab reduces phagocytotic uptake in RPE cells. Graefes Arch Clin Exp Ophthalmol 2010; 248: 819–824.
Bakri SJ, Snyder MR, Reid JM, Pulido JS, Ezzat MK, Singh RJ . Pharmacokinetics of intravitreal ranibizumab (Lucentis). Ophthalmology 2007; 114: 2179–2182.
Bakri SJ, Snyder MR, Reid JM, Pulido JS, Singh RJ . Pharmacokinetics of intravitreal bevacizumab (Avastin). Ophthalmology 2007; 114: 855–859.
Gaudreault J, Fei D, Beyer JC, Ryan A, Rangell L, Shiu V et al. Pharmacokinetics and retinal distribution of ranibizumab, a humanized antibody fragment directed against VEGF-A, following intravitreal administration in rabbits. Retina 2007; 27: 1260–1266.
Gaudreault J, Fei D, Rusit J, Suboc P, Shiu V . Preclinical pharmacokinetics of ranibizumab (rhuFabV2) after a single intravitreal administration. Invest Ophthalmol Vis Sci 2005; 46: 726–733.
Thaler S, Fiedorowicz M, Choragiewicz TJ, Bolz S, Tura A, Henke-Fahle S et al. Toxicity testing of the VEGF inhibitors bevacizumab, ranibizumab and pegaptanib in rats both with and without prior retinal ganglion cell damage. Acta Ophthalmol 2010; 88: e170–e176.
Kim H, Robinson SB, Csaky KG . FcRn receptor-mediated pharmacokinetics of therapeutic IgG in the eye. Mol Vis 2009; 15: 2803–2812.
Wu WC, Lai CC, Chen KJ, Chen TL, Wang NK, Hwang YS et al. Long-term tolerability and serum concentration of bevacizumab (avastin) when injected in newborn rabbit eyes. Invest Ophthalmol Vis Sci 2010; 51: 3701–3708.
Dib E, Maia M, Longo-Maugeri IM, Martins MC, Mussalem JS, Squaiella CC et al. Subretinal bevacizumab detection after intravitreous injection in rabbits. Invest Ophthalmol Vis Sci 2008; 49: 1097–1100.
Nomoto H, Shiraga F, Kuno N, Kimura E, Fujii S, Shinomiya K et al. Pharmacokinetics of bevacizumab after topical, subconjunctival, and intravitreal administration in rabbits. Invest Ophthalmol Vis Sci 2009; 50: 4807–4813.
Byeon SH, Kang SY . Pharmacokinetics. Ophthalmology 2009; 116: 168–169; author reply 169–170.
Miki K, Miki A, Matsuoka M, Muramatsu D, Hackett SF, Campochiaro PA . Effects of intraocular ranibizumab and bevacizumab in transgenic mice expressing human vascular endothelial growth factor. Ophthalmology 2009; 116: 1748–1754.
Heier JS, Boyer DS, Ciulla TA, Ferrone PJ, Jumper JM, Gentile RC et al. Ranibizumab combined with verteporfin photodynamic therapy in neovascular age-related macular degeneration: year 1 results of the FOCUS Study. Arch Ophthalmol 2006; 124: 1532–1542.
Antoszyk AN, Tuomi L, Chung CY, Singh A . Ranibizumab combined with verteporfin photodynamic therapy in neovascular age-related macular degeneration (FOCUS): year 2 results. Am J Ophthalmol 2008; 145: 862–874.
Regillo CD, Brown DM, Abraham P, Yue H, Ianchulev T, Schneider S et al. Randomized, double-masked, sham-controlled trial of ranibizumab for neovascular age-related macular degeneration: PIER Study year 1. Am J Ophthalmol 2008; 145: 239–248.
Boyer DS, Heier JS, Brown DM, Francom SF, Ianchulev T, Rubio RG . A Phase IIIb study to evaluate the safety of ranibizumab in subjects with neovascular age-related macular degeneration. Ophthalmology 2009; 116: 1731–1739.
Funk M, Karl D, Georgopoulos M, Benesch T, Sacu S, Polak K et al. Neovascular age-related macular degeneration: intraocular cytokines and growth factors and the influence of therapy with ranibizumab. Ophthalmology 2009; 116: 2393–2399.
Sawada O, Miyake T, Kakinoki M, Sawada T, Kawamura H, Ohji M . Aqueous vascular endothelial growth factor after intravitreal injection of pegaptanib or ranibizumab in patients with age-related macular degeneration. Retina 2010; 30: 1034–1038.
Lu JF, Bruno R, Eppler S, Novotny W, Lum B, Gaudreault J . Clinical pharmacokinetics of bevacizumab in patients with solid tumors. Cancer Chemother Pharmacol 2008; 62: 779–786.
Beer PM, Wong SJ, Hammad AM, Falk NS, O’Malley MR, Khan S . Vitreous levels of unbound bevacizumab and unbound vascular endothelial growth factor in two patients. Retina 2006; 26: 871–876.
Funk M, Kriechbaum K, Prager F, Benesch T, Georgopoulos M, Zlabinger GJ et al. Intraocular concentrations of growth factors and cytokines in retinal vein occlusion and the effect of therapy with bevacizumab. Invest Ophthalmol Vis Sci 2009; 50: 1025–1032.
Chan WM, Lai TY, Chan KP, Li H, Liu DT, Lam DS et al. Changes in aqueous vascular endothelial growth factor and pigment epithelial-derived factor levels following intravitreal bevacizumab injections for choroidal neovascularization secondary to age-related macular degeneration or pathologic myopia. Retina 2008; 28: 1308–1313.
Zhu Q, Ziemssen F, Henke-Fahle S, Tatar O, Szurman P, Aisenbrey S et al. Vitreous levels of bevacizumab and vascular endothelial growth factor-A in patients with choroidal neovascularization. Ophthalmology 2008; 115: 1750–1755, 1755 e1751.
Krohne TU, Eter N, Holz FG, Meyer CH . Intraocular pharmacokinetics of bevacizumab after a single intravitreal injection in humans. Am J Ophthalmol 2008; 146: 508–512.
Modarres M, Naseripour M, Falavarjani KG, Nikeghbali A, Hashemi M, Parvaresh MM . Intravitreal injection of 2.5 vs 1.25 mg bevacizumab (Avastin) for treatment of CNV associated with AMD. Retina 2009; 29: 319–324.
Meyer C, Krohne T, Holz F . Intraocular pharmacokinetics after single intravitreal injection of 1.5 vs 3.0 mg bevacizumab in humans. Retina 2011 (In Press).
Wang JJ, Mitchell P, Smith W, Cumming RG, Attebo K . Impact of visual impairment on use of community support services by elderly persons: the Blue Mountains Eye Study. Invest Ophthalmol Vis Sci 1999; 40: 12–19.
Stewart MW . Predicted biologic activity of intravitreal bevacizumab. Retina 2007; 27: 1196–1200.
Shah AR, Del Priore LV . Duration of action of intravitreal ranibizumab and bevacizumab in exudative AMD eyes based on macular volume measurements. Br J Ophthalmol 2009; 93: 1027–1032.
Stepien KE, Rosenfeld PJ, Puliafito CA, Feuer W, Shi W, Al-Attar L et al. Comparison of intravitreal bevacizumab followed by ranibizumab for the treatment of neovascular age-related macular degeneration. Retina 2009; 29: 1067–1073.
Chang TS, Kokame G, Casey R, Prenner J, Feiner L, Anderson N . Short-term effectiveness of intravitreal bevacizumab versus ranibizumab injections for patients with neovascular age-related macular degeneration. Retina 2009; 29: 1235–1241.
Subramanian ML, Ness S, Abedi G, Ahmed E, Daly M, Feinberg E et al. Bevacizumab vs ranibizumab for age-related macular degeneration: early results of a prospective double-masked, randomized clinical trial. Am J Ophthalmol 2009; 148: 875–882 e871.
Subramanian ML, Abedi G, Ness S, Feinberg E, Fenberg MJ, Daly M et al. Bevacizumab vs ranibizumab: one year outcomes of a head-to-head, prospective, double-masked, randomized clinical trial. Invest Ophthalmol Vis Sci 2010; 51: E-Abstract 517.
Kent JS, Iordanous Y, Mao A, Shukla S, Sheidow TG . Comparison of outcomes when switching treatment from intravitreal bevacizumab to ranibizumab in neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2010; 51: E-Abstract 82.
Tufail A, Patel PJ, Egan C, Hykin P, da Cruz L, Gregor Z et al. Avastin (Bevacizumab) for choroidal neovascularisation in age-related macular degeneration (ABC) trial. BMJ 2010; 340: c2459.
Good TJ, Kimura AE, Mandava N, Kahook MY . Sustained elevation of intraocular pressure after intravitreal injections of anti-VEGF agents. Br J Ophthalmol; doi:10.1136/bjo.2010.180729.
Meyer CH, Krohne TU, Holz FG . Concentrations of unbound bevacizumab in the aqueous of untreated fellow eyes after a single intravitreal injection in humans. Acta Ophthalmol; doi:10.1111/j.1755-3768.2009.01842.x.
Sawada O, Kawamura H, Kakinoki M, Ohji M . Vascular endothelial growth factor in fellow eyes of eyes injected with intravitreal bevacizumab. Graefes Arch Clin Exp Ophthalmol 2008; 246: 1379–1381.
Miyake T, Sawada O, Kakinoki M, Sawada T, Kawamura H, Ogasawara K et al. Pharmacokinetics of bevacizumab and its effect on vascular endothelial growth factor after intravitreal injection of bevacizumab in macaque eyes. Invest Ophthalmol Vis Sci 2010; 51: 1606–1608.
Velez-Montoya R, Fromow-Guerra J, Burgos O, Landers III MB, Morales-Caton V, Quiroz-Mercado H . The effect of unilateral intravitreal bevacizumab (avastin), in the treatment of diffuse bilateral diabetic macular edema: a pilot study. Retina 2009; 29: 20–26.
Schmid-Kubista KE, Krebs I, Gruenberger B, Zeiler F, Schueller J, Binder S . Systemic bevacizumab (Avastin) therapy for exudative neovascular age-related macular degeneration. The BEAT-AMD-Study. Br J Ophthalmol 2009; 93: 914–919.
Wu Z, Sadda SR . Effects on the contralateral eye after intravitreal bevacizumab and ranibizumab injections: a case report. Ann Acad Med Singapore 2008; 37: 591–593.
Matsuyama K, Ogata N, Matsuoka M, Wada M, Takahashi K, Nishimura T . Plasma levels of vascular endothelial growth factor and pigment epithelium-derived factor before and after intravitreal injection of bevacizumab. Br J Ophthalmol 2010; 94: 1215–1218.
Petrou P, Georgalas I, Giavaras G, Anastasiou E, Ntana Z, Petrou C . Early loss of pregnancy after intravitreal bevacizumab injection. Acta Ophthalmol 2010; 88: e136.
Yoon YH, Kim JG, Chung H, Lee SY . Rapid progression of subclinical age-related macular degeneration in the untreated fellow eye after intravitreal bevacizumab. Acta Ophthalmol 2009; 87: 685–687.
Mennel S, Callizo J, Schmidt JC, Meyer CH . Acute retinal pigment epithelial tear in the untreated fellow eye following repeated bevacizumab (Avastin) injections. Acta Ophthalmol Scand 2007; 85: 689–691.
Eremina V, Jefferson JA, Kowalewska J, Hochster H, Haas M, Weisstuch J et al. VEGF inhibition and renal thrombotic microangiopathy. N Engl J Med 2008; 358: 1129–1136.
Novartis. Lucentis prescribing information. 2006.
Gamulescu MA, Helbig H . Lack of therapeutic effect of ranibizumab in fellow eyes after intravitreal administration. J Ocul Pharmacol Ther 2010; 26: 213–216.
Barbazetto IA, Saroj N, Shapiro H, Wong P, Ho AC, Freund KB . Incidence of new choroidal neovascularization in fellow eyes of patients treated in the MARINA and ANCHOR trials. Am J Ophthalmol 2010; 149: 939–946 e931.
Rouvas A, Liarakos VS, Theodossiadis P, Papathanassiou M, Petrou P, Ladas I et al. The effect of intravitreal ranibizumab on the fellow untreated eye with subfoveal scarring due to exudative age-related macular degeneration. Ophthalmologica 2009; 223: 383–389.
Schmidt-Erfurth U . Clinical safety of ranibizumab in age-related macular degeneration. Expert Opin Drug Saf 2010; 9: 149–165.
USP 28/NF 23. Chapter <789> ‘Particulate matter in ophthalmic solutions’. In: United States Pharmacopeial Convention, Inc: Rockville, MD, 2005.
USP 28/NF 23. Chapter <788> ‘Particulate matter in injections’. In: United States Pharmacopeial Convention, Inc: Rockville, MD, 2005.
Acknowledgements
We acknowledge Matthew Cunningham of Alpha-Plus Medical Communications Ltd., UK, who provided medical writing services, with funding from Novartis Pharma AG, Basel, Switzerland. This service encompassed the preparation of a first draft, editing, checking content and language, formatting, referencing, preparing tables and figures, and incorporating the authors’ revisions, all carried out under our direction. At all stages, we had control over the content of this manuscript, for which we have given final approval and taken full responsibility.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Frank Holz has provided expert consultation services to and received speaker honoraria from Novartis Pharmaceuticals Corporation, Pfizer, Genentech, and Alcon. Carsten Meyer has no conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Meyer, C., Holz, F. Preclinical aspects of anti-VEGF agents for the treatment of wet AMD: ranibizumab and bevacizumab. Eye 25, 661–672 (2011). https://doi.org/10.1038/eye.2011.66
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.66
Keywords
This article is cited by
-
Nanomedicine and drug delivery to the retina: current status and implications for gene therapy
Naunyn-Schmiedeberg's Archives of Pharmacology (2022)
-
Preclinical assessment of intravitreal ramucirumab: in vitro and in vivo safety profile
International Journal of Retina and Vitreous (2020)
-
Evaluation of long-term intravitreal anti-vascular endothelial growth factor injections on renal function in patients with and without diabetic kidney disease
BMC Nephrology (2019)
-
Early changes in macular optical coherence tomography parameters after Ranibizumab intravitreal injection in patients with exsudative age-related macular degeneration
International Journal of Retina and Vitreous (2018)
-
Makula-Atrophie bei feuchter altersabhängiger Makuladegeneration
Der Ophthalmologe (2016)