Abstract
High-resolution genome-wide array analysis enables detailed screening for cryptic and submicroscopic imbalances of microscopically balanced de novo rearrangements in patients with developmental delay and/or congenital abnormalities. In this report, we added the results of genome-wide array analysis in 54 patients to data on 117 patients from seven other studies. A chromosome imbalance was detected in 37% of all patients with two-breakpoint rearrangements. In 49% of these patients, the imbalances were located in one or both breakpoint regions. Imbalances were more frequently (90%) found in complex rearrangements, with the majority (81%) having deletions in the breakpoint regions. The size of our own cohort enabled us to relate the presence of an imbalance to the clinical features of the patients by using a scoring system, the De Vries criteria, that indicates the complexity of the phenotype. The median De Vries score was significantly higher (P=0.002) in those patients with an imbalance (5, range 1–9) than in patients with a normal array result (3, range 0–7). This study provides accurate percentages of cryptic imbalances that can be detected by genome-wide array analysis in simple and complex de novo microscopically balanced chromosome rearrangements and confirms that these imbalances are more likely to occur in patients with a complex phenotype.
Similar content being viewed by others
Introduction
The estimated frequency of balanced chromosome rearrangements in a population of unselected newborns is 0.52%.1 The majority of these translocations, insertions and inversions is transmitted from one of the parents and not associated with abnormal phenotypes.2 In 1991, Warburton3 reported data on the frequency and outcome of cases with apparently balanced, de novo, rearrangements detected at amniocentesis in over 350 000 pregnancies. She found that a microscopically balanced, de novo, reciprocal translocation was detected in 1 out of every 2000 pregnancies. The frequency of congenital abnormalities in fetuses and newborns with de novo, reciprocal translocations or inversions has been estimated at 6.1 and 9.4%, respectively.3 This is more than twice as high as the risk of 2–3% in the general population. The increased number of abnormal phenotypes can be caused by: (1) a microdeletion or microduplication at the translocation or inversion breakpoint(s) which is only detectable by high-resolution techniques, (2) disruption or modulation of the expression of gene(s) located at the breakpoint(s) and (3) otherwise inactivation (position effect) of gene(s) at the breakpoint region(s). Thus, an apparently balanced, de novo, chromosome rearrangement can underlie an abnormal phenotype, but it may also be coincidental. The actual confirmation or rejection of causality by detecting a cryptic deletion or duplication at the assumed breakpoints or elsewhere in the genome is often lacking. The unbalanced nature of small rearrangements will most often escape detection, as the resolution of standard cytogenetic banding techniques is only 5–10 Mb. It has already been shown that the yield of chromosome abnormalities in patients with developmental delay (DD) and/or multiple congenital anomalies (MCA) increases considerably with the resolution of the technique used. A microscopically visible chromosome abnormality can be detected by routine karyotyping in 3–5% of all DD/MCA patients, excluding Down's syndrome,4, 5, 6 whereas genome-wide array-based techniques are able to detect a chromosome imbalance in up to 15–20% of such cases.6, 7, 8
Recent studies have reported on genome-wide array analysis used to identify cryptic imbalances in cohorts of DD/MCA patients with an apparently balanced, de novo, chromosome rearrangement (Table 1).9, 10, 11, 12, 13, 14, 15 A cryptic imbalance was detected by genome-wide array analysis in 33–100% of DD/MCA patients with a de novo chromosome rearrangement. In the majority of patients, the imbalance was detected at one or more breakpoints, although a large percentage of imbalances (15–40%) was found elsewhere in the genome. The frequency of detected imbalances is significantly higher in patients with a more complex chromosome rearrangement (CCR), involving more than two chromosomes and/or more than two breakpoints.9, 10, 14 In all studies, the reported imbalances were assumed to cause the abnormal phenotype.
In contrast to the studies performed in DD/MCA patients, Baptista et al12, 16 compared a cohort of 31 phenotypically normal individuals carrying a balanced chromosome rearrangement with a cohort of 14 DD/MCA patients. No genomic imbalances at the breakpoints, or elsewhere in the genome, were detected in the 31 normal carriers, whereas a disease-causing imbalance was detected in 4 out of 14 DD/MCA patients. The authors concluded that translocations in patients with a clinically abnormal phenotype are molecularly distinct from those in normal individuals. An unexpected finding was that the frequency of gene disruption due to a chromosome rearrangement did not differ between phenotypically abnormal patients and the normal study population.12 However, the percentage of disrupted genes that have a role in the nervous system was higher in the phenotypically abnormal patients.
Since there is limited data on patients with apparently balanced chromosome rearrangements, we decided to evaluate the results obtained from genome-wide array analysis in a cohort of 54 DD/MCA patients and a cytogenetically balanced, de novo, chromosome rearrangement. Since this is the largest postnatal cohort of DD/MCA patients with de novo balanced rearrangements reported thus far, we were able to improve the estimated percentage of submicroscopic imbalances detected by genome-wide array analysis in de novo chromosome rearrangements. The size of the cohort also enabled us to relate the probability of finding an imbalance to the clinical phenotype of the patient by using the De Vries scoring system.17
Patients and methods
Patient selection
Clinical data and samples were collected from 54 patients with an apparently balanced, de novo, structural chromosome rearrangement. All patients had been referred for karyotyping because of DD and/or MCA and were enrolled in the study for diagnostic purposes. All chromosome rearrangements were detected by routine cytogenetic analysis at a minimum band level of 500: 46 patients carried a two-breakpoint rearrangement; 40 patients had a reciprocal translocation, while 6 patients carried an inversion. Eight patients had a CCR with at least three breakpoints.
All patients, parents or legal representatives gave informed consent for this study, according to local guidelines.
Collection of clinical data
Clinical data were derived from medical records using a standardized form. Additional information was requested from the referring clinicians whenever necessary. All patients were scored according to adapted De Vries criteria, which provided a checklist for patients with submicroscopic subtelomeric rearrangements (Table 2).17 Family history was replaced by DD in this scoring system, because a positive family history, either compatible or non-compatible with Mendelian inheritance, does not enhance the chance of finding imbalances in the breakpoint regions in patients with a de novo chromosome rearrangement. In contrast, the De Vries criteria were developed for patients with an intellectual disability, while not all the patients in our study had a DD. Therefore, one and two points were given for mild-to-moderate and severe DD, respectively. Severe DD was defined as a Developmental Quotient <30, while mild-to-moderate DD was a Developmental Quotient between 30 and 70. In this way, the maximum number of points that could be scored remained 10 (Table 2).
Genome-wide array analysis
Array analysis with an average genome-wide resolution of ∼200 kb was performed using either an Agilent 105k or 244k oligo array, a 32k BAC array as previously described,18 or the Affymetrix 250k SNP array platform,19 following the protocols provided by the manufacturers (Agilent Technologies and Affymetrix Inc., Santa Clara, CA, USA).
For the Agilent array reference DNA, a mixture of 40 male or female DNA samples of the same gender was used as control. The data were processed using Feature Extraction V.9.1 and CGH analytics V.3.4.27 provided by the manufacturer (Agilent Technologies). For the SNP array experiments, copy number estimates were determined using the updated version 2.0 of the CNAG (Copy Number Analyzer for Affymetrix GeneChip mapping) software package.20 The normalized ratios were then analyzed for genomic imbalances by a standard Hidden Markov Model, essentially as described before.18 The SNP array data obtained from patient DNA were compared with SNP array data from 10 healthy, sex-matched individuals.
Regardless of the array platform employed, genome-wide data analysis was performed using previously determined criteria which provide 95% confidence of representing a true copy number variation (CNV).21 A CNV was considered significant if five or more consecutive probes showed a single copy number loss (N=1), or at least seven consecutive SNPs showed a single copy number gain (N=3) for the Affymetrix array, or four or more consecutive probes showed gains or losses for the Agilent array. For interpretation purposes, various public web sources were consulted, including the Online Mendelian Inheritance of Man (http://www.ncbi.nlm.nih.gov/Omim), the DECIPHER database (http://decipher.sanger.ac.uk) and ECARUCA (http://www.ecaruca.net). A CNV was considered a normal genomic variant if it had been detected in at least three control individuals as reported in the Database of Genomic Variants (http://projects.tcag.ca/variants), and/or been encountered in at least three in-house control samples. Data analyses were based on the NCBI36/hg18 build of the human genome.
Fluorescent in situ hybridization analysis
To validate the gains or losses identified by genome-wide array analysis, region-specific fluorescent in situ hybridization (FISH) was performed following routine protocols. Bacterial Artificial Chromosome (BAC) clones were selected from the human library RPCI-11 according to the UCSC Human Genome Assembly (freeze March 2006) and kindly provided by the Wellcome Trust Sanger Institute (http://www.sanger.ac.uk) or obtained from the 32k set of BAC DNAs in the Nijmegen laboratory. BAC DNA was indirectly labeled with biotin- or digoxigenin-11-dUTP using Nick translation. Slides were hybridized overnight at 37 °C and fluorescently labeled with FITC or Texas Red.
Multiplex ligation-dependent probe amplification
To validate the gains identified by array analysis, region-specific multiplex ligation-dependent probe amplification (MLPA) was performed. For each region, two uniquely sized probes were developed in accordance with a protocol provided by MRC Holland (Amsterdam, the Netherlands). Ten probes were combined in one MLPA assay together with a DNA quantity and a DNA denaturation control mix (EK-1 kit, MRC Holland). The procedure was further carried out as described by De Vries et al.18
Results
In this study, 54 patients with an apparently balanced, de novo chromosome rearrangement and an abnormal clinical phenotype were analyzed for submicroscopic chromosome imbalances by genome-wide array analysis. Forty-six patients had a two-breakpoint rearrangement upon routine karyotyping. In eight patients, a more complex aberration was found. All patients had facial dysmorphisms and/or congenital malformations and 46 out of 52 patients (88%) showed DD, varying from mild psychomotor retardation and speech delay to severe DD. Development could not be assessed in two patients because they died at the age of 1 day and 2 months, respectively (patients 12 and 43). A detailed description of all the phenotypes is presented in Table 3.
The total number of CNVs, including well-known benign CNVs, detected by the platforms used ranged from 2 to 12 with an average of 5.6 per patient (Table 3). All the potentially causative, copy number alterations detected by array could be confirmed by FISH (losses), MLPA (gains) or an independent array platform.
CNVs at or near the breakpoint regions
In 11 out of 54 patients (20%), the apparently balanced rearrangement was found to be unbalanced at the breakpoint region(s). We found no gains but 16 losses in these 11 patients in total (Table 4A). The size of the losses varied from 0.1 to 15.3 Mb. Seven patients had a single loss, two patients (6 and 53) had losses at multiple breakpoints and two patients (49 and 51) had multiple, non-overlapping losses in one breakpoint region. Patient 51 also had a loss elsewhere in the genome (Table 4B). In patient 6, with a loss at both breakpoints (1p22.1 and 6q15), the 1.1-Mb loss of chromosome 1 appeared to contain no known genes. The 4.25-Mb deletion in patient 42 contained the FBN1 gene, explaining the observed Marfan phenotype.22
Five out of forty-six (11%) patients with a two-breakpoint chromosome rearrangement had a cryptic imbalance related to their reciprocal translocation. No imbalances were found related to inversions (n=6). Six out of eight (75%) patients with a CCR (more than two breakpoints) appeared to have an abnormal genome profile upon array analysis. All of these six patients had losses at the breakpoint regions.
Imbalances elsewhere in the genome
Copy number changes elsewhere in the genome were present in seven patients: six patients had a reciprocal translocation and one patient had a CCR (Table 4B). Six losses and three gains not related to the breakpoints were detected in total in these seven patients. Only the patient with a CCR (51) had additional copy number alterations at one of the breakpoint regions (Table 4A). In this and two other patients (30 and 32), the respective CNV was inherited from a healthy parent. Patient 29 had three imbalances: two losses were de novo (on the paternal allele) and one loss was also observed in his healthy father.
In an adult patient (10) with a translocation (1;17)(p36.1;q11), a 650-kb gain in 1p34.1 was found. Unfortunately, this patient's parents were not available for further investigation. A partially overlapping, de novo 650 kb gain was found in a clinically more severely affected boy (18). Both gains overlap a 450-kb region in 1p34.1.
The last imbalance detected elsewhere was a 270-kb deletion at 5p13.1 in a patient with a translocation (2;10) (patient 16). Unfortunately, this patient's parents were not available for further investigation.
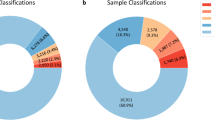
Clinical criteria
All but three patients (n=51) could be scored according to the adapted clinical De Vries criteria (Tables 2 and 3).17 Patient 43 died 1 day postpartum, patient 12 died at the age of 2 months, and patient 52 had Sotos syndrome due to an NSD1 mutation interfering with the phenotype. The distribution of the scores is shown in Supplementary Figure 1. All patients with a chromosome imbalance in the breakpoint region (n=11) had a score of at least 3 with a median score of 5 (range 3–9). The highest score was found in the patient with imbalances both at a breakpoint and elsewhere (score 9 in patient 51). Patients with a chromosome imbalance restricted to elsewhere in the genome (n=6) tended to have a lower score (median 4.5, range 1–6). One of the imbalances in this group was considered not clinically relevant (see Discussion and Table 4B). Correction for this patient 32 led to a median score of 5 (range 1–6). The median score in the total group with a possibly clinically relevant CNV (n=16) was 5 (range 1–9), while the median score in the group without a significant CNV (n=35) was 3 (range 0–7). The difference between these two groups is significant (P=0.002, Mann–Whitney U-test).
Discussion
In this study, 54 patients with an apparently balanced, de novo chromosome rearrangement were examined by high-resolution genome-wide array analysis. The mean number of CNVs, including well-known recurrent copy number polymorphisms, that was detected was 5.6 per patient (range 2–12). In general, the number of CNVs detected per patient depends on the platform and detection thresholds used, but the number found in our study does not differ substantially from patients without apparently balanced rearrangements.18, 23
Out of 46 patients with a two-breakpoint chromosome rearrangement, 11 (25%) appeared to have an abnormal genome profile encompassing six losses, each at one of the breakpoints in five patients, and five losses and three gains elsewhere in the genome in six patients. From analysis of their parents, two of the latter category could be specified as rare, inherited CNVs. Six out of eight patients with a CCR were found to have one or more clinically significant losses at one of the breakpoints. In addition, one of these six patients had a paternally inherited imbalance elsewhere in the genome. Although the overall percentage of patients with a cryptic or submicroscopic, clinically significant imbalance in this cohort is 31%, there is a remarkable difference between patients with a two-breakpoint chromosome rearrangement (24%) and those with a more complex rearrangement (75%).
The number of imbalances seen in our patient cohort is similar to the studies of Sismani et al11 and Baptista et al,12 but lower than the studies of others (Table 1).9, 10, 13, 14, 15 This might be due to differences in patient selection (reflected in the high number of aberrations found elsewhere in the genome in the studies of Gribble, Higgins and Gijsbers) and to the higher number of complex rearrangements studied by De Gregori. Compiling the data of the previous and present studies, we conclude that in almost half of the patients with a de novo chromosome rearrangement, a genomic imbalance can be detected by genome-wide array analysis. We confirmed that, in complex rearrangements, the chance of finding copy number alterations at the breakpoints is very high: 75 and 72%, in our study and the combined studies, respectively.
Imbalances are not always located at breakpoints
In most patients (20%) with clinically relevant copy number alterations, the imbalance is detected in or near the breakpoints of the chromosomes involved (Table 4A). However, in 13% an imbalance is found elsewhere in the genome (Table 4B). As shown here and in previous studies, this was especially true for two-breakpoint de novo aberrations. In 19% of all patients with a two-breakpoint rearrangement, imbalances are found elsewhere. Especially in these cases, the clinical significance of the detected CNVs should be determined by parental analysis, among other investigations. The observed percentage of 19% is in agreement with the general figure of 17% of imbalances that is found in the DD/MCA population.7, 8 These results underline the importance of a genome-wide approach in patients with an apparently balanced, de novo chromosome rearrangement. If imbalances are found independent of the rearrangement breakpoints, this may have implications for the recurrence risk and warrants studies in the parents to exclude cryptic balanced translocations and insertions. Furthermore, it is crucial to critically examine an apparently balanced rearrangement after initial detection, because they are often more complex than they appear at first.
Losses are more frequent than gains at breakpoints
The clinically significant imbalances at the breakpoint regions found in this study were all deletions. Breakpoint deletions are more frequent in patients with a CCR than in patients with a two-breakpoint rearrangement. In the present study, we detected deletions in six out of eight CCR patients (75%). This is comparable to the results of De Gregori et al10 and Schluth-Bolard et al,14 who detected deletions in 69 and 80% of patients with a de novo CCR, respectively. Thus, deletions may be the main cause of phenotypic abnormalities in patients with a CCR.
The preponderance of deletions is similar to the results of others (Table 1).9, 10, 12, 13, 14 Recently, Howarth et al24 showed that in breast cancer cell lines reciprocal translocations arising during mitosis may result in both deletions (up to 31 Mb) and duplications (up to 200 kb) at the breakpoint regions. They demonstrated that the underlying mechanism most likely is stalled replication bubbles during the interchromosomal exchange. De novo constitutional translocations have their origin during meiosis. Nonetheless, the same mechanism may cause imbalances during meiotic interchromosomal exchanges. That we and others did not find breakpoint duplications in DD/MCA patients might be explained by their size (often under the detection threshold) and the fact that small duplications rarely result in a phenotype.
Clinical significance of the detected imbalances
The size of the deletions and gains in our patients ranged from 100 kb to 15.3 Mb and from 240 to 650 kb, respectively. In patient 6 with deletions at both breakpoints, the abnormal phenotype was considered to be a consequence of the 9.2-Mb deletion at chromosome 6, because the small deletion at chromosome 1 did not contain any known genes. All other breakpoint deletions were considered pathogenic based on the criteria mentioned in Methods.
In four of the seven patients with an imbalance elsewhere in the genome, the imbalance was found to be inherited from a clinically unaffected parent. The deletion 16p13.11 (patient 30) and deletion 1q21.1 (patient 51) are known microdeletion syndromes with variable phenotypes.25, 26, 27 Patient 51 also carries two significant losses at a breakpoint region, but we cannot exclude that the 1q21.1 deletion also contributes to the phenotype. The maternally inherited gain in 1q23.3 (patient 32) was considered unlikely to be clinically relevant because a larger gain has been detected in two control individuals from one study in the Database of Genomic Variants.23 The paternally inherited loss in patient 29 is in a gene-less region of 12p11.22 and therefore likely to be benign. Of the two de novo losses in the same patient (29), the 4.9-Mb loss in 2q33.3q34 is most likely to be clinically relevant. The 9q21.12q21.1 loss has not been detected before; and thus, its clinical significance remains uncertain, although a contribution to the clinical phenotype of patient 29 cannot be excluded.
The 650-kb gain in 1p34 in patient 10 is not a known polymorphism according to the Database of Genomic Variants, and is only partially overlapping gains that have been found in normal individuals (Nijmegen and Groningen in-house control data). Patient 18 had a similarly sized duplication, of which 450 kb overlapped with the gain of patient 10. The distal 200 kb, non-overlapping region, contains several genes, including POMGNT1. The phenotype of patient 18 is similar to previously published patients with larger overlapping duplications that included this gene.28
The 270-kb loss in 5p13.1 (patient 16) is not a known polymorphism but only contains the LIFR gene involved in autosomal recessive Stuve-Wiedemann syndrome, although the patient's clinical features do not resemble this syndrome. Unfortunately, the parents were unavailable for further studies and the clinical significance of the deletion remains unclear, as no similar microdeletion has been found in controls or other patients so far.
Thus, in at least four of the seven patients with imbalances elsewhere, the detected imbalance was considered to contribute to the abnormal phenotype.
Clinical features pointing to an imbalance
All 16 patients with a potentially clinically relevant CNV showed DD, ranging from mild psychomotor or speech delay (in five patients) to severe DD (in seven patients). As discussed above, the gain in patient 32 with severe DD was, in retrospect, considered very unlikely to be causative for the phenotype. If we had only analyzed patients with an adapted De Vries score >3, we would not have missed any clinically relevant chromosome imbalances at the breakpoint regions (Supplementary Figure 1). This is in line with the results of the original study using De Vries criteria: all patients with a subtelomeric aberration had a De Vries score of at least 3.17
Two out of six patients with an aberration elsewhere in the genome had a score <3. This concerned the maternally inherited 1q23 gain in patient 32 (score 2) that was considered unlikely to be clinically relevant, and one 1p34 gain in patient 10 of uncertain clinical relevance (score 1). The median De Vries score of all 14 patients with a certainly clinically relevant CNV (Table 4) was 5 (range 3–9), while in the 35 patients without a relevant CNV the median score was 3 (range 0–7). Three patients could not be scored (see Results), and two patients had an imbalance of uncertain clinical relevance.
Other mechanisms causing DD/MCA in balanced rearrangements
A truly balanced, de novo chromosome rearrangement may still contribute to an abnormal clinical phenotype due to disruption of a gene or due to a position effect. An example of the former was seen in patient 45 who appeared to have a disruption of the TCF4 gene at 18q21.1, as described in a previous study.29 Conventional methods for mapping chromosome breakpoints, such as FISH, are laborious, and often fail to identify the disrupted gene. Combining DNA array hybridization with chromosome sorting improves the efficiency of breakpoint mapping, but can only be applied when the physical properties of the derivative chromosomes allow them to be flow sorted. Nowadays more efficient and accurate breakpoint identification can be performed by next-generation paired-end sequencing.30
A position effect was most likely responsible for the split-hand-feet syndrome (SHFM) in patient 37 with an inversion breakpoint in 7q near the SHFM1 locus and the candidate genes DSS1, DLX5 and DLX6.31
Conclusion
The combined results of our study and previous reports show that in 79/171 (46%) of DD/MCA patients with a de novo chromosome rearrangement, a genomic imbalance could be detected by genome-wide array analysis. In patients with a rearrangement involving more than two breakpoints, there is a high chance of detecting an imbalance at one of the breakpoints (21/29; 72%). In two-breakpoint rearrangements, an imbalance located at a breakpoint was detected in 26/142 (18%) patients. However, a substantial number of imbalances were also detected outside the breakpoint regions: in 33/171 (19%) patients, an imbalance was found elsewhere in the genome, which is comparable to the general DD/MCA population. In conclusion, diagnostic studies should not only focus on the rearrangement breakpoints, but a genome-wide approach should be used to investigate patients with apparently balanced, de novo chromosome rearrangements.
References
Jacobs PA, Browne C, Gregson N, Joyce C, White H : Estimates of the frequency of chromosome abnormalities detectable in unselected newborns using moderate levels of banding. J Med Genet 1992; 29: 103–108.
Gardner RJMS, Sutherland GR : Chromosome Abnormalities and Genetic Counseling, 3rd edn. Oxford University Press: New York, 2004.
Warburton D : De novo balanced chromosome rearrangements and extra marker chromosomes identified at prenatal diagnosis: clinical significance and distribution of breakpoints. Am J Hum Genet 1991; 49: 995–1013.
Rauch A, Hoyer J, Guth S et al: Diagnostic yield of various genetic approaches in patients with unexplained developmental delay or mental retardation. Am J Med Genet A 2006; 140: 2063–2074.
Hochstenbach R, van Binsbergen E, Engelen J et al: Array analysis and karyotyping: workflow consequences based on a retrospective study of 36 325 patients with idiopathic developmental delay in the Netherlands. Eur J Med Genet 2009; 52: 161–169.
Miller DT, Adam MP, Aradhya S et al: Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am J Hum Genet 2010; 86: 749–764.
Stankiewicz P, Beaudet AL : Use of genome-wide array analysis in the evaluation of dysmorphology, malformations, developmental delay, and idiopathic mental retardation. Curr Opin Genet Dev 2007; 17: 182–192.
Vissers LE, de Vries BB, Veltman JA : Genomic microarrays in mental retardation: from copy number variation to gene, from research to diagnosis. J Med Genet 2010; 47: 289–297.
Gribble SM, Prigmore E, Burford DC et al: The complex nature of constitutional de novo apparently balanced translocations in patients presenting with abnormal phenotypes. J Med Genet 2005; 42: 8–16.
De Gregori M, Ciccone R, Magini P et al: Cryptic deletions are a common finding in ‘balanced’ reciprocal and complex chromosome rearrangements: a study of 59 patients. J Med Genet 2007; 44: 750–762.
Sismani C, Kitsiou-Tzeli S, Ioannides M et al: Cryptic genomic imbalances in patients with de novo or familial apparently balanced translocations and abnormal phenotype. Mol Cytogenet 2008; 1: 15.
Baptista J, Mercer C, Prigmore E et al: Breakpoint mapping and genome-wide array analysis in translocations: comparison of a phenotypically normal and an abnormal cohort. Am J Hum Genet 2008; 82: 927–936.
Higgins AW, Alkuraya FS, Bosco AF et al: Characterization of apparently balanced chromosomal rearrangements from the developmental genome anatomy project. Am J Hum Genet 2008; 82: 712–722.
Schluth-Bolard C, Delobel B, Sanlaville D et al: Cryptic genomic imbalances in de novo and inherited apparently balanced chromosomal rearrangements: array CGH study of 47 unrelated cases. Eur J Med Genet 2009; 52: 291–296.
Gijsbers ACJ, Bosch CAJ, Dauwerse JG et al: Additional cryptic CNVs in mentally retarded patients with apparently balanced karyotypes. Eur J Med Genet 2010; 53: 227–233.
Baptista J, Prigmore E, Gribble SM, Jacobs PA, Carter NP, Crolla JA : Molecular cytogenetic analyses of breakpoints in apparently balanced reciprocal translocations carried by phenotypically normal individuals. Eur J Hum Genet 2005; 13: 1205–1212.
de Vries BB, White SM, Knight SJ et al: Clinical studies on submicroscopic subtelomeric rearrangements: a checklist. J Med Genet 2001; 38: 145–150.
de Vries BB, Pfundt R, Leisink M et al: Diagnostic genome profiling in mental retardation. Am J Hum Genet 2005; 77: 606–616.
McMullan DJ, Bonin M, Hehir-Kwa JY et al: Molecular karyotyping of patients with unexplained mental retardation by SNP arrays: a multicenter study. Hum Mutat 2009; 30: 1082–1092.
Nannya Y, Sanada M, Nakazaki K et al: A robust algorithm for copy number detection using high-density oligonucleotide single-nucleotide polymorphism genotyping arrays. Cancer Res 2005; 65: 6071–6079.
Hehir-Kwa J, Egmont-Petersen M, Janssen I, Smeets D, van Kessel A, Veltman J : Genome-wide copy number profiling on high-density bacterial artificial chromosomes, single-nucleotide polymorphisms, and oligonucleotide microarrays: a platform comparison based on statistical power analysis. DNA Res 2007; 14: 1–11.
Hilhortst-Hofstee Y, Hamel BCJ, Verheij JBGM et al: The clinical spectrum of complete FBN1 allele deletions. Eur J Hum Genet 2011; 19: 247–252.
Shaikh TH, Gai X, Perin JC et al: High-resolution mapping and analysis of copy number variations in the human genome: a data resource for clinical and research applications. Genome Res 2009; 19: 1682–1690.
Howarth KD, Pole JCM, Beavis JC et al: Large duplications at reciprocal translocation breakpoints that might be the counterpart of large deletions and could arise from stalled replication bubbles. Genome Res 2011; 21: 525–534.
Mefford HC, Muhle H, Ostertag P et al: Genome-wide copy number variation in epilepsy: novel susceptibility loci in idiopathic generalized and focal epilepsies. PLoS Genet 2010; 6: e1000962.
de Kovel CG, Trucks H, Helbig I et al: Recurrent microdeletions at 15q11.2 and 16p13.11 predispose to idiopathic generalized epilepsies. Brain 2010; 133: 23–32.
Mefford HC, Sharp AJ, Baker C et al: Recurrent rearrangements of chromosome 1q21.1 and variable pediatric phenotypes. N Engl J Med 2008; 359: 1685–1699.
Hanemaaijer N, Dijkhuizen T, Haadsma M et al: A 649 kb microduplication in 1p34.1, including POMGNT1, in a patient with microcephaly, coloboma and laryngomalacia; and a review of the literature. Eur J Med Genet 2009; 52: 116–119.
Kalscheuer VM, Feenstra I, van Ravenswaaij-Arts CM et al: Disruption of the TCF4 gene in a girl with mental retardation but without the classical Pitt-Hopkins syndrome. Am J Med Genet A 2008; 146: 2053–2059.
Chen W, Ullmann R, Langnick C et al: Breakpoint analysis of balanced chromosome rearrangements by next-generation paired-end sequencing. Eur J Hum Genet 2010; 18: 539–543.
van Silfhout AT, van den Akker PC, Dijkhuizen T et al: Split hand/foot malformation due to chromosome 7q aberrations (SHFM1): additional support for functional haploinsufficiency as the causative mechanism. Eur J Hum Genet 2009; 17: 1432–1438.
Verhoeven WMA, Tuerlings JHAM, van Ravenswaay-Arts CMA, Boermans JAJ, Tuinier S : Chromosome abnormalities in clinical psychiatry: a report of two older patients. Eur J Psychiatry 2007; 21: 207–211.
Verhoeven WMA, van Ravenswaaij-Arts CMA, de Leeuw N et al: Disturbed serine metabolism and psychosis in a patient with a de novo translocation (2;10)(p23;q22.1). Genet Couns 2006; 17: 421–428.
Concannon N, Hegarty AM, Stallings RL, Reardon W : Coffin-Lowry phenotype in a patient with a complex chromosome rearrangement. J Med Genet 2002; 39: e41.
Acknowledgements
We are grateful to all the patients and their parents for their kind cooperation. We would also like to thank the requesting physicians, Bregje van Bon, Ineke van de Burgt, Ton van Essen, Ben Hamel, Marjolijn Jongmans, Tjitske Kleefstra, Carlo Marcelis, Sonja de Munnik, Gretel Oudesluijs, C Nur Semerci, Liesbeth Spruijt, Irene Stolte-Dijkstra, Peter van Tintelen, Joep Tuerlings and Michèl Willemsen, for their contribution. Special thanks to the Array Diagnostics teams of Groningen and Nijmegen, to Hanneke Mieloo for extensive FISH analyses, to Marian Bakker for statistical assistance and to Jackie Senior for editorial support. This work was supported by grants from the Netherlands Organization for Health Research and Development (ZonMW 917-86-319 to BdV) and the Brain Foundation of the Netherlands (Hersenstichting) (BdV)
Web resources
The URLs for data presented here are as follows:
Database of Genomic Variants (DGV), http://projects.tcag.ca/variation/
DECIPHER database, http://decipher.sanger.ac.uk/
European Cytogeneticists Association Register for Unbalanced Chromosome Aberrations (ECARUCA), http://ecaruca.net
Ensembl Human Genome Browser, http://www.ensembl.org/Homo_sapiens/
Online Mendelian Inheritance in Man, http://www.ncbi.nlm.nih.gov/Omim
University of California-Santa Cruz Human Genome Browser, http://genome.ucsc.edu/
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on European Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Feenstra, I., Hanemaaijer, N., Sikkema-Raddatz, B. et al. Balanced into array: genome-wide array analysis in 54 patients with an apparently balanced de novo chromosome rearrangement and a meta-analysis. Eur J Hum Genet 19, 1152–1160 (2011). https://doi.org/10.1038/ejhg.2011.120
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2011.120
Keywords
This article is cited by
-
Evaluation of genetic risk of apparently balanced chromosomal rearrangement carriers by breakpoint characterization
Journal of Assisted Reproduction and Genetics (2024)
-
Identification of a familial complex chromosomal rearrangement by optical genome mapping
Molecular Cytogenetics (2022)
-
The phenotypic spectrum and genotype-phenotype correlations in 106 patients with variants in major autism gene CHD8
Translational Psychiatry (2022)
-
Mosaicism for structural non-centromeric autosomal rearrangements in disease-defined carriers: sex differences in the rearrangements profile and maternal age distributions
Molecular Cytogenetics (2017)
-
Targeted sequencing identifies 91 neurodevelopmental-disorder risk genes with autism and developmental-disability biases
Nature Genetics (2017)