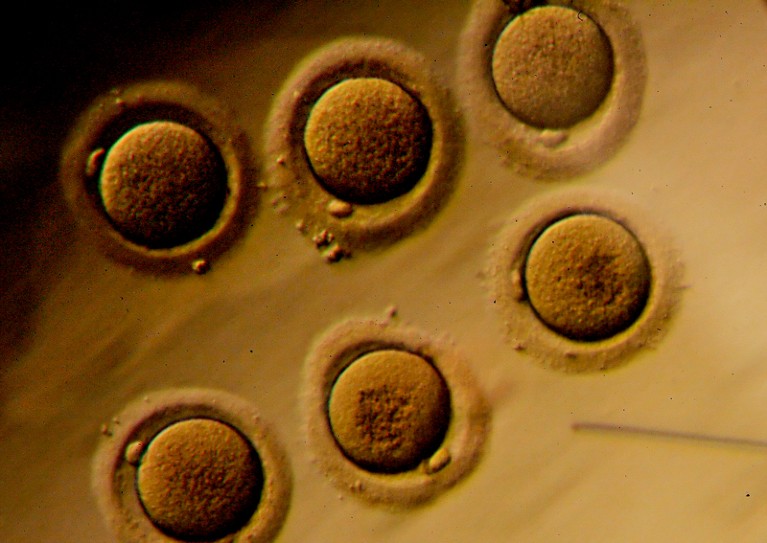
The ethical and moral issues around gene editing in human embryos have become a topic of debate worldwide.Credit: Sandy Huffaker/Bloomberg/Getty
Late last month, China’s health ministry released draft guidelines aimed at stopping rogues from prematurely using new and unapproved biomedical technologies in the clinic. The regulations require that the riskiest of techniques — including human gene editing — be approved by China’s health ministry first.
Nowhere in the announcement, in the regulations or in a background document, is the name He Jiankui. But the controversy surrounding He — who last year announced the birth of gene-edited babies — was clearly the driving force behind the guidelines. China is embarrassed by He’s widely condemned work, which flouted conventions of safety and research ethics. Its latest regulations — which include threats of fines and blacklists, and references to pre-existing laws — are clearly designed to create a stronger deterrent.
Adopt a moratorium on heritable genome editing
How to stop the next gene-editing rogue is a pressing topic for researchers around the world. In Nature this week, an international group of ethicists and researchers, including some of those who originally developed CRISPR–Cas9 as a gene-editing tool, call for a moratorium on clinical use of human germline editing — introducing heritable changes to sperm, eggs or embryos — until the safety of the technique has been better investigated and acceptable uses agreed on. The US National Institutes of Health has supported the call.
Whether such a moratorium would be effective is one point being actively debated by the research community, national academies and groups such as the World Health Organization (WHO). Just as important is whether it would facilitate a deeper consideration of the ethical and moral issues surrounding clinical uses of germline editing from people with diverse perspectives. So far, there is no sign of resolution. It is a debate that requires the wider participation of society at large, especially families affected by genetic conditions. It is also unclear how a global moratorium would be enforced. China had regulations on gene editing that amounted to a national moratorium, but they clearly didn’t work.
Whether or not a moratorium receives more widespread support, several things need to be done to ensure that germline gene-editing studies, done for the purposes of research only, are on a safe and sensible path. As a starting point, proposals for all ethically vetted and approved basic research studies that use gene-editing tools in human embryos and gametes, including those aimed at assessing efficacy and safety, should be deposited in an open registry.
Second, researchers need to develop a system that allows early recognition of any research that risks overstepping predefined boundaries. A useful model to follow could be the WHO guidance for regulating research with a potential biosecurity risk. The system should include a mechanism — perhaps affiliated with the open registry — that allows researchers to flag up potentially dangerous research. Analysing whether He’s work could have been prevented will help. It’s important to hammer out whether, how and to whom scientists and ethicists who became aware of the project could have voiced their concerns — and how they could do so more easily in future. Raising the alarm would require a change of practice for researchers who, for the sake of scientific independence, often do not intervene in the choice of research projects undertaken by their peers.
Unfortunately, there will always be countries with relatively lax legal frameworks that could be exploited by would-be mavericks, so global efforts should also be aimed at developing and integrating legal strategies for the prevention and penalization of unacceptable research.
A global framework could be inspired by the UK Human Fertilisation and Embryology Authority, an independent regulator of research involving human embryos and gametes. Researchers could present to such a body proposals designed to assess the safety and feasibility of a particular genetic modification in embryos, as well as justification for the work. To be allowed to proceed, researchers could be asked to adhere to a set of principles by signing a code of conduct. Research institutions and funders, meanwhile, should define and monitor clear protocols for germline genome-editing research. Institutes must take responsibility for carefully reviewing any such studies at their inception and regularly along the way.
Journals need to agree to properly documented minimum standards for ethical conduct and reporting, to which submitted research should be held. Nature Research journals, like many others, seek ethical advice alongside scientific review when considering sensitive categories of human embryo research (see Nature 557, 6; 2018).
Stakeholders must act now to reach a consensus, and the WHO is well placed to take the lead. In a welcome move, scientific academies around the world have now stated their intention to lead a commission on the scientific and ethical issues of germline gene editing.
One small contribution Nature can make is to air debate and encourage more of it. In this spirit, we welcome readers’ views (see go.nature.com/correspondence). Could the clinical use of germline gene-editing tools one day be justifiable? If so, under what framework should this come about?
We would particularly like to hear from those whose voices have been somewhat sidelined so far. This includes patient groups and those with valuable experience in working with human embryos, embryonic stem cells and germ cells, as well as experience with related research and regulations, such as the governance of innovation, disability rights, citizen-engagement methodologies and the history and philosophy of science and dual-use technologies. The right decisions on human germline modification can be reached only through frank and open discussion, followed by swift action. With so much at stake, that must happen now.

 Adopt a moratorium on heritable genome editing
Adopt a moratorium on heritable genome editing
 The CRISPR-baby scandal: what’s next for human gene-editing
The CRISPR-baby scandal: what’s next for human gene-editing
 Genome-edited baby claim provokes international outcry
Genome-edited baby claim provokes international outcry







