Abstract
Background:
Cytotoxic chemotherapy remains the main systemic therapy for gastro-oesophageal adenocarcinoma, but resistance to chemotherapy is common, resulting in ineffective and often toxic treatment for patients. Predictive biomarkers for chemotherapy response would increase the probability of successful therapy, but none are currently recommended for clinical use. We used global gene expression profiling of tumour biopsies to identify novel predictive biomarkers for cytotoxic chemotherapy.
Methods:
Tumour biopsies from patients (n=14) with TNM stage IB–IV gastro-oesophageal adenocarcinomas receiving platinum-based combination chemotherapy were used as a discovery cohort and profiled with Affymetrix ST1.0 Exon Genechips. An independent cohort of patients (n=154) treated with surgery with or without neoadjuvant platinum combination chemotherapy and gastric adenocarcinoma cell lines (n=22) were used for qualification of gene expression profiling results by immunohistochemistry. A cisplatin-resistant gastric cancer cell line, AGS Cis5, and the oesophageal adenocarcinoma cell line, OE33, were used for in vitro validation investigations.
Results:
We identified 520 genes with differential expression (Mann–Whitney U, P<0.020) between radiological responding and nonresponding patients. Gene enrichment analysis (DAVID v6.7) was used on this list of 520 genes to identify pathways associated with response and identified the adipocytokine signalling pathway, with higher leptin mRNA associated with lack of radiological response (P=0.011). Similarly, in the independent cohort (n=154), higher leptin protein expression by immunohistochemistry in the tumour cells was associated with lack of histopathological response (P=0.007). Higher leptin protein expression by immunohistochemistry was also associated with improved survival in the absence of neoadjuvant chemotherapy, and patients with low leptin protein-expressing tumours had improved survival when treated by neoadjuvant chemotherapy (P for interaction=0.038). In the gastric adenocarcinoma cell lines, higher leptin protein expression was associated with resistance to cisplatin (P=0.008), but not to oxaliplatin (P=0.988) or 5fluorouracil (P=0.636). The leptin receptor antagonist SHLA increased the sensitivity of AGS Cis5 and OE33 cell lines to cisplatin.
Conclusions:
In gastro-oesophageal adenocarcinomas, tumour leptin expression is associated with chemoresistance but a better therapy-independent prognosis. Tumour leptin expression determined by immunohistochemistry has potential utility as a predictive marker of resistance to cytotoxic chemotherapy, and a prognostic marker independent of therapy in gastro-oesophageal adenocarcinoma. Leptin antagonists have been developed for clinical use and leptin and its associated pathways may also provide much needed novel therapeutic targets for gastro-oesophageal adenocarcinoma.
Similar content being viewed by others
Main
The incidence of adenocarcinomas of the oesophagus and gastro-oesophageal junction has risen sharply in Western countries in recent decades (Edgren et al, 2012). The majority present with late stage, incurable disease or relapse after initial curative treatment. The current 1-year and 5-year survival is 40–50% and 10–15%, respectively (Kunz et al, 2012). The rising incidence and poor clinical outcomes with current therapeutic approaches not only indicate the urgent clinical need for new improved treatment regimens, but also a need for the optimised use of currently available therapeutic modalities to avoid the use of ineffective and potentially toxic treatments.
The addition of trastuzumab to cisplatin and 5fluorouracil (5FU) has been shown to be an effective palliative approach in patients with advanced gastro-oesophageal adenocarcinoma that are HER2 positive (Bang et al, 2010). Progress with targeted therapies has otherwise been limited (Ohtsu et al, 2011; Lordick et al, 2013; Waddell et al, 2013). As only 10–15% of patients have HER2-positive cancers, there is currently no targeted therapy option available for the majority of patients in whom conventional cytotoxic chemotherapy remains the only systemic option. Combination chemotherapy is effective in both early-stage and advanced-stage disease. In early-stage disease, neoadjuvant chemotherapy with cisplatin and 5FU, or perioperative chemotherapy (neoadjuvant and adjuvant) with epirubicin, cisplatin and 5FU, has proven to be effective (Cunningham et al, 2006). In advanced disease, combination chemotherapy with cisplatin or oxaliplatin together with 5FU or capectiabine has palliative benefits (Cunningham et al, 2008). The addition of epirubicin or docetaxel as triplet regimens may provide small additional benefits (Cunningham et al, 2008; Pozzo and Barone, 2008). However, only those patients who respond to chemotherapy benefit from it. Although patients who respond clinically, radiologically or histopathologically to neoadjuvant chemotherapy have an improved survival, the survival for those who do not respond is not significantly different to those treated with surgery alone (Kelsen et al, 2007). Similarly, in advanced disease, objective response rates to chemotherapy are 30–60%, and there is a significant relationship between radiological response and survival (Ichikawa and Sasaki, 2006). The delivery of ineffective chemotherapy treatment in this palliative setting can be catastrophic, as treatment-related toxicity has a significant negative impact on the quality of life of patients and because disease progression and associated deconditioning means that only a minority of patients are suitable for second-line chemotherapy. The importance of optimising the delivery of effective chemotherapy and the avoidance of ineffective chemotherapy in patients with both early- and advanced-stage gastro-oesophageal cancer is accordingly emphasised.
To address these clinical concerns, a small number of recent studies have utilised or advocated biomarker stratified treatment selection in patients with gastro-oesophageal cancer (Ferry et al, 2007; Bang et al, 2010; Ohtsu et al, 2011; Petty, 2012). Molecular biomarkers assayed in tumour pretreatment (usually diagnostic) endoscopic biopsies have been demonstrated to be of value for prediction of response to both cytotoxic and targeted therapies in a number of human cancers including gastro-oesophageal adenocarcinomas (Bang et al, 2010; Sun et al, 2011). However, with the exception of HER2 for trastuzumab, no other biomarker is currently used in routine clinical practice in patients with gastro-oesophageal adenocarcinoma, and specifically none for the prediction of response to cytotoxic chemotherapy. The discovery of predictive biomarkers that allow patient treatment stratification for chemotherapy with sufficient sensitivity and specificity would be very advantageous. These biomarkers could also provide new therapeutic targets that might effectively be combined with chemotherapy.
Because of the absence of qualified biomarkers for chemotherapy response in gastro-oesophageal adenocarcinoma, we decided to use gene expression profiling to discover novel predictive biomarkers. Our experimental design involved the initial analysis of gene expression profiling data derived from 14 patients in order to identify genes that were differentially expressed in radiological responders and nonresponders. Subsequently, we used gene enrichment analysis to identify potential candidate predictive biomarkers. Leptin, an adipocytokine, was one of the identified candidate biomarkers and was selected for further validation as the most biologically and clinically plausible predictive biomarker in this cohort. The relationship between leptin expression, histopathological response to chemotherapy and survival was investigated in an independent set of gastro-oesophageal adenocarcinomas using a tissue microarray. Leptin expression was also investigated in a panel of gastric adenocarcinoma cell lines to assess the relationship between leptin expression and resistance to cisplatin, oxaliplatin and 5FU, and the effect of a leptin receptor antagonist on chemosensitivity in cell lines was investigated.
Materials and methods
Patients and treatment
The study was approved by the North of Scotland Research Ethics Committee. Eligible patients had histologically proven clinical TNM (7th edition) stage IB–IV (staged with endoscopic ultrasound, CT scan chest, abdomen and pelvis and FDG PET CT scan) distal oesophageal or gastro-oesophageal junction adenocarcinomas, with measurable disease on CT and were deemed suitable for treatment with either preoperative/neoadjuvant or palliative chemotherapy following multidisciplinary review at Aberdeen Royal Infirmary, Aberdeen, UK. Neoadjuvant chemotherapy comprised treatment with three cycles of epirubicin, cisplatin and capecitabine, and palliative treatment comprised up to eight cycles of epirubicin, oxaliplatin and capecitabine (regimen details provided in Supplementary Information 1). Radiological response was assessed by computer tomography (CT) of the chest and abdomen before therapy and after three (neoadjuvant) or four (palliative) cycles of chemotherapy according to RECIST criteria v1.1. Within the current study, stable disease and progressive disease according to RECIST were classified as radiological ‘nonresponders’ and partial and complete response as ‘responders’.
Fourteen patients were recruited to the discovery set between January 2009 and April 2010 (for patient details see Table 1). Of the 14 patients, 10 were classified as responders and 4 as nonresponders.
Gene expression profiling data were qualified in an independent set of 154 gastro-oesophageal adenocarcinoma patients. Of these, 64 were treated with perioperative chemotherapy with 3 cycles of epirubicin, cisplatin and capecitabine before surgery and 3 cycles after surgery and 90 patients were treated by surgery alone at Aberdeen Royal Infirmary, Aberdeen, UK, between 2004 and 2009 (TNM (6th edition) was used; for patient details see Table 2 and for treatment details see Supplementary Information 1). Histopathology of the resected specimens was reported by a specialist gastrointestinal pathologist (GIM) according to the Royal College of Pathologists, London, data set. Tumour regression after neoadjuvant therapy was graded according to Mandard tumour regression grade (TRG) and 3 out of 65 were TRG1, 5 out of 64 were TRG2, 12 out of 64 were TRG3, 24 out of 64 were TRG4 and 20 out of 64 were TRG5. TRG1–3 were classified as histopathological responders and TRG4–5 histopathological nonresponders (Mandard et al, 1994). Tissue microarrays (TMAs) were constructed as described previously with duplicate cores of tumour taken for each case (Hope and Murray, 2011).
Biospecimens
A fresh specimen from the tumour was collected endoscopically before starting chemotherapy (<5 days) and placed immediately into RNALater (Life Technologies, Carlsbad, CA, USA), washed in ice-cold RNAase free water for 5 min and ‘snap’ frozen in liquid nitrogen and stored at −80 C within 24 h.
Cell lines
AGS, KatoIII, NCI-N87 and Hs746T were obtained from American Type Culture Collection (http://www.atcc.org/; Manassas, VA, USA) and cultured as recommended by the supplier. The OE33 was obtained from the European Collection of Animal and Cell Culture (Centre for Applied Microbiology and Research, Salisbury, UK, and cultured as recommended by the supplier). The AZ521, Fu97, IM95, Ist1, MKN1, MKN45, MKN7, MKN28, MKN45 and TMK1 cells were obtained from the Japanese Collection of Research Bioresources/Japan Health Science Research Resource Bank (http://cellbank.nibio.go.jp/) and cultured as recommended. The SCH cells were a gift from Yoshiaki Ito (Institute of Molecular and Cell Biology, Singapore) and grown in RPMI media. The YCC1, YCC3, YCC6, YCC7, YCC10, YCC11 and YCC16 cells were a gift from Sun-Young Rha (Yonsei Cancer Center, Seoul, South Korea) and were grown in minimum essential medium supplemented with 10% fetal bovine serum, 100 U ml−1 penicillin, 100 U ml−1 streptomycin and 2 mmol l−1 L-glutamine (Invitrogen, Carlsbad, CA, USA). Cell lines were harvested and fixed in 4% paraformaldehyde, cell pellets were prepared from individual cell lines and further processed for paraffin embedding as described previously (Waterworth et al, 2005). Generation of a cisplatin-resistant gastric cancer cell line from AGS cells is described in Supplementary Information 5.
In vitro cell proliferation assay
Adherent or semi-adherent cell lines with doubling times <48 h were used in this analysis. Cells were seeded in 100 μl of media in a 96-well plate and left to adhere for 24 h, then 100 μl of drug diluted in media added at appropriate concentrations and then incubated for 72 h at 37 °C and 5% CO2. Complete media alone (no cells) served as a background control. Blank and vehicle controls were included on each plate and then cell proliferation assay performed. Cell proliferation assays were performed using a tetrazolium compound-based colorimetric method (MTS kit; Promega, Madison, WI, USA) according to the manufacturer’s instructions and measured using an EnVision 2104 multilabel plate reader (Perkin Elmer, Turku, Finland) at 490 nm and a dose curve was fitted and IC50 values representing the drug concentration required to elicit a 50% growth inhibition calculated in Prism software (GraphPad PRISM v.5.02, La Jolla, CA, USA). Inhibition of cell growth due to drug treatment was also confirmed microscopically. Drugs used were cisplatin (479306-1G; Sigma, St Louis, MO, USA), oxaliplatin (O9512; Sigma) and 5FU (F6627-1G; Sigma). For each drug treatment, a minimum of three independent replicate experiments with three intra-assay replicates per data point were performed. The IC50 data for cisplatin, oxaliplatin and 5FU for each cell line are provided in Supplementary Information 6.
Leptin receptor antagonist experiments
The highly specific and highly potent leptin receptor antagonist, superactive human leptin antagonist (SHLA; Shpilman et al, 2011), was obtained from Protein Laboratories Rehovot Ltd (PLR, Rehovot, Israel). The AGS Cis5 or OE33 cells were seeded on to a 96-well plate in 100 μl media and allowed to attach for 24 h, and then serum starved for 24 h. Subsequently, 100 μl of cisplatin diluted in media and/or SHLA was added at the indicated concentrations, and cells were incubated for 72 h at 37 °C and 5% CO2. Complete media alone (no cells) served as a background control. Blank and vehicle controls for cisplatin and SHLA when either was added alone were included on each plate. Following the incubation period, MTT assay (Sigma-Aldrich, Gillingham, UK) was performed according to the manufacturer’s instructions and as described above. Results presented are from experiments performed in triplicate, repeated 4 times.
Gene expression profiling
After histopathological confirmation, gene expression was assessed in fresh tumour specimens using the Affymetrix Exon 1.0 ST Array (1 084 639 exons and over 300 000 transcript clusters on each oligonucleotide microarray; www.affymetrix.com). Details of RNA extraction, sample preparation and quality control are described in Supplementary Information 2.
Analysis of gene expression data
Gene expression data was analysed using Genespring v.11.1 (Agilent, Wokingham, UK) and DAVID v6.7 (NIH, Bethesda, MD, USA) (Huang et al, 2009) for pathway analysis (described in Results and Supplementary Information as indicated). Core probe sets on the Human Exon 1.0 ST array were processed using the RMA16 algorithm (Affymetrix, Santa Clara, CA, USA) that employs quantile normalisation of log2 transformed data. Data were transformed to median of all samples. Expression above background was defined as all entities with signal intensities ⩾20th percentile of all intensity values in at least one sample. Gene expression data and experimental details are available in MIAME compliant format in ArrayExpress (http://www.ebi.ac.uk/arrayexpress/) accession number E-MEXP-3730.
Immunohistochemistry (IHC)
Sections were cut from the tissue microarrays and the cell line paraffin blocks. After dewaxing according to a standard protocol, antigen retrieval was performed by microwaving in 10 mmol l−1 citrate (pH, 6.0) for 20 min. Leptin mouse monoclonal antibody (Y-20, Santa Cruz Biotechnology, Santa Cruz, CA, USA) was diluted 1 : 400 for TMA sections and 1 : 1200 for cell line sections. Immunohistochemistry was performed using an autostainer (Dakocytomation, Glostrup, Denmark) incubating the sections with the primary antibody for 1 h at room temperature and using the Envision (Dakocytomation) detection system according to the manufacturer’s instructions and as previously described (Duncan et al, 2008). Tissue and cell line positive and negative controls without primary antibody were used. All sections were double scored by two independent investigators who were blinded to the clinical and chemosensitivity data. Leptin expression was scored in tumour cells as negative, weak, moderate or strong based on the intensity of cytosolic staining irrespective of the number of positive cells. Overall, 92% agreement in scoring was observed (κ-statistic=0.87). Scoring discrepancies were resolved by examination of relevant sections jointly.
Statistical analyses
All other statistical analyses including survival analysis were performed using PASW statistics v20 (IBM Corporation, Armonk, NY, USA). Kaplan–Meier and Cox proportional hazards analysis were used for survival analysis and survival time was calculated in days from date of histological diagnosis until date of death. Fisher’s exact test was used for the assessment of categorical variables. All reported P-values are two sided. A P-value of <0.05 was considered statistically significant.
Results
Gene expression profiling identified the adipocytokine signalling pathway as differentially expressed between chemotherapy responders and nonresponders
We used a discovery set (n=14 patients, for clinicopathological data see Table 1) to identify genes whose expression was significantly different between radiological responders and nonresponders, resulting in a list of 520 genes (Mann–Whitney U, P<0.020, 520 genes listed in Supplementary Information 3). In order to investigate potential mechanisms of response and identify potential predictive biomarkers and potential therapeutic targets for further qualification, gene enrichment analysis (DAVID, v6.7 (Huang et al, 2009)) was used to identify ‘over represented’ pathways in the list of 520 genes. This analysis revealed six pathways as shown in Table 3 including the adipocytokine pathway. Genes from this particular pathway include leptin that was increased in nonresponding tumours (Figure 1 and Table 4). Clinical and preclinical data support the involvement of adipocytokine signalling in gastro-oesophageal adenocarcinoma pathogenesis. Epidemiological studies demonstrate a strong relationship between body mass index (BMI), measures of visceral adiposity and risk of oesophageal and gastro-oesophageal junctional adenocarcinoma and leptin receptor is expressed in the majority of gastro-oesophageal adenocarcinomas (Abnet et al, 2008; Howard et al, 2010). Leptin has been shown to stimulate proliferation and inhibit cell death in gastric and oesophageal adenocarcinoma cells (Pai et al, 2005; Shida et al, 2005; Ogunwobi et al, 2006; Beales and Ogunwobi, 2007; Abnet et al, 2008; Howard et al, 2010; Dong et al, 2013). Therefore the involvement of the adipocytokine pathway in the response of gastro-oesophageal adenocarcinomas to chemotherapy is plausible biologically and clinically. For these reasons leptin was selected for further investigation. We hypothesised that high leptin expression in gastro-oesophageal adenocarcinomas is associated with resistance and lack of response to chemotherapy.
Qualification of predictive and prognostic impact of leptin in an independent clinical reference set
To provide further evidence to support the potential utility of tumour leptin expression as a predictive biomarker for chemotherapy response, the relationship between leptin tumour protein expression in gastro-oesophageal adenocarcinoma and response to treatment and survival was investigated using IHC in an independent set of 154 resected gastro-oesophageal adenocarcinomas, 64 of which received neoadjuvant chemotherapy (for clinicopathological details see Table 2, and treatment details see Supplementary Information 1). Cytoplasmic leptin expression was seen in 92% of cases and, when present, was invariably present in the majority of tumour cells, with little observed variation in the proportion of tumour cells staining positive for leptin. However, clear variation in the intensity of leptin IHC staining was observed, and classified as strong, moderate or weak (Figure 2A). This scoring system was therefore based upon the observed biological variability for leptin IHC staining in gastro-oesophageal adenocarcinomas. Gastric and junctional (Siewert type III) adenocarcinomas were more likely to be strongly leptin positive (P=0.0001, defined as strong vs weak/moderate/negative), but otherwise there was no association between leptin expression level and any of the clinicopathological variables (gender, T stage, N stage, stage grouping; see Supplementary Information 4). There was a highly significant relationship between strong leptin expression and lack of histopathological response to neoadjuvant chemotherapy (P=0.007, Figure 2B), consistent with the results from gene expression profiling in the discovery set.
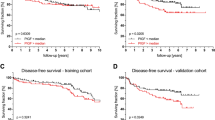
Leptin IHC in gastro-oesophageal adenocarcinomas. (A) Representative IHC (weak and medium × 200; strong × 400). (B) Leptin IHC and histopathological response to neoadjuvant platinum-based combination chemotherapy (χ2, P=0.007). Mandard TRG 4–5 have a medium survival of 23.8 months and Mandard TRG 1–3 median survival not reached but >72 months (Kaplan–Meier analysis, log rank P=0.009, data not shown) in this series and survival of Mandard TRG 4–5 is not different to those who had surgery only and no neoadjuvant chemotherapy in this cohort (median survival=34.4 months, Kaplan–Meier log rank P=0.757, data not shown). (C) Leptin IHC and overall survival (Kaplan–Meier analysis, log rank P=0.021). (D) Leptin IHC and survival stratified by neoadjuvant chemotherapy (P for interaction=0.038). Leptin positive=leptin IHC strong; leptin negative=leptin IHC negative, weak or moderate.
Strong leptin expression was also associated with better survival in this cohort (P=0.021, Figure 2C). This appeared to be inconsistent with our observations that leptin expression is associated with chemoresistance. To address this issue, we investigated the interaction between leptin expression, survival and whether or not patients had received neoadjuvant chemotherapy. This analysis revealed that patients with tumours with strong leptin expression have better survival, but in this group there appears to be no impact of neoadjuvant chemotherapy on survival. In contrast, for patients with leptin moderate/weak/negative tumours, survival is improved in those patients who received neoadjuvant chemotherapy (Figure 2D, P for interaction=0.038). In multivariate analysis in the entire cohort (n=154), leptin is significantly associated with survival (Table 5). Overall, this suggests that leptin expression is associated with chemoresistance, consistent with the observed associations in our gene expression profiling experiments, but also that leptin expression in gastro-oesophageal adenocarcinomas has a therapy-independent prognostic impact as well.
Leptin staining in stromal cells was observed in 50% of tumours. There was no significant correlation between leptin staining in the stroma and leptin tumour cell staining, nor with histopathological response or survival.
Leptin expression in gastric adenocarcinoma cell lines correlates with chemoresistance
To extend our findings from patient samples to an in vitro system, and examine the effects of leptin on chemosensitivity to individual cytotoxic drugs, we examined the expression of leptin by IHC in a panel of gastric cancer cell lines (n=22). Similar to the scoring performed in primary cancers, leptin expression was categorised as negative, weak, moderate or strong based upon the intensity of cytoplasmic staining, with negative=0 out of 22, weak=5 out of 22, moderate=11 out of 22 and strong=6 out of 22 cell lines. Strong leptin protein expression was significantly associated with lower in vitro sensitivity to cisplatin in these cell lines (mean GI50 concentration 86.8 μ M l−1 vs 16.8 μ M l−1, P=0.008, Figure 3). There was no significant relationship between leptin expression and in vitro sensitivity to oxaliplatin (P=0.988) or 5FU (P=0.636) (Figure 3). These results support the potential role of leptin expression in resistance to cytotoxic chemotherapy and suggest that the impact of leptin expression may be agent specific.
Leptin IHC and in vitro chemosensitivity to ( A ) cisplatin, ( B ) oxaliplatin and ( C ) 5FU in gastric adenocarcinoma cell panel ( n =22 cell lines). Figures show mean IC50 (drug concentration for 50% growth inhibition) performed in triplicate and a minimum of three replicates, P-values, Student’s t-test and error bars±s.e.m. Representative examples of (C) weak, (D) moderate and (F) strong leptin IHC staining in cell lines. Magnification × 100 in all cases. Effects of leptin receptor antagonist on cisplatin sensitivity of (G) a highly cisplatin-resistant gastric adenocarcinoma cell line AGS Cis5, IC50=16 μ M, cisplatin=8 μ M, SHLA=0.32 ng ml−1, and (H) oesophageal adenocarcinoma cell line OE33, IC50=1.5 μ M, cisplatin=0.5 μ M, SHLA=0.64 ng ml−1. (G and H) Mean growth from four independent experiments repeated in triplicate, relative cell survival (%)=(MTT OD value for cells only/MTT OD value for cells+treatment as indicated) × 100, with P-values for ANOVA with Tukey’s post hoc test shown where significant (P<0.05), and error bars±s.e.m.
Leptin receptor antagonist SHLA increases sensitivity to cisplatin
In order to provide mechanistic evidence for the role of leptin in response to cisplatin in gastroesophageal adenocarcinoma, and to investigate the importance of autocrine/paracrine leptin signalling in cisplatin response, we examined the effect of the leptin receptor antagonist SHLA (Shpilman et al, 2011) on in vitro sensitivity to cisplatin. Experiments were performed using two cell lines that were not part of the previous panel: an oesophageal adenocarcinoma cell line OE33 and a gastric cancer cell line AGS Cis5 that had been selected for acquired resistance to cisplatin (Supplementary Information 5). In both OE33 and AGS Cis5, SHLA increased sensitivity to cisplatin (Figure 3). In addition, SHLA inhibited the growth of OE33 cells when given alone, but not AGSCis5 (Figure 3). In both AGS Cis5 and OE33, SHLA inhibited leptin-induced cell proliferation (Supplementary Information 7).
Discussion
We performed gene expression profiling to identify potential predictive biomarkers of chemotherapy response in patients with gastro-oesophageal adenocarcinoma. Higher leptin mRNA expression was associated with lack of radiological response. Subsequently, we demonstrated that higher leptin protein expression was associated with lack of histological response to neoadjuvant chemotherapy in an independent cohort of patients, and with resistance to cisplatin in a panel of gastric adenocarcinoma cell lines. Patients with lower leptin tumour expression had better survival when treated with neoadjuvant chemotherapy, whereas those with higher leptin expression did not have a survival benefit from neoadjuvant chemotherapy. Finally, we demonstrated that a leptin receptor antagonist increased sensitivity to cisplatin, including in a highly cisplatin-resistant cell line. The strong association of leptin mRNA and protein expression with both radiological and histopathological response, and also patient survival and in vitro cisplatin sensitivity, together with increased cisplatin sensitivity by a leptin receptor antagonist, provides consistent evidence of the importance of leptin in gastro-oesophageal cancer pathogenesis and response to chemotherapy.
Leptin is an adipocytokine that is secreted from adipocytes as well as other cells, and it acts through specific receptors to control satiety in the central nervous system, and in peripheral tissues to regulate glucose and insulin homeostasis and other functions such as angiogenesis (Bjorbaek and Kahn, 2004). The increased risk of cancer in obese individuals and the deregulation of adipocytokines in obesity has led to investigation of leptin signalling in cancer pathogenesis (VanSaun, 2013). Leptin secretion has been demonstrated from breast cancer and glioblastoma cells, and autocrine or paracrine actions appear to be important in carcinogenesis (Miyoshi et al, 2006; Ferla et al, 2011; Nejati-Koshki et al, 2012). Epidemiological studies demonstrate a strong relationship between BMI, visceral adipose tissue and risk of oesophageal and gastro-oesophageal junction adenocarcinoma (Abnet et al, 2008). In addition, there are several lines of evidence supporting a role for leptin in the pathogenesis of gastro-oesophageal adenocarcinoma, including clinical and preclinical data implicating leptin as a growth-promoting signal, stimulating proliferation and inhibiting cell death of gastric and oesophageal adenocarcinoma cells (Pai et al, 2005; Shida et al, 2005; Ogunwobi et al, 2006; Beales and Ogunwobi, 2007; Abnet et al, 2008; Howard et al, 2010; Dong et al, 2013). Leptin receptors have been shown to be expressed in the majority of gastroesophageal adenocarcinomas (Howard et al, 2010). Accordingly, based on our results we hypothesise that leptin acts via an autocrine or paracrine mechanism involving its specific receptor(s) in gastro-oesophageal adenocarcinoma tumour cells, promoting cell survival and hence chemoresistance in the presence of a cytotoxic drug insult.
We observed no significant correlation between BMI and leptin tumour expression (R=0.006, P=0.983) or between BMI and response to chemotherapy (nonresponders=31.4 vs responders=28.5, P=0.293). Our study was not adequately powered or intended to address the question of whether tumour leptin concentration correlates with BMI. A larger study would be required to fully investigate any relationship between tumour leptin and BMI. In light of our findings implicating tumour leptin expression in resistance to therapy, an investigation of the relationship between tumour leptin expression, serum leptin concentration, BMI, visceral adiposity and therapy outcome would be valuable to provide new insights into gastro-oesophageal cancer pathogenesis.
Interestingly, higher leptin protein expression was also associated with improved survival in the absence of neoadjuvant chemotherapy, implying contrasting predictive and therapy-independent prognostic impacts. Similar associations between leptin expression and improved therapy independent prognosis have been reported in colorectal and breast cancer (Kim, 2009; Paik et al, 2009). Similar contrasting relationships between response to treatment and prognosis have been observed for other markers, most notably for oestrogen receptors (ER) in breast cancer, where ER expression correlates with not only chemoresistance but also better survival, and is also a useful therapeutic target (Petit et al, 2010). In addition, recently in triple-negative breast cancer, high BCL2 expression by IHC was noted to be associated with a lack of benefit from adjuvant anthracycline-based chemotherapy but a better therapy-independent prognosis (Abdel-Fatah et al, 2013). This is similar to our findings in gastro-oesophageal cancer of high leptin leading to specific chemotherapy resistance but better overall prognosis. These findings suggest that clinically relevant molecular mechanisms exist that lead to resistance to chemotherapy but a better therapy-independent prognosis (and the converse of worse therapy-independent prognosis that is improved by sensitivity to chemotherapy). We believe characterisation of such mechanisms is important as they allow the discovery of clinically very useful biomarkers that identify chemotherapy regimens that will be ineffective, but whose occurrence are associated with a better prognosis subset of patients in whom other targets might be more optimally pursued.
The predictive and prognostic impact of leptin tumour expression demonstrated in the current study suggests that it has potential utility as a biomarker. High tumour leptin expression would identify a tumour that is chemoresistant, but has a good therapy-independent prognosis, whereas low tumour leptin expression would identify a tumour with a poor therapy-independent prognosis that is chemosensitive, implying that chemotherapy is likely to improve outcome in patients with low tumour leptin expression. In the 64 patients who received neoadjuvant chemotherapy before surgery, 0 out of 32 patients in the strong leptin expression group had major histopathological responses (Mandard TRG 1 or 2). All major histological responses occurred in the negative/weak/moderate leptin expression group. Therefore, although tumours with strong leptin protein expression are unlikely to respond to and hence benefit from neoadjuvant chemotherapy, some clinicians might believe that even a low probability of a minor response (12% chance of moderate – Mandard TRG3 – response in leptin high protein expression in our series) would justify the administration of neoadjuvant chemotherapy. However, strong leptin-positive patients have a good therapy-independent prognosis – the estimated 5-year survival in our series is 50% in strong leptin expression patients who did not have neoadjuvant chemotherapy – that is not significantly different from leptin-positive patients who were given neoadjuvant chemotherapy (estimated 5-year survival 52%).
To confirm the predictive and prognostic impact of tumour leptin expression, a prospective investigation of leptin expression in tumours from a randomised study would need to be undertaken. This could be performed as a ‘prospective-retrospective’ analysis using available tissue collections from neoadjuvant chemotherapy trials where randomisation to chemotherapy and surgery or surgery alone was undertaken. The development and technical validation of an IHC assay for leptin in our study means that this is feasible and the magnitude of the effect of leptin that we have observed suggests that tissue collections available from such trials would be adequately powered. Ultimately, further technical validation and optimisation would be required to produce a robust leptin IHC assay for routine clinical application. Our gene expression profiling discovery set also included patients with advanced disease who received palliative chemotherapy and hence leptin may also be useful as a predictive biomarker for palliative chemotherapy in advanced disease. This role of leptin would also require prospective qualification. In a prospective qualification study, it would also be important to determine whether the effect of leptin on chemosensitivity is specific to certain chemotherapy drugs, as is perhaps suggested by the data from our gastric cancer cell line panel, or a more general effect.
In the discovery set, all 4 nonresponders and 6 out of 10 responders received ECX (Table 1). In light of our cell line findings, the inclusion of patients not treated with cisplatin, but instead with oxaliplatin, may have affected the results from the original discovery cohort. However, if, as the cell line studies suggest, leptin is associated with resistance to cisplatin and not oxaliplatin, treatment with oxaliplatin and not cisplatin in the responding group would have potentially diluted any relationship between leptin and resistance. Therefore, we do not believe that the inclusion of patients not treated with cisplatin has critically influenced the study outcome; in addition, the impact of leptin on chemosensitivity and clinical outcome for neoadjuvant ECX chemotherapy has been validated. In the absence of any qualified biomarkers for chemotherapy response in gastro-oesophageal adenocarcinoma, a discovery approach using gene expression profiling to identify leads for novel predictive biomarkers is justified, and the analysis of tumour specimens from patients treated with chemotherapy represents the most clinically relevant translational experimental model. However, adopting this approach means that patients receive combination regimens as this is standard clinical practice, and necessitates further investigation to determine the effects of any leads on individual drugs (as we have undertaken for leptin), because for clinical application it is important to determine the effect of markers on individual drugs. However, the approach also has the significant advantage of capturing data from clinical response involving the majority of the drugs commonly used in the advanced and neoadjuvant settings for gastro-oesophageal adenocarcinomas, and hence provides the opportunity to identify molecules that may be involved in response or resistance to multiple agents that are hence potentially of great value as predictive biomarkers or targets. Overall, our experimental approach in the discovery set provided the greatest opportunity to identify leads from gene expression profiling that would have clinical and translational relevance, but required that leads would need to be validated in specific cohorts of patients and in vitro model systems – as we have undertaken.
The discordant effects of leptin on resistance to cisplatin and oxaliplatin observed in our gastric cancer cell line panel are interesting and of potential value for the use of leptin as a predictive biomarker. A randomised trial has demonstrated that oxaliplatin is equivalent to cisplatin in the treatment of advanced gastro-oesophageal adenocarcinoma (Cunningham et al, 2008). However, although related, there are also differences in the mechanisms of action of cisplatin and oxaliplatin, and preclinical investigation in gastric cancer suggests that there are distinct subsets that exhibit differential sensitivity to oxaliplatin and cisplatin. Gene expression profiling of gastric cancer cell lines (validated in primary gastric cancer tumour specimens) identified two subsets with differential sensitivity to oxaliplatin and cisplatin (Tan et al, 2011). In addition, molecular determinants of resistance to cisplatin have been demonstrated in gastric cancer that do not affect oxaliplatin sensitivity (Ivanova et al, 2013). In our gastric adenocarcinoma cell line panel, there is no correlation between IC50 for cisplatin and oxaliplatin (R=−0.078, P=0.730) or between IC50 for cisplatin and 5FU (R=0.084, P=0.780), but oxaliplatin and 5FU GI50 do significantly correlate (R=0.0494, P=0.019 and Supplementary Information 6). These consistent observations suggest that differential sensitivity to oxaliplatin and cisplatin occurs in gastro-oesophageal cancer and implies the existence of distinct mechanisms of action and determinants of resistance and sensitivity to these two cytotoxic drugs. Our data suggest that leptin may play a similar role in mediating differential sensitivity to oxaliplatin and cisplatin in gastro-oesophageal adenocarcinomas. A differential effect on sensitivity to oxaliplatin and cisplatin would enhance the clinical utility of leptin as a clinical predictive biomarker as high leptin would imply resistance to cisplatin, but sensitivity maintained to oxaliplatin that would be a suitable alternative agent to use in such patients.
There have been conflicting results for the impact of the tumour expression of leptin on prognosis in human cancer, including gastric cancer. Methodological issues and patient case mix in series are more likely to provide explanations for these differences rather than tumour biology. Specifically, Geng et al (2012) reported leptin IHC associated with worse survival in 110 patients with resected gastric cancer; however although it is apparent that some patients have received chemotherapy, it is not reported what the chemotherapy regimen is or whether the chemotherapy was given adjuvant, neoadjuvant or on relapse. Leptin IHC expression in tumours is reported as being an independent factor in the Cox regression survival analysis that also includes ‘absence’ of chemotherapy, but the specific impact of leptin in chemotherapy-treated patients is not reported. In light of our data reporting a significant interaction between leptin tumour expression and chemotherapy response, it is difficult to interpret the clinical relevance of Geng et al data and to make valid comparisons with our own data set in which the interaction of leptin and chemotherapy has been examined. The choice of threshold between leptin IHC positive and negative has the potential to strongly influence outcome data in retrospective studies. In our series, the biological rationale for the threshold we used can be demonstrated by examination of the KM curves in Figure 2C that shows a ‘dose response’ relationship between leptin expression and survival – in this figure, the distinct survival outcome of leptin strong positive cases can be seen, whereas moderate or weak staining show no distinct difference from each other. In the paper by Geng et al, no data regarding the dose–response relationship between leptin IHC and outcome are presented and, accordingly, no rationale for the applied cutoff threshold they have used in their analysis. Zhao et al (2007) demonstrated no relationship between leptin IHC and survival after surgery for gastric cancer patients with KM survival analysis, and it is therefore surprising that leptin is subsequently reported as an independent prognostic factor in the Cox multivariate analysis. This inconsistency suggests that caution should be applied in the interpretation of these data that may reflect the balance of chance alone.
The interaction between leptin expression and response to chemotherapy and the therapy-independent prognostic impact demonstrated in our data suggests that leptin may be a useful therapeutic target in gastro-oesophageal adenocarcinoma. A number of leptin receptor antagonists have been developed for therapeutic use, including as anticancer agents, with several completing preclinical testing and they are likely to enter early-phase clinical trials soon (Otvos et al, 2011; Shpilman et al, 2011; Gertler and Solomon, 2013). We chose to examine the effect of a leptin receptor antagonist on cisplatin sensitivity in gastro-oesophageal adenocarcinoma in order to further evaluate the role of leptin signalling, particularly autocrine and paracrine signalling and, given the stage of development of leptin receptor antagonists, to evaluate the translational potential of such agents as novel therapeutics. Our data suggest that leptin receptor antagonists may be useful to administer in combination with chemotherapy, or as monotherapy – administration with chemotherapy may reverse clinical resistance and increase response rates; alternatively, high tumour leptin expression may indicate a chemoresistant tumour that is dependent upon leptin signalling and that may be more optimally treated by a leptin antagonist, avoiding chemotherapy.
In conclusion, the results presented indicate that leptin could be a useful clinical biomarker in gastro-oesophageal adenocarcinoma for chemotherapy selection and also a novel therapeutic target. We believe that further prospective biomarker qualification studies and mechanistic investigations are indicated.
Accession codes
Change history
18 March 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abdel-Fatah TMA, Perry C, Dickinson P, Ball G, Moseley P, Madhusudan S, Ellis IO, Chan SYT (2013) Bcl2 is an independent prognostic marker of triple negative breast cancer (TNBC) and predicts response to anthracycline combination (ATC) chemotherapy (CT) in adjuvant and neoadjuvant settings. Ann Oncol 24 (11): 2801–2807.
Abnet CC, Freedman ND, Hollenbeck AR, Fraumeni JF Jr., Leitzmann M, Schatzkin A (2008) A prospective study of BMI and risk of oesophageal and gastric adenocarcinoma. Eur J Cancer 44: 465–471.
Bang Y, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T, Aprile G, Kulikov E, Hill J, Lehle M, Rüschoff J, Kang Y (2010) Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet Oncol 376: 687–697.
Beales ILP, Ogunwobi OO (2007) Leptin synergistically enhances the anti-apoptotic and growth-promoting effects of acid in OE33 oesophageal adenocarcinoma cells in culture. Mol Cell Endocrinol 274: 60–68.
Bjorbaek C, Kahn BB (2004) Leptin signaling in the central nervous system and the periphery. Recent Prog Horm Res 59: 305–331.
Cunningham D, Allum W, Stenning S, Thompson J, VandeVelde CH, Nicolson M, Scarffe JH, Lofts F, Falk S, Iveson T, Smith D, Langley R, Verma M, Weeden S, Chua Y the MAGIC Trial Participants (2006) Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med 355: 11–20.
Cunningham D, Starling N, Rao S, Iveson T, Nicolson M, Coxon F, Middleton G, Daniel F, Oates J, Norman AR (2008) Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med 358: 36–46.
Dong Z, Xu X, Du L, Yang Y, Cheng H, Zhang X, Li Z, Wang L, Li J, Liu H, Qu X, Wang C (2013) Leptin-mediated regulation of MT1-MMP localization is KIF1B dependent and enhances gastric cancer cell invasion. Carcinogenesis 34: 974–983.
Duncan R, Carpenter B, main LC, Telfer C, Murray GI (2008) Characterisation and protein expression profiling of annexins in colorectal cancer. Br J Cancer 98: 426–433.
Edgren G, Adami H, Weiderpass E, Nyrén O (2012) A global assessment of the oesophageal adenocarcinoma epidemic. Gut 62 (10): 1406–1414.
Ferla R, Bonomi M, Otvos L Jr, Surmacz E (2011) Glioblastoma-derived leptin induces tube formation and growth of endothelial cells: comparison with VEGF effects. BMC Cancer 11: 303.
Ferry DR, Anderson M, Beddard K, Tomlinson S, Atherfold P, Obszynska J, Harrison R, Jankowski J (2007) A phase II study of gefitinib monotherapy in advanced esophageal adenocarcinoma: evidence of gene expression, cellular, and clinical response. Clin Cancer Res 13: 5869–5875.
Geng Y, Wang J, Wang R, Wang K, Xu Y, Song G, Wu C, Yin Y (2012) Leptin and HER-2 are associated with gastric cancer progression and prognosis of patients. Biomed Pharmacother 66 (6): 419–424.
Gertler A, Solomon G (2013) Leptin-activity blockers: development and potential use in experimental biology and medicine. Can J Physiol Pharmacol 91: 873–882.
Hope NR, Murray GI (2011) The expression profile of RNA-binding proteins in primary and metastatic colorectal cancer: relationship of heterogeneous nuclear ribonucleoproteins with prognosis. Hum Pathol 42: 393–402.
Howard JM, Beddy P, Ennis D, Keogan M, Pidgeon GP, Reynolds JV (2010) Associations between leptin and adiponectin receptor upregulation, visceral obesity and tumour stage in oesophageal and junctional adenocarcinoma. Br J Surg 97: 1020–1027.
Huang DW, Sherman BT, Lempicki RA (2009) Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc 4: 44–53.
Ichikawa W, Sasaki Y (2006) Correlation between tumor response to first-line chemotherapy and prognosis in advanced gastric cancer patients. Ann Oncol 17: 1665–1672.
Ivanova T, Zouridis H, Wu Y, Cheng LL, Tan IB, Gopalakrishnan V, Ooi CH, Lee J, Qin L, Wu J, Lee M, Rha SY, Huang D, Liem N, Yeoh KG, Yong WP, Teh BT, Tan P (2013) Integrated epigenomics identifies BMP4 as a modulator of cisplatin sensitivity in gastric cancer. Gut 62: 22–33.
Kelsen DP, Winter KA, Gunderson LL, Mortimer J, Estes NC, Haller DG, Ajani JA, Kocha W, Minsky BD, Roth JA, Willett CG (2007) Long-term results of RTOG trial 8911 (USA Intergroup 113): a random assignment trial comparison of chemotherapy followed by surgery compared with surgery alone for esophageal cancer. J Clin Oncol 25: 3719–3725.
Kim HS (2009) Leptin and leptin receptor expression in breast cancer. Cancer Res Treat 41: 155–163.
Kunz PL, Gubens M, Fisher GA, Ford JM, Lichtensztajn DY, Clarke CA (2012) Long-term survivors of gastric cancer: a California population-based study. J Clin Oncol 30: 3507–3515.
Lordick F, Kang Y, Chung H, Salman P, Oh SC, Bodoky G, Kurteva G, Volovat C, Moiseyenko VM, Gorbunova V, Park JO, Sawaki A, Celik I, Götte H, Melezínková H, Moehler M (2013) Capecitabine and cisplatin with or without cetuximab for patients with previously untreated advanced gastric cancer (EXPAND): a randomised, open-label phase 3 trial. Lancet Oncol 14: 490–499.
Mandard A, Dalibard F, Mandard J, Marnay J, Henry-Amar M, Petiot J, Roussel A, Jacob J, Segol P, Samama G, Ollivier J, Bonvalot S, Gignoux M (1994) Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma. Clinicopathologic correlations. Cancer 73: 2680–2686.
Miyoshi Y, Funahashi T, Tanaka S, Taguchi T, Tamaki Y, Shimomura I, Noguchi S (2006) High expression of leptin receptor mRNA in breast cancer tissue predicts poor prognosis for patients with high, but not low, serum leptin levels. Int J Cancer 118: 1414–1419.
Nejati-Koshki K, Zarghami N, Pourhassan-Moghaddam M, Rahmati-Yamchi M, Mollazade M, Nasiri M, Esfahlan RJ, Barkhordari A, Tayefi-Nasrabadi H (2012) Inhibition of leptin gene expression and secretion by silibinin: possible role of estrogen receptors. Cytotechnology 64: 719–726.
Ogunwobi O, Mutungi G, Beales ILP (2006) Leptin stimulates proliferation and inhibits apoptosis in Barrett’s esophageal adenocarcinoma cells by cyclooxygenase-2-dependent, prostaglandin-E2-mediated transactivation of the epidermal growth factor receptor and c-Jun NH2-terminal kinase activation. Endocrinology 147: 4505–4516.
Ohtsu A, Shah MA, Van Cutsem E, Rha SY, Sawaki A, Park SR, Lim HY, Yamada Y, Wu J, Langer B, Starnawski M, Kang Y (2011) Bevacizumab in combination with chemotherapy as first-line therapy in advanced gastric cancer: a randomized, double-blind, placebo-controlled phase III study. J Clin Oncol 29: 3968–3976.
Otvos L Jr, Kovalszky I, Riolfi M, Ferla R, Olah J, Sztodola A, Nama K, Molino A, Piubello Q, Wade JD, Surmacz E (2011) Efficacy of a leptin receptor antagonist peptide in a mouse model of triple-negative breast cancer. Eur J Cancer 47: 1578–1584.
Pai R, Lin C, Tran T, Tarnawski A (2005) Leptin activates STAT and ERK2 pathways and induces gastric cancer cell proliferation. Biochem Biophys Res Commun 331: 984–992.
Paik SS, Jang S, Jang K, Lee KH, Choi D, Jang SJ (2009) Leptin expression correlates with favorable clinicopathologic phenotype and better prognosis in colorectal adenocarcinoma. Ann Surg Oncol 16 (2): 297–303.
Petit T, Wilt M, Velten M, Rodier J, Fricker J, Dufour P, Ghnassia J (2010) Semi-quantitative evaluation of estrogen receptor expression is a strong predictive factor of pathological complete response after anthracycline-based neo-adjuvant chemotherapy in hormonal-sensitive breast cancer. Breast Cancer Res Treat 124: 387–391.
Petty RD (2012) Exclusive rights in gastric cancer genomics. Gut 61: 638–640.
Pozzo C, Barone C (2008) Is there an optimal chemotherapy regimen for the treatment of advanced gastric cancer that will provide a platform for the introduction of new biological agents? Oncologist 13: 794–806.
Shida D, Kitayama J, Mori K, Watanabe T, Nagawa H (2005) Transactivation of epidermal growth factor receptor is involved in leptin-induced activation of janus-activated kinase 2 and extracellular signal–regulated kinase 1/2 in human gastric cancer cells. Cancer Res 65: 9159–9163.
Shpilman M, Niv-Spector L, Katz M, Varol C, Solomon G, Ayalon-Soffer M, Boder E, Halpern Z, Elinav E, Gertler A (2011) Development and characterization of high affinity leptins and leptin antagonists. J Biol Chem 286: 4429–4442.
Sun J, Han J, Ahn JS, Park K, Ahn M (2011) Significance of thymidylate synthase and thyroid transcription factor 1 expression in patients with nonsquamous non-small cell lung cancer treated with pemetrexed-based chemotherapy. J Thorac Oncol 6: 1392–1399.
Tan IB, Ivanova T, Lim KH, Ong CW, Deng N, Lee J, Tan SH, Wu J, Lee MH, Ooi CH, Rha SY, Wong WK, Boussioutas A, Yeoh KG, So J, Yong WP, Tsuburaya A, Grabsch H, Toh HC, Rozen S, Cheong JH, Noh SH, Wan WK, Ajani JA, Lee J, Salto–Tellez M, Tan P (2011) Intrinsic subtypes of gastric cancer, based on gene expression pattern, predict survival and respond differently to chemotherapy. Gastroenterology 141: 476–485.e11.
VanSaun MN (2013) Molecular pathways: adiponectin and leptin signaling in cancer. Clin Cancer Res 19: 1926–1932.
Waddell T, Chau I, Cunningham D, Gonzalez D, Frances A, Okines C, Wotherspoon A, Saffery C, Middleton G, Wadsley J, Ferry D, Mansoor W, Crosby T, Coxon F, Smith D, Waters J, Iveson T, Falk S, Slater S, Peckitt C, Barbachano Y (2013) Epirubicin, oxaliplatin, and capecitabine with or without panitumumab for patients with previously untreated advanced oesophagogastric cancer (REAL3): a randomised, open-label phase 3 trial. Lancet Oncol 14: 481–489.
Waterworth A, Hanby A, Speirs V (2005) A novel cell array technique for high-throughput, cell-based analysis. In Vitro Cell Dev Biol Anim 41: 185–187.
Zhao X, Huang K, Zhu Z, Chen S, Hu R (2007) Correlation between expression of leptin and clinicopathological features and prognosis in patients with gastric cancer. J Gastroenterol Hepatol 22 (8): 1317–1321.
Acknowledgements
This research was supported by The Friends of Aberdeen and the North Centre for Oncology, Haematology and Radiotherapy, The Scottish Government Chief Scientist Office (Grant number CZB/4/747), the Grampian Gastro-oesophageal Cancer Research Fund (GASTROCAN), and National Health Service Grampian Research & Development. We are grateful to Nicky Fyfe for assistance with construction of the tissue microarray and to Dr Khyati Parikh for assistance with the leptin antagonist experiments. We are also grateful to the NHS Grampian bio-repository for their assistance.
Author contributions
Design and conception: RDP; provision of study materials and patients: RDP, GHB, GIM, JL, PP, KP, SN, HIG and PT; collection and assembly of data: RDP, EC-D, GHB, GIM, FJG,AD, FM, TA, IF, AW, AD-S, LS, GU, MF, HIG and PT; data analysis and interpretation: RDP, GHB, EC-D, GIM, FJG, AD, FM, TA, IF, HG and PT; writing of manuscript and final approval of manuscript: all authors.
Data Archiving
Gene expression data and experimental details are available in MIAME compliant format in ArrayExpress (http://www.ebi.ac.uk/arrayexpress/), accession number E-MEXP-3730.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work was presented in part as an oral presentation (Abstract No. 1) at the American Society for Clinical Oncology 2012 Gastrointestinal Cancers Symposium, 19 January 2012, in San Francisco.
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Bain, G., Collie-Duguid, E., Murray, G. et al. Tumour expression of leptin is associated with chemotherapy resistance and therapy-independent prognosis in gastro-oesophageal adenocarcinomas. Br J Cancer 110, 1525–1534 (2014). https://doi.org/10.1038/bjc.2014.45
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2014.45
Keywords
This article is cited by
-
Obesity and cancer: focus on leptin
Molecular Biology Reports (2023)
-
The ambiguous role of obesity in oncology by promoting cancer but boosting antitumor immunotherapy
Journal of Biomedical Science (2022)
-
Leptin activates Akt in oesophageal cancer cells via multiple atorvastatin-sensitive small GTPases
Molecular and Cellular Biochemistry (2021)
-
Novel biomarkers for risk stratification of Barrett’s oesophagus associated neoplastic progression–epithelial HMGB1 expression and stromal lymphocytic phenotype
British Journal of Cancer (2020)
-
Leptin-induced signaling pathways in cancer cell migration and invasion
Cellular Oncology (2019)